Introduction
Thyroid cancer and lung cancer are two of the most
common malignancies worldwide. The incidence rate of thyroid cancer
is 3.2 cases per 100,000 individuals globally, and the mortality
rate is 0.5 cases per 100,000 individuals (1). With regard to lung cancer, the
incidence and mortality rates are 22.5 cases per 100,000
individuals and 18.6 cases per 100,000 individuals, respectively
(2). However, the incidence of
multiple primary cancers of the thyroid and lung has rarely been
reported in the literature. Tumor invasion of the larynx or trachea
is observed in ~6% of differentiated thyroid cancer cases (3) and increases the mortality rate.
Surgery is the benchmark for treatment (4). Lung adenocarcinoma is the most
dominant subtype of lung cancer (5). Surgical resection is the first step of
standard treatment procedures for early stage lung cancer. However,
simultaneous surgery for papillary thyroid cancer (PTC) with
tracheal invasion and lung cancer is a great challenge for the
patient and the surgeon. The present study reports a rare case with
PTC involving the trachea and primary lung cancer that was
successfully treated simultaneously by one-stage surgery on two
organs.
Case report
Patient
A 64-year-old female patient with hemoptysis that
had persisted for 1 year was admitted to Ningbo No. 2 Hospital
(Ningbo, China) in April 2019. The patient had no smoking history
or any other underlying diseases, except for hypertension. A
physical examination showed a 3-cm fixed nodule in the right
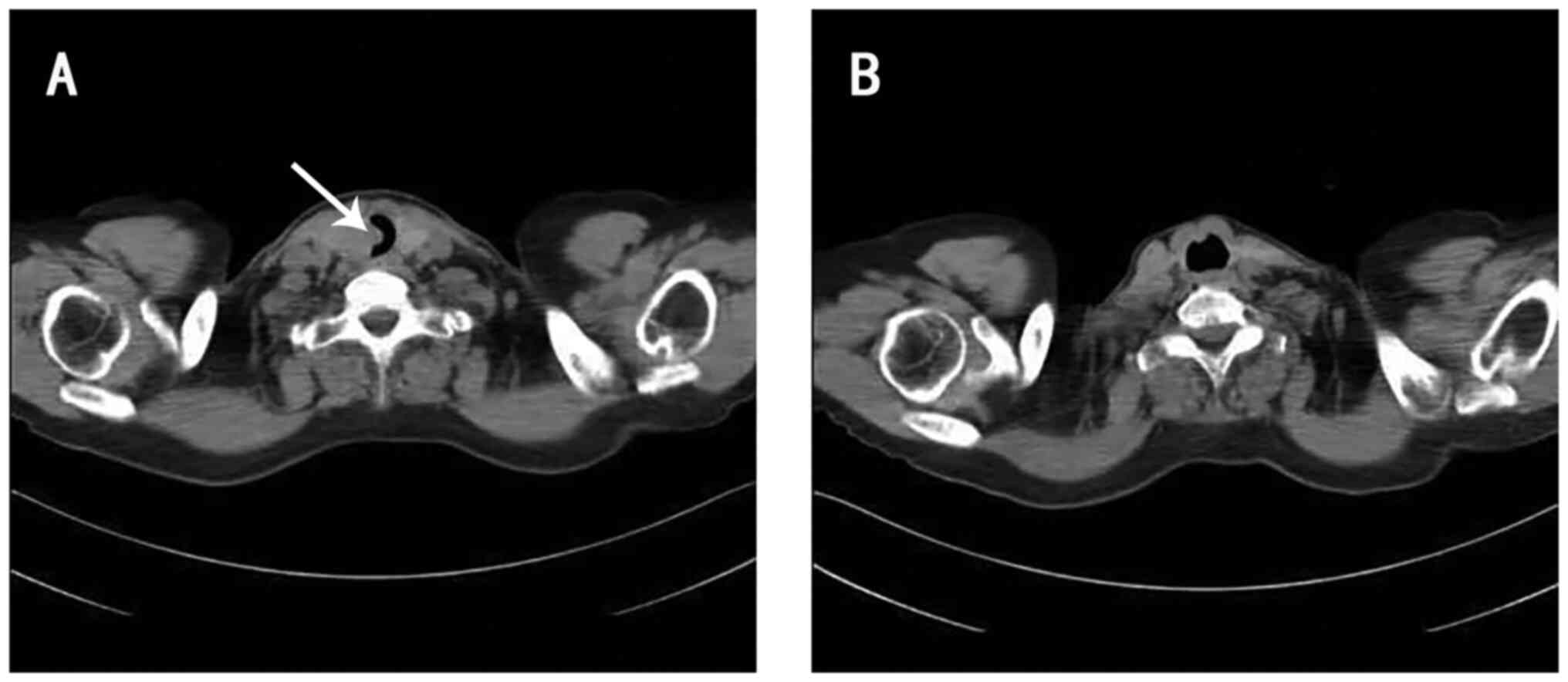
thyroid lobe. Ultrasound and contrast-enhanced computed tomography
(CT) of the neck indicated a suspected thyroid carcinoma in the
right lobe with tracheal invasion (Fig.
1A) and right lateral cervical lymph node (LN) metastasis.
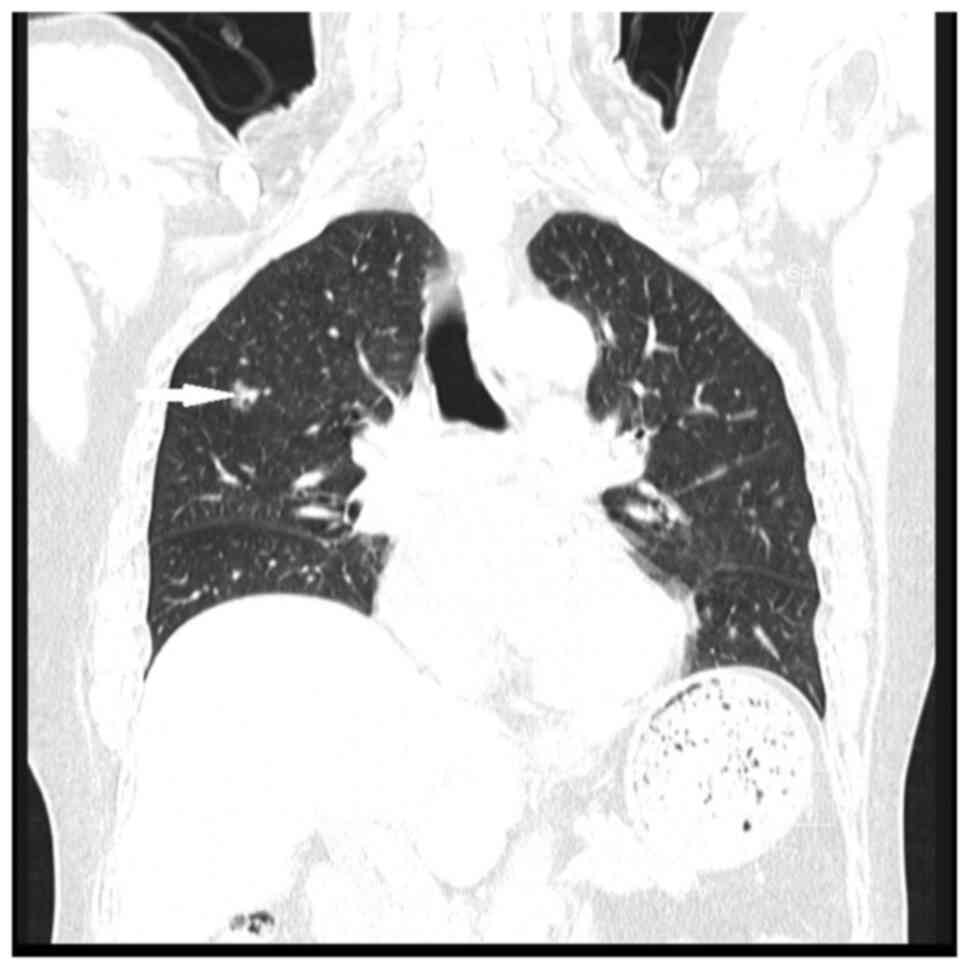
Chest CT revealed a ground-glass nodule in the anterior segment of
the upper lobe of the right lung, which was also highly suspected
to be a malignancy (Fig. 2).
Preoperative tracheoscopy showed an endotracheal
neoplasm, which occupied 90% of the lumen. The patient received
tumor electrocautery under tracheoscopy and the luminal stenosis
was reduced to ~15%, leaving sufficient space for tracheal
intubation. Pathological examination and immunohistochemistry
confirmed that the endotracheal neoplasm originated from PTC. The
immunohistochemistry results were as follows: Pan-cytokeratin
(CK)(+), CK7(+), CK19(+), thyroid transcription factor 1(+),
NapsinA(−), mesothelial cell marker-human bone marrow endothelial
cell marker [MC(HBME-1)](+), paired-box protein pax-8(+) and
Ki-67(10%+).
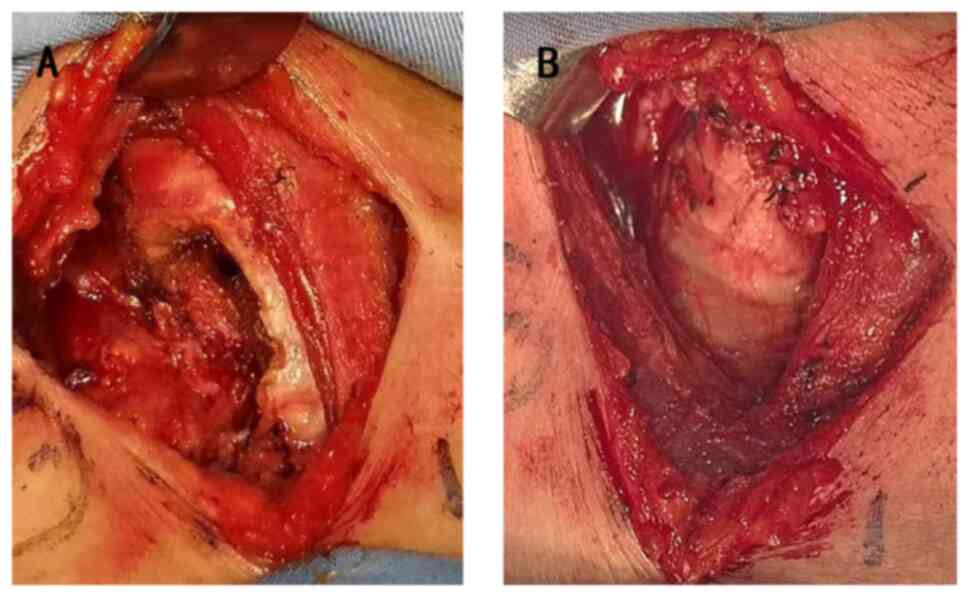
The patient successfully received a thoracoscopic
radical resection of the right upper lung cancer, a radical
thyroidectomy and a window tracheal resection. The tumor had
invaded 3×2.5 cm into the trachea. The bilateral thyroid gland and
3.5×3 cm of the trachea were removed simultaneously (Fig. 3A). 0# silk sutures were used to seam
the tracheal gap (Fig. 3B). Next,
the level II–V LNs of the right lateral neck and the bilateral
level VI LNs were dissected.
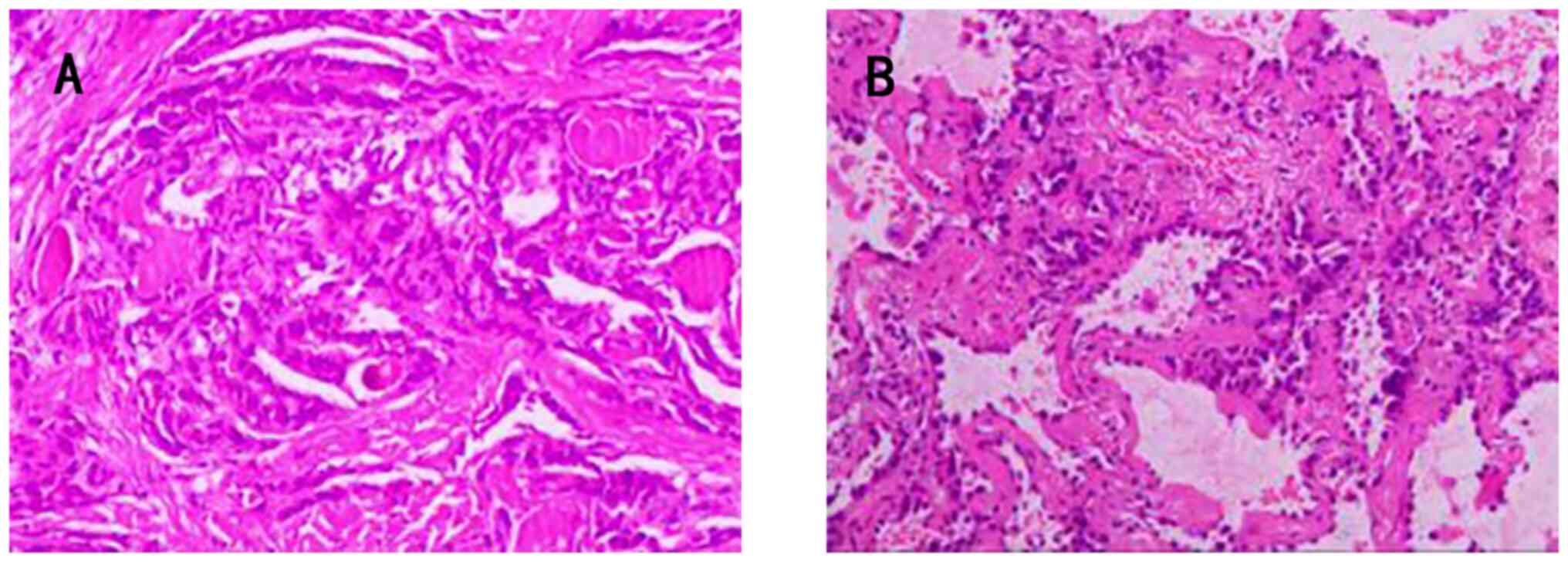
The postoperative pathological examination (Fig. 4) revealed a 1.2-cm microinvasive
adenocarcinoma of the right upper lung (H&E staining;
magnification, ×100), without lymphatic metastasis (T1bN0M0), stage
Ia, according to the eighth edition of the Tumor-Node-Metastasis
Classification of Lung Cancer (6).
The tumor showed a predominately lepidic growth pattern, with a
central focus of invasion measuring ≤5 mm that was associated with
a scar. The thyroid tumor was confirmed as a right papillary
thyroid carcinoma (H&E staining; magnification, ×100), with
tracheal invasion plus right level II–VI LN metastasis (11 positive
nodes/28 total nodes) and left level VI LN metastasis (1 positive
node/5 total nodes) (T4aN1bM0). The tumor showed a complex
papillary architecture, intranuclear inclusions and mitotic
activity. Genetic testing of the PTC was negative, without ret
proto-oncogene mutation or fusion. The patient did not receive
genetic testing of the lung cancer, as the postoperative
pathological examination only revealed a 1.2-cm microinvasive
adenocarcinoma without lymphatic metastasis; this could be
classified as early stage lung cancer with a very good prognosis.
Targeted therapy or immunotherapy was therefore not required.
After the surgery, the patient was sent to the
intensive care unit and was extubated 7 days later. The patient
received thyroid-stimulating hormone inhibitory therapy
(levothyroxine sodium, 100 µg/day) and iodine-131 (131I)
treatment postoperatively (3.70 GBq). Bimonthly follow-up was
conducted for 14 months, with no evidence of recurrence observed on
CT (Fig. 1B) (Table I).
 | Table I.Basic information on the papillary
thyroid cancer and lung cancer. |
Table I.
Basic information on the papillary
thyroid cancer and lung cancer.
| Parameter | Thyroid cancer | Lung cancer |
|---|
| Diameter, cm | 3.0 | 1.2 |
| Pathological
type | Papillary thyroid
carcinoma | Microinvasive
adenocarcinoma |
| Local invasion | Tracheal
invasion | No |
| Lymphatic
metastasis | Yes | No |
| Distant
metastasis | No | No |
| TNM stage | T4aN1bM0 | T1bN0M0 |
| Genetic testing | Negative | Not available |
| Recurrence | No | No |
Methods
Hematoxylin and eosin of thyroid and
lung specimens
Specimens were fixed with a fixation solution
containing 10% formalin at room temperature for 24 h, prior to
being embedded in paraffin, cut into 4-µm sections and stained for
5 min at room temperature with hematoxylin and eosin. The tissues
were observed with a light microscope (Nikon Corporation) at ×100
magnification.
Immunohistochemical staining of the
thyroid tumor
The tissue was fixed with 10% formalin at room
temperature for 24 h, cut into 2- to 3-mm sections and embedded in
paraffin. Paraffin-embedded tissues were cut into 4-µm sections and
sealed with 3% hydrogen peroxide at room temperature for 10 min.
Antigen retrieval was performed with EDTA at 100°C for 2.5 min,
followed by washing with PBS. Primary antibody incubation was
performed at 37°C for 60 min and secondary antibody incubation at
37°C for 20 min. The primary antibodies were purchased ready to use
from OriGene Technologies, Inc. The following primary antibodies
were used: Pan-CK (1:1,000; cat. no. ZM-0069), CK7 (1:1,000; cat.
no. ZA-0573), CK19 (1:1,000; cat. no. ZA-0670), thyroid
transcription factor 1 (1:1,000; cat. no. ZM-0270), NapsinA
(1:1,000; cat. no. ZM-0473), MC(HBME1) (1:1,000; cat. no. ZM-0386),
paired-box protein pax-8 (1:1,000; cat. no. ZA-0666) and Ki-67
(1:1,000; cat. no. ZM-0166). Secondary antibodies were obtained
from Fuzhou Maixin Biotech. Co., Ltd. Goat anti-mouse IgG polymer
III (1:200; cat. no. 220426S935c) was used as the secondary
antibody. The results were observed using a light microscope (Nikon
Corporation) at ×100 magnification.
Discussion
In general, patients with PTC have a good prognosis
and the 10-year survival rate can reach 90% (7). Extrathyroidal spread is an important
determinant of outcome, and deep tracheal invasion and infiltration
are correlated with a poorer prognosis (8,9).
Surgical resection is the first step of standard treatment
procedures for early stage lung cancer. A one-stage operation for
lung cancer and thyroid cancer with tracheal invasion and lateral
cervical lymph node metastasis is a great challenge that needs
rigorous preoperative evaluation, multidisciplinary collaboration
and good postoperative care. These points mean that the patient
should not have severe disease, which would affect the surgery and
anesthesia. The thyroid surgeon and the thoracic surgeon should
make efforts in the two procedures to shorten the operation time.
After the operation, care is needed in case of difficult
decannulation, anastomotic infection, pulmonary infection or
phlebothrombosis, among others.
Most patients with superficial invasion of the
trachea are asymptomatic. Symptoms will appear when they experience
intraluminal invasion. Common symptoms include hemoptysis, stridor,
dyspnea and airway hemorrhage (10). When the tumor involves the recurrent
laryngeal nerve, hoarseness is also inevitable.
The tracheoscopic examination should be performed in
patients with PTC and tracheal invasion. It is of great importance
to measure the extent of tracheal invasion. Meanwhile, the
anesthetist should evaluate whether the tumor will affect tracheal
intubation. In the present case, the tumor occupied 90% of the
tracheal lumen with no space for intubation. Tracheoscopic tumor
electrocautery was a prerequisite for the subsequent treatment.
Survival rate will be increased in patients with
thyroid cancer who undergo airway-resection (11,12).
Shave excision of the affected tissue, window tracheal resection
and sleeve tracheal resection are the main surgical management
techniques for tracheal invasion. Shave excision is only applied in
patients with superficial tracheal invasion. Once the tracheal
cartilage is transgressed, patients require window tracheal
resection and sleeve tracheal resection. It has been reported in
the literature that for patients with involvement of less than four
tracheal rings and endotracheal involvement of <50% of the
tracheal rings, a window resection of the trachea can be adopted.
Sleeve tracheal resection is used in cases that have significant
cricotracheal infiltration, for those cases with thyroid carcinoma
invading >50% of the tracheal rings and for those with tracheal
involvement of 4–6 cartilage rings (13). In the present case, although the
tumor occupied 90% of the lumen, endotracheal involvement was
<50% of the tracheal rings. Thus, a window tracheal resection
was adopted. Considering that the incision into the trachea was
limited, the tracheal gap was seamed closed with 0# silk sutures.
However, for larger defects, closure should be performed using a
myofascial flap or by forming a temporary tracheotomy through the
defect with a delayed closure time (14).
The role of 131I treatment has not been
separately investigated in tracheal invasion. One study indicated
that it may have limited effectiveness, as tumors invading the
airway are less differentiated and may take up less of the
radioactive iodine, therefore making them resistant to the therapy
(15). However, adjuvant
131I therapy is commonly applied in advanced
differentiated thyroid carcinoma for the reason that postoperative
131I therapy can reduce the risk of recurrence and
improve the survival rate (16).
Surgical resection is the most effective therapy for
stages I to II and selected cases of stage IIIA non-small-cell lung
cancer (NSCLC) (17). The benefit
of adjuvant cytotoxic therapy with a cisplatin-based doublet has
been shown in patients with completely resected stage II and IIIA
NSCLC (18). Targeted agents, such
as erlotinib, gefitinib, afatinib and crizotinib, have been
demonstrated to decrease the tumor burden and symptoms, and
markedly improve the quality of life for patients with specific
genetic alterations (19). The
introduction of immune-checkpoint blockers such as monoclonal
antibodies that target cytotoxic T-lymphocyte antigen-4 (CTLA-4)
and antibodies against programmed cell death protein 1 (PD-1) or
programmed cell death ligand 1 (PD-L1) has signaled a new direction
for lung cancer care (20). The
case discussed in the present study was stage Ia, so the prognosis
is good and no treatment is needed temporarily.
In conclusion, simultaneous surgery of PTC with
tracheal invasion and lung cancer is a great challenge for both the
patient and surgeon. Appropriate surgical management of tracheal
invasion is of great importance to the operation and prognosis.
Acknowledgements
Not applicable.
Funding
This study received funds from the Natural Science Foundation of
Ningbo (grant no. 2021J313) and Ningbo Leading Medical & Health
Discipline (grant no. 2022-F18) to cover publication costs.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
WZ, LD, KY, YW and QL made substantial contributions
to the study conception and design, the acquisition/analysis of
data and the writing of the manuscript. XW performed the operation,
revised the manuscript and provided general supervision. WZ, LD,
KY, YW, QL and XW confirm the authenticity of all the raw data. All
authors contributed to the review of the manuscript and have read
and approved the final manuscript.
Ethics approval and consent to
participate
The research was conducted ethically in conformity
with the World Medical Association Declaration of Helsinki. Ethical
approval for this case report was waived as the patient provided
consent and the report contains nothing that may be considered a
risk to patient privacy and integrity.
Patient consent for publication
The patient provided written informed consent for
the publication of this report and any accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Deng Y, Li H, Wang M, Li N, Tian T, Wu Y,
Xu P, Yang S, Zhai Z, Zhou L, et al: Global burden of thyroid
cancer from 1990 to 2017. JAMA Netw Open. 3:e2087592020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sun X, Xu X, Wang Y, Hou B, Luo T, Meng D,
Wang S and Ning F: Incidence and mortality rates of lung cancer in
Qingdao, China (2013–2017). Asia Pac J Clin Oncol. 18:e73–e78.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Czaja JM and McCaffrey TV: The surgical
management of laryngotracheal invasion by well-differentiated
papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg.
123:484–490. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lin S, Huang H, Liu X, Li Q, Yang A, Zhang
Q, Guo Z and Chen Y: Treatments for complications of tracheal
sleeve resection for papillary thyroid carcinoma with tracheal
invasion. Eur J Surg Oncol. 40:176–181. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Detterbeck FC, Chansky K, Groome P,
Bolejack V, Crowley J, Shemanski L, Kennedy C, Krasnik M, Peake M,
Rami-Porta R, et al: The IASLC lung cancer staging project:
Methodology and Validation used in the development of proposals for
revision of the stage classification of NSCLC in the Forthcoming
(Eighth) Edition of the TNM Classification of Lung Cancer. J Thorac
Oncol. 11:1433–1446. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Carhill AA, Litofsky DR, Ross DS, Jonklaas
J, Cooper DS, Brierley JD, Ladenson PW, Ain KB, Fein HG, Haugen BR,
et al: Long-Term outcomes following therapy in differentiated
thyroid carcinoma: NTCTCS Registry Analysis 1987–2012. J Clin
Endocrinol Metab. 100:3270–3279. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nishida T, Nakao K and Hamaji M:
Differentiated thyroid carcinoma with airway invasion: Indication
for tracheal resection based on the extent of cancer invasion. J
Thorac Cardiovasc Surg. 114:84–92. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wada N, Nakayama H, Masudo Y, Suganuma N
and Rino Y: Clinical outcome of different modes of resection in
papillary thyroid carcinomas with laryngotracheal invasion.
Langenbecks Arch Surg. 391:545–549. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Moritani S: Surgical management of
cricotracheal invasion by papillary thyroid carcinoma. Ann Surg
Oncol. 22:4002–4007. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shadmehr MB, Farzanegan R, Zangi M,
Mohammadzadeh A, Sheikhy K, Pejhan S, Daneshvar A and
Abbasidezfouli A: Thyroid cancers with laryngotracheal invasion.
Eur J Cardiothorac Surg. 41:635–640. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gaissert HA, Honings J, Grillo HC, Donahue
DM, Wain JC, Wright CD and Mathisen DJ: Segmental laryngotracheal
and tracheal resection for invasive thyroid carcinoma. Ann Thorac
Surg. 83:1952–1959. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang J, Fu C, Cui K and Ma X: Papillary
thyroid carcinoma with tracheal invasion: A case report. Medicine
(Baltimore). 98:e170332019. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ebihara M, Kishimoto S, Hayashi R,
Miyazaki M, Shinozaki T, Daiko H, Saikawa M, Sakuraba M and
Miyamoto S: Window resection of the trachea and secondary
reconstruction for invasion by differentiated thyroid carcinoma.
Auris Nasus Larynx. 38:271–275. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Honings J, Stephen AE, Marres HA and
Gaissert HA: The management of thyroid carcinoma invading the
larynx or trachea. Laryngoscope. 120:682–689. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yang Z, Flores J, Katz S, Nathan CA and
Mehta V: Comparison of survival outcomes following postsurgical
radioactive iodine versus external beam radiation in stage IV
differentiated thyroid carcinoma. Thyroid. 27:944–952. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hirsch FR, Scagliotti GV, Mulshine JL,
Kwon R, Curran WJ Jr, Wu YL and Paz-Ares L: Lung cancer: Current
therapies and new targeted treatments. Lancet. 389:299–311. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kris MG, Gaspar LE, Chaft JE, Kennedy EB,
Azzoli CG, Ellis PM, Lin SH, Pass HI, Seth R, Shepherd FA, et al:
Adjuvant systemic therapy and adjuvant radiation therapy for stage
I to IIIA completely resected non-small-cell lung cancers: American
Society of clinical oncology/cancer care ontario clinical practice
guideline update. J Clin Oncol. 35:2960–2974. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Masters GA, Temin S, Azzoli CG, Giaccone
G, Baker S Jr, Brahmer JR, Ellis PM, Gajra A, Rackear N, Schiller
JH, et al: Systemic therapy for stage IV nonsmall-cell lung cancer:
American society of clinical oncology clinical practice guideline
update. J Clin Oncol. 33:3488–3515. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Garon EB, Rizvi NA, Hui R, Leighl N,
Balmanoukian AS, Eder JP, Patnaik A, Aggarwal C, Gubens M, Horn L,
et al: Pembrolizumab for the treatment of non-small-cell lung
cancer. N Engl J Med. 372:2018–2028. 2015. View Article : Google Scholar : PubMed/NCBI
|