Introduction
Colon cancer (CC) is a malignant tumor originating
in the colon or rectum with a high case-fatality ratio with more
than 600,000 deaths annually (1),
and it accounts for ~6.1% of annual tumor incidences worldwide
(2–4). Radical surgery is the primary
treatment for CC in its early stages (5). Colon adenocarcinoma (COAD) is the most
common pathological type of CC (6).
Whether to use postoperative chemotherapy and targeted therapy to
inhibit tumor recurrence is still ambiguous. Recent research
indicated that the EP4 receptor was a promising targeted therapy in
CC (7). Furthermore, colon polyps
are cell clumps formed on the colon's mucosa and are considered
precursor lesions of CC (8,9). The colonic polyps may be categorized
as adenomas, hyperplastic polyps and inflammatory polyps (10). Adenomas appear to be the most common
type of colon polyp to develop into COAD (10), and surgical resection is the main
treatment method for early-stage COAD (11). However, the concurrence of
early-stage COAD and precancerous colon polyps is infrequent and
the optimal treatment method for such cases is still controversial.
The present study reported a rare case who had a bicentric lesion
of early-stage COAD and precancerous colon polyps and presented
with a postoperative fever along with anemia combined with
deep-wound dehiscence. Blood tests and pathological examinations of
the patient were performed at the laboratory of the present
hospital, and a whole-genome sequencing of the COAD sample was
performed. Based on the test results, the patient was treated with
low-dose and short-course prophylactic adjuvant therapy and gained
a good curative effect. Through this case, we aimed to offer a
diagnosis and treatment plan for this type of patient to better
guide clinical drug use in the future.
Case report
A 48-year-old woman first presented at the
Dongzhimen Hospital of Beijing University of Chinese Medicine
(Beijing, China) in October 2022 with complaints of intermittent
hematochezia, defecation urgency and liquid feces, but with no
distention or abdominal pain. The patient's information on the
medication and examination results follow the timeline from
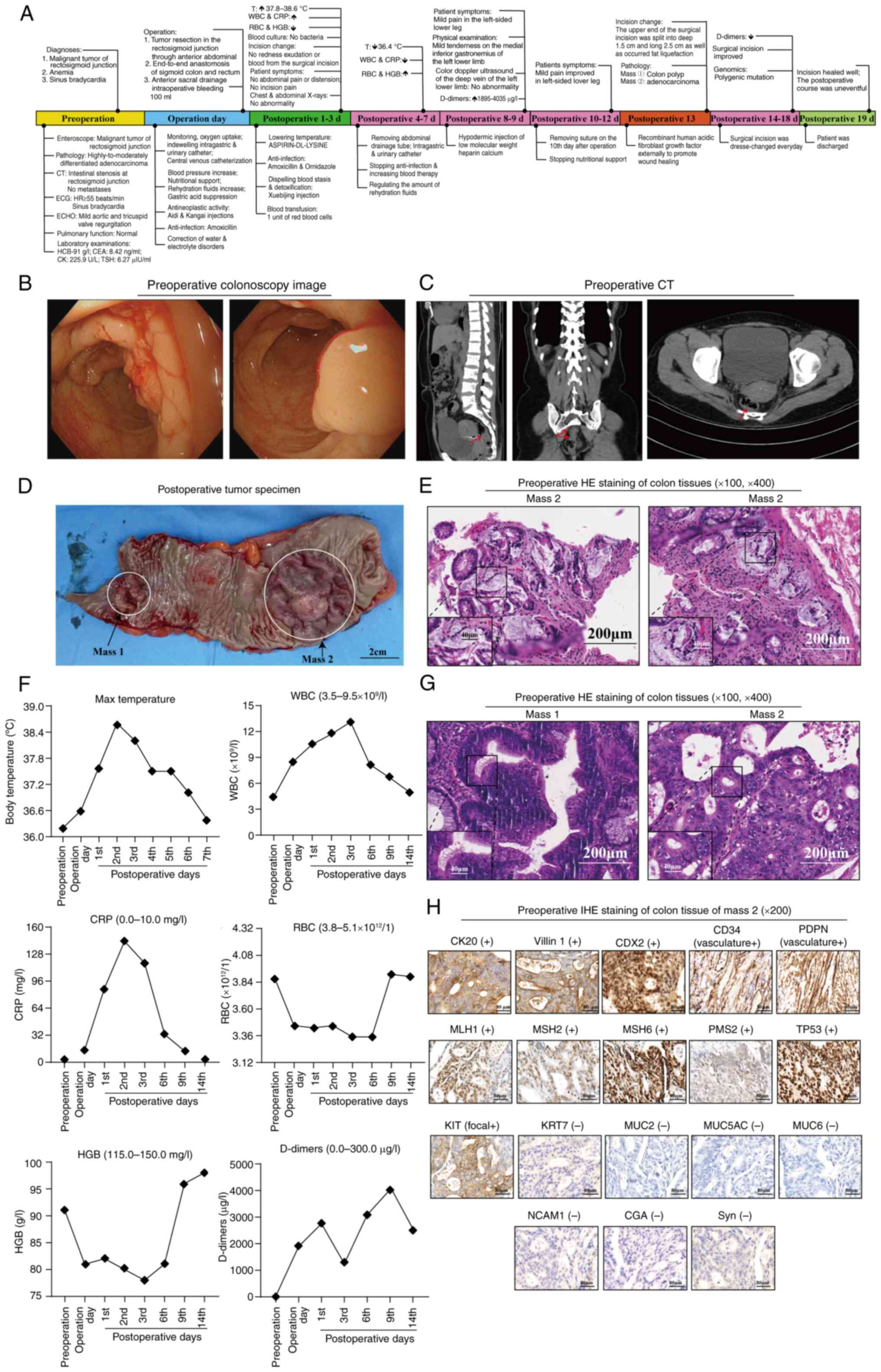
admission to discharge as a clinical course shown in Fig. 1A. Colonoscopy detection suggested an
irregular cauliflower-like mass in the rectosigmoid junction a
range of 15-19 cm from the anal verge occupying 2/5 of the
intestinal lumen (Fig. 1B).
Abdominal computed tomography (CT) revealed intestinal stenosis at
the rectosigmoid junction (Fig.
1C). Pathological examination of mass tissue obtained by
colonoscopy revealed highly-to-moderately differentiated
adenocarcinoma (Fig. 1E). Before
the operative day, laboratory testing showed a hemoglobin (HGB)
level of 91 g/l (normal range, 115.0–150.0 g/l) and a
carcinoembryonic antigen (CEA) level of 8.42 ng/ml (normal range,
0.0–4.5 ng/ml). The patient was diagnosed with a malignant tumor of
the rectosigmoid junction and anemia. On the 4th day after
admission, the patient received surgical treatment.
Intraoperatively, a tumor-like mass (Mass 2) was found at the
junction of the rectosigmoid colon with a length of 4 cm.
Furthermore, a 2-cm-long, firm mass (Mass 1) was palpitated 7 cm
above Mass 2. Next, a whole segment from the intestine including
Mass 1 and Mass 2 was removed, and end-to-end anastomosis as well
as anterior sacral drainage were performed. The bowel excision is
presented in Fig. 1D. After the
operation, the patient was monitored and was provided with oxygen,
indwelling intragastric and urinary catheters, central venous
catheterization, nutritional support, increased rehydration fluids.
Also, we gave the patient the dressing change once every other day.
At the same time, according to the whole genome sequencing (WES)
results of Mass 2, the patient was given the Aidi Injection
(12) [1,000 ml intravenous (IV)
drip once a day (qd)], a traditional Chinese patent medicine with
the function of the reducing swelling and dispersing, purchased
from Guizhou YiBai Pharmaceutical Co., Ltd., and the KangAi
Injection (13) (60 ml IV drip qd),
a traditional Chinese patent medicine with the function of
enhancing the body's immune function, purchased from ChangBaiShan
Pharmaceutical Co., Ltd. for antineoplastic activity. Amoxicillin
clavulanate potassium [0.3 g IV drip three times a day (tid),
purchased from North China Pharmaceutical Co., Ltd.] for
anti-infection, omeprazole sodium [40 mg IV drop bid twice a day
(bid) from Yangzhou Aaosaibo Pharmaceutical Co., Ltd.] for gastric
acid suppression and dopamine hydrochloride injection (100 mg IV
drop once, purchased from Beijing Double-Crane Pharmaceutical Co.,
Ltd.) for increasing blood pressure.
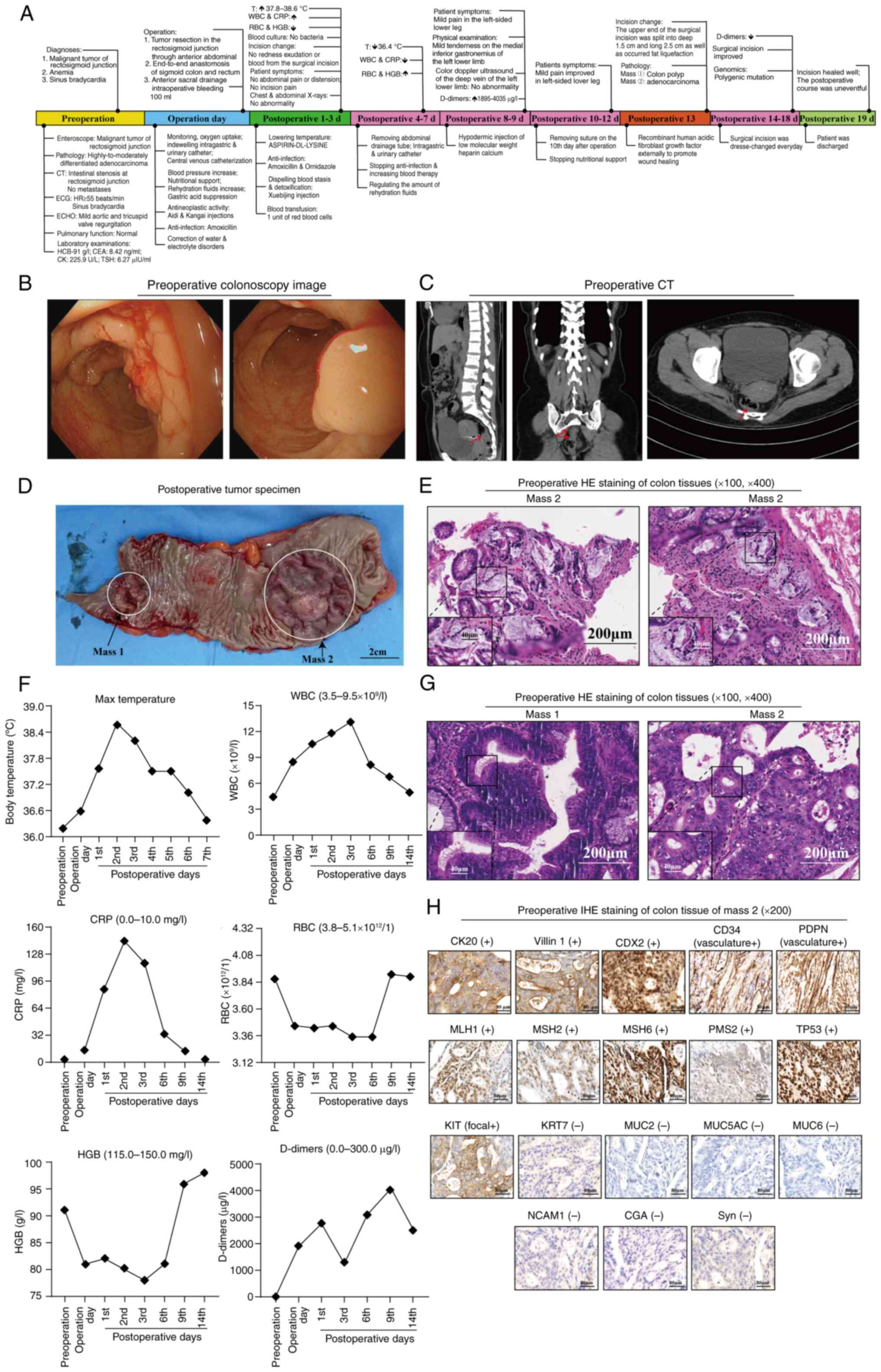 | Figure 1.Timeline and examination results for
the patient. (A) From the first visit at the hospital to the final
discharge, the patient's condition, tests and medication were
recorded. (B) Preoperative colonoscopy image. (C) Preoperative
abdominal CT scanning images (arrows indicate the tumors). (D)
Postoperative tumor specimen (scale bar, 2 cm). (E) Preoperative HE
staining of colon tissues (magnification, ×100 or ×400; scale bar,
200 or 40 µm). (F) Variation trend of laboratory indicators in the
patient, including maximum temperature, WBC, CRP, RBC, HGB and
D-dimer. (G) Postoperative HE staining of colon tissues
(magnification, ×100 or ×400; scale bar, 200 or 40 µm). (H)
Postoperative IHC staining of colon tissue of Mass 2
(magnification, ×200; scale bar, 80 µm). IHC, immunohistochemistry;
WBC, white blood cells; RBC, red blood cells; HGB, hemoglobin; CRP,
C-reactive protein; CT, computed tomography; T, temperature; d,
day; HE, hematoxylin and eosin; ECG, electrocardiogram; HR, heart
rate; ECHO, echocardiogram; CK, creatine kinase; CEA,
carcinoembryonic antigen; TSH, thyroid-stimulating hormone. |
Within 3 days after the operation, the patient's
body temperature increased continuously to range 37.8–38.6°C. The
patient had a fever, felt cold and had general fatigue.
Furthermore, on the first postoperative day, the white blood cells
(WBC) and C-reactive protein (CRP) both increased [WBC count,
10.5×109/l (normal range, 3.5–9.5×109/l); and
CRP, 87.49 mg/l (normal range, 0.0–10.0 mg/l)]. Furthermore, the
patient's HGB and red blood cells (RBC) were decreased [HGB, 82
g/l; and RBC, 3.43×1012/l (normal range,
3.8–5.1×1012/l)]. Blood culture tests for anaerobes and
aerobes were performed and the results indicated no bacterial
growth (Table I). The incision
healed well and the patient was given the transfusion therapy for 1
unit of RBCs, which the erythrocyte suspension, filtered from white
cell, coming from other healthy person, was injected into the
patient to treat anemia. Aspirin-DL-Lysine Injection for reducing
fever, amoxicillin clavulanate potassium [0.3 g IV drip tid,
purchased from North China Pharmaceutical Co., Ltd.] and Ornidazole
and Sodium Chloride Injection [0.5 g IV drip bid, purchased from
Sichuan Kelun Pharmaceutical Co., Ltd.] for anti-infection and
XueBiJing Injection [50 ml IV drip, only for two days, purchased
from Tianjin Hongri Pharmaceutical Co., Ltd.] with the function of
dispelling blood stasis and detoxification to reduce fever
(14). The next day, the patient's
body temperature gradually decreased to normal and the patient's
clinical manifestations, such as feeling cold and fatigue, improved
obviously (Fig. 1F).
 | Table I.Results of the blood laboratory
analysis. |
Table I.
Results of the blood laboratory
analysis.
|
|
| Time point |
|---|
|
|
|
|
|---|
|
|
|
|
| Postoperative
days |
|---|
|
|
|
|
|
|
|---|
| Item | Reference range | Preoperation | Operation day | 1st | 2nd | 3rd | 6th | 9th | 14th |
|---|
| WBC,
×109/l | 3.50–9.50 | 4.40 | 8.49 | 10.50↑ | 11.70↑ | 13.10↑ | 8.20 | 6.70 | 5.10 |
| RBC,
×1012/l | 3.80–5.10 | 3.88 | 3.45↓ | 3.43↓ | 3.45↓ | 3.35↓ | 3.35↓ | 3.91 | 3.89 |
| HGB, g/l | 115.00–150.00 | 91.00↓ | 81.00↓ | 82.00↓ | 80.00↓ | 78.00↓ | 81.00↓ | 96.00↓ | 98.00↓ |
| HCT, % | 35.00–45.00 | 28.50↓ | 25.50↓ | 24.90↓ | 24.90↓ | 24.20↓ | 24.60↓ | 29.40↓ | 29.80↓ |
| MCV, fl | 82.00–100.00 | 73.40↓ | 74.10↓ | 72.80↓ | 72.10↓ | 72.30↓ | 73.60↓ | 75.20↓ | 76.70↓ |
| MCH, pg | 27.00–34.00 | 23.40↓ | 23.50↓ | 23.90↓ | 23.20↓ | 23.40↓ | 24.10↓ | 24.40↓ | 25.10↓ |
| MCHC, g/l | 316.00–354.00 | 319.00 | 317.00 | 328.00 | 321.00 | 323.00 | 327.00 | 325.00 | 328.00 |
| RDW-CV, % | 10.00–20.00 | 16.60 | 15.10 | 16.60 | 16.60 | 16.80 | 17.10 | 18.30 | 21.40 ↑ |
| PLT,
×109/l | 125.00–350.00 | 342.00 | 213.00 | 213.00 | 196.00 | 200.00 | 233.00 | 324.00 | 373.00↑ |
| MPV, fl | 6.80–13.50 | 8.10 | 9.50 | 8.90 | 9.10 | 9.60 | 9.70 | 9.50 | 9.10 |
| PCT, % | 0.11–0.27 | 0.28↑ | 0.20 | 0.19 | 0.18 | 0.19 | 0.23 | 0.31↑ | 0.34↑ |
| PDW, % | 9.00–17.00 | 16.20 | 15.90 | 16.70 | 16.70 | 16.80 | 16.70 | 16.60 | 16.40 |
| NE, % | 50.00–70.00 | 57.70 | 89.20↑ | 91.30↑ | 89.70↑ | 89.40↑ | 74.70↑ | 69.00 | 60.30 |
| NE#,
×109/l | 1.80–6.70 | 2.50 | 7.57↑ | 9.60↑ | 10.50↑ | 11.70↑ | 6.10 | 4.60 | 3.10 |
| LY, % | 20.00–40.0 | 31.70 | 6.70↓ | 4.20↓ | 4.80↓ | 5.10↓ | 13.60↓ | 19.20↓ | 29.20 |
| LY#,
×109/l | 0.70–3.80 | 1.40 | 0.57↓ | 0.40↓ | 0.60↓ | 0.70 | 1.10 | 1.30 | 1.50 |
| MO, % | 0.00–13.00 | 9.10 | 3.40 | 4.20 | 4.70 | 4.30 | 7.50 | 8.20 | 6.00 |
| MO#,
×109/l | 0.00–1.20 | 0.40 | 0.29 | 0.40 | 0.50 | 0.60 | 0.60 | 0.60 | 0.30 |
| EO, % | 0.50–5.00 | 0.80 | 0.60 | 0.20↓ | 0.60 | 0.60 | 3.70 | 3.20 | 3.80 |
| EO#,
×109/l | 0.02–0.50 | 0.00↓ | 0.05 | 0.00↓ | 0.10 | 0.10 | 0.30 | 0.20 | 0.20 |
| BA, % | 0.00–2.00 | 0.70 | 0.10 | 0.10 | 0.20 | 0.60 | 0.50 | 0.40 | 0.70 |
| BA#,
×109/l | 0.00–0.20 | 0.00 | 0.01 | 0.00 | 0.00 | 0.10 | 0.00 | 0.00 | 0.00 |
| CRP, mg/l | 0.00–10.00 | 1.67 | 13.81↑ | 87.49↑ | 143.21↑ | 117.21↑ | 32.90↑ | 11.17↑ | 1.59 |
| Blood culture
(anaerobic bacteria) | Positive | / | / |
|
| Negative |
|
|
| Blood culture
(aerobic bacteria) | Positive | / | / |
|
| Negative |
|
|
Within 9 days after the operation, the patient
complained of mild pain in the left-sided lower leg, and serum
D-dimers increased (4,035 µg/l; normal range, 0.0–300.0 µg/l) on
the ninth postoperative day. The patient was given a hypodermic
subcutaneou sinjection of low molecular weight heparin calcium
4,100 IU qd for 5 days. D-dimers of the patient were decreased to
2,346 µg/l on the 14th postoperative day (Fig. 1F) and the patient's left-sided lower
leg pain improved. The suture was removed on the 10th postoperative
day. After another three days, it was discovered that the upper end
of the patient's surgical incision had split to the anterior rectus
abdominis sheath with a depth of incision of ~1.5 cm and a length
of ~2.5 cm, and fat liquefaction was present according to the
measured length of the swab and visual observation (data not
shown). The patient was externally provided with lyophilized
recombinant human acidic fibroblast growth factor (application as a
spray qd; Shanghai Tengrui Pharmaceutical Co., Ltd.) and dressing
change every day to promote wound healing.
For the pathological examination for the colon
lesions, after treatment with 10% dimethylbenzene for 24 h, the
lesion tissues were mounted and resected to small pieces that were
added into a cassette for dehydration and embedding in paraffin.
The paraffin-embedded lession tissues were then sectioned at 4-µm
thickness. Next, the samples were stained with hematoxylin-eosin
for histopathological assessment. Finally, light microscopy was
used to observe the sections. The pathological examination results
were as follows: The resected bowel was 17 cm in length and 7 cm in
diameter, and two protuberant masses were observed in it. Mass 1
was low-grade tubulovillous adenoma with focal high-grade
intraepithelial neoplasia and Mass 2 was protuberant moderately
differentiated adenocarcinoma, invading the shallow muscle layer
(Fig. 1G).
Mass 2 was further analyzed by immunohistochemical
(IHC) staining. The IHC staining was peformed by a third-party
company, Servicebio, using an IHC kit (cat. no. PV-9001; Zhongshang
Goldenbridge-Bio). Paraffin-embedded colonic mucosa sections were
dewaxed and re-hydrated. Antigen retrieval was conducted using EDTA
or sodium citrate at 98°C for 20 min. Endogenous peroxidase was
blocked with goat serum (Biotopped). Sections were incubated
overnight in a humidified chamber with primary antibody to
cancer-related genes, followed by biotinylated secondary antibody
incubation. Subsequently, diaminobenzidine (DAB) chromogenic
reaction was performed using freshly prepared DAB color developing
solution. The sections were counterstained with hematoxylin,
dehydrated, fixed and mounted. Finally, light microscopy was used
to observe the sections with ×200 magnification. IHC results were
as follows: Tumor-related genes such as cytokeratin 20, Villin 1,
caudal type homeobox 2, CD34 (vasculature), podoplanin
(vasculature), mutL homolog 1, mutS homolog 2 (MSH2), MSH6, PMS1
homolog 2, mismatch repair system component, tumor protein p53
(TP53) and KIT proto-oncogene, receptor tyrosine kinase (focal)
were positive, while keratin 7, mucin 2, oligomeric
mucus/gel-forming (MUC2), MUC5AC, MUC6, neural cell adhesion
molecule 1, glycoprotein hormones, α polypeptide and synapsin were
negative (Fig. 1H). All of the
above-mentioned markers were related to promoting the proliferation
of colon cancer cells and increase the degree of malignancy of
tumors, which further support the pathological diagnosis of
COAD.
The results of the WES (performed by the Life
Healthcare Group Ltd., CN) of Mass 2 showed that the tumor was of
the microsatellite stable type, which is not sensitive to single
immunotherapy based on immune checkpoint inhibitors (15). Meanwhile, substitution for aspartic
acid to glycine at codon 13 of the KRAS proto-oncogene, GTPase
(KRAS-G13D), substitution for alanine to glycine at codon 12 of the
KRAS proto-oncogene, GTPase (KRAS-G12A), substitution for lysine to
glutaic acid at codon 542 of the
phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit α
(PIK3CA-E542K), substitution for histidine to arginine at codon 202
of the GNAS complex locus (GNAS-R202H), substitution for Lysine to
termination codon at codon 1370 of the APC regulator of WNT
signaling pathway (APC-K1370*), substitution for aspartic acid to
glycine at codon 245 of the TP53 (TP53-G245D), substitution for
serine to glycine at codon 245 of the TP53 (TP53-G245S) and
non-frameshift deletion mutations from codon 117 Proline to codon
182 Cysteine of the tumor protein P53 (TP53-P177_C182del) were
found in the analysis of tumor targeting/drug resistance-related
variant genes. Considering that KRAS and TP53 had gene mutations,
but other immunotherapy-related genes exhibited no change,
antiangiogenic targeted therapy and chemotherapy drugs should be
used but not immunotherapy (16).
The final diagnosis for the patient was rectosigmoid
junction adenocarcinoma (T2N0M0 stage I) and precancerous colon
polyps. According to the above results, the patient was next
treated with chemotherapy and targeted therapy to prevent tumor
recurrence. The therapeutic schedule was bevacizumab 300 mg day (D)
1 (IV drip), irinotecan hydrochloride 100 mg D1 (IV drip) and
capecitabine (1.5 g per os bid) D1-D14. A total of four
cycles of the above-mentioned regimen were used, with treatments
repeated every 3 weeks. During follow-up for 8 months, the patient
was managed by regular review of blood routine and tumor markers
and followed up by phone and by appointment, and the results showed
that no tumor recurrence was found and CEA decreased continuously
to the normal level, and the level of WBC, CRP, RBC and HGB also
became normal in July 2023.
Discussion
In the present study, a noteworthy bicentric lesion
case was described, with an early-stage COAD combined with
precancerous colon polyps, which was treated with low-dose and
short-course prophylactic adjuvant therapy. This special case and
the corresponding therapy could guide clinical drug use in the
future. Furthermore, the patient presented with a postoperative
fever. Through investigation in all aspects, the cause of the
patient's postoperative fever was identified as anemia with deep
wound dehiscence secondary infection. The present study provides a
feasible treatment idea for the clinical solution of postoperative
complications.
Postoperative fever is a common symptom in CC
patients with the underlying causes being infection, anemia,
anastomotic leakage, and drug side effects (17,18).
Usually, inflammation-induced postoperative fever presents as a
high fever, with shallow wound incisional dehiscence, suppuration,
fat liquefaction and other clinical manifestations (17,18),
and postoperative fever caused by anemia is a low fever with a body
temperature <38°C (19). In the
present study, the patient's body temperature increased
continuously to range 37.8–38.6°C, which was between low and high
fever; furthermore, the WBC count and CRP both increased, which are
indicators of inflammation. Thus, the patient of the present study
was given antibiotics, such as amoxicillin for anti-inflammation
and XueBiJing injections to dispel blood stasis and for
detoxification. In addition, the patient received transfusion
therapy, in which the erythrocyte suspension filtered from white
blood cells from a healthy donor was injected into the patient to
treat anemia. Subsequently, the patient's body temperature
decreased to a range of 36.4–37.5°C, and in addition, the WBCs and
level of CRP decreased. Finally, the reason for postoperative fever
was found to be that the upper end of the patient's surgical
incision was split to the anterior rectus abdominis sheath with a
depth of 1.5 cm and a length of 2.5 cm when the suture was removed
on the 10th postoperative day, leading to secondary infection. The
split incision as well as fat liquefaction was noted 3 days after
the suture had been removed. This could explain why the patient had
a persistently higher body temperature and level of WBC and CRP,
although the incision healed well. It was finally concluded that
the reasons were anemia with deep wound dehiscence and secondary
infection.
For the treatment of early-stage COAD, researchers
advised that middle-aged patients with stage I disease receive
postoperative chemotherapy (20,21).
Traditional Chinese medicine or other auxiliary therapies can
inhibit the recurrence or even canceration of colon polyps,
particularly precancerous polyps (22). However, to the best of our
knowledge, there are few reports of bicentric lesions of
early-stage COAD and precancerous colon polyps, and whether to use
adjuvant therapy is still controversial. In this case, the patient
not only had a bicentric lesion, but also had mutations in the
genes KRAS, PIK3CA, GNAS, APC and TP53. Thus, the patient was given
low-dose and short-course bevacizumab combined with hydrochloride
and capecitabine after the operation.
Although the etiology of postoperative fever was
finally confirmed in this case and prophylactic adjuvant therapy
was given, the study has several limitations. First, the patient's
anemia should have been corrected preoperatively. Second, abdominal
ultrasonography should have been performed to determine whether
deep wound dehiscence and secondary infection had occurred. Third,
detailed preoperative colonoscopy and detailed medical
communication between doctors are crucial. At last, the long-term
outcome of postoperative low-dose and short-course adjuvant therapy
is still unclear.
In conclusion, the cause of the patient's
postoperative fever was anemia with deep wound dehiscence and
secondary infection. Low-dose and short-course prophylactic
adjuvant therapy is feasible for early-stage COAD with precancerous
colon polyps.
Acknowledgements
Not applicable.
Funding
The research was supported by the Ningxia Hui Autonomous Region
Clinical Medical Research Center for Anorectal Diseases (Integrated
Chinese and Western Medicine; grant no. 2022LCZX0013) and the
Science and Technology Innovation Team of Yinchuan City (grant no.
2022CXTD15).
Availability of data and materials
The WES data generated in the present study may be
found in the Mendeley Data database at the following URL:
(https://data.mendeley.com/datasets/jmtpwdb6vv/1). The
data generated in the present study may be requested from the
corresponding author.
Authors' contributions
MYW and XBZ wrote and revised the manuscript. SXZ,
YY, ZMG, MYW and XBZ initiated and designed the project. XXF, LJ,
HBZ, BXT, YJL, JCZ and LYS collected and organized all data. MYW,
JLL and YFW drew and analyzed the images. All authors reviewed and
edited the manuscript. All authors have read and approved the final
manuscript. YY and SXZ checked and confirmed the authenticity of
the raw data.
Ethics approval and consent to
participate
Ethics approval was provided by the Ethics Committee
of Dongzhimen Hospital Affiliated of the Beijing University of
Chinese Medicine (Beijing, China; approval no. 2023DZMEC-048).
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of their clinical details and
images.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
CC
|
colon cancer
|
|
CEA
|
carcinoembryonic antigen
|
|
COAD
|
colon adenocarcinoma
|
|
CRP
|
C-reactive protein
|
|
CT
|
computed tomography
|
|
DAB
|
diaminobenzidine
|
|
EDTA
|
ethylene diamine tetraacetic acid
|
|
HE
|
hematoxylin-eosin
|
|
HGB
|
hemoglobin
|
|
IHC
|
immunohistochemistry
|
|
RBC
|
red blood cell
|
|
WBC
|
white blood cell
|
|
KRAS
|
KRAS proto-oncogene, GTPase
|
|
PIK3CA
|
phosphatidylinositol-4,5-bisphosphate
3-kinase catalytic subunit α
|
|
GNAS
|
GNAS complex locus
|
|
APC
|
APC regulator of WNT signaling
pathway
|
|
TP53
|
tumor protein 53
|
References
|
1
|
Zhou Y, Yang J, Zhang Q, Xu Q, Lu L, Wang
J and Xia W: P4HB knockdown induces human HT29 colon cancer cell
apoptosis through the generation of reactive oxygen species and
inactivation of STAT3 signaling. Mol Med Rep. 19:231–237.
2019.PubMed/NCBI
|
|
2
|
Siegel RL, Miller KD, Fuchs HE and Jemal
A: Cancer statistics, 2022. CA Cancer J Clin. 72:7–33. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Allison JE: Colorectal cancer screening
guidelines: The importance of evidence and transparency.
Gastroenterology. 138:1648–1652.e2. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Labianca R, Beretta GD, Kildani B, Milesi
L, Merlin F, Mosconi S, Pessi MA, Prochilo T, Quadri A, Gatta G, et
al: Colon cancer. Crit Rev Oncol Hematol. 74:106–133. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhang Z, Qian W, Wang S, Ji D, Wang Q, Li
J, Peng W, Gu J, Hu T, Ji B, et al: Analysis of lncRNA-Associated
ceRNA network reveals potential lncRNA biomarkers in human colon
adenocarcinoma. Cell Physiol Biochem. 49:1778–1791. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Karpisheh V, Joshi N, Zekiy AO, Beyzai B,
Hojjat-Farsangi M, Namdar A, Edalati M and Jadidi-Niaragh F: EP4
receptor as a novel promising therapeutic target in colon cancer.
Pathol Res Pract. 216:1532472020. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim YJ, Bae JP, Chung JW, Park DK, Kim KG
and Kim YJ: New polyp image classification technique using transfer
learning of network-in-network structure in endoscopic images. Sci
Rep. 11:36052021. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Suzuki T, Kitagawa Y, Nankinzan R and
Yamaguchi T: Usefulness of cold polypectomy under linked color
imaging. Endosc Int Open. 8:E87–E91. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Suh SS, Kim TK, Kim JE, Hong JM, Nguyen
TTT, Han SJ, Youn UJ, Yim JH and Kim IC: Anticancer activity of
ramalin, a secondary metabolite from the antarctic lichen ramalina
terebrata, against colorectal cancer cells. Molecules. 22:13612017.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhao L and Li Y: Application of
dexmedetomidine combined with sufentanil in colon cancer resection
and its effect on immune and coagulation function of patients.
Oncol Lett. 20:1288–1294. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Song J, Zhou H, Sun C, Jiao L, Gong Y, Yao
J and Xu L: Combination of Brucea javanica oil emulsion and Aidi
injection associated with the long-term survival of a patient with
colon cancer and lung metastases post-chemotherapy: A case report.
Oncol Lett. 28:3612024. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen Y, Hu Z, Jiang J, Liu C, Gao S, Song
M and Hang T: Evaluation of pharmacological and pharmacokinetic
herb-drug interaction between irinotecan hydrochloride injection
and Kangai injection in colorectal tumor-bearing mice and healthy
rats. Front Pharmacol. 14:12820622023. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Liang SB, Zhang YY, Shen C, Liang CH, Lai
BY, Dai N, Li YQ, Tian ZY, Zhang XW, Jiang Y, et al: Chinese herbal
medicine used with or without conventional western therapy for
COVID-19: An evidence review of clinical studies. Front Pharmacol.
11:5834502021. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhao W and Huang Z: Durable responses to
tislelizumab plus fruquintinib and radiotherapy in refractory
microsatellite stable metastatic colorectal cancer: A case report.
Am J Transl Res. 15:2918–2925. 2023.PubMed/NCBI
|
|
16
|
Wang Z, Piha-Paul S, Janku F, Subbiah V,
Shi N, Gong J, Wathoo C, Shaw K, Hess K, Broaddus R, et al:
Antiangiogenesis and gene aberration-related therapy may improve
overall survival in patients with concurrent KRAS and TP53 hotspot
mutant cancer. Oncotarget. 8:33796–33806. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chiarello MM, Fransvea P, Cariati M, Adams
NJ, Bianchi V and Brisinda G: Anastomotic leakage in colorectal
cancer surgery. Surg Oncol. 40:1017082022. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chen JS, Changchien CR and Tang R:
Postoperative fever and survival in patients after open resection
for colorectal cancer: A long-term follow-up study of 2,311
prospectively enrolled patients. Dis Colon Rectum. 51:1649–1655.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Knuesel SJ, Guseh JS II, Karp Leaf R,
Ciaranello AL and Eng GM: Case 6-2018: A 35-year-old woman with
headache, subjective fever, and anemia. N Engl J Med. 378:753–760.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wu C: Systemic therapy for colon cancer.
Surg Oncol Clin N Am. 27:235–242. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Manjelievskaia J, Brown D, McGlynn KA,
Anderson W, Shriver CD and Zhu K: Chemotherapy use and survival
among young and middle-aged patients with colon cancer. JAMA Surg.
152:452–459. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wu H, Huang Y, Yang L, Su K, Tian S, Chen
X, Li S and Liu W: Effects of Jianpi Lishi Jiedu granules on
colorectal adenoma patients after endoscopic treatment: Study
protocol for a randomized, double-blinded, placebo-controlled
clinical trial. Trials. 23:3452022. View Article : Google Scholar : PubMed/NCBI
|