Introduction
Pulmonary embolism (PE) is a common acute and
potentially fatal cardiovascular disorder that needs immediate
medical intervention (1). According
to guidelines, PE should be diagnosed by a combination of clinical
features (common symptoms include dyspnea, chest pain, hemoptysis
and syncope), D-dimer levels and radiological detection. However,
the diagnosis of PE is challenging and often delayed due to lack of
specific clinical presentation. In the past 10 years, the increased
sensitivity of imaging modalities has doubled rates of hospital
admission for pulmonary embolism (1). The causes of PE consist of venous
thromboembolism and non-thrombotic embolism, such as fat, air,
amniotic fluid, septic and tumor embolism (2).
Choriocarcinoma is a highly malignant trophoblastic
cancer that is characterized by secreting high levels of human
chorionic gonadotropin β-subunit (β-hCG) and hematogenous spread to
various organs, particularly to the lungs (3). Although the lungs are the most common
metastatic site, pulmonary artery embolism by choriocarcinoma is
extremely rare. Currently, to the best of our knowledge, the total
number of case studies that have reported pulmonary artery embolism
by choriocarcinoma in the literature is <15. The present study
reports a case of pulmonary artery embolism with choriocarcinoma in
a 21-year-old woman who was initially misdiagnosed with pulmonary
pneumonia, and then successfully treated with chemotherapy and the
β-hCG level normalized. Additionally, the existing literature was
reviewed and the clinical features and treatment outcomes were
summarized.
Case report
A 21-year-old female was admitted to the Pulmonary
and Critical Care Medicine Ward at Qingdao West Coast Area Central
Hospital (Qingdao, China) in January 2022 with complaints of chest
pain and slight fever for 4 months. No cough, sputum production and
dyspnea was present. At that time, the patient was diagnosed with
acute pneumonia based on chest computed tomography (CT), which
revealed several scattered shadows on both lungs. Acid-fast bacilli
staining using bronchoalveolar lavage showed negative results.
Antibiotic treatment (specific medication not available) was
administered, and the condition of the patient improved during the
antibiotics course.
Subsequently, 4 months later (May 2022), the patient
was referred to the Affiliated Hospital of Qingdao University
(Qingdao, China) due to an episode of chest pain and slight fever
again. On examination, the patient had a body weight of 48.5 kg, a
respiratory rate of 19 breaths per min, a pulse rate of 77
beats/min and a blood pressure of 88/55 mm/Hg. The routine blood
test showed the white blood cell count was 4.86×109/l,
platelet count was 346×109/l and the hemoglobin level
was 100 g/l. Liver function test showed that the glutamic-pyruvic
transaminase level was 7.2 U/l (normal range, 7–40 U/l) and the
glutamic oxaloacetic transaminase level was 13.5 U/l (normal rage,
13–35 U/l). The coagulation function tests showed that the
prothrombin time was 12.3 sec (normal range, 10–14 sec) and the
activated partial thromboplastin time was 35.2 sec (normal range,
22–38 sec). The D-dimer value was 420 ng/ml (normal rage, <500
ng/ml). The levels of tumor biomarkers, including carcinoembryonic
antigen, α-fetoprotein, squamous cell carcinoma antigen,
neuron-specificenolase, carbohydrate antigen (CA)125, CA19-9,
CA15-3 and CA72-4, were also in the normal ranges. Serum
tuberculosis antibody test result was negative. The
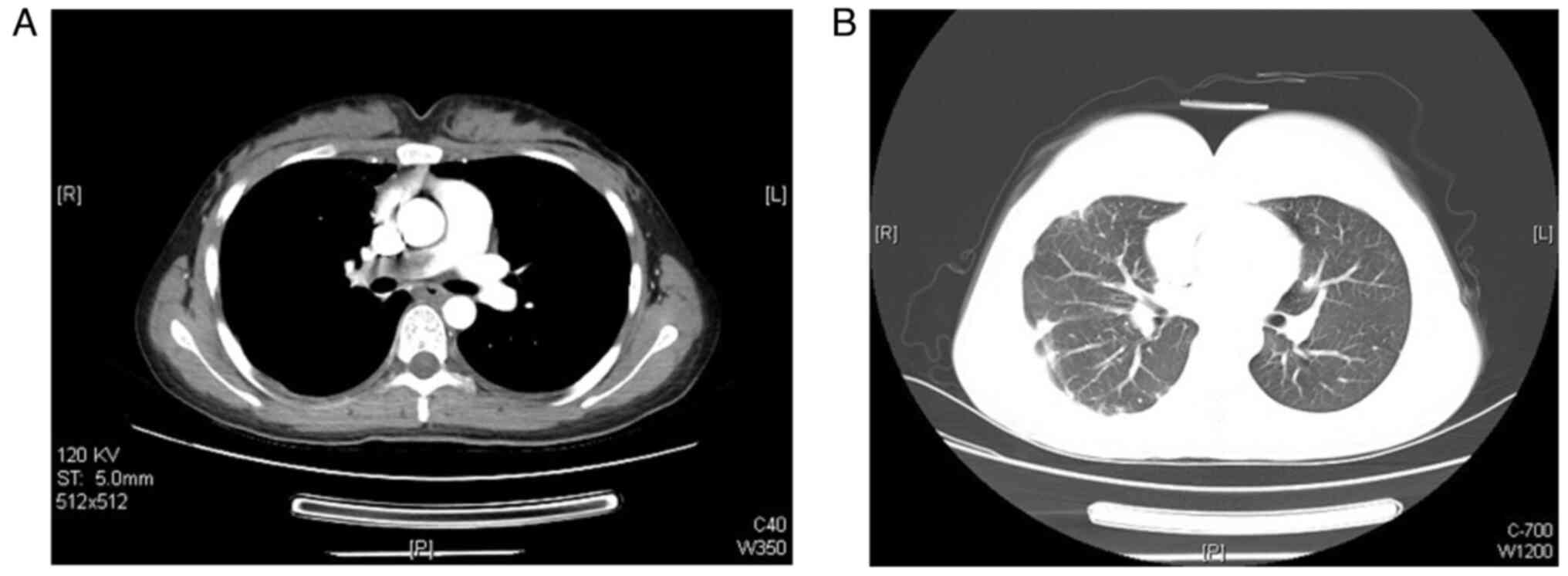
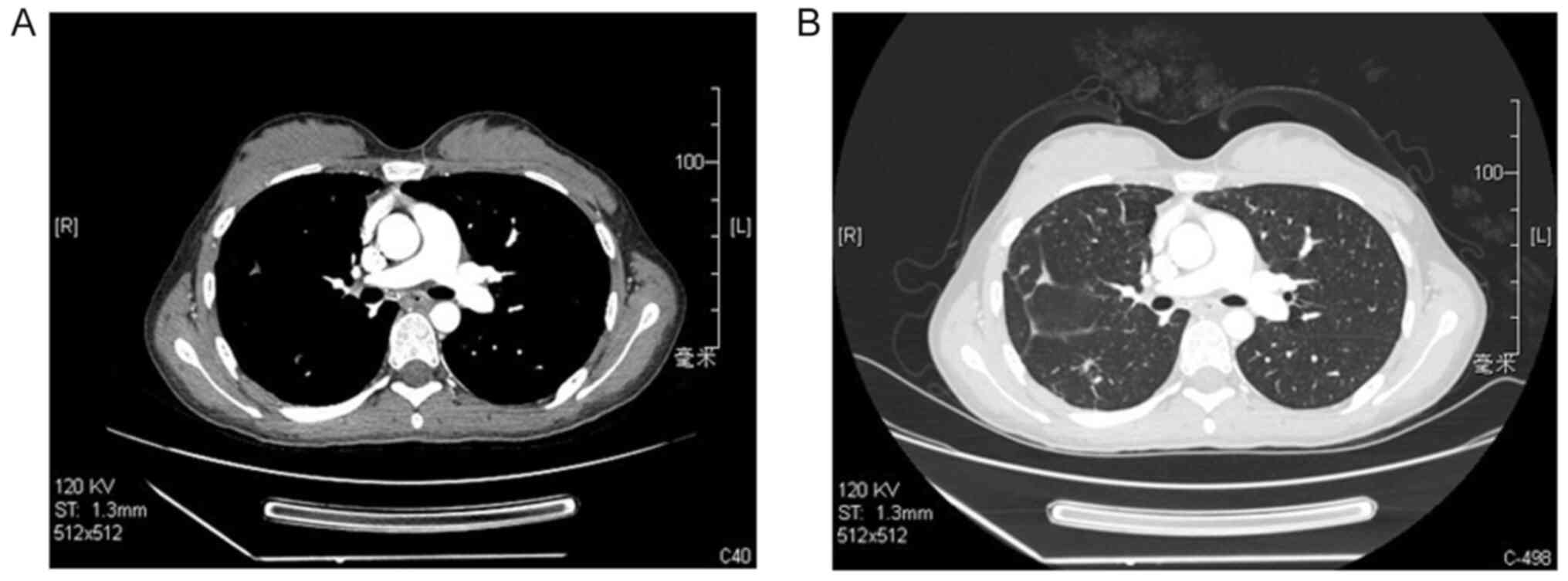
contrast-enhanced chest CT scan revealed complete occlusion of the
right pulmonary artery (Fig. 1A).
The scan further displayed multiple nodular fuzzy shadows with
necrosis in the bilateral lungs (Fig.
1B). However, echocardiography displayed poor blood flow
filling at the initial segment of the pulmonary artery, pulmonary
hypertension (up to 28 mmHg), along with slight tricuspid
regurgitation. Bilateral ultrasound examination of the vasculature
of the two legs revealed no evidence of deep-vein thrombosis.
To seek the cause of PE, the medical history of the
patient was requested. The patient had experienced one drug-induced
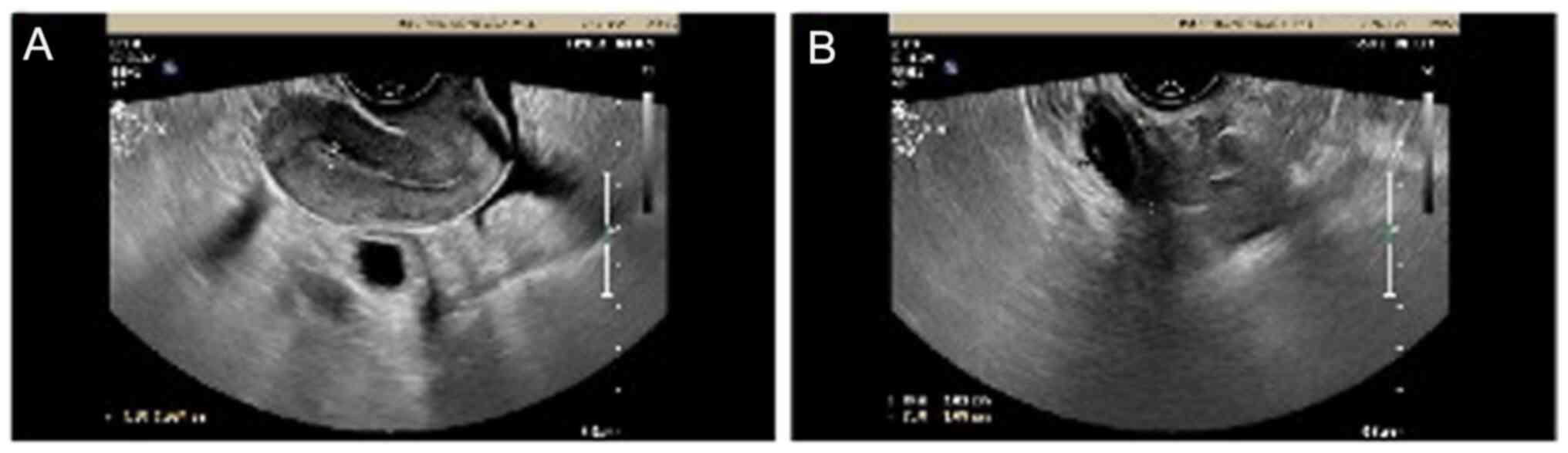
abortion in July 2021. Ultrasonography of the pelvis after the
abortion was normal (Fig. 2). The
serum β-hCG decreased from 11,937.00 to 6,410 mIU/l at 1 week after
abortion. Later, the patient did not undergo further examination
for β-hCG. No intermittent bleeding or complications occurred after
the abortion. The last menstrual period of the patient was May
2022. The patient had a long-term use of oral contraceptives and no
other relevant medical history. Additional tests were conducted in
the Affiliated Hospital of Qingdao University. However, the serum
β-hCG level was significantly elevated (>10,000 mIU/l).
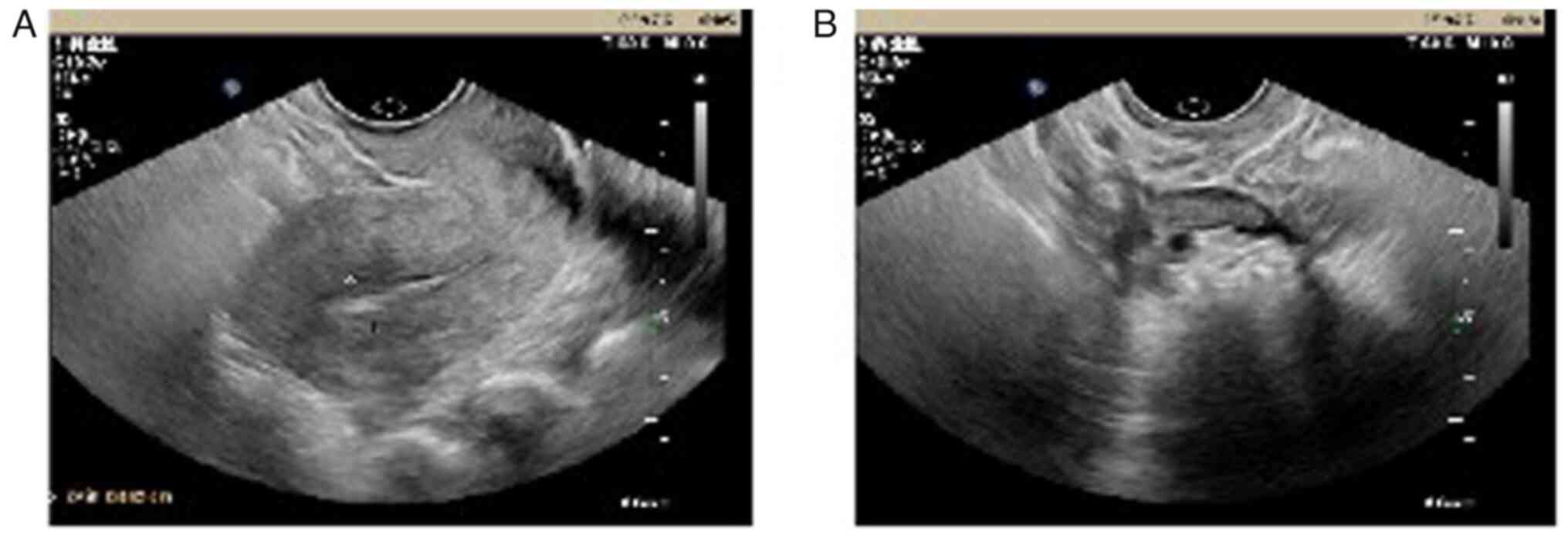
Ultrasound examination of the pelvis did not reveal an ectopic
pregnancy (Fig. 3). Positron
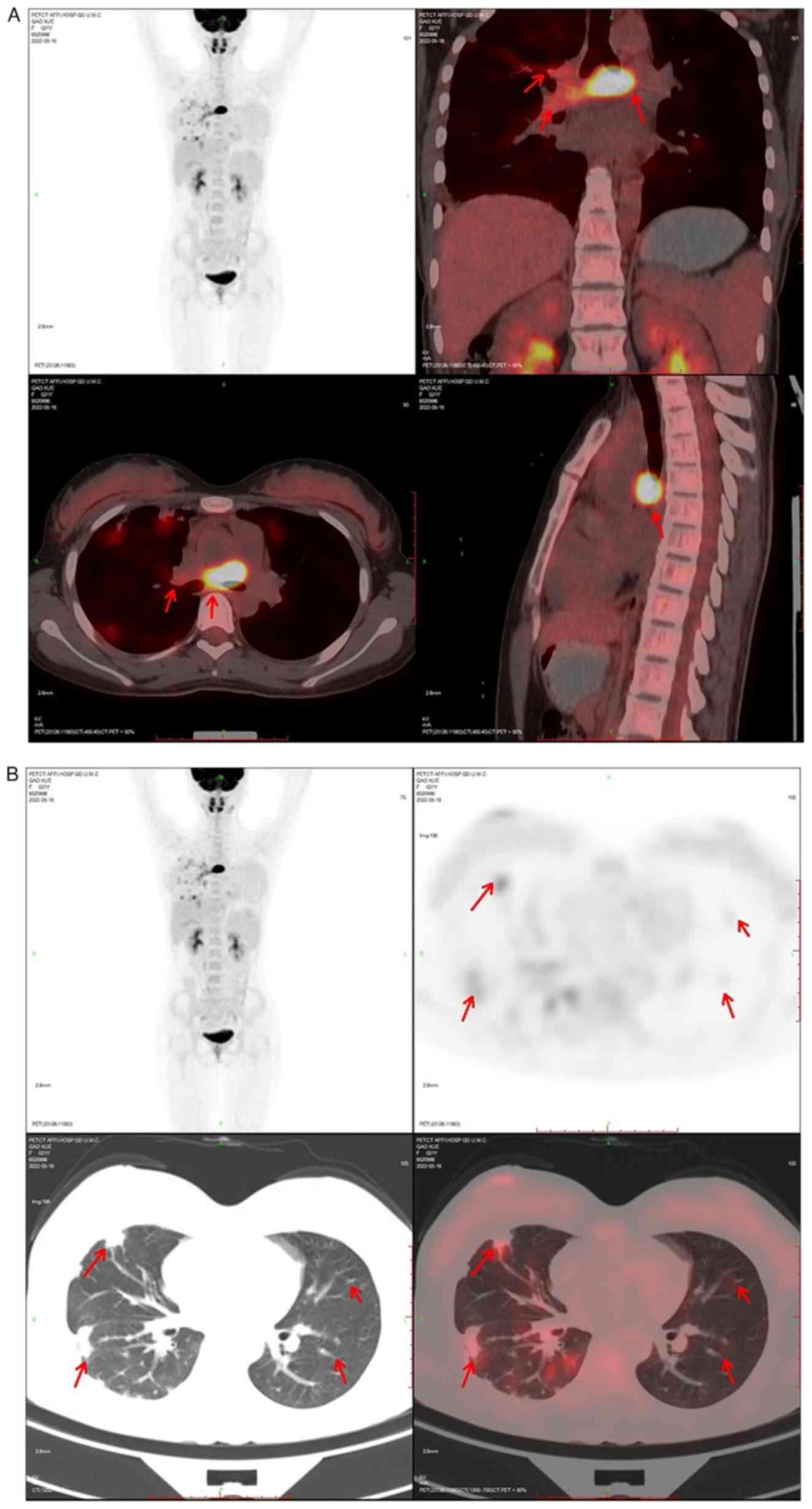
emission tomography with
2-(fluorine-18)-fluoro-2-deoxy-D-glucose/computed tomography
(FDG-PET/CT), with a sensitivity of 71.4% and specificity of 90% in
differentiating between tumor and thromboembolism (4), was performed and revealed the abnormal
hypermetabolic lesion (maximum standardized uptake value, 27.5)
overlying the right pulmonary artery (Fig. 4A). Bilateral peripheral lungs
opacities with mild hypermetabolic lesions were suggestive of a
pulmonary infarction caused by tumor embolism (Fig. 4B). No other focal FDG-avid lesion
was observed in the brain, abdomen or pelvic cavity. According to
the guidelines of European Society for Medical Oncology (5) and the criteria formulated by the
International Federation of Gynecology and Obstetrics (6), the diagnosis of a primary pulmonary
artery with choriocarcinoma was established. Subsequently, the
patient was initiated on chemotherapy (EMACO regimen) and responded
well to the treatment. The period of chemotherapy with EMACO was
from May 2022 to March 2023. After the 12 cycles of chemotherapy,
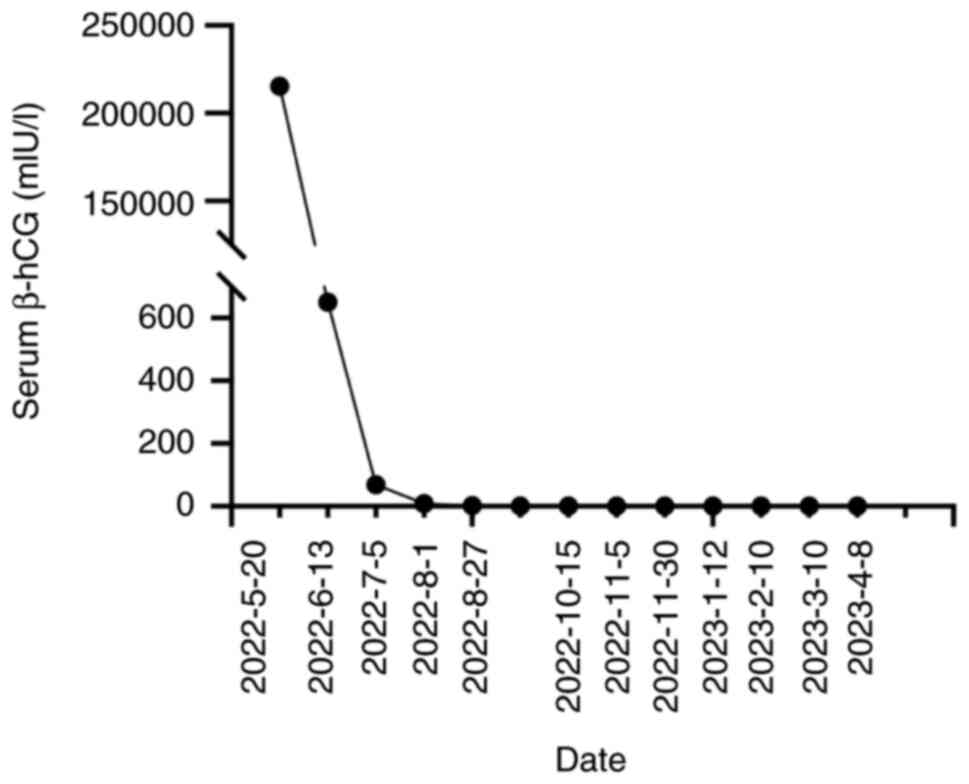
serum β-hCG decreased to <0.10 mIU/l (Fig. 5) and the occlusion in the right
pulmonary artery disappeared on contrast-enhanced chest CT
(Fig. 6). The patient is currently
alive and has achieved complete remission during follow-up.
Discussion
Choriocarcinoma is an aggressive and highly
malignant tumor that can be classified into two subtypes:
Gestational or non-gestational (7),
~50% of cases follow a complete hydatidiform mole, 25% arise after
abortion and 25% occur after normal or ectopic pregnancies
(8). Non-gestational can be found
in various organs, often in the lung (9). Pulmonary artery embolism caused by
choriocarcinoma is extremely rare and has been described as a rare
cause of PE and pulmonary artery hypertension. The present study
searched the PubMed database (https://pubmed.ncbi.nlm.nih.gov) for articles
published from January 1, 1959, to February 28, 2023, using the
term ‘choriocarcinoma’ and ‘pulmonary artery’. The exclusion
criterion was that the choriocarcinoma had not metastasized to the
pulmonary artery. Only 15 cases have previously been documented in
English-language medical literature, which have been reviewed in
Table I (10–21).
The mean age of presentation was 32.06 years (range, 21–51 years),
and the sex were all female. The most common symptoms were dyspnea
(11/15 or 73.3%) and chest pain (8/15 or 53.3%). Approximately 13
cases had a history of spontaneous abortion and no primary uterine
tumor, and the average time for diagnosis of choriocarcinoma after
the onset of symptom was 5 months.
 | Table I.Clinical features of primary pulmonary
artery with choriocarcinoma cases. |
Table I.
Clinical features of primary pulmonary
artery with choriocarcinoma cases.
| First author
(year) | Sex | Age, years | History | Clinical
presentation | Serum HCG, IU/l | Treatment | Survival | (Refs.) |
|---|
| Seckl et al
(1991) | F | 25 | Spontaneous abortion
6 years before | Pleuritic chest pain,
exertional dyspnea | 103,200 | Chemotherapy +
anticoagulation | ANED (4 years) | (10) |
|
| F | 24 | Spontaneous abortion
2 months before | Pleuritic chest pain,
hemoptysis, dyspnea | 280,000 | Chemotherapy +
anticoagulation | ANED |
|
|
| F | 30 | Spontaneous abortion
8 months before | Chest pain | 132,300 | Chemotherapy +
anticoagulation | ANED (8 years) |
|
| Yutani et al
(1993) | F | 47 | Therapeutic abortion
3 years before | Chest pain,
dyspnea | No | EL | DOD | (11) |
| Trubenbach et
al (1997) | F | 33 | Abortion 10 months
before | Exertional dyspnea,
chest pain, cough | 129.5 | Chemotherapy | DOD | (12) |
| Savage et al
(1998) | F | 28 | Three live
pregnancies, the latest one 3 years before | Cough, shortness of
breath, chest pain | 339,535 | Anticoagulation +
chemotherapy | ANED | (13) |
| Chai et al
(2000) | F | 23 | Spontaneous abortion
10 months before | Progressive dyspnea,
cough | >2,000,000 | NO | DOD | (14) |
| Watanabe et al
(2002) | F | 42 | Two previous
spontaneous abortions | Exertional
dyspnea | >70,000 | EL +
chemotherapy | ANED | (15) |
| Brusselle et
al (2005) | F | 31 | Four previous
spontaneous abortions | Progressive
dyspnea | 168,000 | EL +
chemotherapy | ANED | (16) |
| Ong et al
(2008) | F | 51 | Abortion 5 years
before | Dyspnea, dry cough,
hemoptysis | No detail | EL +
chemotherapy | NA | (17) |
| Zaheer et al
(2009) | F | 51 | Two live
pregnancies | Dyspnea, chest
pain, cough, fever | 291,128 | Chemotherapy | ANED | (18) |
| Ma et al
(2013) | F | 24 | Three previous
spontaneous abortions, the latest one 1 years latest | Dyspnea | No detail | EL | DOD | (19) |
| Zhu et al
(2016) | F | 25 | Three spontaneous
abortions | Dyspnea,
cardiopalmus | Undetected | EL | DOD | (20) |
| Yang and Peng
(2017) | F | 26 | Two abortions, the
latest one 3 years before | Cough,
expectoration, night sweat | 128,575.77 | Chemotherapy | DOD | (21) |
| Present case | F | 21 | One previous
abortion | Chest pain, slight
fever | >100,00 | Chemotherapy | ANED |
|
The underlying mechanism of primary choriocarcinoma
of the pulmonary artery is still uncertain. Cases of
choriocarcinoma arising a number of years after total hysterectomy
and bilateral salpingo-oophorectomy are rare (17). Tanimura et al (22) revealed that trophoblasts can be
found in the pulmonary artery in autopsies of 9/10 patients who
died after delivery or abortion. Therefore, it has been
hypothesized that primary pulmonary artery with choriocarcinoma in
women may be due to malignant transformation of the normal villous
trophoblasts that entered the pulmonary artery at the time of
delivery or abortion (22).
However, others hypothesize that a pulmonary choriocarcinoma
without the evidence of pelvic cavity lesions may represent
metastases from an undetected gonadal tumor, which might undergo a
spontaneous regression, the so called ‘burn-out’ phenomenon that is
a unique and specific feature of choriocarcinoma (23–25).
Due to the lack of distinct symptoms, specific signs
or typical radiography, the diagnosis of pulmonary artery
choriocarcinoma embolism is difficult in the early stages. In the
present case, the patient was initially misdiagnosed with acute
pneumonia and given antibiotic treatments. However, most physicians
may pay little attention to the irregular period of menstruation
and abortion, and/or has low awareness of linking the
choriocarcinoma with respiratory symptoms. As found in the
literature review, the average time for the diagnosis of pulmonary
artery choriocarcinoma after the onset of symptoms was 5 months.
Although choriocarcinoma is rare, it should be considered for any
women of child-bearing age who present with dyspnea, chest pain, PE
or pulmonary arterial hypertension, and a history of menstruation,
pregnancy and abortion should be reviewed in detail (21).
Choriocarcinoma is a malignant epithelial tumor
characterized by secretion of β-hCG (26). Accurate and prompt diagnosis of
choriocarcinoma depends on correlation with clinical findings and
the β-hCG levels. Watanabe et al (15) indicated the importance of
considering choriocarcinoma and testing the serum β-hCG levels when
evaluating women of childbearing age presenting with pulmonary
artery hypertension or PE. The serum β-hCG level performed as a
diagnostic indicator and was recommended to be tested in fertile
women to differentiate the causes of a PE. The degree of tumoral
enhancement appears to correlate with β-hCG level. A previous
report suggests that finding an elevated serum β-hCG level may have
led to an earlier diagnosis (21).
In addition, it also plays an important role in the evaluation of
its prognosis of treatment outcomes. In the present study, the
β-hCG levels notably dropped following chemotherapy in the patient.
Thus, testing the β-hCG level is recommended as a parameter of
prognosis and follow-up after treatment (26).
FDG-PET/CT has been increasingly performed to
diagnose and stage primary malignancies. A previous report has
confirmed that PET/CT can be useful to accurately distinguish
between benign and malignant tumors, as malignancy shows high FDG
accumulation (18). Similarly,
PET/CT has been considered to be a sensitive tool for the detection
of lung metastasis from choriocarcinoma (27). In the present case, PET/CT was
performed to reveal a lesion in the right pulmonary artery, which
showed that FDG accumulation to the pulmonary artery was high and
no other abnormal FDG uptake was found in the whole body including
the pelvic cavity. Although PET/CT can demonstrate sites of
metastasis with increased metabolic imaging, it did not have a
greater diagnostic accuracy compared with the conventional imaging
techniques in gestational trophoblastic neoplasia (28,29).
PET-CT may attribute to discriminate ambiguous lesions at
conventional imaging techniques and assess disease recurrence that
may not be revealed at routine imaging with elevated β-hCG levels.
Thus, the present case emphasizes the important role of PET-CT in
differentiating between a tumor and a blood clot.
Choriocarcinoma responds well to chemotherapeutic
agents, which implies timely diagnosis and initiation of
chemotherapy are crucial to achieve the best possible outcome. It
is important to start prompt treatment in order to prolong patient
survival, and complete remission can be achieved with appropriate
chemotherapy (cure rate >89%) (20). The guidelines of the European
Society for Medical Oncology suggest that gestational trophoblastic
neoplasia is treated clinically, as a biopsy of the lesion is
highly risky in the vascular disease (5). Similar to the present case, the
diagnosis of a pulmonary artery with choriocarcinoma is based
mainly on high levels of serum β-hCG and the characteristic
appearance of PET-CT scans in non-pregnant women. EMACO
chemotherapy was initiated immediately and the patient responded
positively, with serum β-hCG levels falling to within normal
levels. Chung et al (30)
reported a case where a patient under venoarterial extracorporeal
membrane oxygenation (ECMO) accepted chemotherapy successfully and
achieved a good outcome. Therefore, chemotherapy compromises an
attractive management approach for pulmonary choriocarcinoma
embolism.
In conclusion, pulmonary artery embolism by
choriocarcinoma is a rare malignant tumor, with a lack of distinct
symptoms, specific signs or typical radiography. Early diagnosis is
challenging, which leads to substantial delays in the treatment.
Choriocarcinoma should be considered for any women of child-bearing
age who presents with a massive PE. It can be diagnosed by the
combination of elevated serum β-HCG with a characteristic
appearance of PET-CT. The present case emphasizes the importance of
early diagnosis and promptly appropriate chemotherapy in this
disease.
Acknowledgements
Not applicable.
Funding
This study was supported by the Youth Foundation of the
Affiliated Hospital of Qingdao University (grant no.
QDFYQN202102033).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
QW and PZ were responsible for patient management
and interpreted the patient data. WX, PW, DR, CG, XD and YC
designed the study, acquired the data and analyzed the data. WX
draft the manuscript and critically revised the manuscript. PW and
WX confirm the authenticity of all the raw data. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case presentation and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Duffett L, Castellucci LA and Forgie MA:
Pulmonary embolism: Update on management and controversies. BMJ.
370:m21772020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sahiti S, Rotman S and Benmachiche M:
Pulmonary tumor embolism. Rev Med Suisse. 17:2034–2037. 2021.(In
French). PubMed/NCBI
|
|
3
|
Yamanari T, Sawamura M, Lee HJ, Kai Chi C
and Katz A: Acquired pulmonary arteriovenous fistula within
metastasis from choriocarcinoma: A case report. Case Rep Oncol.
10:671–675. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sharma P, Kumar R, Jeph S, Karunanithi S,
Naswa N, Gupta A and Malhotra A: 18F-FDG PET-CT in the diagnosis of
tumor thrombus: Can it be differentiated from benign thrombus? Nucl
Med Commun. 32:782–788. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Seckl MJ, Sebire NJ, Fisher RA, Golfier F,
Massuger L and Sessa C; ESMO Guidelines Working Group, :
Gestational trophoblastic disease: ESMO Clinical Practice
Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 24
(Suppl 6):vi39–vi50. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ngan HYS, Seckl MJ, Berkowitz RS, Xiang Y,
Golfier F, Sekharan PK, Lurain JR and Massuger L: Diagnosis and
management of gestational trophoblastic disease: 2021 update. Int J
Gynaecol Obstet. 155 (Suppl 1):S86–S93. 2021. View Article : Google Scholar
|
|
7
|
Telli TA, Demircan NC, Alan O, Tuylu TB,
Arikan R, Ercelep O, Atici AE, Ergelen R, Seven IE, Babacan NA, et
al: A rare case of primary rectal choriocarcinoma and review of the
literature. J Oncol Pharm Pract. 26:989–994. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ngan HYS, Seckl MJ, Berkowitz RS, Xiang Y,
Golfier F, Sekharan PK, Lurain JR and Massuger L: Update on the
diagnosis and management of gestational trophoblastic disease. Int
J Gynaecol Obstet. 143 (Suppl 2):79–85. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Libshitz HI, Baber CE and Hammond CB: The
pulmonary metastases of choriocarcinoma. Obstet Gynecol.
49:412–416. 1977.PubMed/NCBI
|
|
10
|
Seckl MJ, Rustin GJ, Newlands ES, Gwyther
SJ and Bomanji J: Pulmonary embolism, pulmonary hypertension, and
choriocarcinoma. Lancet. 338:1313–1315. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yutani C, Imakita M, Ishibashi-Ueda H,
Katsuragi M, Yoshioka T and Kunieda T: Pulmonary hypertension due
to tumor emboli: A report of three autopsy cases with morphological
correlations to radiological findings. Acta Pathol Jpn. 43:135–141.
1993.PubMed/NCBI
|
|
12
|
Trubenbach J, Pereira PL, Huppert PE,
Farnsworth C, Mayer R, Feine U and Claussen CD: Primary
choriocarcinoma of the pulmonary artery mimicking pulmonary
embolism. Br J Radiol. 70:843–845. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Savage P, Roddie M and Seckl MJ: A
28-year-old woman with a pulmonary embolus. Lancet. 352:301998.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chai L, Ong KC and Ng SB: A case of
pulmonary tumour embolism mimicking miliary tuberculosis.
Respirology. 5:297–299. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Watanabe S, Shimokawa S, Sakasegawa K,
Masuda H, Sakata R and Higashi M: Choriocarcinoma in the pulmonary
artery treated with emergency pulmonary embolectomy. Chest.
121:654–656. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Brusselle G, Van Nooten G, Delrue L,
Vanwalleghem L, Dhaene K, Renard V and Joos G: Cor pulmonale and
respiratory failure in a young woman. Respiration. 72:549–551.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ong C, Low SY, Thirugnanam A, Loh A and
Eng P: Metastatic trophoblastic disease masquerading as pulmonary
embolism. Thorax. 63:10302008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zaheer S, Osmany S, Lai HK and Eng DN:
Usefulness of F-18 fluorodeoxyglucose positron emission
tomography/computed tomography in a case of choriocarcinoma
presenting as pulmonary embolism. Clin Nucl Med. 34:343–345. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ma L, Zhu Y, Sun H, Li F, Shao Y and Zhang
S: A lesson from a rare cause of pulmonary embolism. Respir Care.
58:e149–e152. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhu Y, Yu M, Ma L, Xu H and Li FR:
Choriocarcinoma-associated pulmonary thromboembolism and pulmonary
hypertension: A case report. J Biomed Res. 30:243–247. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yang M and Peng L: Role of chemotherapy
and thrombolysis in treatment of choriocarcinoma accompanied with
pulmonary embolism: A case report with literature review. Medicine
(Baltimore). 96:e78662017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tanimura A, Natsuyama H, Kawano M,
Tanimura Y, Tanaka T and Kitazono M: Primary choriocarcinoma of the
lung. Hum Pathol. 16:1281–1284. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Rossi G, Valli R, Rivasi F and Longo L:
Does primary pulmonary choriocarcinoma really exist? Chest.
123:3132003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Berthod G, Bouzourene H, Pachinger C and
Peters S: Solitary choriocarcinoma in the lung. J Thorac Oncol.
5:574–575. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wu PS: Primary choriocarcinoma of the
lung: A case report and literature review. Int J Clin Exp Pathol.
13:2352–2355. 2020.PubMed/NCBI
|
|
26
|
Shaaban AM, Rezvani M, Haroun RR, Kennedy
AM, Elsayes KM, Olpin JD, Salama ME, Foster BR and Menias CO:
Gestational Trophoblastic Disease: Clinical and Imaging Features.
Radiographics. 37:681–700. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Maruoka Y, Abe K, Baba S, Isoda T, Matsuo
Y, Kubo Y, Ogawa S, Yano T, Sasaki M and Honda H: A case of
pulmonary choriocarcinoma metastasis with unusual FDG-PET and CT
findings: Correlation with pathology. Ann Nucl Med. 26:835–839.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mapelli P, Mangili G, Picchio M, Gentile
C, Rabaiotti E, Giorgione V, Spinapolice EG, Gianolli L, Messa C
and Candiani M: Role of 18F-FDG PET in the management of
gestational trophoblastic neoplasia. Eur J Nucl Med Mol Imaging.
40:505–513. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lok C, Frijstein M and van Trommel N:
Clinical presentation and diagnosis of gestational trophoblastic
disease. Best Pract Res Clin Obstet Gynaecol. 74:42–52. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chung JH, Yeo HJ, Cho HM, Jang JO, Ye BM,
Yoon G, Shin DH, Kim D and Cho WH: Treatment of pulmonary tumor
embolism from choriocarcinoma: Extracorporeal membrane oxygenation
as a bridge through chemotherapy. Cancer Res Treat. 49:279–282.
2017. View Article : Google Scholar : PubMed/NCBI
|