Introduction
The elbow is an uncommon site for malignant bone
tumors. Since the introduction of limb-spearing surgery and
adjuvant chemotherapy, reconstruction of the elbow after resection
of malignant tumors has became an alternative to amputation.
However, surgical options for reconstruction of the elbow are
limited and technically challenging (1–6).
Arthrodesis of the elbow results in restricted
motion and excisional arthroplasty may result in instability
(7). Allografts have been used, but
with a high complication rate (8).
The case of a man with osteosarcoma of the proximal
ulna that was excised and reconstructed using a combination of
extracorporeally irradiated osteochondral autograft and free
vascularised fibula is presented. He has remained free of disease
with excellent function of the affected area 10 years after
surgery.
Case Report
A 48-year old male was referred to us with an
enlarged hard mass in his left elbow. It had been present for 6
months. A physical examination revealed a bony hard lump, 5 × 6 cm
in size, in the posterior aspect of the proximal forearm.
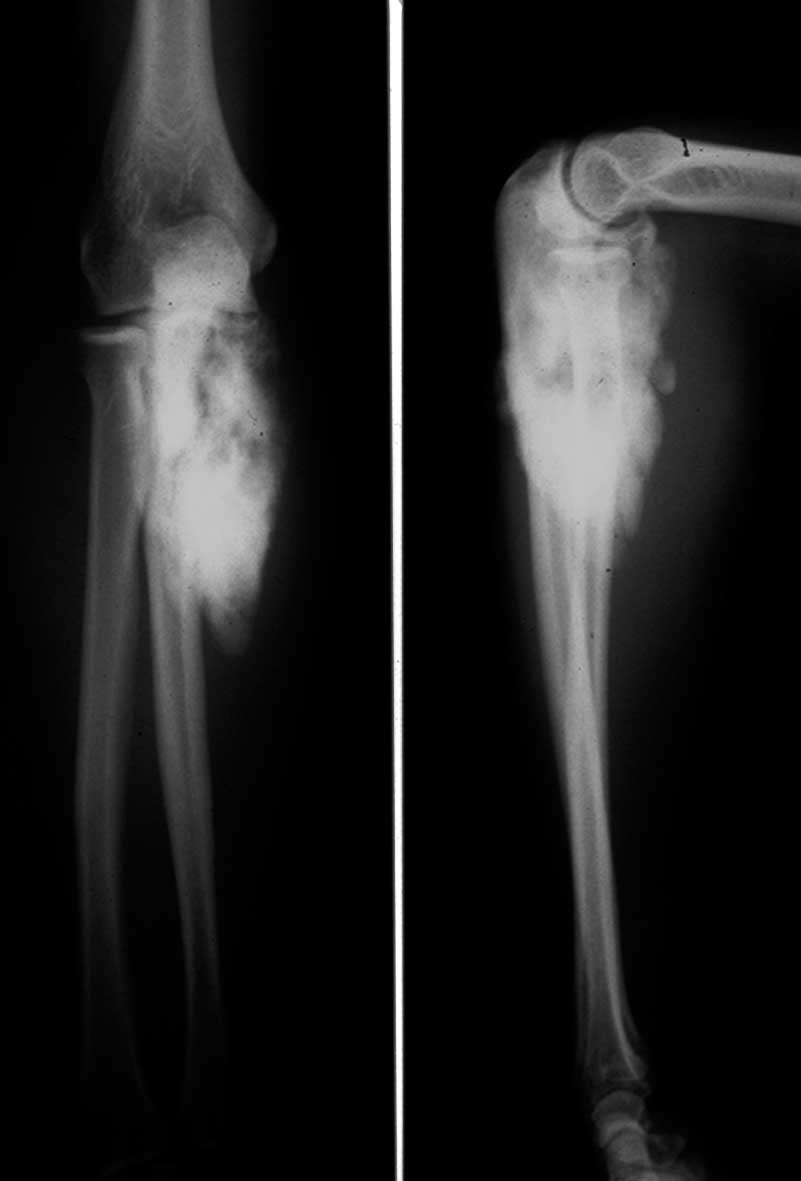
Radiography and CT showed a heavily mineralized tumor of the
proximal ulna (Fig. 1). Magnetic
resonance imaging demonstrated an intramedullary tumor extending to
the posterior soft tissue. Open biopsy was perfromed and low-grade
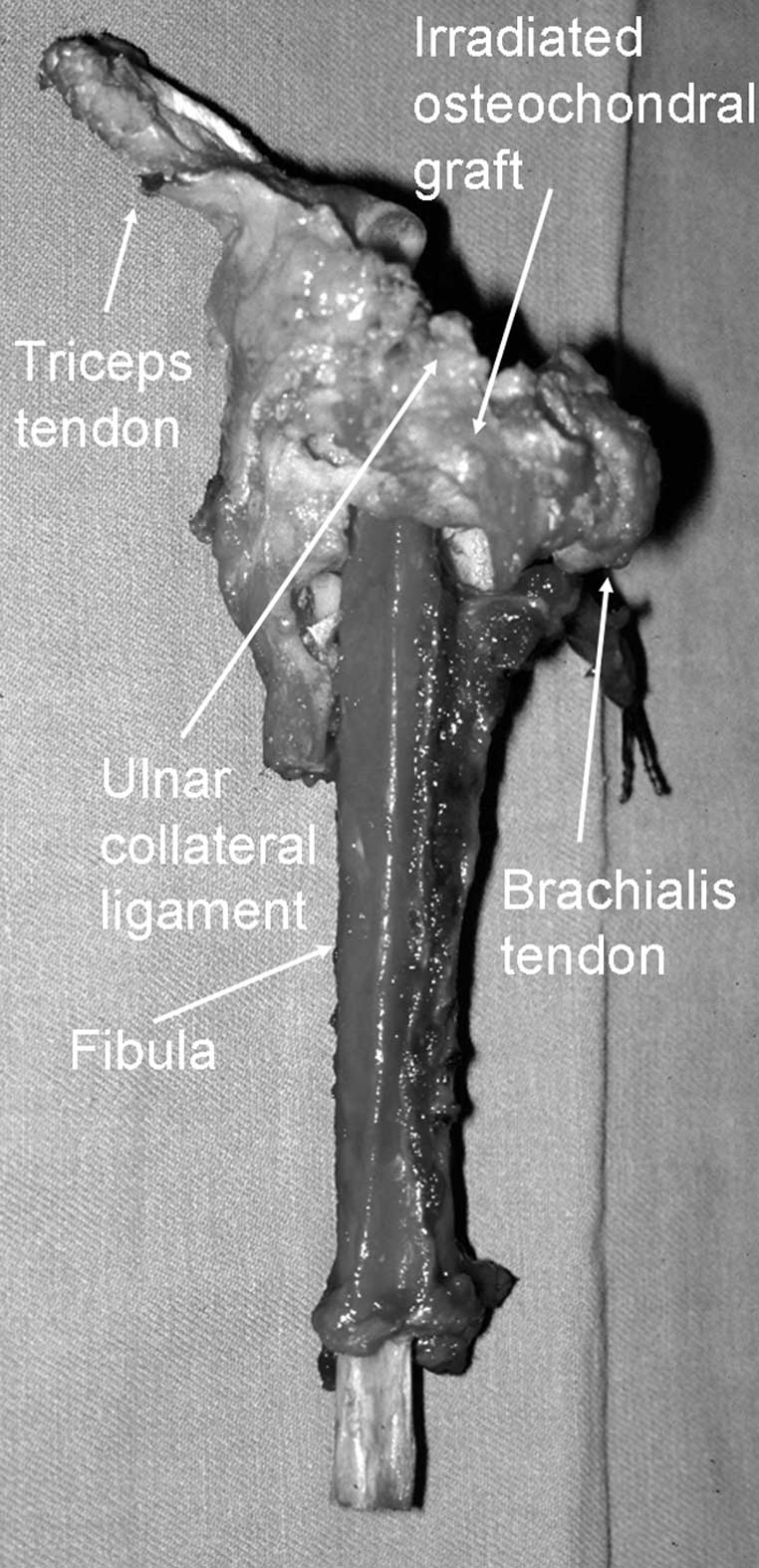
osteosarcoma was diagnozed. During surgery, the left proximal ulna
was approached via anterior and posterior incisions. After
osteotomy of the mid shaft, 13 cm of the proximal ulna were
resected along with the flexor digitorum profundus muscle, the
flexor carpi ulnaris muscle, ulnar collateral ligament and ulnar
half of annular ligament. Tendinous insertions of the brachialis
and triceps were transected. Resected ulna and soft tissue were
placed in a small plastic box filled with saline, and the box was
administered with a single dose of 60 Gy. The irradiated graft was
returned to the operating theater. The distal 7 cm of the resected
ulna was osteotomized and the intramedullary tumor of the olecranon
was curetted. The vascularised fibula was inserted into the
medullary cavity of the olecranon and fixed with screws. The
ligaments and tendinous insertion of the brachialis and triceps
were sutured. Then, distal osteosynthesis was carried out with a
plate and screws. The donor peroneal vessels were side-anastomosed
to the ulnar vessels (Fig. 2).
Fixation with a cast was applied for 4 weeks and an additional
functional hinged-brace was applied for 3 months. Histological
examination of the resected tumor showed low-grade osteosarcoma
with small foci of high-grade components. The patient was given 3
courses of chemotherapy consisting of ifosfamide and doxorubicin.
The iliac cancellous bone graft for proximal non-union site was
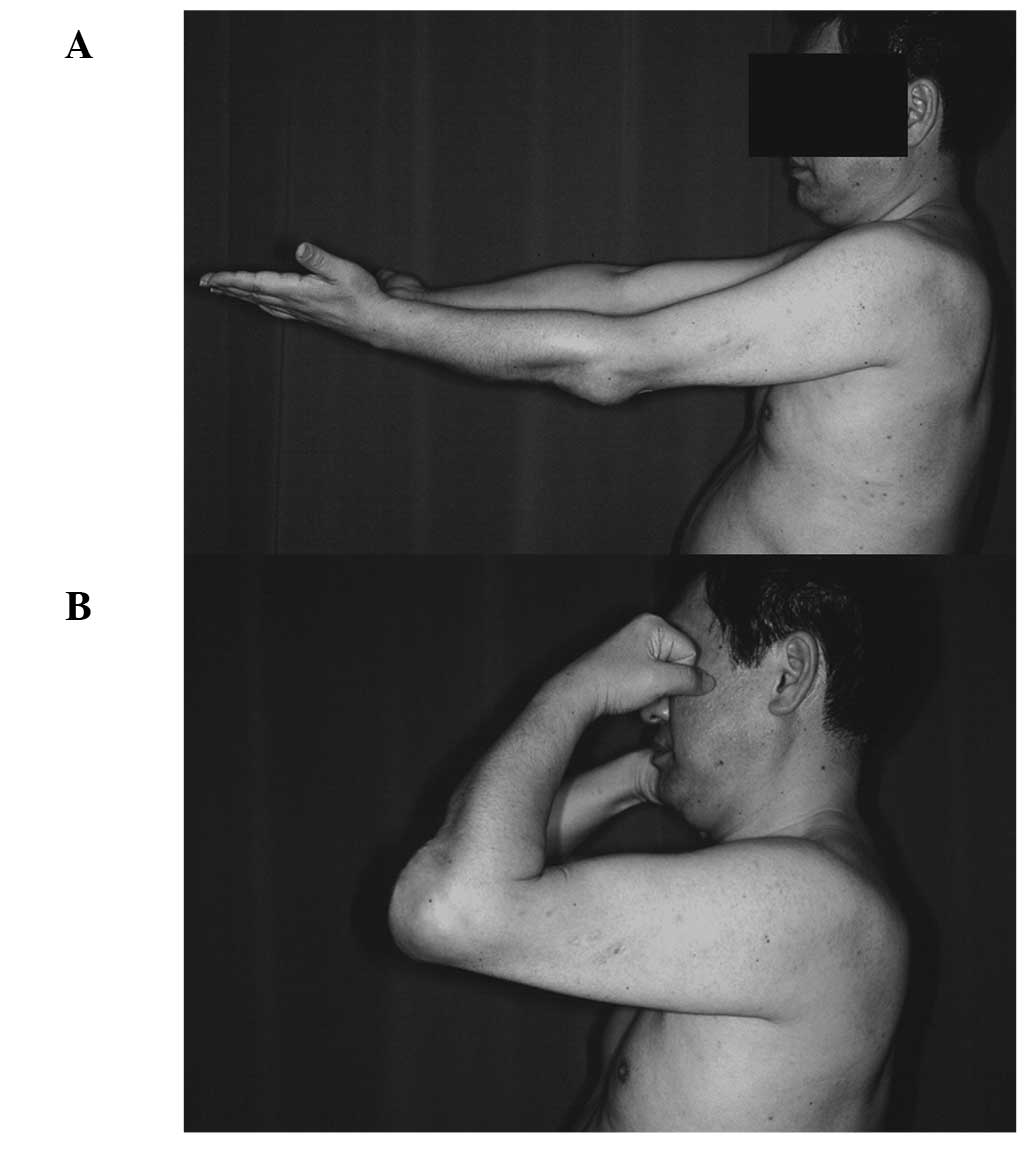
added 16 months after the initial surgery. Ten years after the
initial surgery the patient has recuperated and shows no evidence
of disease (Fig. 3). The appearance
and elbow function are excellent (extension-flexion, −20/120;
pronation, 80; supination 10) (Fig.
4). The patient is able to play golf with no lateral
instability or pain of the elbow joint.
Discussion
Although satisfactory results of endoprosthetic
reconstruction for elbow tumors have been reported, such studies
mainly described humeral bone tumors. Endoprosthetic reconstruction
of a large defect of the proximal ulna is not well established
(1–6). We found only two cases of
endoprosthetic reconstruction for malignant bone tumor of the
proximal ulna (2,3). However, clinical details, including
long-standing durability, were not reported.
Elbow allografts appear to be another option.
However, elbow allografts have been associated with a high risk of
infection and joint degeneration. Dean et al reported that
complications occurred in 16 of 23 patients treated with allograft
implantations for massive bone loss of the elbow. They concluded
that elbow allografts were not recommended for routine use of elbow
surgery (8).
Gianoutsos et al reported a case of
adamantinoma of the proximal ulna treated with en bloc excision and
vascularised fibular graft. The patient had remained free of
disease with good function of the elbow (flexion-extension,
10–100°) 3 years after surgery. However, the elbow joint was
subluxated and the instability of the elbow joint was not mentioned
(9).
Kimura et al also reported excellent results
with 4-year follow-up periods of a case of Ewing sarcoma at the
proximal ulna treated with vascularised fibular graft. They grafted
a fibular head with the biceps femoris tendon and the fibular
ligament. The biceps femoris tendon was sutured to the annular
ligament and the fibular collateral ligament was sutured to the
tendon of the triceps muscle. The functional results were excellent
with active movement of the elbow from 5 to 150°, but joint
stability of the elbow was not reported (10).
Extracorporeal irradiation of tissue followed by
re-implantation can be used to replace bone defects following
removal of tumors (11–19). One of the advantages of irradiated
bone for reconstructive surgery is the possibility of achieved good
joint function, especially where the ligamentous tissues have been
preserved, since the ligaments of the patient can be restored to
their original shape, size and site (12). However, the complication rate of
this reconstruction, including non-union, infection and fracture
was high (12–16). Recently, favorable results of the
combined use of vascularised bone graft and extracorporeally
irradiated bone for reconstruction have been reported (18,19).
This approach has the advantage of combining the biological
properties provided by the vascularised bone graft with the
mechanical endurance of the irradiated osteochondral graft.
In the present case, since the tumor occurred in the
proximal site of the ulna, the ulna had to be excised along with
the joint surface, elbow ligaments and tendons. In order to
reconstruct the elbow joint, we used irradiated osteochondral and
soft tissue graft with vascularised fibular graft to enhance the
neovascularization of irradiated tissue. Although iliac bone graft
for the non-union of the proximal osteosynthetic site was
necessary, long-standing joint stability was excellent. Some degree
of articular change clearly occurs after irradiated osteochondral
graft (18). Further follow-up of
this patient is needed to monitor the risk of severe joint
degeneration.
In conclusion, a vascularised fibula, combined with
extracorporeally irradiated osteochondral graft, with ligamentous
repair, is one of the options for the treatment of malignant bone
tumor of the proximal ulna.
References
|
1
|
Ross AC, Sneath RS and Scales JT:
Endoprosthetic replacement of the humerus and elbow joint. J Bone
Joint Surg. 69-B:652–653. 1987.
|
|
2
|
Weber KL, Lin PP and Yasko AW: Complex
segmental elbow reconstruction after tumor resection. Clin Orthop.
415:31–44. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sperling JS, Prichard DJ and Morrey BF:
Total elbow arthroplasty after resection of tumors at the elbow.
Clin Orthop. 367:256–261. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kulkarni A, Fiorenza F, Grimer RJ, et al:
The results of endoprosthetic replacement for tumours of the distal
humerus. J Bone Joint Surg. 85-B:24–243. 2003.
|
|
5
|
Hanna SA, David LA, Aston WLS, et al:
Endoprosthetic replacement of the distal humerus following
resection of bone tumours. J Bone Joint Surg. 89-B:1498–1503. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Schwab JH, Healey JH and Athanasian EA:
Wide en bloc extra-articular excision of the elbow for sarcoma with
complex reconstruction. J Bone Joint Surg. 90-B:78–83. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Koller H, Kolb K, Assuncao A, et al: The
fate of elbow arthrodesis: Indications, techniques and outcome in
fourteen patients. J Shoulder Elbow Surg. 17:293–306. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dean GS, Holliger EH and Urbaniak JR:
Elbow allograft for reconstruction of the elbow with massive bone
loss. Long term results. Clin Orthop. 341:12–22. 1997.PubMed/NCBI
|
|
9
|
Gianoutsos MP, Marsden FW, McCarthy SW, et
al: Ulnar adamantionoma: en bloc excision and fibular
osteoseptocutaneous free flap reconstruction. J Hand Surg.
19-A:495–499. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kimura K, Tatezaki S, Ishii T, et al:
Hemiarthroplasty of the elbow with a vascularized fibular graft
after excision of Ewing’s sarcoma of the proximal ulna: a case
report. Jpn J Clin Oncol. 32:430–434. 2002.PubMed/NCBI
|
|
11
|
Spira E and Lubin E: Extracorporeal
irradiation of bone tumours: a preliminary report. Isr J Med Sci.
4:1015–1019. 1968.PubMed/NCBI
|
|
12
|
Araki N, Myoui A, Kuratsu S, et al:
Intraoperative extracorporeal autogenous irradiated bone grafts in
tumor surgery. Clin Orthop. 368:196–205. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen WM, Haung CK, Chiang CC and Lo WH:
Treatment of malignant bone tumours by extracorporeal irradiated
autograft-prosthetic composite arthroplasty. J Bone Joint Surg.
84-B:1156–1157. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Davidson AW, Hong A, McCarthy SW and
Stalley PD: En-bloc resection, extracorporeal irradiation, and
re-implantation in limb salvage for bony malignancies. J Bone Joint
Surg. 87-B:851–857. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Uyttendaele D, De Schryver A, Claessens H,
et al: Limb conservation in primary bone tumours by resection,
extracorporeal irradiation and re-implantation. J Bone Joint Surg.
70-B:348–353. 1988.PubMed/NCBI
|
|
16
|
Hatano H, Ogose A, Hotta T, et al:
Extracorporeal irradiated autogenous osteochondral graft: a
histological study. J Bone Joint Surg. 87-B:1006–1011. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yamamoto T, Hitona T and Marui K:
Reimplantation of autoclaved or irradiated cortical bones invaded
by soft tissue sarcomas. Anticancer Res. 22:3685–3690.
2002.PubMed/NCBI
|
|
18
|
Muramatsu K, Ihara K, Hashimoto T, et al:
Combined use of free vascularised bone graft and
extracorporeally-irradated autograft for the reconstruction of
massive bone defects after resection of malignant tumour. J Plast
Reconst Aesth Surg. 60:1–13. 1038:2007.PubMed/NCBI
|
|
19
|
Krieg AH, Davidson AW and Stalley PD:
Intercalary femoral reconstruction with extracorporeal irradiated
autogenous bone graft in limb-salvage surgery. J Bone Joint Surg.
89-B:366–371. 2007. View Article : Google Scholar : PubMed/NCBI
|