Introduction
Liposarcoma is one of the most common types of
retroperitoneal primary tumors, accounting for 10–35% of all soft
tissue sarcoma (1). Retroperitoneal
liposarcoma (RPLS) occurs mostly between the ages of 40 and 60
years, with a slight male predominance (2). Pathologically, liposarcoma is divided
into five types (3):
Well-differentiated liposarcoma (WDLPS), dedifferentiated
liposarcoma (DDLPS), myxoid liposarcoma (MLS), pleomorphic
liposarcoma and myxoid pleomorphic liposarcoma. WDLPS is a typical
indolent malignancy but can be locally aggressive, while DDLPS has
a higher grade histology, faster growth and distant metastatic
potential (4). MLS is the second
most common subtype, accounting for ~5% of all soft tissue sarcomas
in adults (5). Histological lesions
show low grade forms and poorly differentiated round cells. At a
molecular level, translocation (12;16) (q13;p11), resulting in
fused in sarcoma and DNA damage inducible transcript 3 (FUS-DDIT3)
gene fusion, has been described in the majority of these tumors
(6). The treatment is generally
surgical excision with or without radiation therapy. In case of
high-risk disease and positive surgical margins, chemotherapy is
considered (7). Pleomorphic
liposarcoma is rare and represents only 5–10% of liposarcoma
(8). However, it is considered to
be of the highest malignancy grade, with high invasion, metastasis
and recurrence. Radiotherapy only benefits patients with large
tumor size (>10 cm); however, surgery, particularly radical
resection, is the primary treatment option (9). Surgical resection is the first choice
of treatment (10). However, as
RPLS is a large tumor, the boundary is difficult to determine and
relapse is common following surgery (11,12).
Abdominal computed tomography (CT) scan is key for the diagnosis,
staging and follow-up of the disease (13).
Case report
A 40-year-old woman was hospitalized at Shaoxing
Second Hospital (Shaoxing, China) in April 2009 due to the
discovery of a retroperitoneal mass 1 week prior. The patient had
complained of a retroperitoneal mass and abdominal pain for 1 week.
CT examination of the abdomen confirmed a mass in the
retroperitoneal space (~11×15 cm). On April 15, 2009, the patient
underwent the resection of the right retroperitoneal mass and right
nephrectomy due to the large space occupied by the right
retroperitoneal mass. The pathological findings revealed one
gray-red and gray-yellow mass (30×19×10 cm) with a capsule on the
surface and a clear boundary with the surrounding area and one
kidney in the center of the mass (10.5×5.5×3.5 cm), which was
difficult to separate from the mass. No tumor tissue invasion was
found in the kidney. The incisal margin was negative. The
pathological diagnosis indicated retroperitoneal MLS with right
kidney involvement. The results of immunohistochemical analysis
were as follows: S-100 protein (+), p53 (−), myogenin (−), Ki67
(2%), SMA (−), CD68 (−), β-catenin (−) and CD34 (vascular +). The
grade and stage of the disease was T4N0M0, G1, IB (14). No post-operative chemotherapy was
performed due to complete surgical resection.
Since the pathological diagnosis of the patient was
MLS, which is not sensitive to radiotherapy (15), no radiotherapy was administered. The
patient did not receive any other treatment following surgery and
was followed-up regularly until June 2014, when local recurrence of
the tumor was found. The patient relapsed multiple times. RPLS
resection was performed using open surgery on June 3, 2014, January
12, 2017, December 25, 2018 and July 21, 2020. The post-operative
pathological diagnosis in all cases was MLS liposarcoma. In June
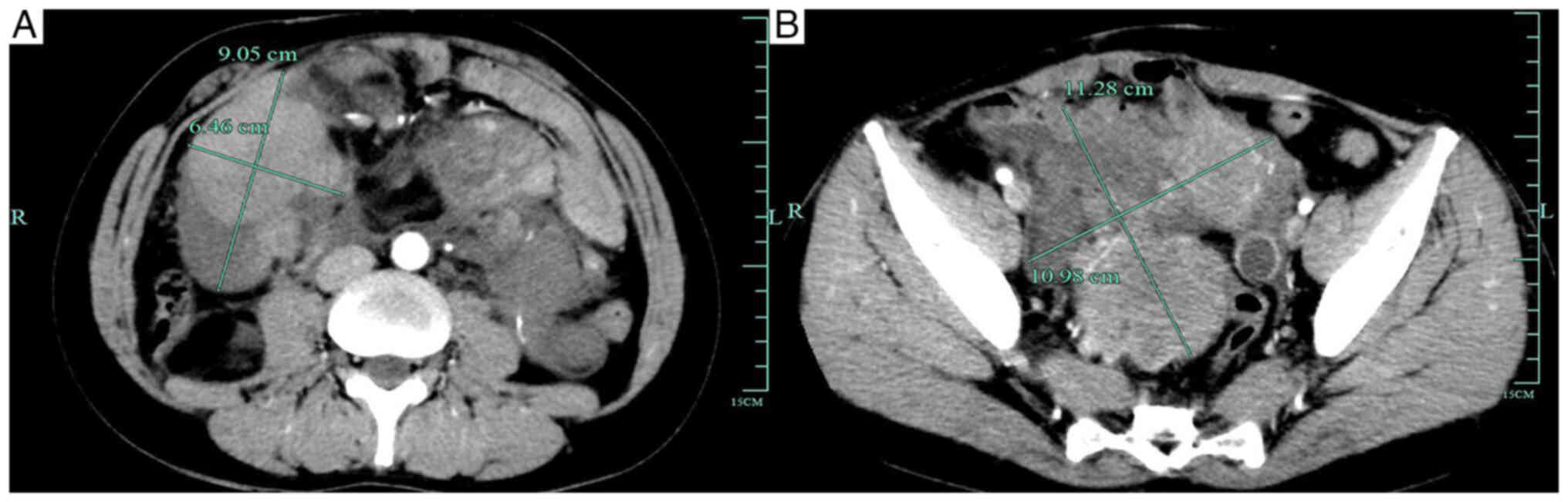
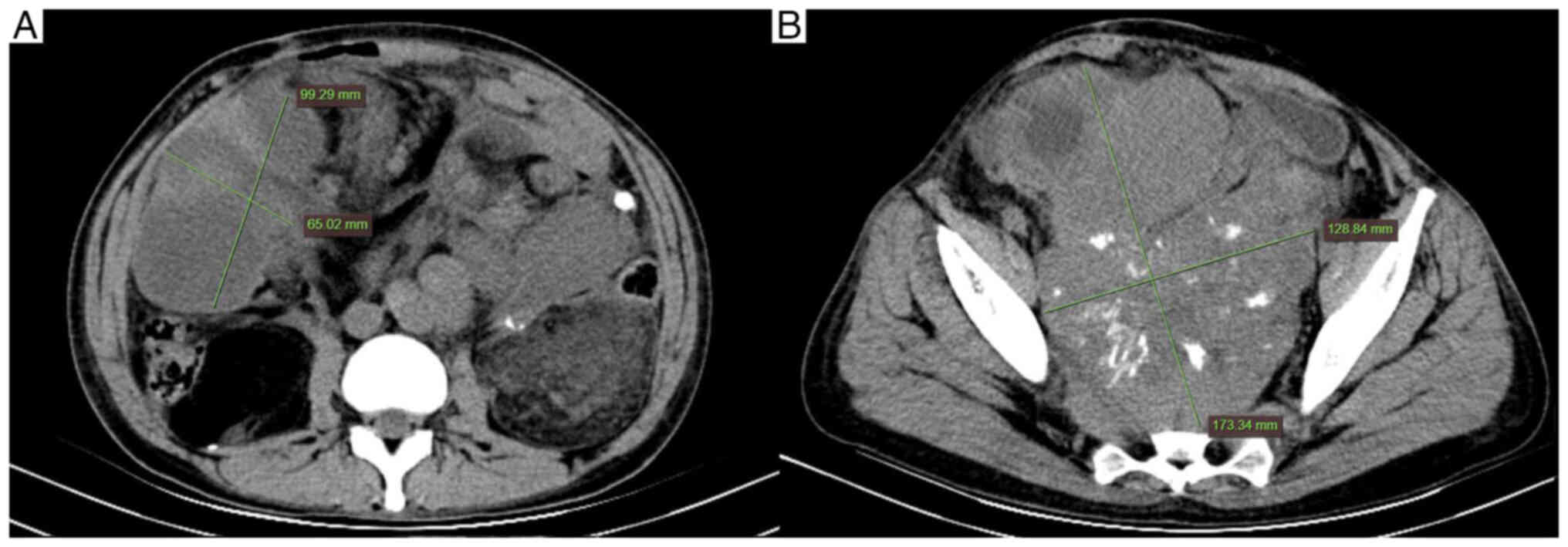
2021, abdominal enhanced CT scan revealed post-operative changes in
the right kidney and recurrence of multiple liposarcoma in the
abdominal, pelvic and retroperitoneal areas (Fig. 1). On June 22, 2021,
endoscopic-assisted resection of retroperitoneal tumor and
intestinal adhesion release were performed due to adhesion between
the tumor and surrounding tissue. More than 10 tumors were
surgically removed. The post-operative pathological analysis
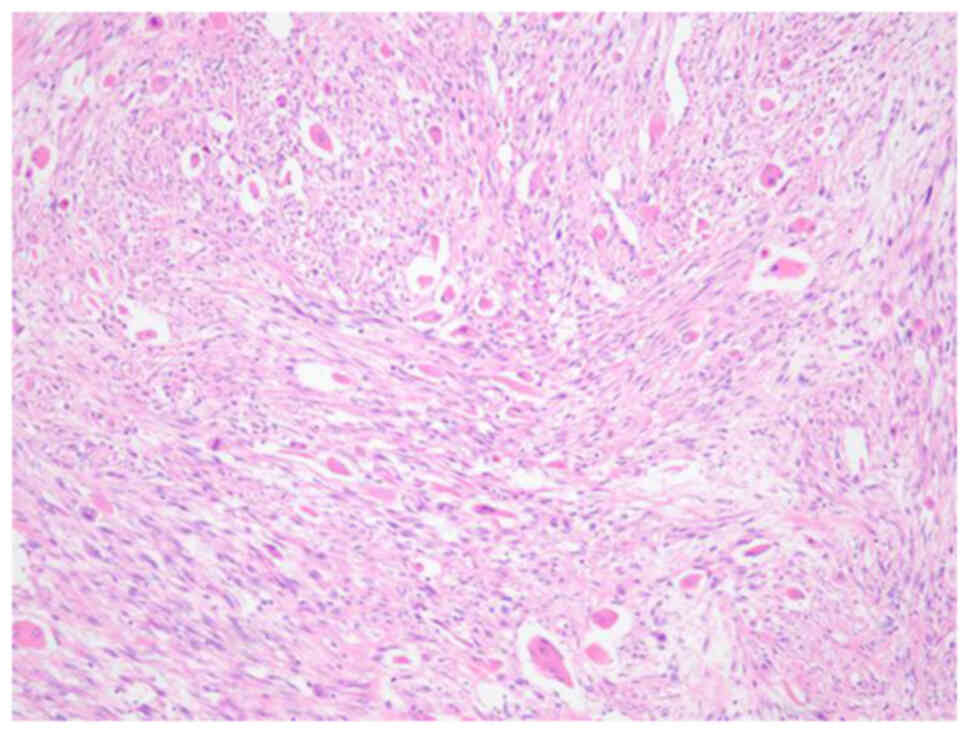
revealed spindle cell soft tissue sarcoma (pelvic and peritoneal
tumors), consistent with multiple types of liposarcoma (DDLPS, MLS
and WDLPS; total size, 27.0×13.5×6.0 cm; Fig. 2). The results of immunohistochemical
analysis were as follows: Creatine kinase (−), succinate
dehydrogenase complex iron sulfur subunit B (+), Ki67 (30%), S-100
(small amount +), desmin (+), CD34 (vascular +), SMA (−), HMB45
(−), β-Catenin (membrane +), anaplastic lymphoma kinase (ALK) (−),
BCL6 co-repressor (−), mouse double minute 2
homolog(MDM2)/chromosome 12 centromere FISH (+) and MDM2 (+). In
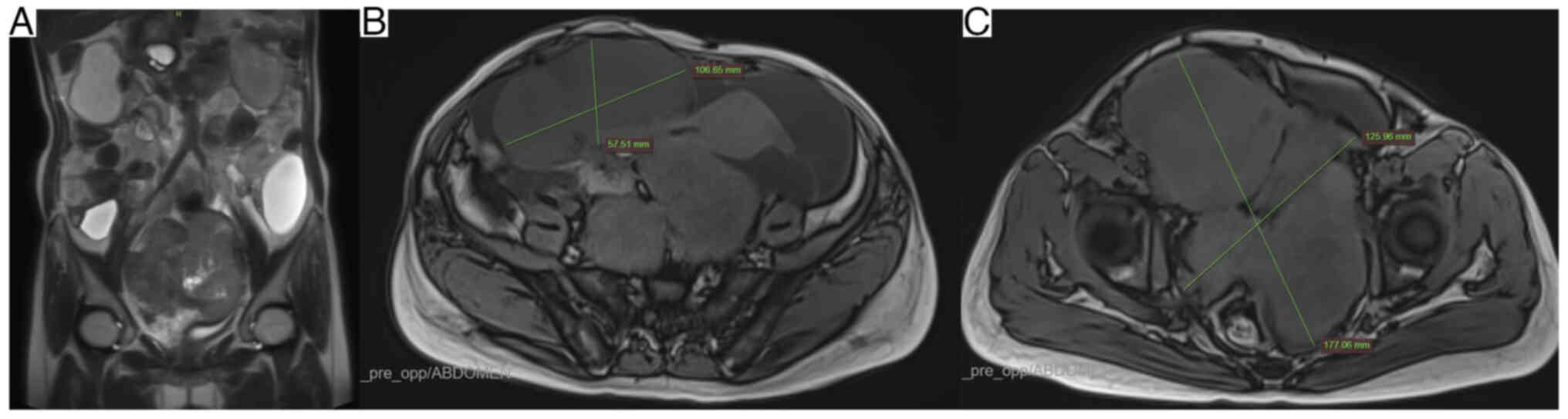
November 2021, the patient underwent re-examination by abdominal
magnetic resonance imaging (MRI; Fig.
3); the mass in the abdominal and pelvic cavities had
increased. Due to progression of the disease, the patient underwent
six cycles of doxorubicin and ifosfamide chemotherapy (day 1, 70 mg
doxorubicin; day 1–3, 2 g ifosfamide 2 g) and anlotinib (12 mg)
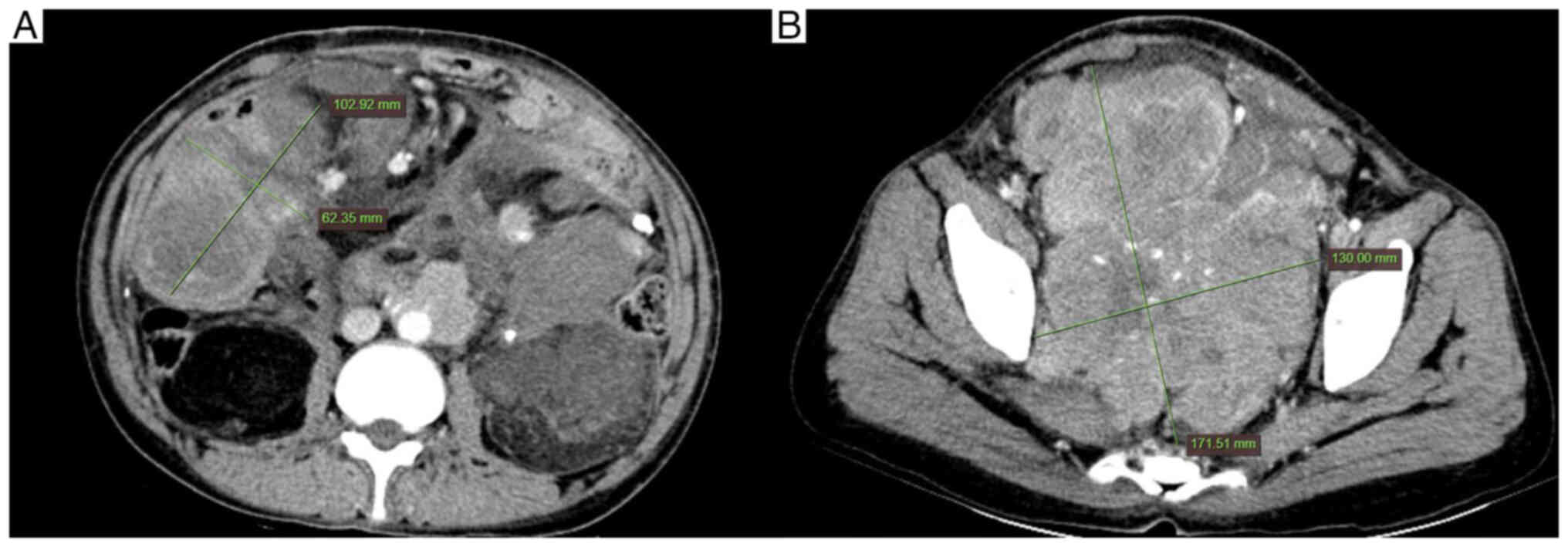
oral targeted therapy once a day. In May 2022, the whole abdominal
enhanced CT scan was performed and it was found that the mass in
the abdominal and pelvic cavities had decreased (Fig. 4). In July 2022, the whole abdominal
CT scan was repeated; the mass had no obvious change compared with
the previous mass (Fig. 5) and
there was no evidence of disease progression. The evaluation of the
chemotherapeutic efficacy was stable disease, as per the Response
Evaluation Criteria In Solid Tumors criteria (16). Since the fifth recurrence in June
2021 of liposarcoma, >1 year survival has been achieved. The
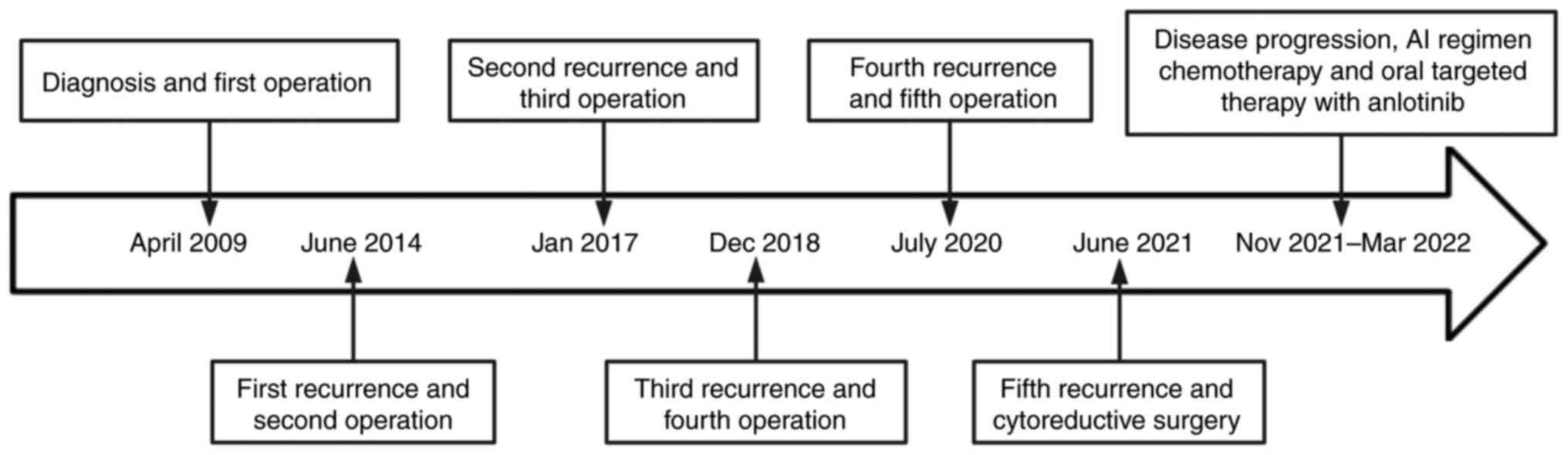
timeline of the case is presented in Fig. 6.
Discussion
RPLS is usually discovered relatively late; as the
retroperitoneal space is large, there are no obvious symptoms in
the early stages of the disease. It often presents as a painless
mass that grows at a slow rate. As tumor increases in size, it
compresses adjacent organs and causes discomfort. Abdominal pain is
the main clinical manifestation, followed by abdominal swelling
(17). As symptoms do not appear
until the late stage of disease progression, patients often have
large tumors when they visit the hospital. The present patient had
no obvious signs at the initial diagnosis, although the abdominal
mass was palpable.
RPLS lacks specific clinical symptoms, thus, it is
very important to detect it through imaging examination. CT scan is
the first choice for the examination of liposarcoma as it can
determine size and location of the tumor and it can preliminarily
evaluate pathological classification and malignancy, clarify the
degree of tumor compression and invasion of surrounding organs and
vessels and provide a reference for the formulation of surgical
plans (13). Compared with CT scan,
an MRI has a higher resolution for soft tissue, more accurately
diagnoses retroperitoneal tumors, clearly displays the distribution
of tumor blood vessels and association between key blood vessels
and can be used to evaluate the degree of tumor invasion (18), which provides guidance for
formulation of surgical plans.
According to the World Health Organization
classification of soft tissue tumors, liposarcoma is divided into
five types (3): WDLPS, DDLPS, MLS,
pleomorphic liposarcoma and myxoid pleomorphic liposarcoma.
Different pathological types have different levels of invasiveness
and prognoses. WDLPS is a low-grade malignancy with the best
prognosis (19). Pleomorphic and
round cell types are highly malignant, prone to local recurrence
and metastasis and have the worst prognosis. The myxoid type is in
between. The present case recurred multiple times but had no
distant metastasis (apart from the fifth recurrence), which may be
due to the higher degree of differentiation. Liposarcoma easily
relapses following surgery due to its unique growth site and
diverse pathological morphology (11,12).
Moreover, with an increased number of recurrences and operations
following the initial surgery, malignancy increases and the
recurrence interval shortens. These two previous research findings
are highly consistent with the disease development characteristics
of our case. The patient experienced five relapses, which is rare,
and the fifth relapse exhibited a transformation of the
pathological type, indicating higher invasion and a poor
prognosis.
For the treatment of RPLS, radical surgical
resection is the first choice and is the only possible cure at
present. In order to achieve therapeutic effects, while ensuring
safety, as much of the tumor should be removed as possible
(20). In cases of malignant
invasion of RPLS, complete resection is often combined with removal
of the adjacent organs that may be affected, such as the kidney,
spleen and gastrointestinal tract. In particular, it is recommended
to perform radical resection of the affected kidney (21). In the present case, at the time of
initial treatment, the right kidney was invaded by the tumor and it
was difficult to separate the tumor tissue. If the right kidney was
not removed, tumor tissue would remain, which would increase the
post-operative recurrence rate. Based on the general condition of
the patient and the function of left kidney being acceptable, the
patient opted to undergo right kidney resection. Even if the tumor
is completely resected, ~50% of patients exhibit tumor recurrence
within 5 years (22). However, the
difficulty and risk of operation following recurrence are
significantly increased and the post-operative efficacy is poor.
The 5-year overall survival rate is ~30%. During the course of
disease, the present patient had five recurrences, five complete
resections and one cytoreductive surgery. At present, the patient
survival period is 13 years, which is rare. Telephone follow-up is
performed every three months for this patient. The patient has good
compliance and often visits the hospital for follow-up.; thus, each
relapse can be identified and treated in a timely manner.
As liposarcoma is not sensitive to radiotherapy,
chemotherapy or immunotherapy, patients generally do not receive
routine adjuvant treatment following surgery (23). With basic and clinical research,
some promising research results and treatment models have emerged.
Systemic treatment methods, such as chemotherapy, molecular
targeted therapy and immunotherapy (24) and radiotherapy (25) have been applied in clinical
practice. Radiotherapy exerts significantly different effects on
various pathological types of RPLS and may improve local control of
patients with WDLPS and G1-2 DDLPS (4). There are reports that chemotherapeutic
drugs have a certain effect on RPLS and anthracycline (26) drugs alone or in combination with
ifosfamide and/or imipramine can be used as the first-line regimen
for the treatment of liposarcoma (27,28).
In the present study, following the fifth relapse, the tumor could
not be completely removed by surgery; thus, the patient was treated
with doxorubicin combined with ifosfamide chemotherapy and oral
targeted therapy with anlotinib.
The present study reviewed cases of recurrent RPLS
reported in the literature published in PubMed (https://pubmed.ncbi.nlm.nih.gov/) over the past
10 years. A total of 16 original studies with complete and
representative data were selected. The clinical data are summarized
in Table I (29–44).
There were eight males (50%) and eight females (50%), with a median
age of 61.5 years (range, 24–73 years). Of these 16 cases, three
(18.75%) had >5 relapses. Two cases (12.5%) exhibited a change
in pathological type following recurrence. Only one case (6.25%)
did not achieve R0 surgical resection. In total, eight patients
(50%) received adjuvant treatment, such as chemotherapy, after
onset or first recurrence. Only one patient (6.25%) succumbed; this
patient experienced recurrence seven times in >3 years and had
undergone eight surgeries. The longest survival time was 24 years.
Surgical resection is still the optimal choice for treatment of
liposarcoma and adjuvant treatment (10), such as chemotherapy, radiotherapy
and targeted therapy, can be administered.
 | Table I.Clinical and histopathological
features, follow-up and clinical outcomes of 16 patients with
recurrent retroperitoneal liposarcoma in the past 10 years. |
Table I.
Clinical and histopathological
features, follow-up and clinical outcomes of 16 patients with
recurrent retroperitoneal liposarcoma in the past 10 years.
| First author,
year | Sex | Age, years | Diameter,
cma | Wide
excisiona | Patho logical
typea | Complete
re-sectiona | Adjuvant therapy | Number of
rela-pses/metastases | Pathological type
after recurrence | Follow-up,
months | (Refs.) |
|---|
| Joel et al,
2020 | M | 73 | 16 | Yes | D | Yes | C, T | 1 | D | NA | (29) |
| Tomoyuki et
al, 2018 | M | 34 | 22 | Yes | D | Yes | C | 2 | D | 42 | (30) |
| Francesk et
al, 2021 | M | 62 | 25 | No | W | No | C | 1 | D | 32 | (31) |
| Niemetz et
al, 2020 | M | 66 | 20 | Yes | Mix | Yes | C, R | 8 | D | 205 | (32) |
| Nagy et al,
2013 | M | 60 | 17 | Yes | D | Yes | C | 7 | NA | 42 (death) | (33) |
| Kanthala et
al, 2021 | F | 40 | NA | No | NA | Yes | C | 2 | D | 72 | (34) |
| Ramu et al,
2018 | M | 61 | 30 | No | NA | Yes | R | 5 | Myx | 89 | (35) |
| El-Helou et
al, 2020 | M | 70 | 50 | No | W | Yes | No | 3 | W | 60 | (36) |
| Nukada et
al, 2018 | F | 60 | NA | No | W | Yes | No | 6 | W | 288 | (37) |
| Li et al,
2021 | F | 24 | 36 | Yes | NA | Yes | No | 1 | D | 24 | (38) |
| Guo et al,
2019 | F | 70 | NA | No | NA | Yes | No | 4 | Myx | 60 | (39) |
| Ono et al,
2018 | M | 62 | NA | Yes | W | Yes | No | 5 | W | 192 | (40) |
| Kuribayashi et
al, 2018 | F | 47 | 4.5 | Yes | D | Yes | No | 1 | D | 53 | (41) |
| Alsalameh et
al, 2019 | F | 63 | 35 | No | W | Yes | No | 1 | W | 34 | (42) |
| Li et al,
2019 | F | 63 | 20 | No | Mix | Yes | C | 1 | NA | 19 | (43) |
| Guo et al,
2022 | F | 60 | 26 | Yes | D | Yes | No | 5 | D | 63 | (44) |
In conclusion, RPLS is rarely observed in clinical
practice. CT scan is the first choice of examination and surgery is
the only curative treatment for this disease. A close follow-up
should be performed to identify recurrence at an early stage. If
recurrence occurs following surgery, operation should be attempted.
If the operation fails to completely remove the tumor, it can be
supplemented with chemotherapy, radiotherapy, targeted therapy and
other auxiliary treatment after the surgery and a positive effect
can still be achieved. In the present case, combination of tumor
reduction surgery, targeted therapy and chemotherapy provided
guidance for the treatment of recurrent RPLS. Considering the
existence of FUS/DDIT3 gene fusion in MLS, FISH assay can better
guide diagnosis and treatment. Periodic review and early diagnosis
and treatment are key to improving the quality of life and survival
time of patients with liposarcoma.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
are available from the corresponding author on reasonable
request.
Authors' contributions
MQ, DL and ZX contributed to the conception and
design of the study. Data collection and analysis were performed by
MQ and DL. The manuscript was written by MQ. MQ and ZX confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The requirement for ethics approval was waived by
the Ethics Committee of Shaoxing Second Hospital (Shaoxing, China)
due to the retrospective nature of the study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of potentially identifying images or
data included in this article.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
AI
|
doxorubicin and ifosfamide
|
|
RPLS
|
retroperitoneal liposarcoma
|
|
WDLPS
|
well-differentiated liposarcoma
|
|
DDLPS
|
dedifferentiated liposarcoma
|
|
MLS
|
myxoid liposarcoma
|
|
FUS-DDIT3
|
fused in sarcoma and DNA damage
inducible transcript 3
|
|
CT
|
computed tomography
|
|
MDM2
|
mouse double minute 2 homolog
|
References
|
1
|
Murphey MD, Arcara LK and Fanburg-Smith J:
Imaging of musculoskeletal liposarcoma with Radiologic-pathologic
correlation1. Radiographics. 25:1371–1395. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Molina G, Hull MA, Chen YL, DeLaney TF, De
Amorim Bernstein K, Choy E, Cote G, Harmon DC, Mullen JT and Haynes
AB: Preoperative radiation therapy combined with radical surgical
resection is associated with a lower rate of local recurrence when
treating unifocal, primary retroperitoneal liposarcoma. J Surg
Oncol. 114:814–820. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Choi JH and Ro JY: The 2020 WHO
Classification of tumors of soft tissue: Selected changes and new
entities. Adv Anat Pathol. 28:44–58. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bill KL, Casadei L, Prudner BC, Iwenofu H,
Strohecker AM and Pollock RE: Liposarcoma: Molecular targets and
therapeutic implications. Cell Mol Life Sci. 73:3711–3718. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tfayli Y, Baydoun A, Naja AS and Saghieh
S: Management of myxoid liposarcoma of the extremity. Oncol Lett.
22:5962021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pérez-Losada J, Sánchez-Martín M,
Rodríguez-García MA, Pérez-Mancera PA, Pintado B, Flores T,
Battaner E and Sánchez-Garćia I: Liposarcoma initiated by
FUS/TLS-CHOP: the FUS/TLS domain plays a critical role in the
pathogenesis of liposarcoma. Oncogene. 19:6015–6022. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Antonescu CR, Tschernyavsky SJ, Decuseara
R, Leung DH, Woodruff JM, Brennan MF, Bridge JA, Neff JR, Goldblum
JR and Ladanyi M: Prognostic impact of P53 status, TLS-CHOP fusion
transcript structure, and histological grade in myxoid liposarcoma:
A molecular and clinicopathologic study of 82 cases. Clin Cancer
Res. 7:3977–3987. 2001.PubMed/NCBI
|
|
8
|
Wang L, Luo R, Xiong Z, Xu J and Fang D:
Pleomorphic liposarcoma. Medicine. 97:e99862018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wan L, Tu C, Qi L and Li Z: Survivorship
and prognostic factors for pleomorphic liposarcoma: A
population-based study. J Orthop Surg Res. 16:1752021. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tyler R, Wanigasooriya K, Taniere P,
Almond M, Ford S, Desai A and Beggs A: A review of retroperitoneal
liposarcoma genomics. Cancer Treat Rev. 86:1020132020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Titulaer MJ and Verschuuren JJ:
Lambert-Eaton myasthenic syndrome: Tumor versus nontumor forms.
Annals of the New York Academy of Sciences. 1132:129–134. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Keung EZ, Hornick JL, Bertagnolli MM,
Baldini EH and Raut CP: Predictors of outcomes in patients with
primary retroperitoneal dedifferentiated liposarcoma undergoing
surgery. J Am Coll Surg. 218:206–217. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hu B, Liu Y, Cheng L, Li W and Cao X:
SPECT/CT imaging of retroperitoneal extraskeletal osteosarcoma.
Clin Nucl Med. 39:200–202. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
von Mehren M, Kane JM, Agulnik M, Bui MM,
Carr-Ascher J, Choy E, Connelly M, Dry S, Ganjoo KN, Gonzalez RJ,
et al: Soft tissue sarcoma, version 2.2022, NCCN clinical practice
guidelines in oncology. J Natl Compr Canc Netw. 20:815–833. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Callegaro D and Gronchi A: Radiotherapy in
retroperitoneal liposarcoma: Are We Looking for an Answer in the
Wrong Place? Ann Surg Oncol. 306:675–677. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Schwartz LH, Litière S, de Vries E, Ford
R, Gwyther S, Mandrekar S, Shankar L, Bogaerts J, Chen A, Dancey J,
et al: RECIST 1.1-Update and clarification: From the RECIST
committee. Eur J Cancer. 62:132–137. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Taguchi S, Kume H, Fukuhara H, Morikawa T,
Kakutani S, Takeshima Y, Miyazaki H, Suzuki M, Fujimura T, Nakagawa
T, et al: Symptoms at diagnosis as independent prognostic factors
in retroperitoneal liposarcoma. Mol Clin Oncol. 4:255–260. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kamper L, Brandt AS, Scharwächter C, Kukuk
S, Roth S, Haage P and Piroth W: MR evaluation of retroperitoneal
fibrosis. RoFo. 183:721–726. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sung MS, Kang HS, Suh JS, Lee JH, Park JM,
Kim JY and Lee HG: Myxoid liposarcoma: Appearance at MR imaging
with histologic correlation. Radiographics. 20:1007–1019. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Munoz P, Bretcha-Boix P, Artigas V and
Asencio JM: Surgical principles of primary retroperitoneal sarcoma
in the era of personalized treatment: A review of the frontline
extended surgery. Cancers (Basel). 14:40912022. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mussi C, Colombo P, Bertuzzi A, Coladonato
M, Bagnoli P, Secondino S, Navarria P, Morenghi E, Santoro A and
Quagliuolo V: Retroperitoneal sarcoma: Is it time to change the
surgical policy? Ann Surg Oncol. 18:2136–2142. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
MacNeill AJ, Miceli R, Strauss DC,
Bonvalot S, Hohenberger P, Van Coevorden F, Rutkowski P, Callegaro
D, Hayes AJ, Honoré C, et al: Post-relapse outcomes after primary
extended resection of retroperitoneal sarcoma: A report from the
Trans-Atlantic RPS Working Group. Cancer. 23:1971–1978. 2017.
View Article : Google Scholar
|
|
23
|
Tan MC, Brennan MF, Kuk D, Agaram NP,
Antonescu CR, Qin LX, Moraco N, Crago AM and Singer S:
Histology-based Classification predicts pattern of recurrence and
improves risk stratification in primary retroperitoneal sarcoma.
Annals Surg. 263:593–600. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Miao C, Liu D, Zhang F, Wang Y, Zhang Y,
Yu J, Zhang Z, Liu G, Li B, Liu X and Luo C: Association of FPGS
genetic polymorphisms with primary retroperitoneal liposarcoma. Sci
Rep. 5:90792015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
De Vita A, Mercatali L, Recine F, Pieri F,
Riva N, Bongiovanni A, Liverani C, Spadazzi C, Miserocchi G,
Amadori D and Ibrahim T: Current classification, treatment options,
and new perspectives in the management of adipocytic sarcomas. Onco
Targets Ther. 9:6233–6246. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
De Vita A, Recine F, Miserocchi G, Pieri
F, Spadazzi C, Cocchi C, Vanni S, Liverani C, Farnedi A, Fabbri F,
et al: The potential role of the extracellular matrix in the
activity of trabectedin in UPS and L-sarcoma: Evidences from a
patient-derived primary culture case series in tridimensional and
zebrafish models. J Exp Clin Cancer Res. 40:1652021. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Antman K, Crowley J, Balcerzak SP, Rivkin
SE, Weiss GR, Elias A, Natale RB, Cooper RM, Barlogie B, Trump DL,
et al: An intergroup phase III randomized study of doxorubicin and
dacarbazine with or without ifosfamide and mesna in advanced soft
tissue and bone sarcomas. J Clin Oncol. 11:1276–1285. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Bramwell VHC, Anderson D and Charette MLL;
Sarcoma Disease Site Group, : Doxorubicin-based chemotherapy for
the palliative treatment of adult patients with locally advanced or
metastatic soft tissue sarcoma. Cochrane Database Syst Rev.
2003:CD0032932003.PubMed/NCBI
|
|
29
|
Horowitz J, Singhal M, Marrero D,
Bashjawish F, Leto D, Winters M and Jeberaeel J: A Multi-Modality
treatment of retroperitoneal De-Differentiated liposarcoma. Am J
Case Rep. 21:e9192452020. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Tatenuma T, Mizuno N, Jikuya R, Hashizume
A, Yasui M, Umemoto S, Kawai M, Hiruma T and Kishida T:
Retroperitoneal liposarcoma with multiple recurrence of lung
metastases treated by multimodal therapy centering on the
operation: A case report. Nihon Hinyokika Gakkai Zasshi. 109:25–29.
2018.(In Japanese). PubMed/NCBI
|
|
31
|
Mulita F, Verras GI, Liolis E,
Tchabashvili L, Kehagias D, Kaplanis C, Perdikaris I and Kehagias
I: Recurrent retroperitoneal liposarcoma: A case report and
literature review. Clin Case Rep. 9:e047172021. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Niemetz I, Faß J and Wolf M: Multiple
recurrent retroperitoneal liposarcoma in a 66-year-old man.
Internist (Berl). 61:217–222. 2020.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Nagy V, Bober J, Zavacky P, Brandebur O Jr
and Svajdler M: The recurrent primary retroperitoneal liposarcoma.
Bratisl Lek Listy. 114:662–667. 2013.PubMed/NCBI
|
|
34
|
Kanthala L, Ray S, Aurobindo Prasad Das S,
Nundy S and Mehta N: Recurrent giant retroperitoneal liposarcoma:
Review of literature and a rare case report. Ann Med Surg (Lond).
65:1023292021.PubMed/NCBI
|
|
35
|
Ramu D, Manjunath S and Anuradh G:
Recurrent retroperitoneal liposarcoma: A case report and literature
review. Indian J Surg Oncol. 9:640–643. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
El-Helou E, Alimoradi M, Sabra H, Naccour
J, Haddad MM and Bitar H: Recurrent giant retroperitoneal
liposarcoma with 10 years follow up. Case report and review of
literature. Int J Surg Case Rep. 75:504–512. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Nukada S, Aoyama T, Kamiya M, Amano S,
Tamura S, Harada H, Sato T, Yukawa N, Oshima T, Rino Y and Masuda
M: A case of retroperitoneal liposarcoma resected 6 times in 24
years. Gan To Kagaku Ryoho. 45:106–108. 2018.(In Japanese).
PubMed/NCBI
|
|
38
|
Li RSO, Maglangit SACA, Cartagena-Lim JT
and Dofitas RB: Case of a huge recurrent retroperitoneal
liposarcoma diagnosed in the second trimester of pregnancy. BMJ
Case Rep. 14:e2436392021. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Guo S, Xu Y, Qian F, Ma J, Wang S, Chen P
and Zong L: A recurrent giant retroperitoneal myxoid liposarcoma: A
case report and literature review. Transl Cancer Res. 8:2672–2676.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Ono Y, Aoyama T, Morita J, Amano S,
Sawazaki S, Numata M, Hayashi T, Yamada T, Sato T, Yukawa N, et al:
A case report of retroperitoneal liposarcoma resected six times for
16 years. Gan To Kagaku Ryoho. 45:1507–1509. 2018.(In Japanese).
PubMed/NCBI
|
|
41
|
Kuribayashi S, Nakai Y, Tsuji H, Yumiba S,
Hatano K, Nakayama M, Kakimoto K, Kubo C and Nishimura K: A case of
retroperitoneal liposarcoma in which magnetic resonance imaging was
useful in the decision of resection of primary and recurrent
tumors. Hinyokika Kiyo. 64:145–149. 2018.(In Japanese). PubMed/NCBI
|
|
42
|
Alsalameh BK and Abufkhaida BS: Recurrent
abdominal liposarcoma presenting with intestinal obstruction. J
Surg Case Rep. 2019:rjz1882019. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Li CF, Yang XR, Yao J, Huang JJ, Tan N,
Zhang SY, Xu GQ and Zheng H: Giant recurrent mixed-type liposarcoma
of the retroperitoneum: Report of a case and review of literature.
Int J Clin Exp Pathol. 12:1406–1411. 2019.PubMed/NCBI
|
|
44
|
Guo J, Qiu F, Zhao J, Lu Q, Fu W, Xu Q and
Huang D: Case report: Retroperitoneal sarcoma in six operations:
Our experience in operative management of blood vessels. Front
Oncol. 12:8850332022. View Article : Google Scholar : PubMed/NCBI
|