Introduction
Glioblastoma multiforme (GBM) is one of the most
malignant and aggressive tumors, and has a very poor prognosis and
high recurrence rate with a mean survival time of less than 2 years
even after the recent development of an intensive temozolomide
(TMZ)-based treatment protocol (1,2). Thus,
a novel therapeutic approach to controlling recurrence and
overcoming resistance to treatment is crucially needed for
glioblastoma patients. Novel therapeutic approaches to control
tumor recurrence by targeting crucial signaling molecules such
TGF-β (3), JAK-STAT (4–6) and
WINT (7), adhesion molecules αβ
integrin (8), and pro-angiogenic
factors VEGF and VEGFR (9), have
been tried. However, a new breakthrough has yet to be found.
Immunotherapy is also recognized as a therapeutic
tool against human GBM, and preliminary studies trying to suppress
recurrence have been reported (10–13).
Ardon et al (13) reported that dendritic cell
(DC)-based vaccines against GBM had moderate effects in terms of a
patient’s performance status (PS) or quality of life (QOL) in
clinical phase I/II trial against advanced or newly diagnosed
high-grade gliomas.
As to immunogenic antigens, several studies
regarding glioma-specific cancer antigen including WT1, MAGE,
gp100, HER2, which have been already used for clinical trial, were
reported (14–16). WT-1 expression in glioblastomas was
reported by Oji et al (14).
Liu et al (16) reported
that HER2, gp100 and MAGE-A1 mRNA expression was detected in 81.4,
46.5 and 39.5% of 43 GBM primary cell lines, and determined CTL
epitope specific for each antigen. As to the CT antigen expression
in gliomas, several studies have been reported (17–22).
Debinski et al (17) showed
the specific expression of IL-13RA2 gene, common CT antigen in
high-grade gliomas. Recently, Syed et al (21) demonstrated that two CT antigens
(MAGE-A1 and MAGE-A3) and gp100 may be candidate antigens in
primary GBM cell lines using RT-PCR specific for 11 CT antigens and
4 melanocyte-differentiation antigens, however, those antigen
expression was low-to-variable level. Furthermore, Sahin et
al (22) analyzed expression of
7 CT antigens in 88 brain tumor specimen including meningiomas, and
showed that SCP-1 exhibited the highest expression rate. However, a
comprehensive expression analysis of CT antigens in high-grade
gliomas is very limited.
In the present study, a comprehensive expression
analysis of 54 CT antigens and 13 glioma-associated antigens were
performed using a quantitative PCR in 17 high-grade glioma-derived
primary cell lines, and the co-relation of antigen expression to
overall survival and
O6-methylguanine-DNA-methyltransferase (MGMT) expression
was also investigated.
Materials and methods
Establishment of primary GB cell lines
from high-grade glioma patients
Glioma tumor samples were obtained from surgical
resections by neurosurgeons in Shizuoka Cancer Center. The clinical
research using tumor tissues from glioma patients was approved by
the Institutional Review Board of Shizuoka Cancer Center, Shizuoka,
Japan. All patients gave written informed consent. Seventeen
high-grade glioma patients, who are sources of established primary
glioma cell lines, are characterized in Table I.
 | Table ICharacteristics of the high-grade
glioma patients. |
Table I
Characteristics of the high-grade
glioma patients.
| Total no.
enrolled | 17 |
| Age (years) | 55.3±16.6 |
| Gender | Male (13), Female (4) |
| Pathological
diagnosis | GBM 13 (grade IV), AA
1 (grade III), AO 3 (grade III) |
Tumors were dissociated by teasing with forceps to
make a single cell suspension, and plated in 25 cm2
culture flask in Dulbecco’s modified Eagle’s medium (DMEM) (Sigma,
St. Louis, MO, USA) supplemented with 10% fetal bovine serum (FBS;
Invitrogen), penicillin, streptomycin and gentamycin (Invitrogen)
for serum-derived GB cell line. Glioblastoma cell lines (A172,
T98G, LN-18, U87, U118, U138 and U373) was purchased from the
American Type Culture Collection (ATCC; Manassas, VA, USA) and
maintained in DMEM containing 10% FBS plus penicillin and
streptomycin.
Antibodies and reagents
Antibodies against 6 CT antigens (MAGE-A12, BAGE,
DDX43, IL-13RA2, CTAGE1 and CASC5) were purchased from the
following sources; Abnova for MAGE-A12, LSBio Inc. for BAGE,
Proteintech for DDX43 and IL-13RA2, Santa Cruz Biotechnology for
CTAGE1, Bethyl Laboratories Inc. for CASC5. Antibodies against 10
glioma-associated antigens (HER2, Ki-67, Podplanin, gp100, GFAP,
MGMT, Nestin, Olig2, S100 and CD133) were purchased from the
following sources; Dako for HER2, Ki-67 and gp100, Santa Cruz
Biotechology for Podplanin, AbD Serotec for GFAP, Abcam for MGMT
and IBL for Nestin, Olig2 and CD133.
Quantitative polymerase chain reaction
(qPCR) analysis
The real-time PCR analysis of CT antigen and
glioma-associated genes using the 7500 Real-Time PCR System
(Applied Biosystems, Foster City, CA, USA) was performed as
previously described. Briefly, 54 CT antigen-specific PCR primers
(from CT1.1 to CT50; shown in Table
II) or 13 glioma-associated gene-specific PCR primers (HER2,
Ki-67, Podplanin, gp100, GFAP, MGMT, Nestin, Olig2, S100, CD133,
WT1, MART-1 and Tyrosinase) and TaqMan probes were purchased from
Applied Biosystems. Total RNAs were extracted from each glioma cell
line or primary cells derived from high-grade gliomas.
Complementary DNA was synthesized from 100 ng of the total RNA and
quantitative PCRs were carried using a TaqMan RNA-to-CT 1-Step kit
(Applied Biosystems). As a negative control for tumor RNA, total
RNA from the normal fetal brain (platinum total RNA) was purchased
from Takara Bio Inc. (Otsu, Shiga, Japan).
 | Table IICT antigen PCR primer list. |
Table II
CT antigen PCR primer list.
| CT code | Gene family |
|---|
| CT1.1 | MAGE-A1 |
| CT1.2 | MAGE-A2 |
| CT1.3 | MAGE-A3 |
| CT1.4 | MAGE-A4 |
| CT1.5 | MAGE-A5 |
| CT1.6 | MAGE-A6 |
| CT1.8 | MAGE-A8 |
| CT1.9 | MAGE-A9 |
| CT1.10 | MAGE-A10 |
| CT1.11 | MAGE-A11 |
| CT1.12 | MAGE-A12 |
| CT2.1 | BAGE |
| CT3.1 | MAGE-B1 |
| CT3.2 | MAGE-B2 |
| CT3.4 | MAGE-B6 |
| CT4.1 | GAGE1 |
| CT5.1 | SSX1 |
| CT6.1 | CTAG1B |
| CT7.2 | MAGE-C3 |
| CT8 | SYCP1 |
| CT9 | BRDT |
| CT10 | MAGE-C2 |
| CT11.1 | SPANXA1 |
| CT12.1a | XAGE1 |
| CT13 | DDX43 |
| CT14 | SAGE1 |
| CT15 | ADAM2 |
| CT16.1 | PAGE5 |
| CT17 | LIPI |
| CT19 | IL-13RA2 |
| CT21.1 | CTAGE1 |
| CT24.1 | CSAG1 |
| CT25.1a | DSCR8 |
| CT26 | DDX53 |
| CT27 | CTCFL |
| CT28 | LUZP4 |
| CT29 | CASC5 |
| CT30 | TFDP3 |
| CT32 | LDHC |
| CT33 | MORC1 |
| CT34 | DKKL1 |
| CT35 | SPO11 |
| CT36 | CRISP2 |
| CT37 | FMR1NB |
| CT38 | FTHL17 |
| CT39 | NXF2 |
| CT41.1 | TDRD1 |
| CT42 | TEX15 |
| CT43 | FATE1 |
| CT44 | TPTE |
| CT45 | CT45A1–6 |
| CT47.11 | CT47A11 |
| CT48 | SLC06A1 |
| CT50 | LEMD1 |
Immunohistochemistry (IHC)
Two representative cases, GB-case no. 16 and
9-derived resected tumors were fixed with formalin solution and
used for IHC analysis of CT antigens and glioma-associated
antigens, respectively. Hematoxylin-eosin staining was performed
according to the manufacturer’s instructions. For immunostaining,
antibodies against 6 CT antigens (MAGE-A12, BAGE, DDX43, IL-13RA2,
CTAGE1 and CASC5) and antibodies against 10 glioma-associated
antigens (HER2, Ki-67, Podplanin, gp100, GFAP, MGMT, Nestin, Olig2,
S100 and CD133) were used as primary antibody. Goat anti-mouse IgG
antibody or goat anti-rabbit IgG was used as secondary antibody.
Horseradish peroxidase (HRP) and hydrogen peroxide were utilized
for making color according to the manufacturer’s instructions
(Vectastatin ABC kit; Vector Laboratories, Burlingame, CA,
USA).
Statistical analysis
The overall survival analysis based on the REMBRANDT
dataset regarding target antigen genes was examined by comparing
differences in median survival time (MST) via the Kaplan-Meier
method. A comparative analysis of survival times between groups was
then performed using the log rank test. Values of P<0.05 were
considered statistically significant. For the correlation analysis
to MGMT expression, the correlation coefficient, r, was calculated
and statistical difference was analyzed using the Pearson’s
correlation test. Values of P<0.05 were considered statistically
significant.
Results
Establishment of high-grade glioma
primary cell lines
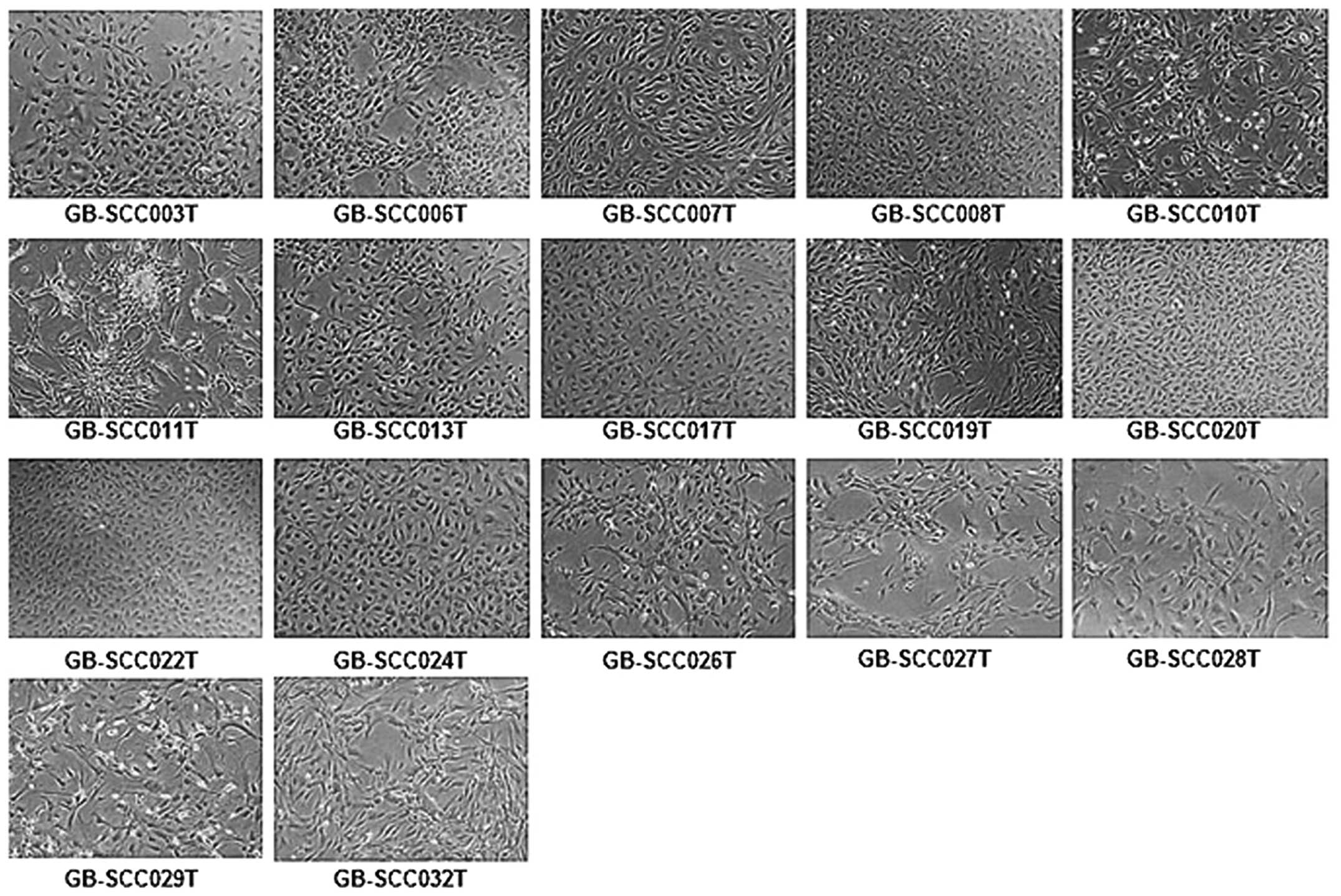
Seventeen serum-derived primary cell lines were
established. These cell lines consisted of 3 anaplastic
oligodendrogliomas, 1 anaplastic astrocytoma and 13 GBMs.
Histologically, 13 of the 17 cases were WHO grade IV. Morphological
appearances seem to be mainly adherent, but different among 17
primary cell lines ranging from round to fibroblast-like shape.
Heterogeneous cell populations were seen, where adherent and
floating cells were mixed (Fig.
1).
Quantitative PCR analysis of CT antigen
or glioma-associated gene mRNA in glioma primary cell lines
A quantitative PCR using 54 cancer-testis (CT)
antigen-specific primers showed that 36 CT antigens were positive
in at least 1 of 17 serum-derived cell lines, and 17 antigens were
positive in >50% cell lines (Table
III). Impressively, 6 genes (BAGE, MAGE-A12, CSAC5, CTAGE1,
DDX43 and IL-13RA2) were detected in all the cell lines. On the
other hand, the expression of other 13 glioma-associated antigens
than CT genes were also investigated, and 10 genes were detected in
>70% of the cell lines (Table
IV). Glioma-specific antigens CD133, S100, Olig2, Podplanin and
Nestin were detected in most primary cells as well as commercially
available cell lines. Notably, gp100 and HER2, common cancer
antigens, were also positively expressed in all cell lines as well
as the regular ones. MGMT was positive in all cell lines except
one.
 | Table IIICT antigen expression in glioma cell
lines and primary cells from high-grade glioma patients. |
Table III
CT antigen expression in glioma cell
lines and primary cells from high-grade glioma patients.
| Antigen | LN-18 | U87 | A172 | T98 | U118 | U138 | U373 | GB primary |
|---|
| MAGEA12 | + | + | + | + | + | + | + | 17 (100%) |
| CSAC5 | + | + | + | + | + | + | + | 17 (100%) |
| CTAGE1 | + | + | + | + | + | + | + | 17 (100%) |
| DDX43 | + | + | + | − | − | − | + | 17 (100%) |
| IL13RA2 | + | + | + | + | + | + | + | 17 (100%) |
| BAGE | + | + | + | + | + | + | + | 17 (100%) |
| CSAG1 | + | + | + | + | + | + | + | 16 (94%) |
| LDHC | + | + | + | + | + | + | + | 16 (94%) |
| TDRD1 | + | − | + | − | − | − | − | 16 (94%) |
| MAGEB6 | + | + | + | + | + | + | + | 16 (94%) |
| TEX15 | + | + | − | + | + | − | + | 15 (88%) |
| TFDP3 | + | + | + | + | + | + | + | 15 (88%) |
| SPANXA1 | + | + | + | + | + | + | + | 14 (82%) |
| CTCFL | + | + | + | − | − | − | + | 13 (76%) |
| MAGEA11 | + | + | + | − | + | − | − | 13 (76%) |
| MORC1 | + | + | + | + | + | + | + | 12 (70%) |
| FMR1NB | + | − | + | + | + | + | + | 11 (64%) |
| DDX53 | + | + | + | + | + | + | + | 8 (47%) |
| CTAG1B | + | − | − | − | − | − | − | 5 (29%) |
| FTHL17 | + | + | + | − | − | − | + | 5 (29%) |
| MAGEC2 | + | + | − | + | − | − | − | 4 (23%) |
| FATE1 | + | + | − | + | + | + | − | 4 (23%) |
| SAGE1 | + | + | − | − | − | − | − | 3 (18%) |
| XAGE1A-E | + | + | + | + | + | + | − | 3 (18%) |
| CT47A11 | + | + | − | + | + | + | − | 3 (18%) |
| SLC06A1 | + | − | − | − | − | − | − | 3 (18%) |
| CRISP2 | + | − | + | − | − | + | − | 2 (11%) |
| LEMD | − | − | + | + | − | − | − | 2 (11%) |
| LUZP4 | + | + | − | − | − | + | − | 2 (11%) |
| CT45A1–6 | + | + | − | − | − | − | − | 2 (11%) |
| NXF | + | + | + | − | + | − | − | 1 (5.8%) |
| BRDT | − | − | − | − | + | + | + | 1 (5.8%) |
| MAGEA3 | + | + | + | + | + | + | + | 1 (5.8%) |
| SSX | + | + | + | + | + | + | − | 1 (5.8%) |
| ADAM2 | + | − | − | − | − | − | − | 1 (5.8%) |
| SPO11 | − | − | − | + | − | − | − | 1 (5.8%) |
 | Table IVGlioma-associated gene expression in
glioma cell lines and primary cells from high-grade glioma
patients. |
Table IV
Glioma-associated gene expression in
glioma cell lines and primary cells from high-grade glioma
patients.
| Antigen | LN-18 | U87 | A172 | T98 | U118 | U138 | U373 | GB primary |
|---|
| HER2 | + | + | + | + | + | + | + | 17 (100%) |
| Ki-67 | + | + | + | + | + | + | + | 17 (100%) |
| Podoplanin | + | + | − | + | + | + | + | 17 (100%) |
| gp100 | + | + | + | + | + | + | + | 17 (100%) |
| MGMT | + | − | − | + | + | + | + | 16 (94%) |
| NES | + | + | + | + | + | + | + | 16 (94%) |
| GFAP | + | + | + | − | + | − | + | 15 (88%) |
| OLIG2 | + | + | + | + | + | + | − | 15 (88%) |
| S100 | + | − | + | + | + | + | + | 14 (82%) |
| CD133 | + | + | + | + | + | + | + | 12 (70%) |
| WT-1 | + | + | + | + | − | − | + | 8 (47%) |
| MelanA | − | − | − | − | − | − | − | 2 (11%) |
| Tyrosinase | − | + | − | − | + | − | − | 1 (5.8%) |
Immunohistochemistry
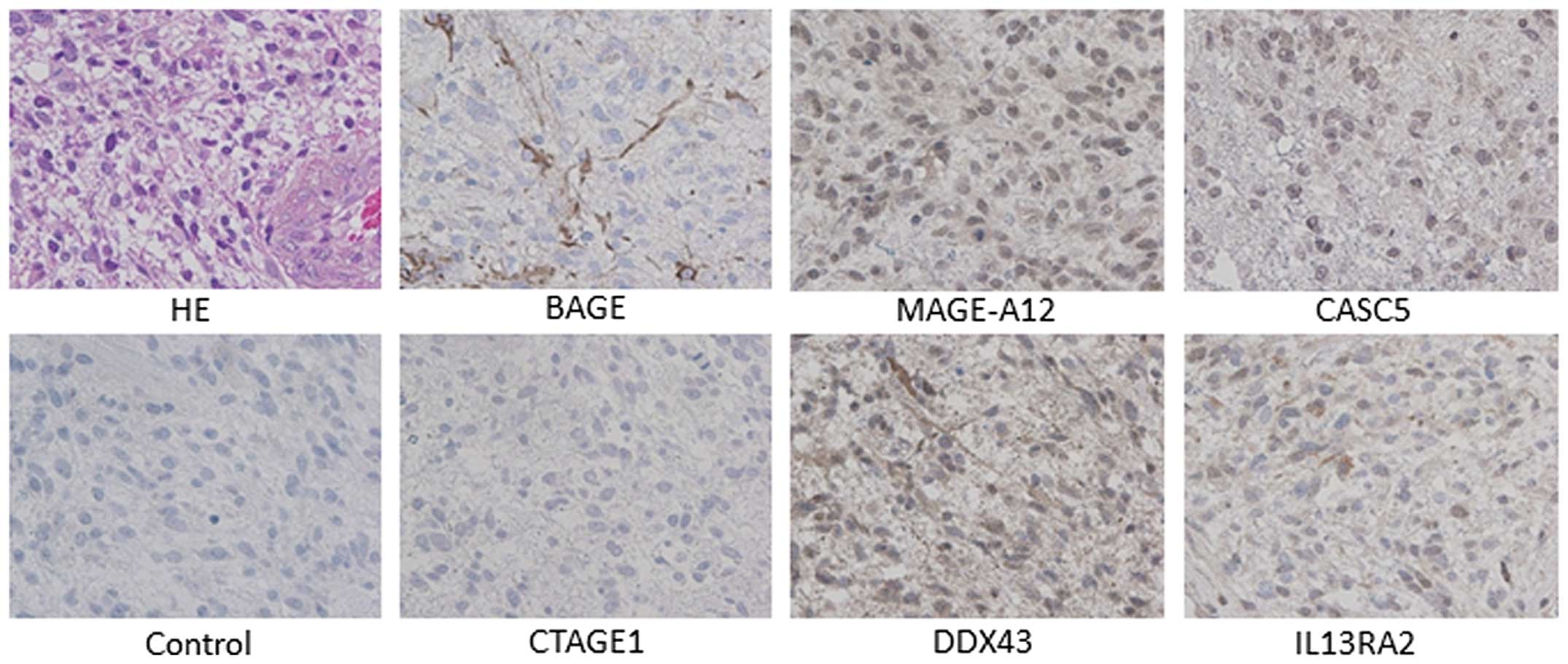
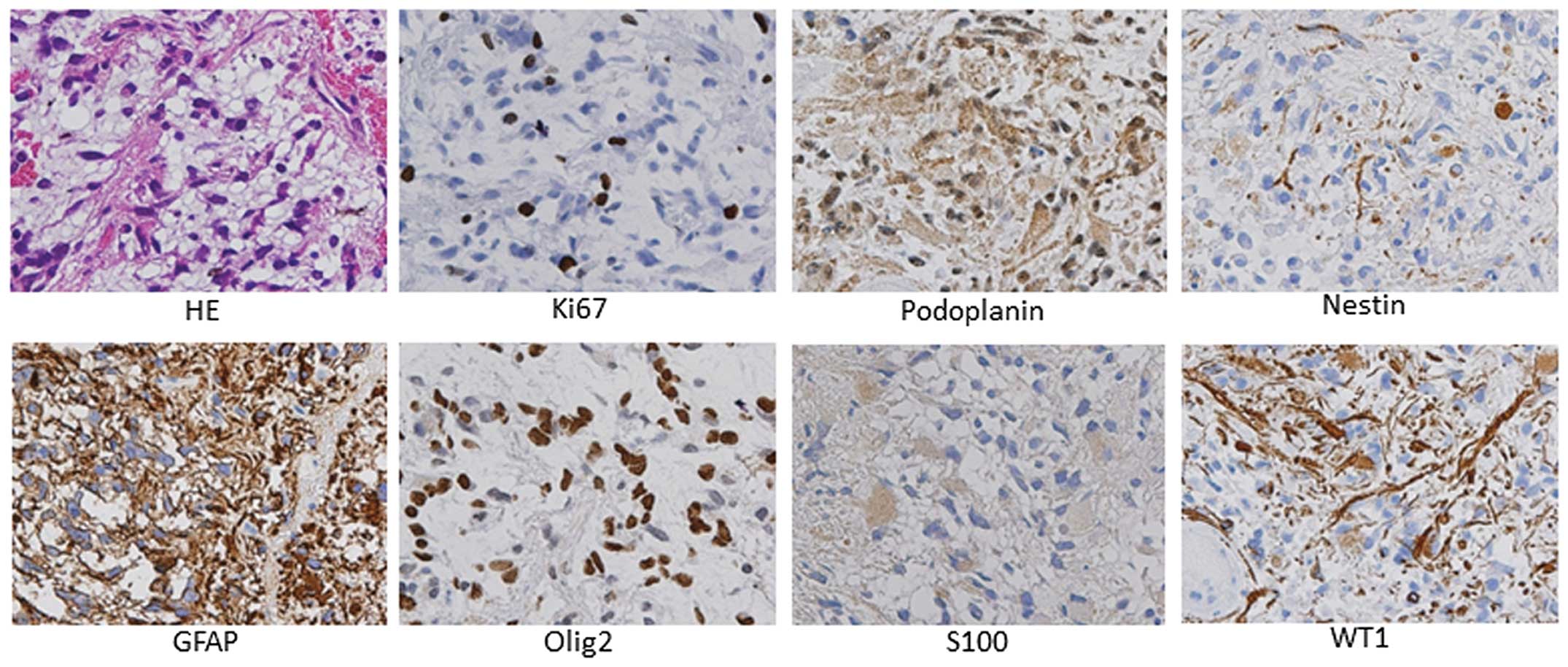
The expression of CT antigen and glioma-associated
antigen genes with a high frequency were verified in IHC analysis
using GB-case 16-derived resected tumor specimen. In 6 CT antigens
(MAGE-A12, BAGE, DDX43, IL-13RA2, CTAGE1 and CASC5), all antigen
proteins other than CTAGE1 were positively expressed in the tumor
from patient (Fig. 2). On the other
hand, 10 glioma-associated antigens (HER2, Ki-67, Podplanin, gp100,
GFAP, MGMT, Nestin, Olig2, S100 and CD133) staining showed that all
antigen proteins besides MGMT, CD133, HER2 and gp100 were detected
in the tumor from GB-case 9 (Fig.
3).
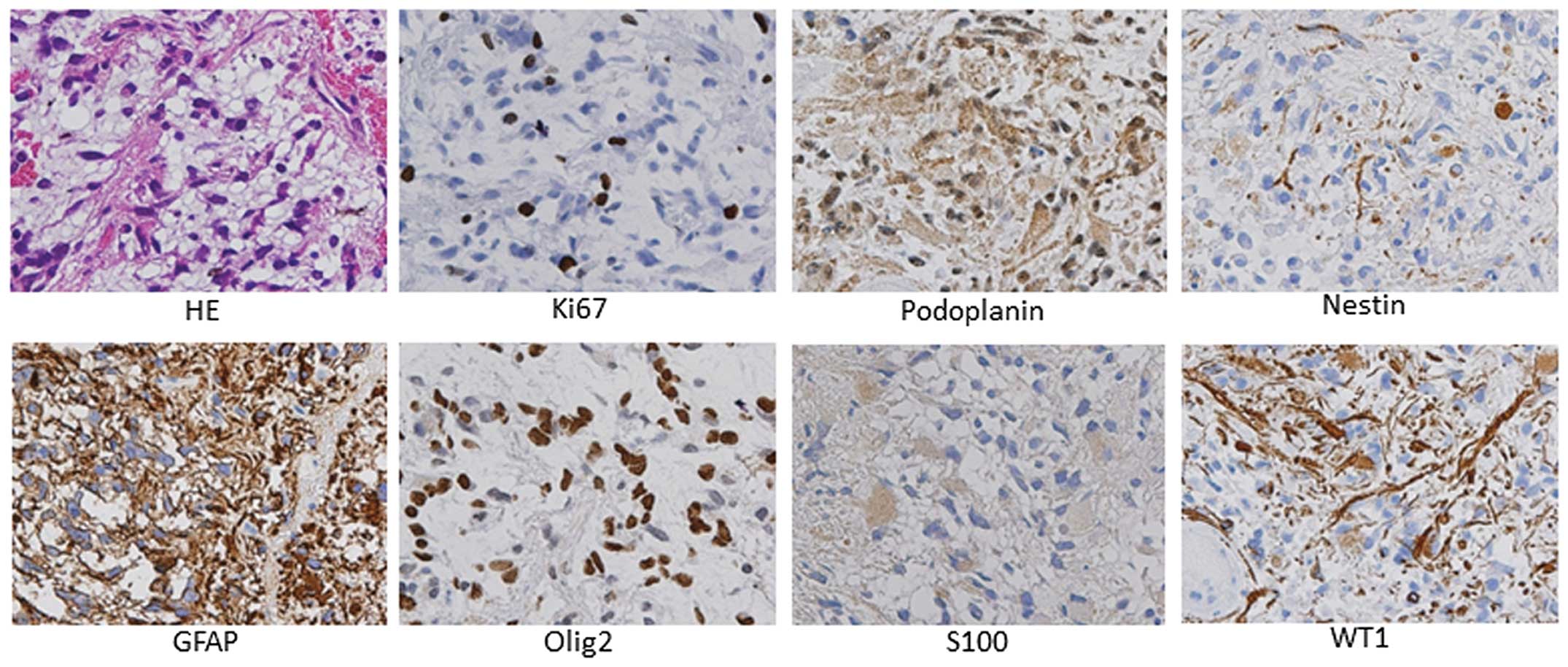 | Figure 3Glioma-associated antigen protein
expression in GBM tumor tissue (GB-no. 9). Primary antibodies
against 10 glioma-associated antigens (HER2, Ki-67, Podplanin,
gp100, GFAP, MGMT, Nestin, Olig2, S100 and CD133) were used for
immunostaining. Expression of MGMT, gp100 and CD133 was negative,
and for all other antigens positive. H&E; hematoxylin-eosin;
magnification, ×400. |
CT antigen gene expression compared with
normal brain tissue
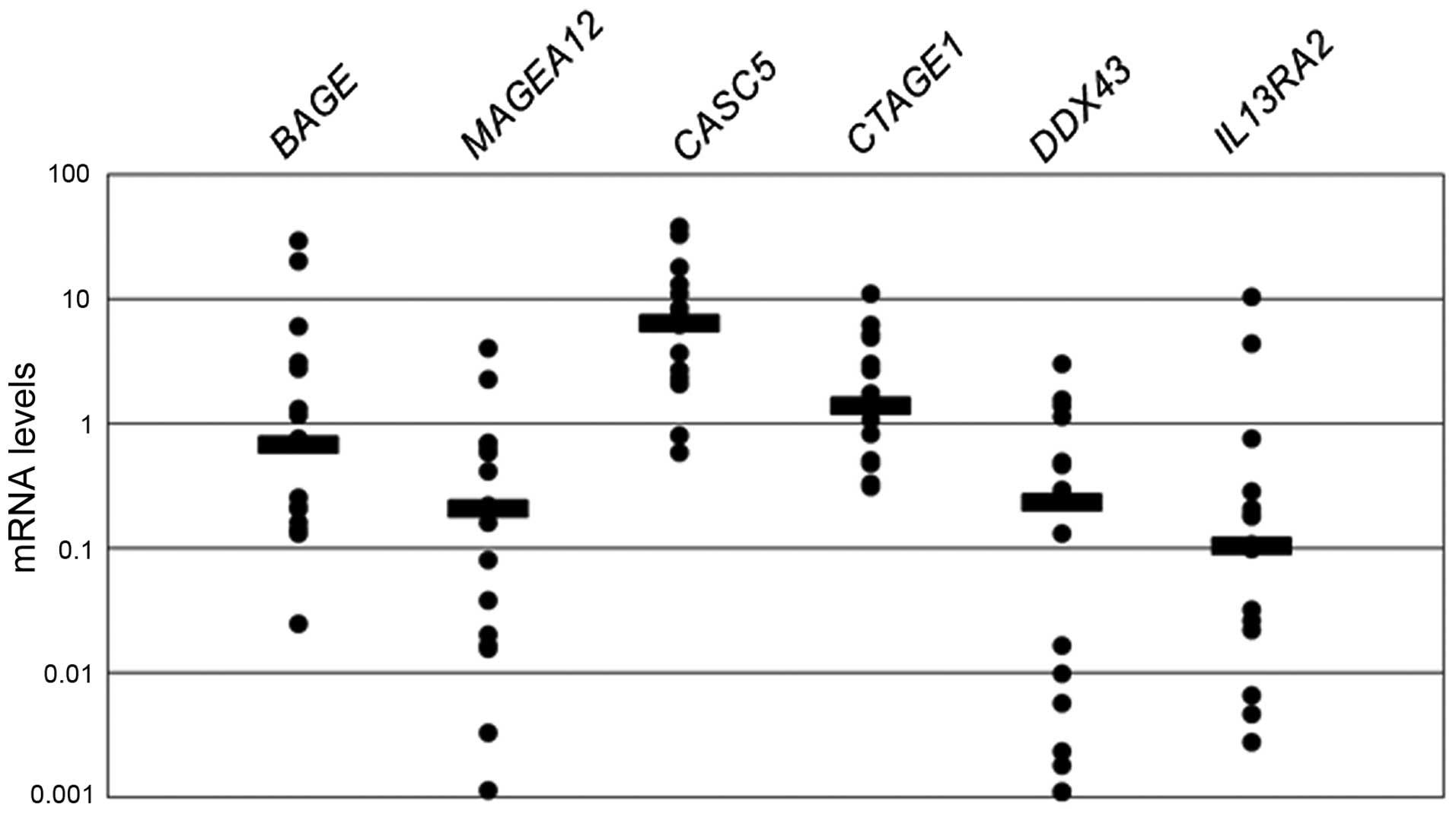
Gene expression levels of 6 CT antigens in primary
high-grade glioma cell lines were significantly upregulated in
CASC5 and CTAGE1 compared with normal brain (Fig. 4). In particular, CASC5 expression
level was higher almost 10-fold than normal brain. Unexpectedly,
IL-13RA2 mean expression level was lower than normal level.
Correlation of CT antigen expression to
overall survival and MGMT expression
The correlation of antigen expression level to
overall survival time was analyzed using REMBRANDT database of the
National Cancer Institute in the 17 CT antigens and 10
glioma-associated genes which were highly expressed in glioma
primary cell lines. The expressions of IL-13RA2, HER2, Ki-67,
podplanin, Olig2 and CD133 were inversely correlated to overall
survival time in high-grade glioma patients given a standard
chemo-radiation after surgery (P<0.01; Table V). Another correlation analysis of
CT antigen and glioma-associated gene to MGMT expression
demonstrated that 4 genes including DDX43, TDRD1, HER2 and gp100
had significant positive relationship to MGMT expression.
Particularly, HER2 and gp100 genes showed very high coefficient
(r=0.751 and 0.894, respectively; Table VI).
 | Table VPrognostic factor candidates. |
Table V
Prognostic factor candidates.
| Gene family | Positive rate
(%) | Gene
expression | P-value |
|---|
| IL-13RA2 | 17/17 (100) | Overexpressed |
2.08×10−4a |
| HER2 | 17/17 (100) | Overexpressed |
8.53×10−7a |
| Ki-67 | 17/17 (100) | Overexpressed |
2.57×10−3a |
| Podplanin | 17/17 (100) | Overexpressed |
7.02×10−14a |
| Olig2 | 15/17 (88) | Overexpressed |
1.75×10−10a |
| CD133 | 12/17 (70) | Overexpressed |
8.1×10−8a |
 | Table VIRelevant factors to MGMT
expression. |
Table VI
Relevant factors to MGMT
expression.
| Gene family | Positive rate
(%) | Correlation
coefficient (r) | P-value |
|---|
| DDX43 | 17/17 (100) | 0.540 | 0.0292a |
| TDRD1 | 16/17 (94.1) | 0.675 | 0.0031b |
| HER2 | 17/17 (100) | 0.751 | 0.0004b |
| gp100 | 17/17 (100) | 0.894 | <0.0001b |
Discussion
Glioblastoma multiforme (GBM) is one of the most
malignant and aggressive tumors, and even with an intensive
treatment including surgery, radiation and chemotherapy, the median
survival time is about 1 year and few cases can survive more than 2
fears (1,2). Therefore, novel therapeutic approach
to control the recurrence and overcome the resistance to treatment
is crucially needed in glioblastoma patients.
A prerequisite for the successful immunotherapy is
the identification of suitable tumor antigens specifically
expressed in cancer tissues and its clinical application as an
advanced translational research. Renkvist et al (23) classified human tumor antigens
recognized by T cells into 6 categories; i) HLA class I-restricted
cancer/testis antigens, ii) differentiation antigens, iii) widely
expressed antigens, iv) tumor-specific antigens, v) HLA class
II-restricted antigens and (vi) fusion proteins. Particularly, CT
antigen and melanoma-associated differentiation antigen have been
focused on, and several peptides including MAGE family, NY-ESO,
IL-13RA2, MART-1, gp100 and tyrosinase were effectively used in
clinical vaccinations for advanced melanoma and glioma patients
(24–28).
To develop novel glioma-specific antigens, in the
present study, we performed a comprehensive expression analysis of
CT antigen and glioma-associated genes in patients-derived primary
glioma cell lines using a quantitative PCR. A quantitative PCR
using 54 cancer-testis (CT) antigen-specific primers showed that 36
CT antigens were positive in at least 1 of 17 serum-derived cell
lines, and 17 antigens were positive in >50% cell lines.
Particularly, 6 genes (BAGE, MAGE-A12, CSAC5, CTAGE1, DDX43 and
IL-13RA2) were detected in all cell lines. Sahin et al
(22) reported the frequency of
selected 7 CT antigen gene expression in 88 human brain tumor
specimen using RT-PCR. The highest frequency was 40% in SCP-1 gene
expression, and 23 astrocytomas expressed at least one CT gene.
Another RT-PCR study by Syed et al (21) using 45 glioma-frozen tissues
revealed that the highest CT antigen expression rates were MAGEA-3
(22%) and MAGEA-1 (16%) in 11 CT genes.
Our highest expression rate was 100% in 6 CT genes,
and all primary cell lines showed expression in at least 14 CT
antigen genes, thus showing significantly better results compared
to the previous study. Possible reasons why our expression
frequency was higher is speculated as; i) higher purity of tumor
cells because newly established serum-derived primary cell cultures
were used for analysis, ii) the number of CT genes analyzed was
higher, iii) validated quantitative PCR primer. On the other hand,
the expression of other 13 glioma-associated antigens than CT genes
were also investigated, and 10 genes were detected in more than 70%
of the cell lines. Specifically, glioma-assocated genes such as
HER2, podoplanin and gp100 were positive in all the cell lines.
HER2 and gp100 as melanocyte-differentiation antigen
(MDA) were reported to be highly expressed in malignant melanoma
and glioma tissues as well as WT1. Interestingly, because both
melanocytes and glial cells are derived from the neuroectoderm, it
is not surprising that they express common MDA and CT antigen genes
(29).
In the present study, correlation analysis of CT
antigen and glioma-associated genes to overall survival time and
MGMT expression was performed. IL-13RA2 and HER2 genes were
demonstrated to be prognostic factor candidates for a poor survival
(Table V), which may suggest that
prognostic analysis can contribute to the understanding the novel
function of CT antigen genes. Both target genes are well known to
be expressed in GBM tumors, therefore specific clinical
immunotherapy against these molecules has been performed in a small
size of trail design. Specifically, obvious evidence that the
downregulation of IL-13RA2 and HER2 antigen expression by
therapeutic agents may contribute to a good prognosis has yet to be
obtained. Furthermore, few studies regarding the correlation
between CT antigens and survival time have been reported to date.
That is why our observations should be stressed in terms of
novelty.
Additionally, we analyzed the correlation of CT
antigen genes to MGMT expression. Interestingly, 4 antigen gene
candidates positively correlated to MGMT expression, were
identified. In particular, HER2 and gp100 showed a high coefficient
(r=0.751 and 0.894, respectively). MGMT expression is considered to
be regulated by DNA methylation mechanism, and crucial in terms of
determining the chemosensitivity of high-grade gliomas to
temozolomide (30). It is
well-known that high expression of MGMT is closely associated with
poor prognosis in high-grade gliomas, and DNA-methylation of MGMT
can be a possible approach to MGMT reduction (31,32).
If some CT antigens are linked to MGMT gene in
DNA-demethylation to promoter area, epigenetic approach to DNA
methylation of CT genes could be a novel therapy, resulting in a
therapeutic effect on high-grade gliomas. However, there is no
evidence for correlation of both gene promoters, and clarification
of the question will need more investigation. Natsume et al
(33) reported that the
DNA-demethylating agent 5-aza-2′-deoxycytidine (5-aza-CdR)
remarkably reactivated NY-ESO-1 gene expression and demonstrated
that 5-aza-CdR-induced expression of epigenetically silenced CT
antigen gene might be a new strategy for immunotherapy against
high-grade glioma.
Little is known about the precise function of CT
antigen genes. Notably, Low et al (34) reported a novel approach to
evaluating the function of CT gene using knockdown technology
against neural stem cell-derived CT antigen, and showed some CT
antigen genes were associated with the stem cell
differentiation.
Finally, in the present study, we analyzed
expression of 54 CT antigens using a quantitative PCR. In near
future, CT antigen repertoire will be expanded up to 100, and more
efficient biomarkers and prognostic markers specific for high-grade
glioma should be collected, where effective target antigens can be
determined for developing novel immunotherapy and antibody
medicines.
Acknowledgements
The present study was supported by a grant from the
Regional Innovation Strategy Support Program of the Ministry of
Education, Culture, Sports, Science and Technology, Japan.
Abbreviations:
|
GBM
|
glioblastoma multiforme
|
|
TMZ
|
temozolomide
|
|
MGMT
|
O6-methylguanine-DNA-methyltransferase
|
|
IHC
|
immunohistochemistry
|
|
RT-PCR
|
reverse transcriptase-polymerase chain
reaction
|
|
CT antigen
|
cancer-testis antigen
|
References
|
1
|
Stupp R, Mason WP, van den Bent MJ, et al:
Radiotherapy plus concomitant and adjuvant temozolomide for
glioblastoma. N Engl J Med. 352:987–996. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mirimanoff RO, Gorlia T, Mason W, et al:
Radiotherapy and temozolomide for newly diagnosed glioblastoma:
recursive partitioning analysis of the EORTC 26981/22981-NCIC CE3
phase III randomized trial. J Clin Oncol. 24:2563–2569. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ikushima H, Todo T, Ino Y, Takahashi M,
Miyazawa K and Miyazono K: Autocrine TGF-β signaling maintains
tumorigenicity of glioma-initiating cells through Sry-related
HMG-box factors. Cell Stem Cell. 5:504–514. 2009.
|
|
4
|
McFarland BC, Ma JY, Langford CP,
Gillespie GY, Yu H, Zheng Y, Nozell SE, Huszar D and Benveniste EN:
Therapeutic potential of AZD1480 for the treatment of human
glioblastoma. Mol Cancer Ther. 10:2384–2393. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sai K, Wang S, Balasubramaniyan V, et al:
Induction of cell-cycle arrest and apoptosis in glioblastoma
stem-like cells by WP1193, a novel small molecule inhibitor of the
JAK2/STAT3 pathway. J Neurooncol. 107:487–501. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ashizawa T, Miyata H, Ishii H, et al:
Antitumor activity of a novel small molecules STAT3 inhibitor
against a human lymphoma cell line with high STAT3 activation. Int
J Oncol. 38:1245–1252. 2011.PubMed/NCBI
|
|
7
|
Zhou Y, Liu F, Xu Q and Wang X: Analysis
of the expression profile of Dickkopf-1 gene in human glioma and
the association with tumor malignancy. J Exp Clin Cancer Res.
29:1382010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Reardon DA, Fink KL, Mikkelsen T, et al:
Randomized phase II study of cilemgitide, an integrin-targeting
arginine-glycine-aspartic acid peptide, in recurrent glioblastoma
multiforme. J Clin Oncol. 26:5610–5617. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jo J, Schiff D and Purow B: Angiogenic
inhibition in high-grade gliomas: past, present and future. Expert
Rev Neurother. 12:733–747. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chang CN, Huang YC, Yang DM, Kikuta K, Wei
KJ, Kubota T and Yang WK: A phase I/II clinical trial investigating
the adverse and therapeutic effects of a postoperative autologous
dendritic cell tumor vaccine in patients with malignant glioma. J
Clin Neurosci. 18:1048–1054. 2011. View Article : Google Scholar
|
|
11
|
Luptrawan A, Liu G and Yu JS: Dendritic
cell immunotherapy for malignant gliomas. Rev Recent Clin Trials.
3:10–21. 2008. View Article : Google Scholar
|
|
12
|
Ardon H, Van Gool SW, Verschuere T, et al:
Intergation of autologous dendritic cell-based immunotherapy in the
standard of care treatment for patients with newly diagnosed
glioblastoma: results of the HGG-2006 phase I/II trial. Cancer
Immunol Immunother. 61:2033–2044. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ardon H, Van Gool S, Lopes IS, et al:
Integration of autologous dendritic cell-based immunotherapy in the
primary treatment for patients with newly diagnosed glioblastoma
multiforme: a pilot study. J Neurooncol. 99:261–272. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Oji Y, Suzuki T, Nakano Y, et al:
Overexpression of the Wilms’ tumor gene WT1 in primary astrocytic
tumors. Cancer Sci. 95:822–827. 2004.
|
|
15
|
Bodey B, Siegel SE and Kaiser HE: MAGE-1,
a cancer/testis-antigen, expression in childhood astrocytomas as an
indicator of tumor progression. In vivo. 16:583–588.
2002.PubMed/NCBI
|
|
16
|
Liu G, Ying H, Zeng G, Wheeler CJ, Black
KL and Yu JS: HER-2, gp100, and MAGE-1 are expressed in human
glioblastoma and recognized by cytotoxic T cells. Cancer Res.
64:4980–4986. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Debinski W and Gibo DM: Molecular
expression analysis of restrictive receptor for interleukin 13, a
brain tumor-associated cancer/testis antigen. Mol Med. 6:440–449.
2000.PubMed/NCBI
|
|
18
|
Schmits R, Cochlovius B, Treitz G, et al:
Analysis of the antibody repertoire of astrocytoma patients against
antigens expressed by gliomas. Int J Cancer. 98:73–77. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yawata T, Nakai E, Park KC, et al:
Enhanced expression of cancer testis antigen genes in glioma stem
cells. Mol Carcinog. 49:532–544. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
20
|
Oba-Shinjo SM, Caballero OL, Jungbluth AA,
Rosemberg S, Old LJ, Simpson AJ and Marie SK: Cancer-testis (CT)
antigen expression in medulloblastoma. Cancer Immun.
8:72008.PubMed/NCBI
|
|
21
|
Syed ON, Mandigo CE, Killory BD, Canoll P
and Bruce JN: Cancer-testis and melanocyte-differentiation antigen
expression in malignant glioma and meningioma. J Clin Neurosci.
19:1016–1021. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sahin U, Koslowski M, Tureci O, et al:
Expression of cancer testis genes in human brain tumors. Clin
Cancer Res. 6:3916–3922. 2000.PubMed/NCBI
|
|
23
|
Renkvist N, Castelli C, Robbins PF and
Parmiani G: A listing of human tumor antigens recognized by T
cells. Cancer Immunol Immunother. 50:3–15. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nestle FO, Alijagic S, Gilliet M, et al:
Vaccination of melanoma patients with peptide- or tumor
lysate-pulsed dendritic cells. Nat Med. 4:328–332. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Akiyama Y, Tanosaki R, Inoue N, et al:
Clinical response in Japanese metastatic melanoma patients treated
with peptide cocktail-pulsed dendritic cells. J Transl Med.
3:42005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tyagi P and Mirakhur B: MAGRIT: the
largest-ever phase III lung cancer trial aims to establish a novel
tumor-specific approach to therapy. Clin Lung Cancer. 10:371–374.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Aoki M, Ueda S, Nishikawa H, et al:
Antibody responses against NY-ESO-1 and HER2 antigens in patients
vaccinated with combinations of cholesteryl pullulan (CHP)-NY-ESO-1
and CHP-HER2 with OK-432. Vaccine. 27:6854–6861. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Okada H, Kalinski P, Ueda R, et al:
Induction of CD8+ T-cell responses against novel
glioma-associated antigen peptides and clinical activity by
vaccinations with α-type 1 polarized dendritic cells and
polyinosinic-polycytidylic acid stabilized by lysine and
carboxymethylcellulose in patients with recurrent malignant glioma.
J Clin Oncol. 29:330–336. 2011.
|
|
29
|
Chi DD, Merchant RE, Rand R, et al:
Molecular detection of tumor-associated antigens shared by human
cutaneous melanomas and gliomas. Am J Pathol. 150:2143–2152.
1997.PubMed/NCBI
|
|
30
|
Hegi ME, Diserens AC, Gorlia T, et al:
MGMT gene silencing and benefit from temozolomide in glioblastoma.
N Engl J Med. 352:997–1003. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hegi ME, Liu L, Herman LG, et al:
Correlation of O6-methylguanine methyltransferase (MGMT)
promoter methylation with clinical outcomes in glioblastoma and
clinical strategies to modulate MGMT activity. J Clin Oncol.
26:4189–4199. 2008.PubMed/NCBI
|
|
32
|
Quinn JA, Jiang SX, Reardon DA, et al:
Phase II trial of temozolomide plus O6-benzylguanine in
adults with recurrent, temozolomide-resistant maliganant glioma. J
Clin Oncol. 27:1262–1267. 2009.PubMed/NCBI
|
|
33
|
Natsume A, Wakabayashi T, Tsujimura K, et
al: The DNA demethylating agent 5-aza-2′-deoxycytidine activates
NY-ESO-1 antigenicity in orthotopic human glioma. Int J Cancer.
122:2542–2553. 2008.
|
|
34
|
Low J, Dowless M, Shiyanova T, et al:
Knockdown of cancer testis antigens modulates neural stem cell
marker expression in glioblastoma tumor stem cells. J Biomol
Screen. 15:830–839. 2010. View Article : Google Scholar : PubMed/NCBI
|