Introduction
Rhabdomyosarcoma (RMS), the most common soft-tissue
sarcoma in children and adolescents, originates from mesenchymal
cells and can be found anywhere in the body (1). RMS is most commonly located in the
head and neck region and genitourinary system, while it is rarely
observed in the pelvis (2). RMS
originating from urachal remnants has been reported in the
pediatric age group. Almost all cases reported in the literature
consist of children with Costello Syndrome (CS) who tend to have
malignant tumors (3). The medial
umbilical ligaments are paired structures related to the umbilical
arteries found either side of the median umbilical ligament. The
median and medial umbilical ligaments form a peritoneal depression
on each side of the urinary bladder referred to as the supravesical
fossae (4). RMS originating from
the umbilical remnants is an exceedingly rare entity, with limited
reported cases in the literature. To the best of our knowledge,
there is no case of medial ligament-originated RMS and also
non-syndromic in the literature review. The challenges of
identifying the tissue origin of the mass, especially in large
tumors, highlight the importance of a thorough exploration by the
surgeon during the procedure. In the present case, the surgeon
played a crucial role in determining the attachment of the mass to
tubular structures and therefore guiding the appropriate
intervention.
Case report
The current study reports the case of a previously
healthy 2-year-old girl who was the first child of healthy and
non-consanguineous parents. The prenatal follow-ups and birth
history were uneventful. The growth and development examinations
were appropriate for the patient's age. The patient was admitted to
the Emergency Department of Sisli Hamidiye Etfal Training and
Research Hospital (Istanbul, Turkey) in March 2020 with ongoing
abdominal pain for a week and abdominal distension, which were
considered to be due to weight gain for a while. The patient was
transferred to the Department of Pediatric Surgery, Sisli Hamidiye
Etfal Training and Research Hospital, after an 11-cm mass filling
the entire pelvis was identified on Doppler ultrasonography. The
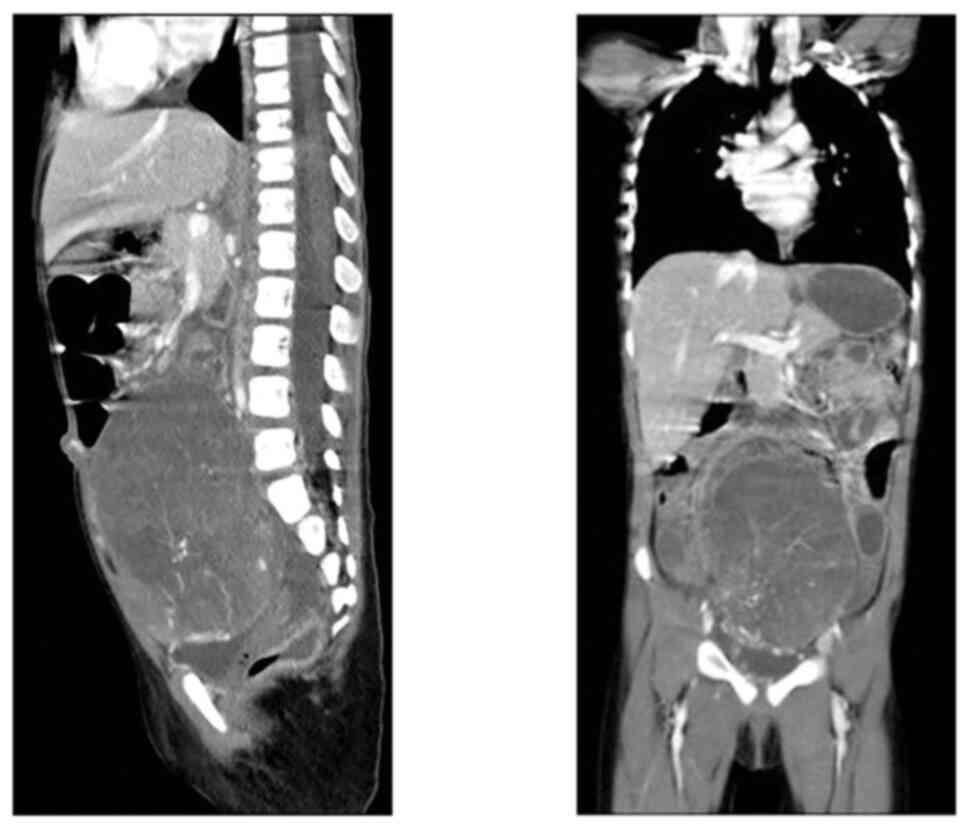
abdominal magnetic resonance imaging (MRI) (Fig. 1) revealed that the 11×8-cm solid
mass with smooth borders and possibly encapsulated was compressing
the sigmoid colon. The mass could not be separated from the bladder
and had high contrast, and it was reported that it could be either
an ovarian solid tumor or bladder-originated RMS. It was also
stated that the bilateral pelvic ectasia detected in the patient
was probably due to the compression of the mass. Tru-cut biopsy was
taken from the mass with an 18-gauge needle under ultrasonography
guidance. The pathological examination reported a small round-cell
malignant tumor. After immunohistochemical staining performed by
the Pathology Department, the patient was diagnosed with
embryonal-type RMS pathologically. As a result of the other
examinations performed by a pediatric oncologist, it was observed
that there was no metastasis. Since the primary mass was unsuitable
for complete resection, the patient was accepted as Intergroup RMS
Studies (IRS) Group III, and neoadjuvant chemotherapy was initiated
according to the COG D9803 protocol (5). The patient was re-evaluated after 4
sessions of neoadjuvant chemotherapy with VAC (vincristine,
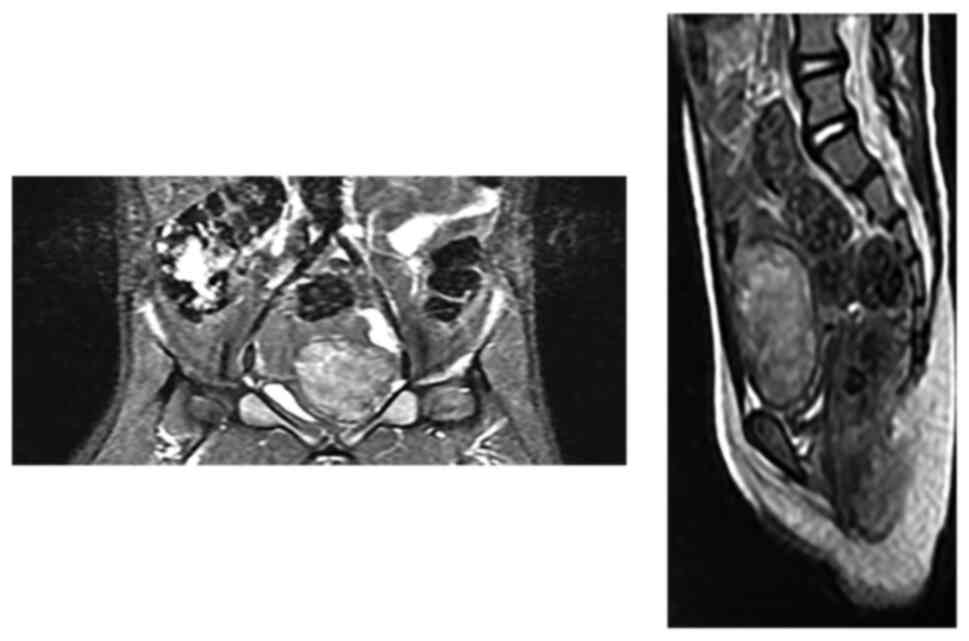
Actinomycin D and Cyclophosphamide). MRI images after the
chemotherapy are presented in Fig.
2.
The patient underwent a diagnostic cystoscopy before
surgery. It was observed that the bladder bulged inward from the
left lateral wall, and the bladder mucosa was normal. After
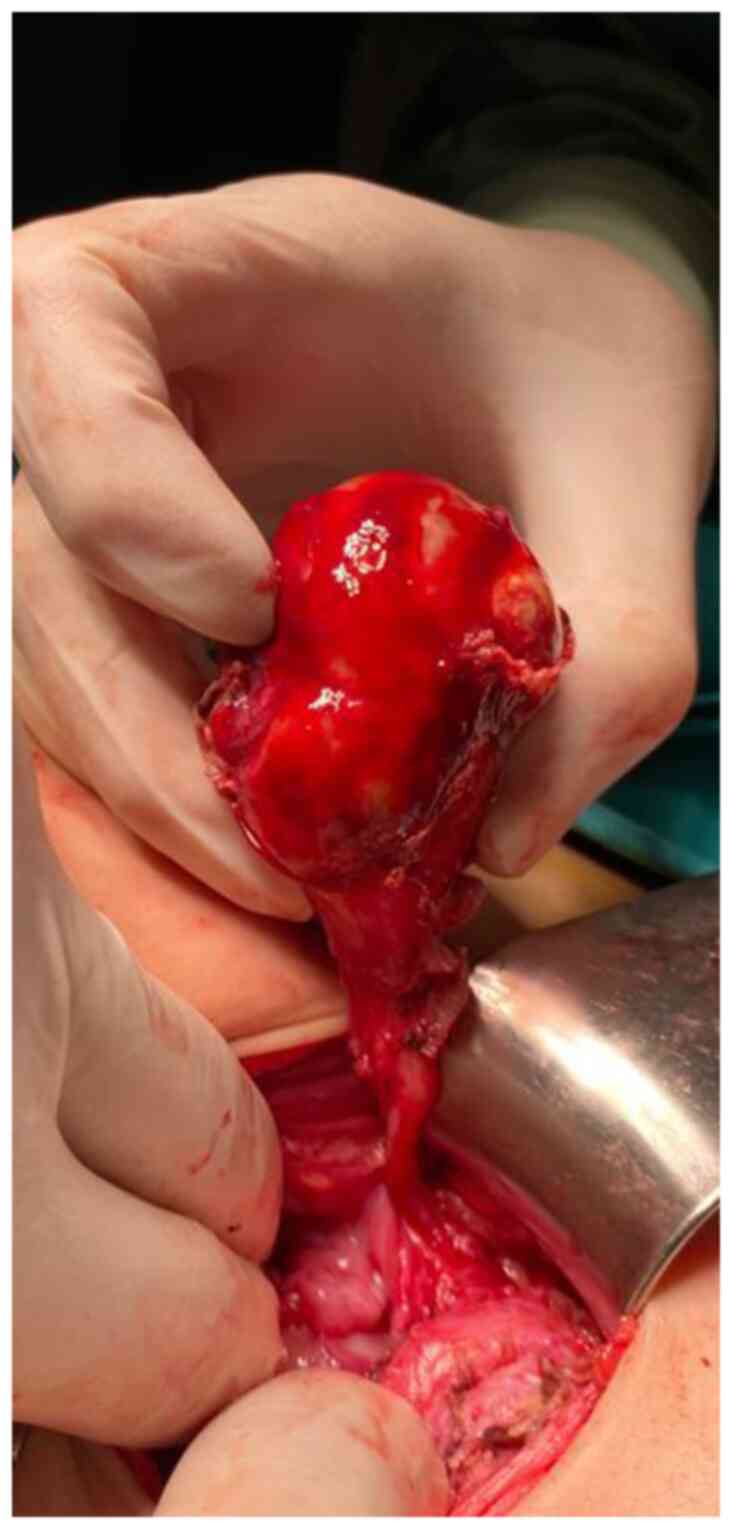
cystoscopy, the mass was freed from peritoneal adhesions on the
left lateral abdominal wall and the posterior wall of the bladder
by laparoscopic surgery. The pelvic end of the mass was observed to
continue with the left medial umbilical ligament. The left medial
umbilical ligament was ligated and cut, and the mass was excised
with a mini-pfannenstiel incision (Fig.
3). The oral intake of the patient was initiated on the first
day after surgery. The patient's wound remained clean, and was
transferred to the oncology service two days after the surgery. The
pathology result of the mass was reported as embryonal-type RMS. No
residual tumor was observed in the postoperative imaging. A total
of four sessions of the VAC chemotherapy protocol were continued
after surgery (0.05 mg/kg vincristine, 0.045 mg/kg Actinomycin D,
73 mg/kg Cyclophosphamide). Moreover, 50.4 Gy of radiotherapy was
applied to the tumor site and 18 Gy to the entire abdomen. After
completing her treatment, the patient had been followed up for 2
years and 3 months without any disease.
Discussion
RMS is the most common soft tissue sarcoma of
childhood. The incidence is 4 to 7 cases per 1 million children
younger than 15 years, and the peaks occur between the ages of 2
and 5 years (3). Similar to other
soft-tissue sarcomas, RMS originates most commonly from the
extremities, followed by the trunk wall, retroperitoneum,
genitourinary tract, head, and neck. Primary pelvic RMS is
extremely rare, included within the so-called ‘Other sites’ as
abdominal or thoracic locations (6). Primary pelvic RMS, mostly observed in
paediatric patient groups (7),
poses a great challenge for clinicians. Tumors in pelvic sites
often grow and spread locally without symptoms, and the exact site
of origin is challenging to determine at the time of diagnosis.
The umbilical artery is located within the umbilical
cord and carries deoxygenated blood from the fetus to the mother.
After the birth, the distal portion obliterates as the medial
umbilical ligament within a fold of the peritoneum. It lies lateral
to the median umbilical ligament (urachus). The persistent proximal
portion of the umbilical artery runs along the side wall of the
pelvis as the superior vesical artery (8). The varied morphology of the umbilical
ring and its surrounding structures are still being investigated to
deepen understanding of this complicated anatomical region
(9,10). Further studies may also shed light
on this unique site selection of RMS in these patients.
In the general population, umbilical ligament
malignant tumors are extremely rare, usually observed in adult
males, accounting for 0.01% of all tumors (11). On the other hand, umbilical ligament
RMS is mostly reported in paediatric patients with CS. In a
literature review published in 2017, the total number of cases of
RMS originating from the umbilical ligaments in paediatric patients
was only 17. A total of 15 cases originated from the urachus, and
two were from the medial umbilical ligaments. Both of these cases
were patients with CS (12,13). Previously, only 12 children with no
CS with urachus-originated RMS have been reported in the
literature. A case of RMS originating from the medial umbilical
ligament without CS has not been encountered in the literature;
therefore, the present case report was the first reported in this
respect.
CS is a rare neurodevelopmental disorder caused by
germline mutations in HRAS. Typical features include a
distinctive facial appearance, growth retardation, intellectual
disability, ectodermal, cardiac, musculoskeletal abnormalities and
cancer susceptibility. A total of ~10% of children with CS develops
cancer. A total of ~60% of these cancers are embryonal RMS and
RMSs, specifically originating from umbilical remnants in children
with CS. CS had been excluded from the present case report, and no
other genetic abnormalities were investigated.
The study presenting the largest series of pediatric
RMS from the urachal origin with 8 cases proved that urachal
localization had a worse prognosis (14). It has been argued that RMS
originating from the umbilical ligaments worsens the prognosis by
allowing metastasis at the time of diagnosis since it presents with
large asymptomatic masses in the preperitoneal area. Although the
present case report presented a mass reaching 11 cm in diameter,
there was no distant metastasis and local spread, and she remained
disease and complaint-free for 3 years after treatment. The other
two cases in the literature originating from the medial umbilical
ligament were also disease-free during their four-year follow-up.
Although the number of cases is too small to be argued about the
prognosis, it may be necessary to address the prognosis difference
between the two localizations despite the anatomical,
embryogenetic, and histological similarities. In order to evaluate
the prognosis of this localization, it is crucial to include rare
disease presentations in the literature. As the number of patients
and data increases, identifying these cases clearly instead of
classifying them within the large so-called ‘others’ group may help
the treatment management of these patients.
The organ or tissues from which the mass originates
may not be clear in large tumors. In the present case report, the
surgeon is the key person to determine which tubular structure the
mass was attached to after exploring and identifying other pelvic
tubular organs. This situation can be decided with the basic
surgical principle to completely or partially excise the organ
originating from the mass considered malignancy, as a result, to be
prepared for very rare situations that may be encountered for the
first time in the operating room. Therefore, it is vital that rare
disease presentations that cannot be serialized should be included
in the literature and that surgeons' attention should be drawn to
the subject.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MK conceived and designed the study, analyzed and
interpreted the results, and prepared the draft of the manuscript.
CAK obtained medical images and analysed the results. SO performed
data collection. DBG advised on patient treatment or analyzed
patient data. All authors reviewed the results, and read and
approved the final version of the manuscript. MK, CAK, SO and DBG
confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
Written informed consent was obtained from the legal
guardians of the patient for participation.
Patient consent for publication
Written informed consent was obtained from the legal
guardians of the patient for publication of the case information
and associated images.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
RMS
|
rhabdomyosarcoma
|
|
CS
|
Costello Syndrome
|
|
MRI
|
magnetic resonance imaging
|
References
|
1
|
Howlader N, Noone AM, Krapcho M, Miller D,
Bishop K, Kosary CL, Yu M, Ruhl J, Tatlovich Z, Mariotto A, Lewis
DR, et al: SEER Cancer Statistics Review, 1975–2014. National
Cancer Institute; Bethesda, MD, USA: https://seer.cancer.gov/csr/1975_2014/based on
November 2016 SEER data submission, posted to the SEER website.
April. 2017
|
|
2
|
Shern JF, Yohe ME and Khan J: Pediatric
Rhabdomyosarcoma. Crit Rev Oncog. 20:227–243. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gripp KW, Scot CI Jr, Nicholson L,
McDonald-McGinn DM, Ozeran JD, Jones MC, Lin AE and Zackai EH: Five
additional Costello syndrome pa=tients with rhabdomyosarcoma:
Proposal for a tumor screening protocol. Am J Med Genet. 108:80–87.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Moore KL, Dalley AF and Agur AMR:
Clinically Oriented Anatomy. 7th edition. Lippincott Williams &
Wilkins; Philadelphia, PA, USA: 2014
|
|
5
|
Arndt CA, Stoner JA, Hawkins DS, Rodeberg
DA, Hayes-Jordan AA, Paidas CN, Parham DM, Teot LA, Wharam MD,
Breneman JC, et al: Vincristine, actinomycin, and cyclophosphamide
compared with vincristine, actinomycin, and cyclophosphamide
alternating with vincristine, topotecan, and cyclophosphamide for
intermediate-risk rhabdomyosarcoma: Children's oncology group study
D9803. J Clin Oncol. 27:5182–5188. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rodary C, Flamant F and Donaldson SS: An
attempt to use a common staging system in rhabdomyosarcoma: A
report of an international workshop initiated by the International
Society of Pediatric Oncology (SIOP). Med Pediatr Oncol.
17:210–215. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hao Z and Yang S: Embryonal
rhabdomyosarcoma within abdomen and pelvis in an adult. Int J
Immunopathol Pharmacol. 32:20587384188067282018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shiffman MA: Pediatric Umbilical
Reconstruction: Principles and Techniques. August;2017.Doi:
10.1007/978-3-319-43890-0ISBN: 978-3-319-43888-7.
|
|
9
|
Oh CS, Won HS, Kwon CH and Chung IH:
Morphologic variations of the umbilical ring, umbilical ligaments
and ligamentum teres hepatis. Yonsei Med J. 49:1004–1007. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kim JH, Hayashi S, Jin ZW, Murakami G and
Rodríguez-Vázquez JF: Umbilical cord vessels other than the
umbilical arteries and vein: A histological study of midterm human
fetuses. Anat Cell Biol. 55:467–474. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fernández EM, Siverio NH, Almaraz RL,
Viota LM, Luis JR and Flores LD: Radical surgery and
IVA-chemotherapeutic regimen to treat embryonal rhabdomyosarcoma of
the urachus: Case report. Pediatr Hematol Oncol. 24:543–550. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bisogno G, Murgia A, Mammi I, Strafella MS
and Carli M: Rhabdomyosarcoma in a patient with
cardio-facio-cutaneous syndrome. J Pediatr Hematol Oncol.
21:424–427. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sánchez-Montenegro C, Vilanova-Sánchez A,
Barrena-Delfa S, Tenorio J, Santos-Simarro F, García-Miñaur S,
Lapunzina P and Martínez-Martínez L: Costello syndrome and
umbilical ligament rhabdomyosarcoma in two pediatric patients: Case
reports and review of the literature. Case Rep Genet.
2017:15876102017.PubMed/NCBI
|
|
14
|
Cheikhelard A, Irtan S, Orbach D,
Minard-Colin V, Rod J, Martelli H and Sarnacki S: Urachal
rhabdomyosarcoma in childhood: A rare entity with a poor outcome. J
Pediatr Surg. 50:1329–1333. 2015. View Article : Google Scholar : PubMed/NCBI
|