Introduction
Prostate cancer (PCa) is the most frequently
diagnosed cancer type in 105 countries (with a total of 36 cancer
types identified in 185 countries) and the most common cause of
death from malignancy among men (1). Based on data obtained between 2010
and 2014, the number of new cases of PCa was 119.8 per 100,000 men
per year, and the number of deaths was 20.1 per 100,000 men per
year in the United States of America (2,3).
Most PCa cases are indolent, with a low risk of lethality. Death
from PCa is mainly caused by metastasis when cancer cells spread to
other areas of the body, such as the pelvic and retroperitoneal
lymph nodes, the bladder, bones and the brain. Bone metastasis is
the most serious type of metastatic PCa (4), and it is a hallmark of progressive
and castration-resistant PCa. Bone metastasis develops in multiple
stages, including colonization (entrance of circulating cancer
cells to the bone marrow compartment), dormancy (adaption of cancer
cells to the bone microenvironment and a long dormancy period),
reactivation and development, (change of cancer cells from dormant
to actively proliferating) and reconstruction (change of the
original bone structure and function by the cancer cells) (5). Following bone metastasis, the
malignant proliferation rate of cancer cells is appreciably
accelerated (6). Patients with
bone metastasis have lost their best opportunity for surgery, and
subsequently, androgen deprivation therapy (ADT) is applied as the
next most common and effective treatment for metastatic PCa
(7). However, metastatic PCa
eventually develops resistance to castration, with few remaining
therapeutic options, and ultimately results in a poor patient
prognosis (8,9). Therefore, exploration of the
underlying mechanism of bone metastasis in PCa and identification
of novel therapeutic targets to address these conditions are
urgently needed.
Metastasis-free survival (MFS) is a new index that
has been demonstrated as a useful surrogate for overall survival
(OS) (10). In recent years, MFS
has gradually replaced OS to evaluate the benefits of ADT in
patients with primary PCa. OS is the traditional primary efficacy
endpoint in clinical studies of advanced PCa; however, owing to the
indolent nature of PCa, adjuvant clinical trials in PCa take more
than a decade to reach the irrefutable endpoint of OS (11). In addition, once tumor metastasis
occurs, the quality of life and outcome of patients decreases
significantly; therefore, it is more reasonable to develop a
meaningful treatment plan by assessing metastatic events. Thus, MFS
may be a useful indicator of prognoses in PCa research. MFS was
defined in clinical trials as the time from enrollment in the study
or from treatment initiation until the detection of generalized
disease manifesting with the development of distant metastases, or
until the patient's death; non-PCa deaths were not counted as an
event (12).
Kinesin family member 11 (KIF11), a molecular motor
protein essential in mitosis, promotes bipolar spindle formation
and chromosome movement during mitosis, and mediates diverse
trafficking processes in the cytoplasm during interphase (13). Reports have indicated that KIF11 is
overexpressed in various malignancies and is correlated with poor
prognoses. Li et al (14)
showed that migration and invasion abilities decreased after
inhibiting KIF11 in breast cancer. The KIF11 inhibitor also
significantly reduced the tumor volume. In addition, Daigo et
al (15) reported that a high
level of KIF11 expression is significantly associated with poor
prognoses in patients with oral cancer. Piao et al (16) showed that the KIF11 expression may
be indicative of PCa aggressiveness.
Vascular endothelial growth factor (VEGF) is a
cytokine that plays a key role in angiogenesis and is essential in
the formation of various solid tumors (17). VEGF is critical for tumor growth.
Agents targeting VEGF, including VEGF antibodies, bevacizumab and
VEGF receptor tyrosine kinase inhibitors, are gradually being
incorporated into clinical cancer therapies, leading to major
advances in the treatment of various tumors, such as metastatic
breast cancer, non-small cell lung cancer, glioblastoma, renal cell
carcinoma, ovarian cancer and cervical cancer (18,19).
Angiogenesis is essential in PCa development and metastasis.
Moreover, VEGF has already been associated with metastasis and
angiogenesis in PCa (20). High
VEGF expression levels predict a strong invasive and metastatic
capacity of PCa.
A combination of statistical and bioinformatic
methods was used in the present study to identify genes that
promote bone metastasis in PCa. Bioinformatic analysis represents
the application of information technology and computer science in
the field of molecular biology, and is widely used in functional
analyses of DNA, RNA and proteins; these analysis results are vital
for guiding clinical work. KIF11 was identified as an independent
risk factor for bone metastasis in PCa in the present study. The
study evaluated the correlation between KIF11 and VEGF expression
in PCa tissue samples, and investigated the influence of KIF11
expression on MFS in patients with PCa.
Materials and methods
Bioinformatics analysis
Gene profile download and
processing
The raw expression profile was downloaded from the
Gene Expression Omnibus (GEO; http://www.ncbi.nlm.nih.gov/geo/) to compare gene
expression levels between PCa bone metastasis tissues and primary
PCa tissues. The gene expression datasets GSE32269 (21), GSE74367 (22) and GSE77930 (23) were downloaded based on the GPL147,
GPL15659 and GPL21289 platforms, respectively. Clinical information
on the corresponding samples was available.
A robust multi-array average was used to correct and
normalize the raw expression data for each dataset. The three
datasets were then merged using the Perl programming language
(https://www.perl.org/). The ‘SVA’ package of R
software (http://www.r-project.org/) was
performed to eliminate batch effects and other unrelated variables
in high-throughput experiments.
Co-expression network
construction
The weighted gene co-expression network analysis
(WGCNA) R package (https://cran.r-project.org/web/packages/WGCNA/index.html)
was used to construct the gene co-expression network in the
datasets. The soft-thresholding power β was calculated during the
construction of each module using the pickSoftThreshold function of
the WGCNA. The power value was screened using a gradient algorithm
to test the independence, and the power values of the different
modules ranged from 1 to 20. Gene modules were constructed after
determining a suitable power value when the index value for the
reference dataset exceeded 0.8. A minimum number of 30 was set for
each module, and the heatmap tool package was used to analyze and
visualize the strength of the correlation between each module. A
cut line (0.25) was chosen to generate a dendrogram plot.
Construction of module-clinic trait
relationships
Modules from the WGCNA were identified based on gene
expression similarities in the samples. The relationship between
clinical traits (occurrence or absence of bone metastasis of PCa)
and each module was calculated to acquire the module of interest.
The gene module most significantly correlated with ‘type,’ namely
the presence or absence of bone metastasis in PCa, was retained for
the next step.
Functional enrichment analysis
Metascape (http://metascape.org) is a free, thoroughly maintained
and user-friendly gene list analysis tool for gene annotation and
analysis. Specifically, it is an automated meta-analysis tool used
to understand common and unique pathways within a group of
orthogonal target discovery studies. In the present study,
Metascape was used to conduct pathway and process enrichment
analyses of the gene module most relevant to the clinical traits
screened out in WGCNA. Gene Ontology (GO; http://geneontology.org/) and Kyoto Encyclopedia of
Genes and Genomes (KEGG; http://www.kegg.jp/) enrichment analysis mainly
described the biological processes, cellular components and
molecular functions associated with the module genes. Information
on the role and function of modular genes was enriched using
Metascape. Terms with P<0.05, a minimum count of 3, and an
enrichment factor of >1.5 were considered significant.
Screening of differentially expressed
genes
The differentially expressed genes (DEGs) of bone
metastasis in PCa and primary PCa tissues were detected using the
‘Limma’ package of R software (https://cran.r-project.org/src/contrib/Archive/limma/),
with cut-off criteria of P<0.05 and absolute |logFC|>1. The
DEGs and the module of interest from WGCNA were then overlapped to
obtain the common DEGs.
Construction of protein-protein
interaction (PPI) and selection of hub genes
A PPI network was constructed using the STRING
online database (http://string-db.org) and imported into the Cytoscape
software (https://cytoscape.org/) for
visualization and subsequent analysis. Four algorithms were used
(betweenness, closeness, Eccentricity and Radiality) in Cytoscape
to calculate the top 10 hub genes. A Venn plot was constructed to
identify common hub genes. The Gene Expression Profiling
Interactive Analysis (GEPIA; http://gepia.cancer.pku.cn/) database was used to
analyze disease-free survival (DFS) time between samples with high
and low expression of the hub genes. The Comparative Toxicogenomics
Database (CTD; http://ctdbase.org/) is a web-based
database that provides information on the relationship between
genes, proteins and diseases; the relationships between gene
products and malignancy were analyzed using this database.
Clinical samples and ethics
statement
Inclusion criteria: i) Patients diagnosed with PCa;
ii) those who refused or were unable to tolerate surgical
management; and iii) those who accepted a prostate needle biopsy.
Exclusion criteria: i) A history of other malignant tumors; ii)
incomplete clinical data; iii) distant metastasis at diagnosis; and
iv) a life expectancy of >5 years. A total of 60 patients with
primary PCa who visited the Fourth Affiliated Hospital of Hebei
Medical University (Shijiazhuang, China) between January 2014 and
December 2016 were involved in this study, 45 of whom eventually
developed bone metastasis. All patients underwent prostate biopsy
and ADT. Tissues from PCa biopsies were collected from all
patients. Tumor biopsy tissues were fixed in 10% formalin buffer
for 24 h at 25°C, paraffin-embedded and then sectioned to a 5-µm
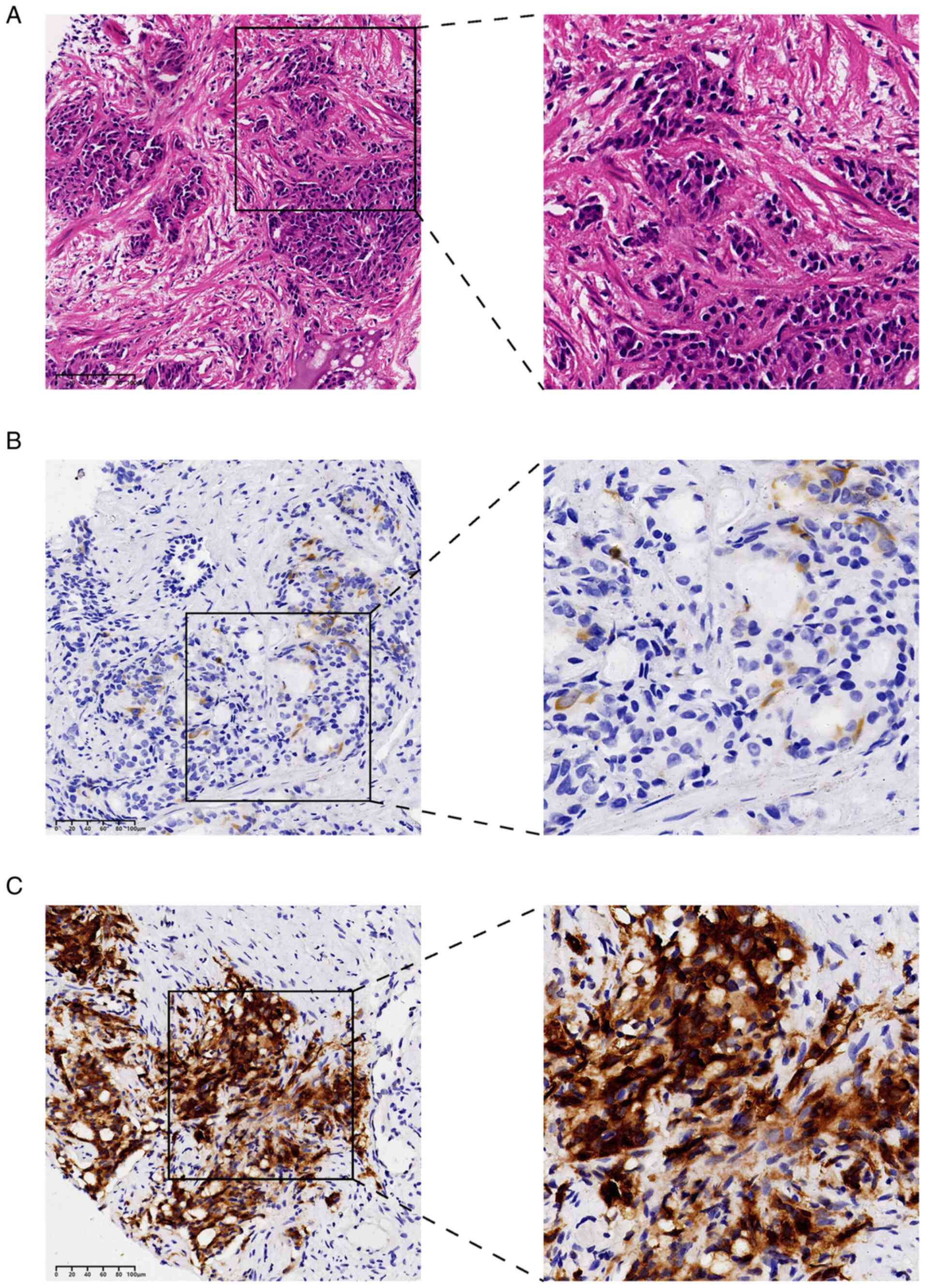
thickness. Tumor biopsy tissues was used to perform H&E and
immunohistochemistry. The detailed experimental procedures for
H&E staining were as described previously (24). Participants were followed through a
time horizon of 5 years. The demographic and clinical
characteristics [age, primary tumor size, T stage,
prostate-specific antigen (PSA) level and Gleason score (25)], follow-up time and survival
information of each patient were collected retrospectively. The
staging standard referred to the AJCC Cancer Staging Manual (8th
Edition) (26). Furthermore, the
patients were not treated with radiochemotherapy.
Ethical approval was obtained from the Ethics
Committee of the Fourth Affiliated Hospital of Hebei Medical
University (approval no. 2022KY066). Written informed consent was
obtained from all participants in this study. All experiments were
performed in accordance with the Declaration of Helsinki.
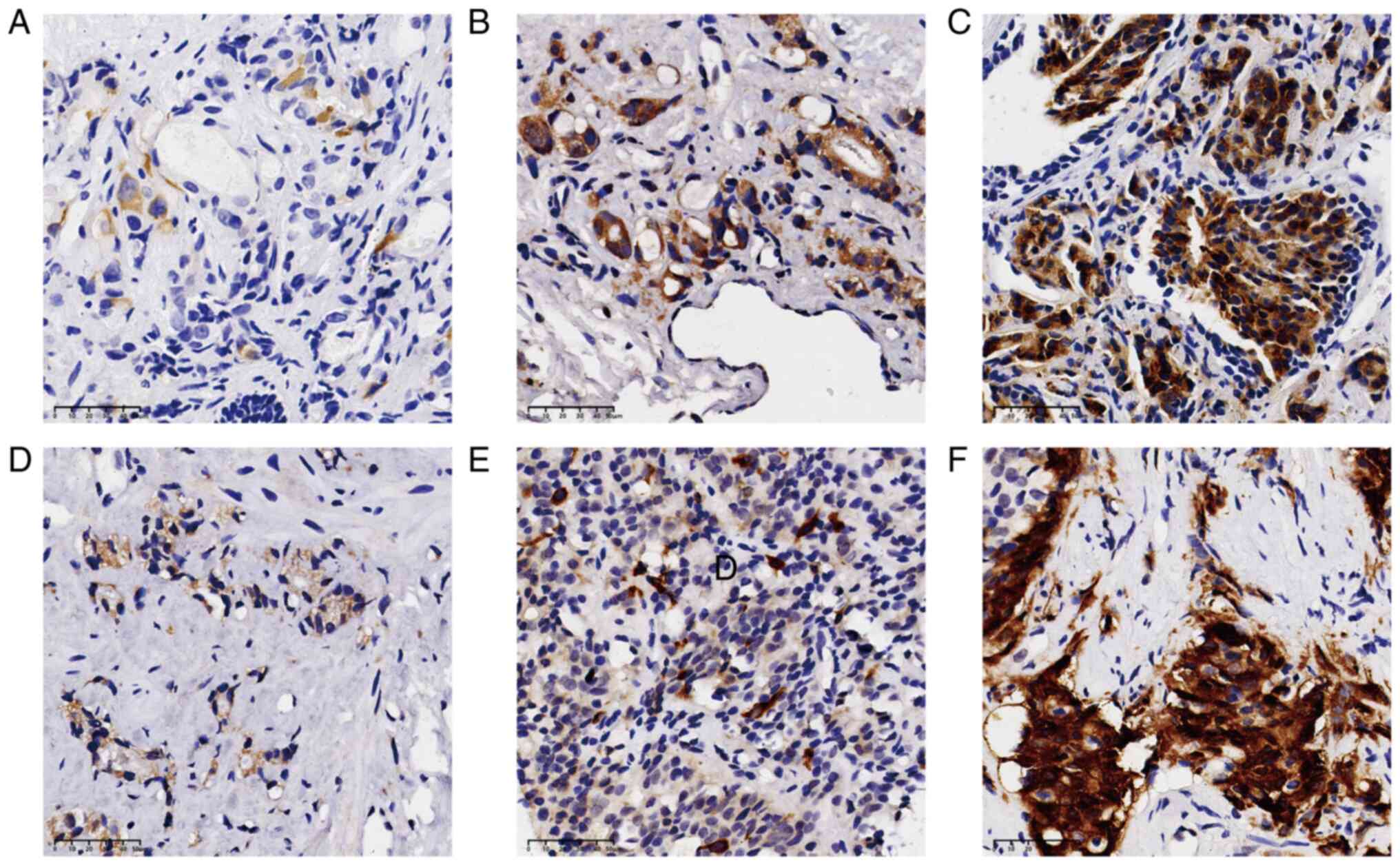
Immunohistochemistry
For immunohistochemistry, biopsy tissues sections
were blocked with 3% hydrogen peroxide at room temperature for 10
min. Primary antibody incubation was performed overnight at 4°C
using rabbit KIF11 (1:4,000; catalog no. ab254298; Abcam) and
rabbit VEGF (1:100; catalog no. ab52917; Abcam) antibodies.
Secondary antibody incubation was performed for 1 h using using
goat anti-rabbit IgG antibodies (1:100; catalog no. ab150077;
Abcam). Finally, the staining was independently evaluated using a
high-resolution optical scanner, Nanozoomer 2.0 HT, by three
pathologists blinded to all the data. If differences were observed,
disagreements were settled through discussion. KIF11 and VEGF were
scored based on the staining intensity of brown-colored
diaminobenzidine (DAB) as follows: Score of 0, <1%; score of 1,
1–25%; score of 2, 25–50%; score of 3, 51–80%; and score of 4,
>80%. The intensity of staining was recorded as follows: Grade
0, negative; grade 1, buff; grade 2, brownish-yellow; and grade 3,
tan. The product of the staining percentage and intensity grade was
used to evaluate the final immunostaining score, and the results
were defined as low (score 0–3), moderate (score 4–7) or high
(score >7).
Statistical analysis
To determine independent risk factors for PCa bone
metastasis, univariate and multivariate logistic proportional
hazard regression analyses were conducted for hub genes using
bioinformatic analysis. The occurrence of a bone metastasis event
or the last follow-up date through to December 2020 was defined as
the endpoint. Metastasis-free survival (MFS) was defined as the
time from diagnosis to bone metastasis or last follow-up.
Correlation analysis was performed using Spearman's ρ test. Cox's
proportional hazards regression was used as the univariate and
multivariate analysis methodology. The Kaplan-Meier curve method
was used to evaluate MFS using the log-rank test. All statistical
analyses were performed using SPSS 25.0 (IBM Corp.). P<0.05 was
used to indicate a statistically significant difference.
Results
Bioinformatic analysis
GEO dataset
The three datasets (GSE32269, GSE74367 and GSE77930)
downloaded from the GEO database included 49 PCa samples with bone
metastasis and 46 primary PCa samples in total (Table I).
 | Table I.Prostate cancer bone metastasis
microarray datasets from different Gene Expression Omnibus
datasets. |
Table I.
Prostate cancer bone metastasis
microarray datasets from different Gene Expression Omnibus
datasets.
| Series | Platform | Primary samples,
n | Bone metastasis
samples, n | Total, n |
|---|
| GSE32269 | GPL96 | 22 | 29 | 51 |
| GSE74367 | GPL15659 | 11 | 7 | 18 |
| GSE77930 | GPL21289 | 13 | 13 | 26 |
| Total |
| 46 | 49 | 95 |
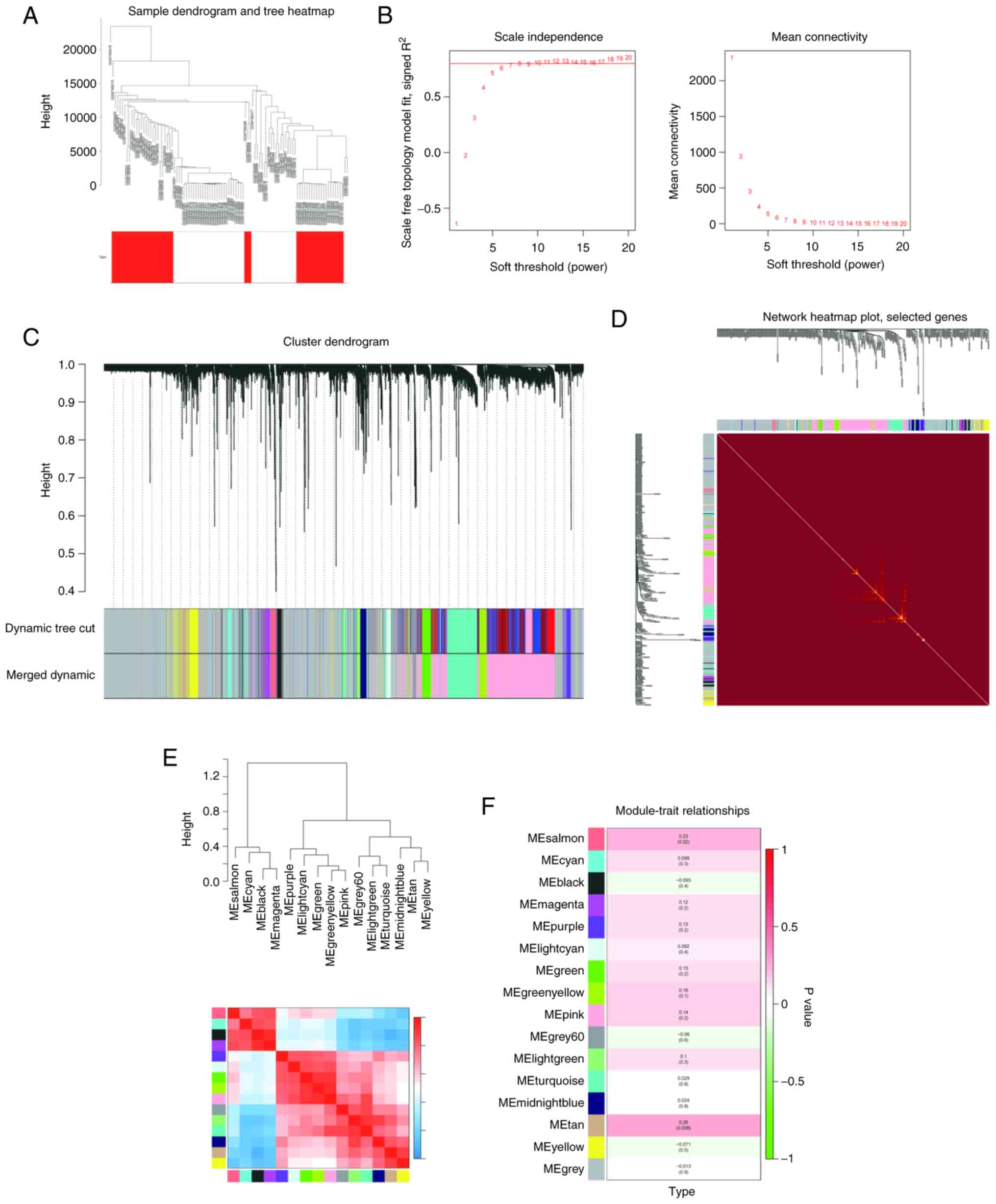
WGCNA construction
All the samples were included in the analysis. The
results of the hierarchical clustering analysis showed that there
were no obvious outliers, and all 95 samples were included in the
co-expression network analysis. A total of 16 corresponding modules
were determined (Fig. 1A-E).
Subsequently, clinical information (occurrence of PCa bone
metastasis) was imported, and the correlation coefficient between
each module and PCa bone metastasis was calculated (Fig. 1F). The results showed that the tan
module was most closely associated with PCa bone metastasis
(ρ=0.26; P=0.008), including 147 genes. Therefore, the tan module
was selected for further analyses.
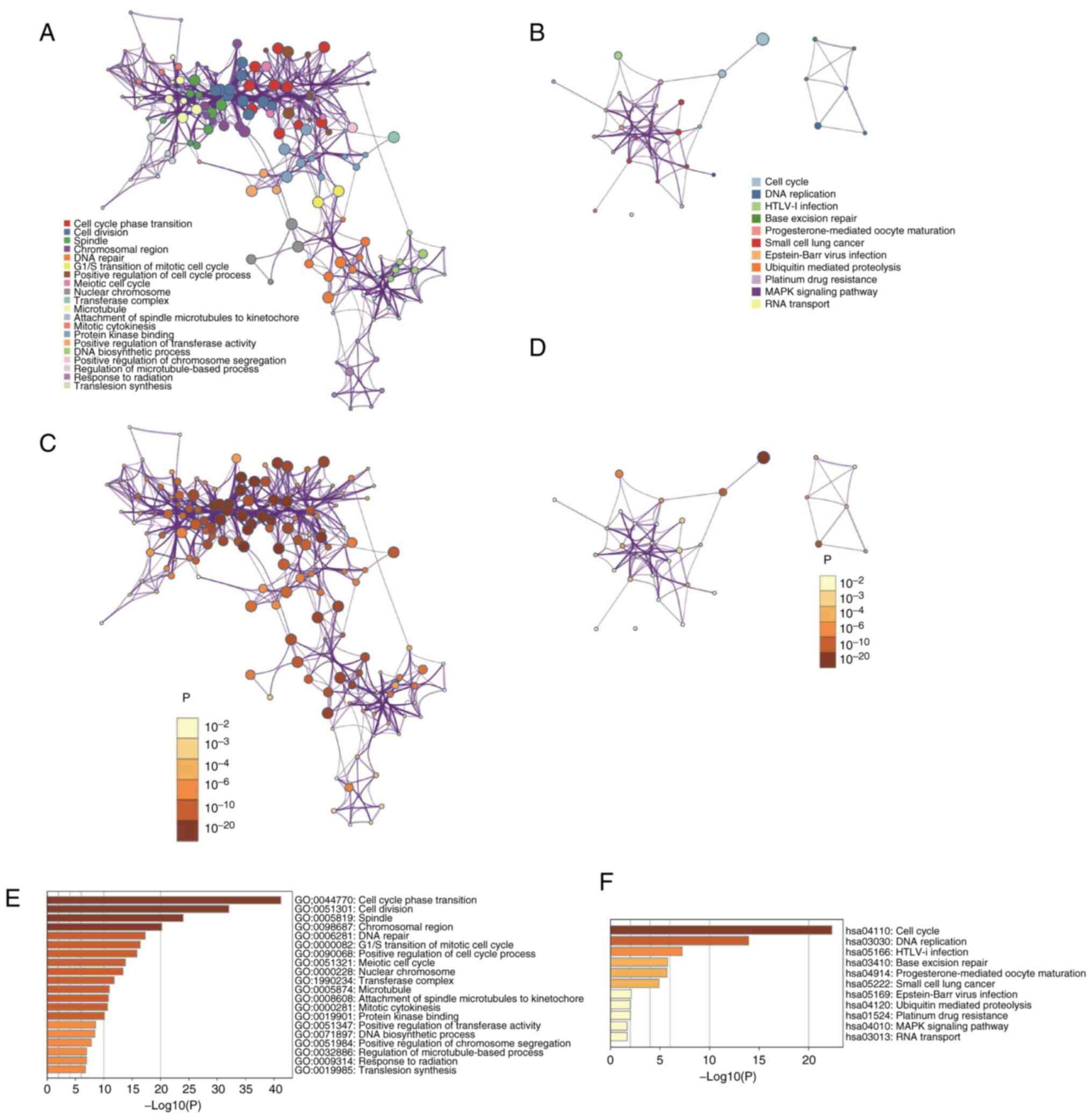
Functional enrichment analysis
GO and KEGG function enrichment analyses were used
to explore the potential functions and pathways of the genes in the
tan module of Metascape. The GO analysis results showed that the
genes in the tan module mainly regulated (top 5 terms) ‘cell cycle
phase transition’, ‘cell division’, ‘spindle’, ‘chromosomal
regions’ and ‘DNA repair’. KEGG pathway analysis showed enrichment
in the ‘cell cycle’, ‘DNA replication’, ‘HTLV–I infection’, ‘base
excision repair’ and ‘progesterone-mediated oocyte maturation’
(Fig. 2A-F).
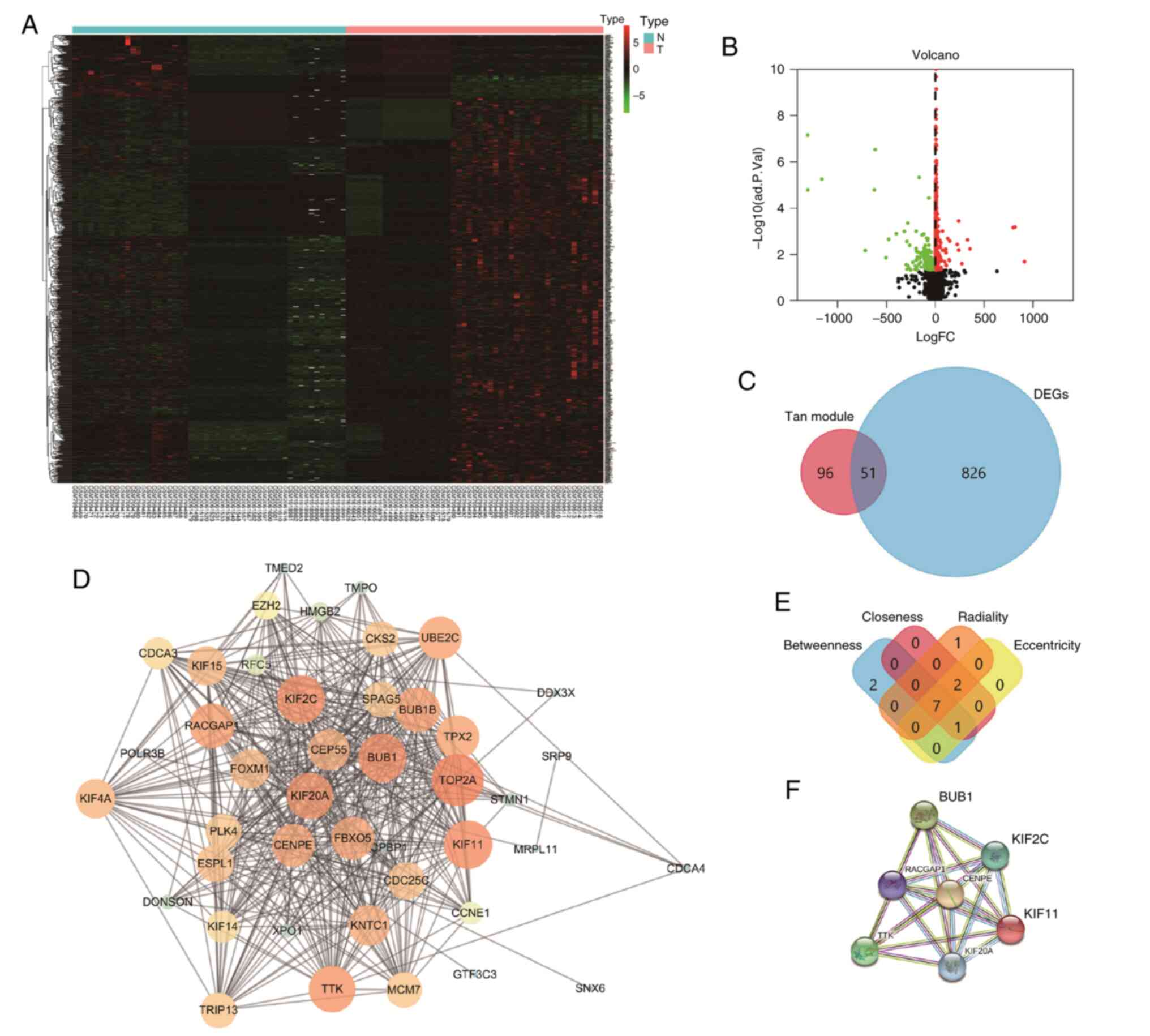
Selection of DEGs
All 49 PCa samples with bone metastasis and 46
primary PCa samples were included in a differential expression
analysis. A total of 877 DEGs were screened, and volcano plots and
heat maps were subsequently created (Fig. 3A and B). A Venn plot was
constructed showing the overlap of 51 common genes between the DEGs
and tan model genes (Fig. 3C).
Construction of PPIs and selection of
hub genes
A PPI network was constructed for the 51 common
genes (Fig. 3D). Four different
algorithms (betweenness, closeness, eccentricity and radiality)
were used to calculate hub genes, and the common hub genes of the
four different algorithms were obtained (Fig. 3E). Ultimately, seven hub genes
(BUB1, KIF2C, RACGAP1, CENPE, KIF11, TTK and KIF20A) were
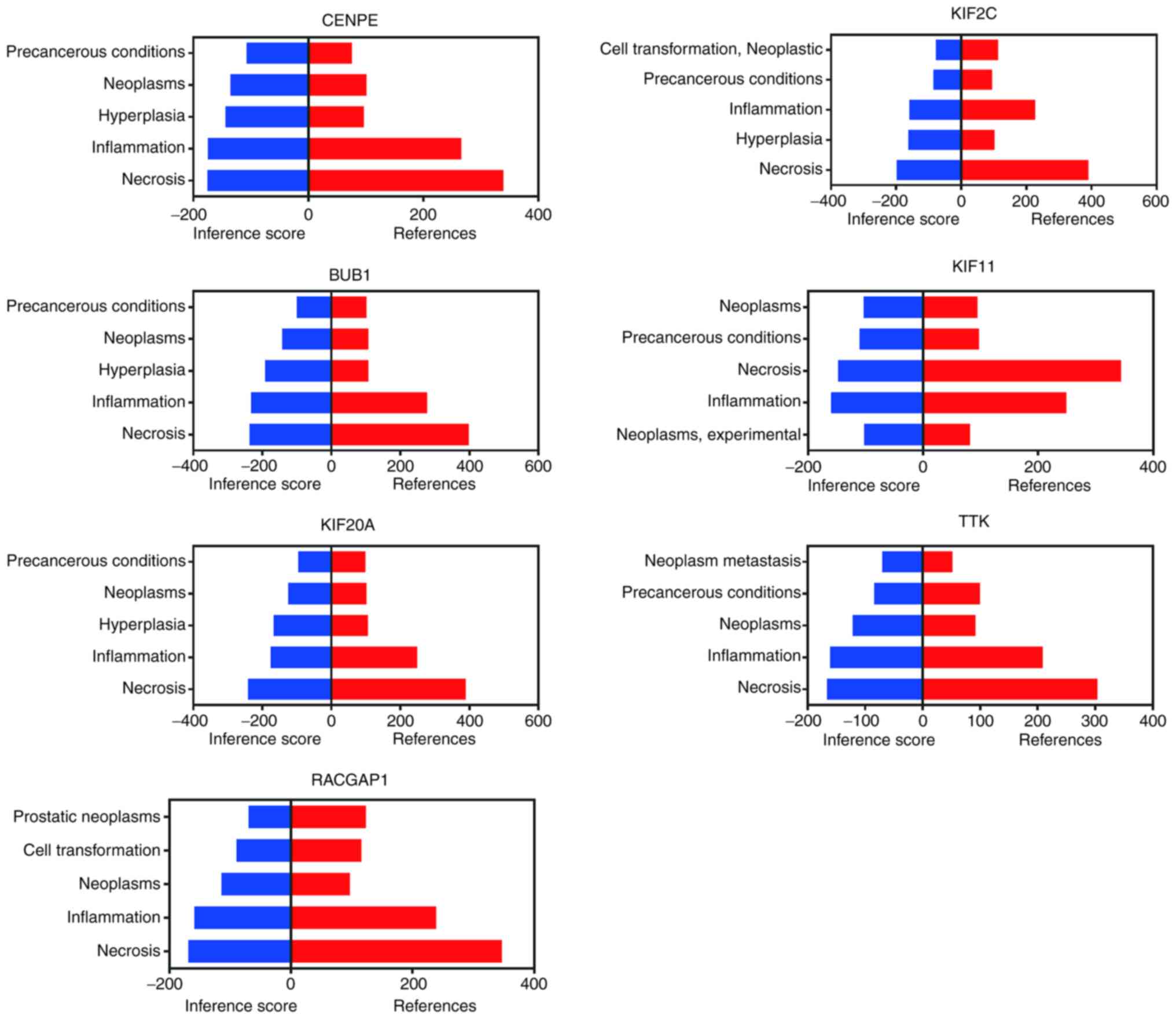
identified (Fig. 3F). The results
of the CTD analysis showed that all seven hub genes had a strong
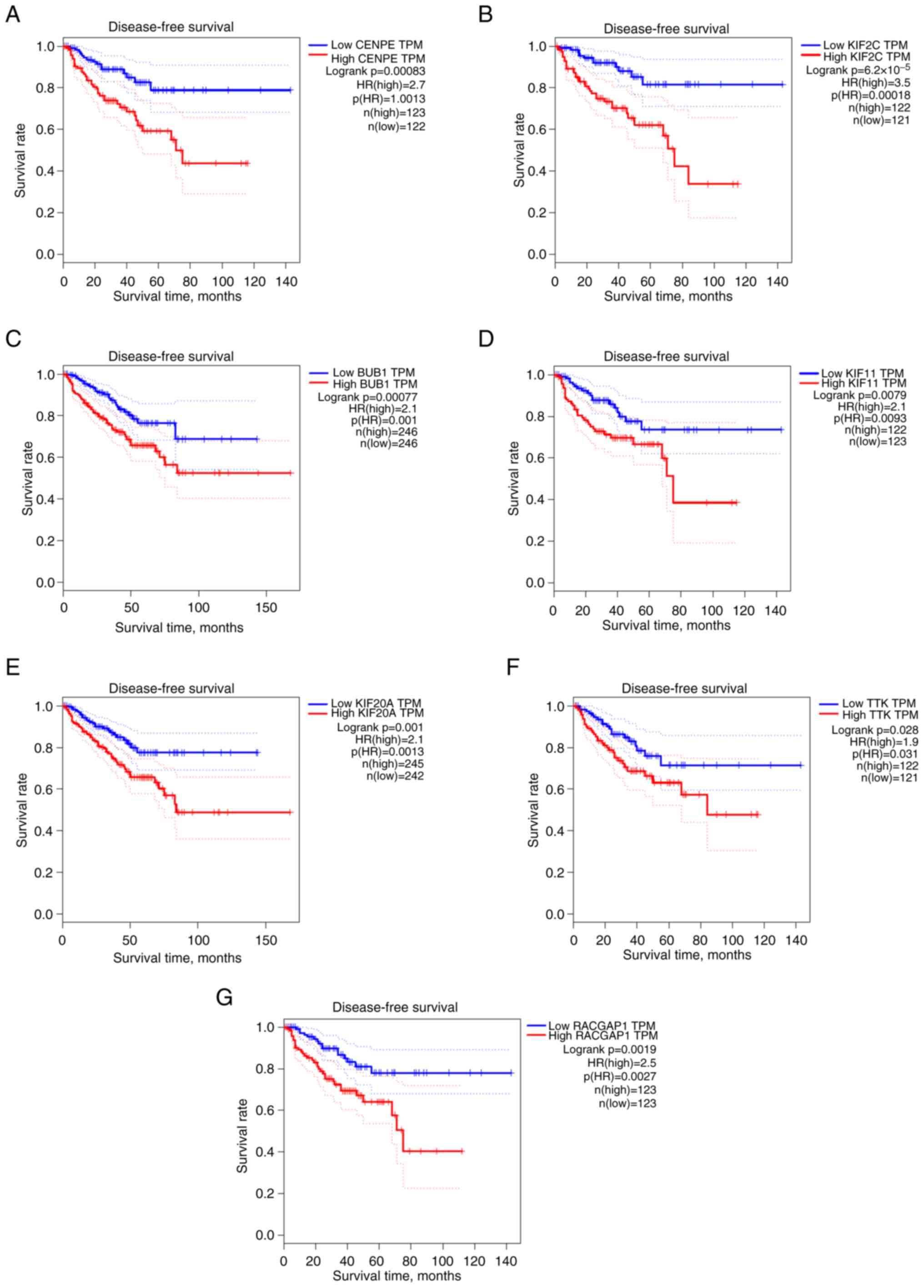
correlation with necrosis-related biological process (Fig. 4). The GEPIA website was used to
analyze the DFS rates of the seven hub genes. Results from GEPIA
showed that all seven genes, including CENPE (log rank P=0.00083;
HR, 2.7), KIF2C (log rank P=6.2×10−5; HR, 3.5), BUB1
(log rank P=0.00077; HR, 2.1), KIF11 (log rank P=0.0079; HR, 2.1),
KIF20A (log rank P=0.001; HR, 2.1), TTK (log rank P=0.028; HR, 1.9)
and RACGAP1 (log rank P=0.0019; HR, 2.5), were significantly
associated with DFS (Fig. 5).
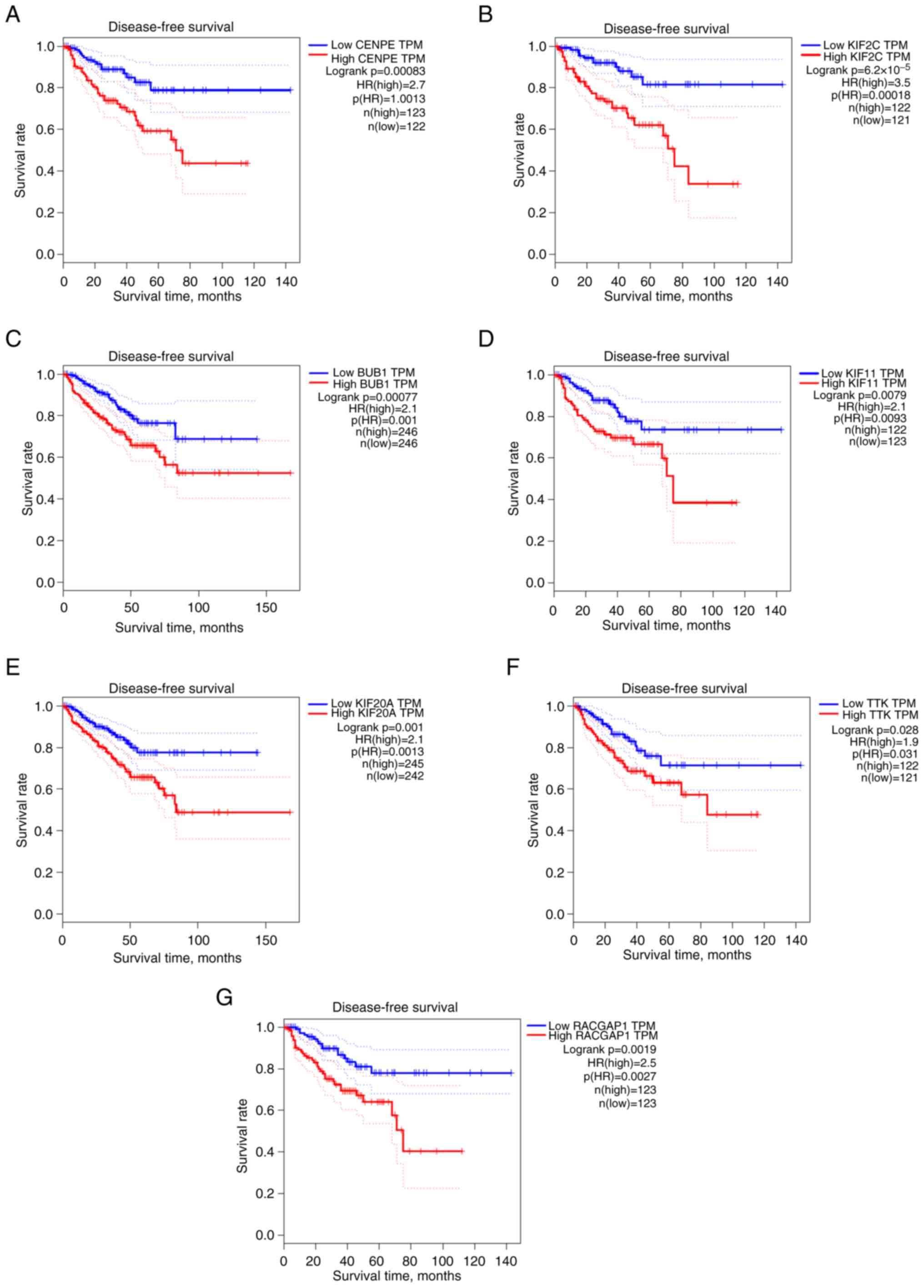 | Figure 5.DFS analysis, based on Gene
Expression Profiling Interactive Analysis, for the hub genes. (A-G)
DFS analysis of seven hub genes (BUB1, KIF2C, RACGAP1, CENPE,
KIF11, TTK and KIF20A). KIF11, kinesin family member 11; DFS,
disease-free survival; HR, hazard ratio; TPM, transcripts per
kilobase million. |
Logistics regression analysis
Univariate and multivariate logistic proportional
hazard regression analyses were conducted for the seven hub genes
(Table II). The results of
multivariate regression indicated that only KIF11 (P=0.038; HR,
2.331; 95% CI, 1.049-5.178) represented an independent factor that
significantly influenced bone metastasis in PCa.
 | Table II.Univariate and multivariate logistic
proportional regression analysis to assess the association between
hub genes and bone metastasis of prostate cancer. |
Table II.
Univariate and multivariate logistic
proportional regression analysis to assess the association between
hub genes and bone metastasis of prostate cancer.
|
| Univariate | Multivariate |
|---|
|
|
|
|
|---|
| Gene | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| KIF11 | 2.331 | 1.049-5.178 | 0.038 | 2.331 | 1.049-5.178 | 0.038 |
| CENPE | 1.681 | 0.765-3.694 | 0.196 | - | - | - |
| KIF2C | 0.758 | 0.347-1.658 | 0.488 | - | - | - |
| BUB1 | 1.221 | 0.515-2.456 | 0.767 | - | - | - |
| KIF20A | 0.550 | 0.250-1.211 | 0.138 | - | - | - |
| TTK | 1.221 | 0.559-2.667 | 0.617 | - | - | - |
| RACGAP1 | 0.646 | 0.295-1.417 | 0.276 | - | - | - |
Expression of KIF11 and VEGF in
clinical samples
A summary of the associations between the two
proteins (KIF11 and VEGF) and clinicopathological characteristics
from the 60 clinical samples is shown in Table III. The expression of KIF11 was
low in 15 (25.0%), moderate in 19 (31.7%) and high in 26 (43.3%)
patients, whereas the expression of VEGF was low in 16 (26.7%),
moderate in 18 (30.0%) and high in 26 (43.3%) patients. The
expression of KIF11 was significantly higher in bone metastatic PCa
tissue than in non-metastatic tissue (Fig. 6). Moreover, both proteins (KIF11
and VEGF) were significantly associated with the T stage (P=0.001
and P=0.002, respectively), PSA (P=0.015 and P=0.044, respectively)
and Gleason score (P<0.001 and P=0.001, respectively) (Table III). However, there were no
statistically significant differences between KIF11 and VEGF for
other clinicopathological features. The results also indicated that
the expression of KIF11 was correlated with the expression of VEGF
(P<0.001) (Table IV; Fig. 7).
 | Table III.Clinicopathological variables and the
expression of KIF11 and VEGF. |
Table III.
Clinicopathological variables and the
expression of KIF11 and VEGF.
| Variable | Total patients,
n | KIF11, n (%) |
| VEGF, n (%) |
|
|---|
|
|
|
|
|---|
| -/+ | ++ | +++ | P-value | -/+ | ++ | +++ | P-value |
|---|
| Age, years |
|
|
|
| 0.617 |
|
|
| 0.126 |
|
≥65 | 32 | 9 (28.1) | 11 (34.4) | 12 (37.5) |
| 10 (31.2) | 6 (18.8) | 16 (50.0) |
|
|
<65 | 28 | 6 (21.4) | 8 (28.6) | 14 (50.0) |
| 6 (21.4) | 12 (42.9) | 10 (35.7) |
|
| Primary tumor size,
cm |
|
|
|
| 0.633 |
|
|
| 0.493 |
|
<2 | 33 | 7 (21.2) | 10 (30.3) | 16 (48.5) |
| 8 (24.2) | 12 (36.4) | 13 (39.4) |
|
| ≥2 | 27 | 8 (29.6) | 9 (33.3) | 10 (37.0) |
| 8 (29.6) | 6 (22.2) | 13 (48.1) |
|
| T stage |
|
|
|
| 0.001a |
|
|
| 0.002a |
|
T1/T2 | 17 | 9 (52.9) | 2 (11.8) | 6 (35.3) |
| 10 (58.8) | 4 (23.5) | 3 (17.6) |
|
| T3 | 28 | 5 (17.9) | 14 (50.0) | 9 (32.1) |
| 6 (21.4) | 10 (35.7) | 12 (42.9) |
|
| T4 | 15 | 1 (6.7) | 3 (20.0) | 11 (73.3) |
| 0 (0.00) | 4 (26.7) | 11 (73.3) |
|
| PSA, ng/ml |
|
|
|
| 0.015a |
|
|
| 0.044a |
|
<20 | 37 | 13 (35.1) | 13 (35.1) | 11 (29.7) |
| 14 (37.8) | 9 (24.3) | 14 (37.8) |
|
|
≥20 | 23 | 2 (8.7) | 6 (26.1) | 15 (65.2) |
| 2 (8.7) | 9 (39.1) | 12 (52.2) |
|
| Gleason score |
|
|
|
|
<0.001a |
|
|
| 0.001a |
| ≤6 | 9 | 8 (88.9) | 1 (11.1) | 0 (00.0) |
| 7 (77.8) | 2 (22.2) | 0 (00.0) |
|
| 7
(3+4) | 20 | 7 (35.0) | 10 (50.0) | 3 (15.0) |
| 7 (35.0) | 7 (35.0) | 6 (30.0) |
|
| 7
(4+3) | 15 | 0 (00.0) | 5 (33.3) | 10 (66.6) |
| 1 (6.7) | 5 (33.3) | 9 (60.0) |
|
| ≥8 | 16 | 0 (00.0) | 3 (18.8) | 13 (81.3) |
| 1 (6.3) | 4 (25.0) | 11 (68.8) |
|
 | Table IV.Correlation between KIF11 and VEGF
expression. |
Table IV.
Correlation between KIF11 and VEGF
expression.
|
|
| KIF11 |
|
|---|
|
|
|
|
|
|---|
|
Characteristics | Total patients,
n | -/+, n (%) | ++, n (%) | +++, n (%) | P-value |
|---|
| VEGF |
|
|
|
|
<0.001a |
|
-/+ | 16 | 12 (20.0) | 3 (5.0) | 1 (1.7) |
|
| ++ | 18 | 2 (3.3) | 8 (13.3) | 8 (13.3) |
|
|
+++ | 26 | 1 (1.7) | 8 (13.3) | 17 (28.3) |
|
| Total | 60 | 15 | 19 | 26 |
|
High expression of KIF11 and VEGF
leads to poor MFS in patients with PCa
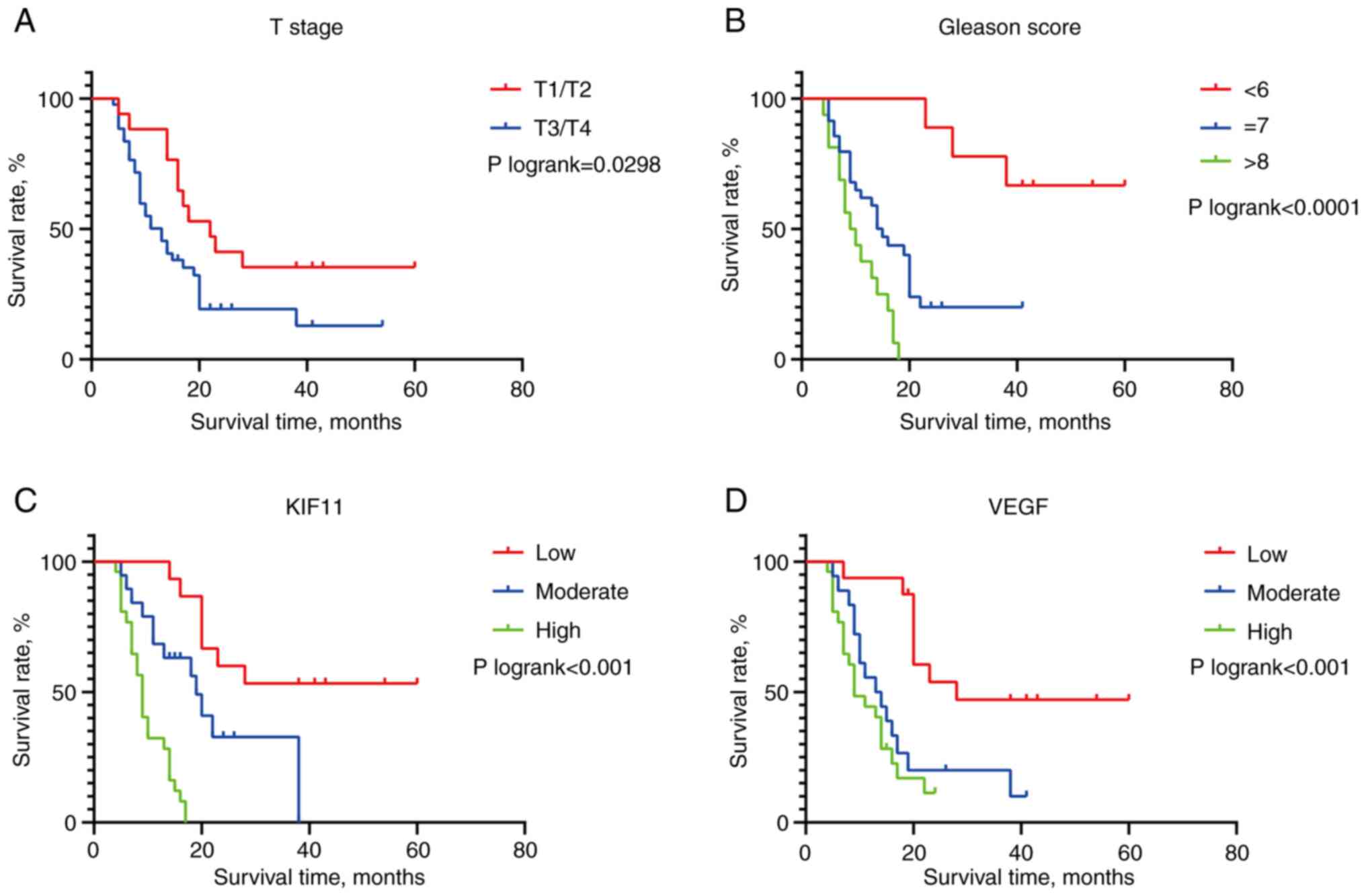
The association between the expression of the two
proteins (KIF11 and VEGF) and the MFS of patients with PCa was
examined using a univariate Cox analysis. The results showed that
the high T stage (P=0.001), high PSA level (P=0.013) and high
Gleason score (P<0.001) were significant prognostic factors for
poor MFS for patients with PCa. Furthermore, the univariate Cox
regression analysis indicated that upregulated KIF11 (moderate
P=0.022 and High P<0.001, compared with low expression) and VEGF
(moderate P=0.005 and high P<0.001, compared with low
expression) expression was associated the poor prognosis of
patients with PCa (Table V).
 | Table V.Univariate Cox proportional
regression analysis of clinicopathological factors associated with
MFS. |
Table V.
Univariate Cox proportional
regression analysis of clinicopathological factors associated with
MFS.
|
|
| MFS |
|---|
|
|
|
|
|---|
|
Characteristics | Total patients,
n | HR | 95% CI | P-value |
|---|
| Age, years |
|
|
|
|
|
≥65 | 32 | 1.000 | - | - |
|
<65 | 28 | 1.312 | 0.725-2.376 | 0.370 |
| Primary tumor size,
cm |
|
|
|
|
|
<2 | 33 | 1.000 | - | - |
| ≥2 | 27 | 0.859 | 0.467-1.581 | 0.625 |
| T stage |
|
|
|
|
|
T1/T2 | 17 | 1.000 | - | 0.001 |
| T3 | 28 | 1.613 | 0.766-3.397 | 0.208 |
| T4 | 15 | 5.217 | 2.115-12.867 | <0.001 |
| PSA,
ng/mla |
|
|
|
|
|
≤20 | 37 | 1.000 | - |
|
|
≥20 | 23 | 2.171 | 1.174-4.015 | 0.013 |
| Gleason
scorea |
|
|
|
|
| ≤6 | 9 | 1.000 | - | <0.001 |
| 7
(3+4) | 20 | 4.682 | 1.262-17.378 | 0.021 |
| 7
(4+3) | 15 | 35.443 | 7.514-167.186 | <0.001 |
| ≥8 | 16 | 30.689 | 6.940-135.713 | <0.001 |
| KIF11a |
|
|
|
|
| Low
(−/+) | 15 | 1.000 | - | <0.001 |
|
Moderate (++) | 19 | 3.125 | 1.175-8.311 | 0.022 |
| High
(+++) | 26 | 16.468 | 5.618-48.276 | <0.001 |
| VEGFa |
|
|
|
|
| Low
(−/+) | 16 | 1.000 | - | 0.001 |
|
Moderate (++) | 18 | 3.527 | 1.464-8.496 | 0.005 |
| High
(+++) | 26 | 5.127 | 2.160-12.167 | <0.001 |
KIF11: An independent MFS predictor
for patients with PCa
The results of the multivariate regression analysis
indicated that T stage (P=0.043; HR, 1.665; 95% CI, 1.016-2.729),
Gleason score (P=0.016; HR, 1.734; 95% CI, 1.108-2.714) and KIF11
(P=0.007; HR, 2.776; 95% CI, 1.315-5.859) represented independent
factors that significantly influenced the bone metastasis of PCa;
however, PSA (P=0.496; HR, 0.770; 95% CI, 0.362-1.637) and VEGF
(P=0.744; HR, 0.918; 95% CI, 0.548-1.536) showed no significance
(Table VI). The Kaplan-Meier
survival analysis is shown in Fig.
8, reflecting associations with T stage
(Plog-rank=0.0298), Gleason score
(Plog-rank<0.001), KIF11 expression
(Plog-rank<0.001) and VEGF expression
(Plog-rank<0.001).
 | Table VI.Multivariate Cox regression analysis
of clinicopathological factors associated with MFS. |
Table VI.
Multivariate Cox regression analysis
of clinicopathological factors associated with MFS.
|
| MFS |
|---|
|
|
|
|---|
| Factors | HR | 95% CI | P-value |
|---|
| PSA | 0.770 | 0.362-1.637 | 0.496 |
| VEGF | 0.918 | 0.548-1.536 | 0.744 |
| T stage | 1.665 | 1.016-2.729 | 0.043 |
| Gleason score | 1.734 | 1.108-2.714 | 0.016 |
| KIF11 | 2.776 | 1.315-5.859 | 0.007 |
Discussion
Bones represent a frequent site of metastasis in
patients with advanced solid tumors, such as breast, lung, thyroid
and renal cancer (27). Bone
metastasis is the most common type of metastasis in patients with
PCa, and it occurs in ~80% of patients with advanced PCa.
Skeletal-related events have been correlated with reduced survival
rates and quality of life in patients with PCa. The occurrence of
bone metastasis leads to a poor prognosis in these patients
(28).
KIFs are mainly involved in intracellular transport
in various cell types. KIF11, also known as kinesin-5, mediates
centrosome separation and the formation of the bipolar mitotic
spindle, driving mitosis to support cell proliferation. KIF11
inactivation results in inappropriate cell division and cell cycle
arrest during mitosis, which eventually leads to apoptosis
(29). KIF11 also appears to have
non-mitotic functions. Moreover, it regulates axonal branching and
growth cone motility, and has recently been proven to be involved
in cell motility (30,31).
WGCNA can determine the correlation between genes
and clinical traits as well as quantitatively analyze the strength
of the correlations between genes (26). In the present study, evidence from
bioinformatic analysis and multivariate logistic regression
revealed that, among seven recorded hub genes, KIF11 was an
independent factor affecting the bone metastasis of PCa. Thus, we
hypothesized that the expression of KIF11 could be used as a
prognostic marker of MFS in patients with PCa. Clinical validation
revealed that KIF11 was highly expressed in the tissues of patients
with PCa and bone metastasis, which suggests that KIF11 may be
involved in the bone metastasis process. Furthermore, a significant
correlation was found between KIF11 and VEGF expression, suggesting
a potential association between KIF11 and tumor angiogenesis. KIF11
may promote the occurrence of bone metastases by influencing
angiogenesis. Angiogenesis plays a major role in the development
and progression of PCa. However, in the field of PCa-targeted
therapy, the performance of anti-angiogenic drugs has been
disappointing. Multiple previous clinical trials have often yielded
discouraging outcomes (20,32,33).
Nevertheless, recent studies have suggested that anti-angiogenic
treatment continues to be promising (34,35).
Additionally, combination strategies, such as combination with
vaccines, immunotherapy agents and novel poly (ADP-ribose)
polymerase inhibitors, have potential applicability as treatment
options (36). The present study
findings could potentially pave the way for a change in targeted
therapy.
In the present study, follow-up data were analyzed
by Cox regression analysis. Results from univariate Cox regression
indicated that KIF11 and VEGF upregulation were correlated with
poor prognoses. PSA is the most common index used in the diagnosis
and prediction of prognosis for PCa. However, PSA was not
significant in the multivariate analysis results, which indicates
PSA may not be an independent MFS prognostic factor of bone
metastasis in PCa. This may be related to the fact that PSA can be
affected by various clinical situations such as smoking status
(37). Meanwhile, KIF11 expression
represented an independent risk factor for poor MFS upon
multivariate Cox regression analysis. This suggested that KIF11
could be used as a predictor of MFS in patients with PCa.
Elucidating the timeline of bone metastasis events is of great
significance for patients with PCa, and can contribute to the
formulation of clinical medication and markedly improve the quality
of life of the patients. KIF11 is a suitable candidate for use in
clinical research to assess the risk of bone metastasis in patients
with PCa, which may be beneficial to them.
In conclusion, the findings of the present study
improve our understanding of the molecular mechanisms underlying
bone metastasis in PCa. The results demonstrated that KIF11 may
promote bone metastasis and act as a reliable prognostic biomarker
for predicting bone metastasis in patients with PCa. This
information may be utilized to guide future clinical practices.
Acknowledgements
Not available.
Funding
The study was founded by Department of Finance of Hebei China
[grant no. jcyf (2020)397].
Availability of data and materials
The datasets generated and/or analyzed during the
current study are available in the Gene Expression Omnibus
repository, (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE32269,
https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE74367
and http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE77930).
Authors' contributions
HW and XN were responsible for study conception and
design. BL, SL and SW provided administrative support and revised
the manuscript. SW, SL, TW, TL and JL were involved in the
collection and assembly of data, and performed the experiments.
Data analysis and interpretation was performed by HW, BL and SL. HW
and XN wrote the manuscript. HW and XN confirm the authenticity of
all the raw data. All authors read and approved the final version
of the manuscript.
Ethics approval and consent to
participate
This study complied with the Declaration of Helsinki
and was approved by Ethics Committees of The Fourth Hospital of
Hebei Medical University (approval no. 2022KY066).
Patient consent for publication
Written informed consent was obtained from all
participants in this study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yang Q, Lang C, Wu Z, Dai Y, He S, Guo W,
Huang S, Du H, Ren D and Peng X: MAZ promotes prostate cancer bone
metastasis through transcriptionally activating the KRas-dependent
RalGEFs pathway. J Exp Clin Cancer Res. 38:3912019. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhu Z, Wen Y, Xuan C, Chen Q, Xiang Q,
Wang J, Liu Y, Luo L, Zhao S, Deng Y and Zhao Z: Identifying the
key genes and microRNAs in prostate cancer bone metastasis by
bioinformatics analysis. FEBS Open Bio. 10:674–688. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hu ZD, Jiang Y, Sun HM, Wang JW, Zhai LL,
Yin ZQ and Yan J: KIF11 Promotes proliferation of hepatocellular
carcinoma among patients with liver cancers. Biomed Res Int.
2021:26767452021. View Article : Google Scholar
|
|
4
|
Peng P, Chen T, Wang Q, Zhang Y, Zheng F,
Huang S, Tang Y, Yang C, Ding W, Ren D, et al: Decreased miR-218-5p
levels as a serum biomarker in bone metastasis of prostate cancer.
Oncol Res Treat. 42:165–185. 2019. View Article : Google Scholar
|
|
5
|
Wang M, Xia F, Wei Y and Wei X: Molecular
mechanisms and clinical management of cancer bone metastasis. Bone
Res. 8:302020. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhang X: Interactions between cancer cells
and bone microenvironment promote bone metastasis in prostate
cancer. Cancer Commun (Lond). 39:762019. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sathianathen NJ, Koschel S, Thangasamy IA,
Teh J, Alghazo O, Butcher G, Howard H, Kapoor J, Lawrentschuk N,
Siva S, et al: Indirect comparisons of efficacy between combination
approaches in metastatic hormone-sensitive prostate cancer: A
systematic review and network meta-analysis. Eur Urol. 77:365–372.
2020. View Article : Google Scholar
|
|
8
|
Boevé L, Hulshof M, Vis AN, Zwinderman AH,
Twisk JWR, Witjes WPJ, Delaere KPJ, van Moorselaar RJA, Verhagen
PCMS and G van Andel: Effect on survival of androgen deprivation
therapy alone compared to androgen deprivation therapy combined
with concurrent radiation therapy to the prostate in patients with
primary bone metastatic prostate cancer in a prospective randomised
clinical trial: Data from the HORRAD trial. Eur Urol. 75:410–418.
2019. View Article : Google Scholar
|
|
9
|
Teo MY, Rathkopf DE and Kantoff P:
Treatment of advanced prostate cancer. Annu Rev Med. 70:479–499.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Reis LO: Metastasis-free survival-progress
or lowering the bar on nonmetastatic prostate cancer. Eur Urol.
74:682–683. 2018. View Article : Google Scholar
|
|
11
|
Kuzma M and Kliment J: Metastasis-free
survival as a new endpoint in castration-resistant prostate cancer.
Bratisl Lek Listy. 121:411–414. 2020.PubMed/NCBI
|
|
12
|
Xie W, Regan MM, Buyse M, Halabi S,
Kantoff PW, Sartor O, Soule H, Clarke NW, Collette L, Dignam JJ, et
al: Metastasis-free survival is a strong surrogate of overall
survival in localized prostate cancer. J Clin Oncol. 35:3097–3104.
2017. View Article : Google Scholar
|
|
13
|
Wang Y, Smallwood PM, Williams J and
Nathans J: A mouse model for kinesin family member 11
(Kif11)-associated familial exudative vitreoretinopathy. Hum Mol
Genet. 29:1121–1131. 2020. View Article : Google Scholar
|
|
14
|
Li TF, Zeng HJ, Shan Z, Ye RY, Cheang TY,
Zhang YJ, Lu SH, Zhang Q, Shao N and Lin Y: Overexpression of
kinesin superfamily members as prognostic biomarkers of breast
cancer. Cancer Cell Int. 20:1232020. View Article : Google Scholar
|
|
15
|
Daigo K, Takano A, Thang PM, Yoshitake Y,
Shinohara M, Tohnai I, Murakami Y, Maegawa J and Daigo Y:
Characterization of KIF11 as a novel prognostic biomarker and
therapeutic target for oral cancer. Int J Oncol. 52:155–165.
2018.
|
|
16
|
Piao XM, Byun YJ, Jeong P, Ha YS, Yoo ES,
Yun SJ and Kim WJ: Kinesin family member 11 mRNA expression
predicts prostate cancer aggressiveness. Clin Genitourin Cancer.
15:450–454. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Apte RS, Chen DS and Ferrara N: VEGF in
signaling and disease: Beyond discovery and development. Cell.
176:1248–1264. 2019. View Article : Google Scholar
|
|
18
|
Murukesh N, Dive C and Jayson GC:
Biomarkers of angiogenesis and their role in the development of
VEGF inhibitors. Br J Cancer. 102:8–18. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Garcia J, Hurwitz HI, Sandler AB, Miles D,
Coleman RL, Deurloo R and Chinot OL: Bevacizumab
(Avastin®) in cancer treatment: A review of 15 years of
clinical experience and future outlook. Cancer Treat Rev.
86:1020172020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Melegh Z and Oltean S: Targeting
angiogenesis in prostate cancer. Int J Mol Sci. 20:26762019.
View Article : Google Scholar
|
|
21
|
Cai C, Wang H, He HH, Chen S, He L, Ma F,
Mucci L, Wang Q, Fiore C, Sowalsky AG, et al: ERG induces androgen
receptor-mediated regulation of SOX9 in prostate cancer. J Clin
Invest. 123:1109–1122. 2013. View
Article : Google Scholar
|
|
22
|
Roudier MP, Winters BR, Coleman I, Lam HM,
Zhang X, Coleman R, Chéry L, True LD, Higano CS, Montgomery B, et
al: Characterizing the molecular features of ERG-positive tumors in
primary and castration resistant prostate cancer. Prostate.
76:810–822. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kumar A, Coleman I, Morrissey C, Zhang X,
True LD, Gulati R, Etzioni R, Bolouri H, Montgomery B, White T, et
al: Substantial interindividual and limited intraindividual genomic
diversity among tumors from men with metastatic prostate cancer.
Nat Med. 22:369–378. 2016. View
Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lee H, Lee M, Byun SS, Lee SE and Hong SK:
Evaluation of prostate cancer stage groups updated in the 8th
edition of the American joint committee on cancer
tumor-node-metastasis staging manual. Clin Genitourin Cancer.
17:e221–e226. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Epstein JI, Egevad L, Amin MB, Delahunt B,
Srigley JR and Humphrey PA; Grading Committee, : The 2014
international society of urological pathology (ISUP) consensus
conference on gleason grading of prostatic carcinoma: Definition of
grading patterns and proposal for a new grading system. Am J Surg
Pathol. 40:244–252. 2016. View Article : Google Scholar
|
|
26
|
Berish RB, Ali AN, Telmer PG, Ronald JA
and Leong HS: Translational models of prostate cancer bone
metastasis. Nat Rev Urol. 15:403–421. 2018. View Article : Google Scholar
|
|
27
|
Fizazi K, Shore N, Tammela TL, Ulys A,
Vjaters E, Polyakov S, Jievaltas M, Luz M, Alekseev B, Kuss I, et
al: Nonmetastatic, castration-resistant prostate cancer and
survival with darolutamide. N Engl J Med. 383:1040–1049. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Talapatra SK, Anthony NG, Mackay SP and
Kozielski F: Mitotic kinesin Eg5 overcomes inhibition to the phase
I/II clinical candidate SB743921 by an allosteric resistance
mechanism. J Med Chem. 56:6317–6329. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Even-Ram S, Doyle AD, Conti MA, Matsumoto
K, Adelstein RS and Yamada KM: Myosin IIA regulates cell motility
and actomyosin-microtubule crosstalk. Nat Cell Biol. 9:299–309.
2007. View
Article : Google Scholar
|
|
30
|
Venere M, Horbinski C, Crish JF, Jin X,
Vasanji A, Major J, Burrows AC, Chang C, Prokop J, Wu Q, et al: The
mitotic kinesin KIF11 is a driver of invasion, proliferation, and
self-renewal in glioblastoma. Sci Transl Med. 7:304ra1432015.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Nomiri S, Karami H, Baradaran B,
Javadrashid D, Derakhshani A, Nourbakhsh NS, Shadbad MA, Solimando
AG, Tabrizi NJ, Brunetti O, et al: Exploiting systems biology to
investigate the gene modules and drugs in ovarian cancer: A
hypothesis based on the weighted gene co-expression network
analysis. Biomed Pharmacother. 146:1125372022. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Carmeliet P and Jain RK: Molecular
mechanisms and clinical applications of angiogenesis. Nature.
473:298–307. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ferrara N: VEGF as a therapeutic target in
cancer. Oncology. 69 (Suppl 3):S11–S16. 2005. View Article : Google Scholar
|
|
34
|
Zhao Y, Cai C, Zhang M, Shi L, Wang J,
Zhang H, Ma P and Li S: Ephrin-A2 promotes prostate cancer
metastasis by enhancing angiogenesis and promoting EMT. J Cancer
Res Clin Oncol. 147:2013–2023. 2021. View Article : Google Scholar
|
|
35
|
Bono AV, Celato N, Cova V, Salvadore M,
Chinetti S and Novario R: Microvessel density in prostate
carcinoma. Prostate Cancer Prostatic Dis. 5:123–127. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ioannidou E, Moschetta M, Shah S, Parker
JS, Ozturk MA, Pappas-Gogos G, Sheriff M, Rassy E and Boussios S:
Angiogenesis and anti-angiogenic treatment in prostate cancer:
Mechanisms of action and molecular targets. Int J Mol Sci.
22:99262021. View Article : Google Scholar
|
|
37
|
Tarantino G, Crocetto F, Vito CD, Martino
R, Pandolfo SD, Creta M, Aveta A, Buonerba C and Imbimbo C:
Clinical factors affecting prostate-specific antigen levels in
prostate cancer patients undergoing radical prostatectomy: A
retrospective study. Future Sci OA. 7:FSO6432021. View Article : Google Scholar : PubMed/NCBI
|