Introduction
Colorectal cancer (CRC) is the third most commonly
occurring and the second leading cause of cancer-related mortality
worldwide; ~1.8 million new CRC cases and 900,000 deaths are
reported annually. In addition, the incidence of CRC at a
relatively young age has begun to increase (1). With the deepening understanding of
antitumour immunity, it is being shown that immune factors are
crucial to outcomes of patients with cancer (2). However, previous studies have mainly
focused on the effect of adaptive immunity on CRC (3,4),
whereas studies on innate immunity are limited.
Mast cells are the progeny of haematopoietic stem
cells, identified as
CD4−CD8−CD19−CD14−CD117+FcεRI+
(5); mast cell progenitors (MCps)
circulate in the peripheral blood, reach the target organ through
chemoattraction to mediators, and then mature and eventually
differentiate in peripheral tissues (6). In 2016, Dahlin et al (7) first identified MCps as
CD4−CD8−CD19−CD14−CD34hiCD117+FcεRI+
cells. This discovery facilitated the quantification and
characterization of this rare cell population in healthy
individuals and patients with CRC.
Mast cells, as a group of innate immune cells, are
widely distributed in human tissues (8). Mast cells can release large amounts
of potent biologically active mediators and serve key roles in
angiogenesis, tissue remodelling and immune regulation (9). The effect of mast cell infiltration
on the tumour microenvironment has been widely studied (10–14).
Previous studies have focused on mast cell density, which was
identified by immunohistochemistry and is related to CRC prognosis
and local angiogenesis (15–19).
However, our understanding of the characteristics of circulating
MCps and tumour-infiltrating mast cells in CRC remains
inadequate.
In the present study, the MCp phenotype and the
changes in MCp distribution in patients with CRC were investigated
based on tumour progression.
Materials and methods
Human tissue samples
A total of 37 patients with newly diagnosed CRC were
recruited from the First Hospital of Jilin University (Changchun,
China) between July 2019 and April 2021. None of the participants
received chemotherapy or radiotherapy before surgery. Patients with
infectious disease, autoimmune disease or multiple primary cancers
were excluded. Tumour staging was based on the
Tumour-Node-Metastasis (TNM) cancer staging system of the American
Joint Committee for Cancer 2017 (20). All samples were pathologically
confirmed to be adenocarcinoma. A total of 15 pairs of fresh
intestinal tumour tissue (six from colon and nine from rectum) and
adjacent normal tissue (at least 5 cm distant from the tumour site)
were collected and separated by a professional surgeon. In
addition, 12 age- and sex-matched healthy control (HC) patients
were recruited; these patients had no other gastrointestinal
disease. A total of seven HC tissue control samples were obtained
from these patients who underwent a procedure for the treatment of
prolapse and haemorrhoids.
The patients with CRC were divided into two groups
according to TNM staging: 22 patients with stage I/II disease were
considered early stage, and the other 15 patients with stage III/IV
disease were considered advanced stage. All patients provided
written informed consent. The present study was approved (approval
no. 2018-464) by the Ethics Committee of The First Hospital of
Jilin University, and the experimental protocol was established
according to the guidelines of The Declaration of Helsinki.
Clinical examination
Clinical data including sex, age, clinical staging,
pathological grading and laboratory test results were obtained from
hospital records. The level of serum carcinoembryonic antigen (CEA)
was detected with an ADVIA Centaur XP immunoassay system (Siemens
AG).
Isolation of single cells
A total of 37 preoperative blood samples and 10
postoperative peripheral blood samples were collected. Peripheral
blood mononuclear cells were acquired by density gradient
centrifugation (800 × g, 30 min, 20°C) using Ficoll-Paque Plus
(Amersham; Cytiva).
Fresh intestinal tissue was repeatedly flushed with
0.9% normal saline. Samples were cut into 5-mm2 pieces.
The samples were placed in D-Hanks (Hank's Balanced Salt Solution
without Ca2+ and Mg2+; Beijing Solarbio
Science & Technology Co., Ltd.) containing DL-dithiothreitol,
ethylenediaminetetraacetic acid and 2-mercaptoethanol (all from
Sigma-Aldrich; Merck KGaA) and incubated for 20 min in a constant
temperature water bath at 37°C. Subsequently, the samples were
washed with D-Hanks 3–4 times to completely remove any residual
reagent. Then, the samples were digested with Hanks buffered saline
solution (Beijing Solarbio Science & Technology Co., Ltd.)
containing Liberase™ DL Research Grade and DNase I (both from
Sigma-Aldrich; Merck KGaA) for 20 min in a constant temperature
water bath at 37°C. The filtrate was collected using a cell
strainer (Falcon; Thermo Fisher Scientific, Inc.) to separate the
tissues and cell suspension, and then the cells were acquired by
centrifugation (300 × g, 10 min, 4°C).
Flow cytometric analysis
Isolated cells and the live/dead marker Fixable
Viability Stain 780 (BD Biosciences; 1 µl stain for 1 ml of cell
suspension at 1–10×106 cells/ml) were mixed and
incubated in the dark for 10 min at room temperature. Subsequently,
the cells were washed with phosphate-buffered saline (PBS); after
centrifugation (336 × g, 5 min, 4°C), the supernatant was
discarded. The cells were stained with anti-human CD45-BB515 HI30
(cat. no. 564585), anti-human CD4-APC-H7 RPA-T4 (cat. no. 560158),
anti-human CD8-APC-H7 SK1 (cat. no. 560179), anti-human CD14-APC-H7
M5E2 (cat. no. 561384), anti-human CD19-APC-H7 HIB19 (cat. no.
560727), anti-human CD34-APC 581 (cat. no. 555824), anti-human
CD117-BV421 104D2 (cat. no. 563856) and anti-human FcεR1α-PE AER-37
(cat. no. 566607) (all 1:100; all from BD Biosciences) antibodies
at room temperature for 30 min in the dark. After washing with PBS,
cells were examined on a CytoFLEX S flow cytometer (Beckman
Coulter, Inc.). The number of CD45+ cells/sample (at
least 500,000 events) was analysed using CytExpert software v. 2.0
(Beckman Coulter, Inc.).
Treatment and follow-up
All patients with primary CRC underwent surgery, and
peripheral blood samples were collected from 10 patients 7 days
after surgery. None of the 10 patients showed symptoms such as
fever after surgery, and they did not receive chemotherapy or
radiotherapy during this period.
Statistical analyses
The horizontal line in each figure represents the
mean and 95% CI of each group. Results in table were presented as
the median and minimum-maximum range. Differences between two
groups were analysed using independent Student's t-test or a
Mann-Whitney U test if appropriate. Statistical differences among
the four groups were analysed using the Kruskal-Wallis test with
the Dunnett's post hoc test. Receiver operating characteristic
(ROC) curve was calculated using SPSS. The Wilcoxon test was used
to compare groups before and after treatment. Correlation analysis
was performed with the Spearman's rank correlation test. SPSS
statistics v. 24.0 (IBM Corp.) was used for all statistical
analyses and GraphPad Prism v. 9.3.1 (GraphPad Software, Inc.) was
used to generate the graphs. P<0.05 was considered to indicate a
statistically significant difference.
Results
Patient characteristics
To investigate the distribution of circulating MCps
in patients with newly diagnosed CRC, a total of 37 patients with
CRC and 12 age- and sex-matched HCs were recruited; patient data
are presented in Table I. The 37
patients with CRC included 22 patients with early-stage disease and
15 patients with advanced-stage disease. There were no differences
in sex, age, or leukocyte levels among the three groups, and no
difference in tumour location was observed between the early-stage
and advanced-stage patients with CRC. Patients with advanced-stage
CRC had higher serum CEA levels compared with those with
early-stage CRC (P=0.0128). HC tissue, tumour tissue and adjacent
normal tissue from 15 patients with CRC were analysed in this
study.
 | Table I.Clinicopathological characteristics
of subjects. |
Table I.
Clinicopathological characteristics
of subjects.
|
|
| Blood | Tissue |
|---|
|
|
|
|
|
|---|
| Clinicopathological
characteristic | Healthy controls
(n=12) | Early CRC
(n=22) | Advanced CRC
(n=15) | Early CRC
(n=5) | Advanced CRC
(n=10) |
|---|
| Median age,
yearsa | 61.5 (55–69) | 64.5 (48–79) | 59 (47–82) | 56 (48–63) | 50.5 (49–75) |
|
≤60 | 6 | 8 | 9 | 4 | 7 |
|
>60 | 6 | 14 | 6 | 1 | 3 |
| Sex |
|
|
|
|
|
|
Male | 8 | 14 | 10 | 3 | 8 |
|
Female | 4 | 8 | 5 | 2 | 2 |
| Tumour
location |
|
|
|
|
|
|
Colon | NA | 6 | 6 | 2 | 4 |
|
Rectum | NA | 16 | 9 | 3 | 6 |
| TNM stage |
|
|
|
|
|
|
I/II | NA | 13 | 10 | 3 | 7 |
|
III/IV | NA | 9 | 5 | 2 | 3 |
| Serum CEA
(ng/ml)a | NA | 2.44
(0.20-38.47) | 5.13
(1.55-113.00)b | 1.11
(0.20-38.47) | 5.00
(1.55-113.00) |
| WBC count
(×109 cells/l)a | 5.44
(3.67-8.59) | 5.58
(2.78-12.00) | 5.92
(3.92-10.00) | 4.94
(4.79-5.77) | 5.90
(3.92-10.00) |
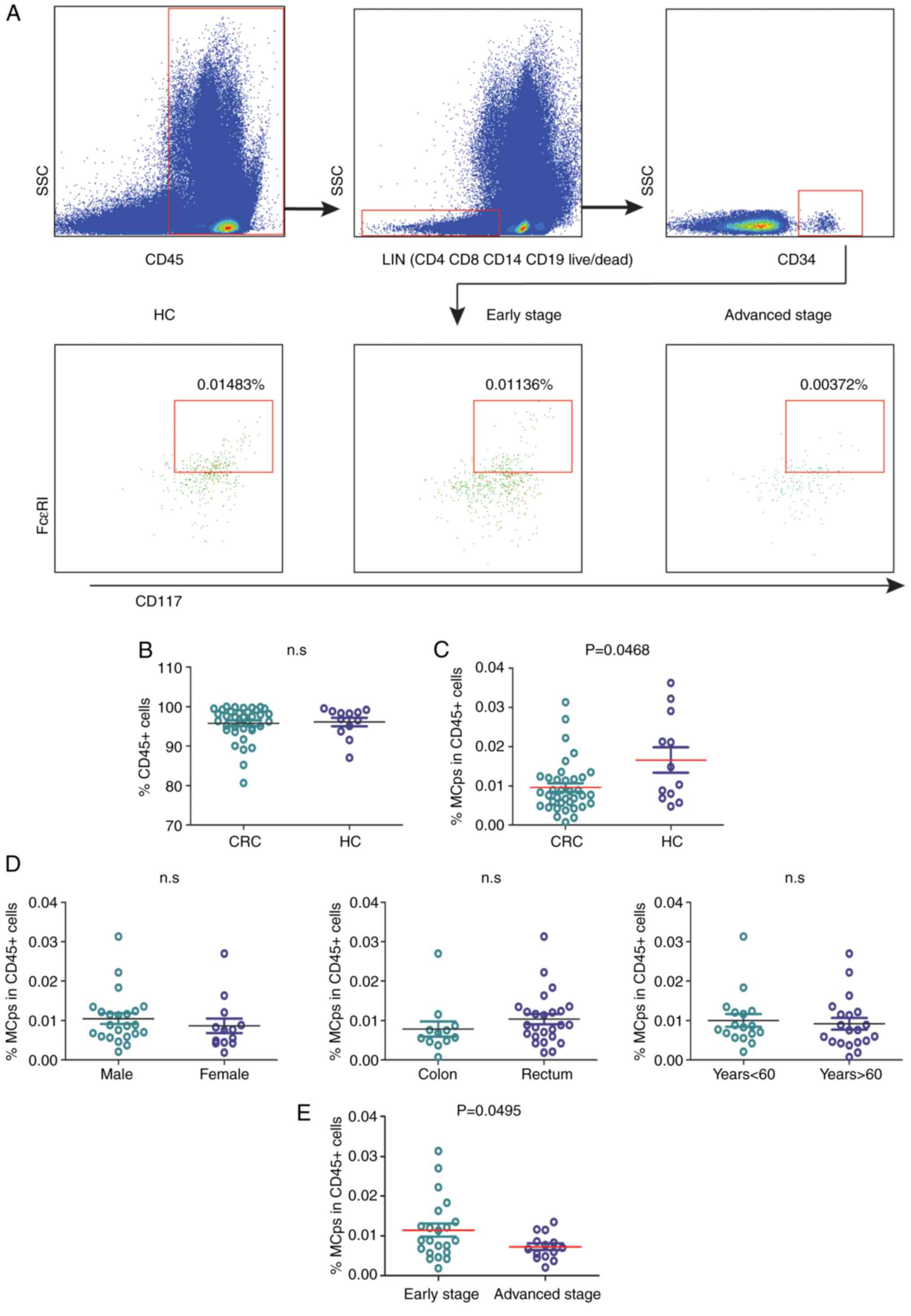
Frequency of circulating MCps is
decreased in patients with CRC and is related to CRC
progression
The MCp frequency in patients with CRC and HC
patients was analysed by flow cytometry (Fig. 1A). The patients with CRC and HCs
had similar percentages of CD45+ leukocytes in the
peripheral blood (Fig. 1B). The
frequency of MCps in patients with CRC was significantly lower
compared with that in HCs (P=0.0468; Fig. 1C). Age, sex and tumour location had
no influence on the quantification of MCps in patients with CRC
(Fig. 1D). Moreover, the MCp level
in patients with advanced-stage disease was lower compared with
that in patients with early-stage disease (P=0.0495; Fig. 1E).
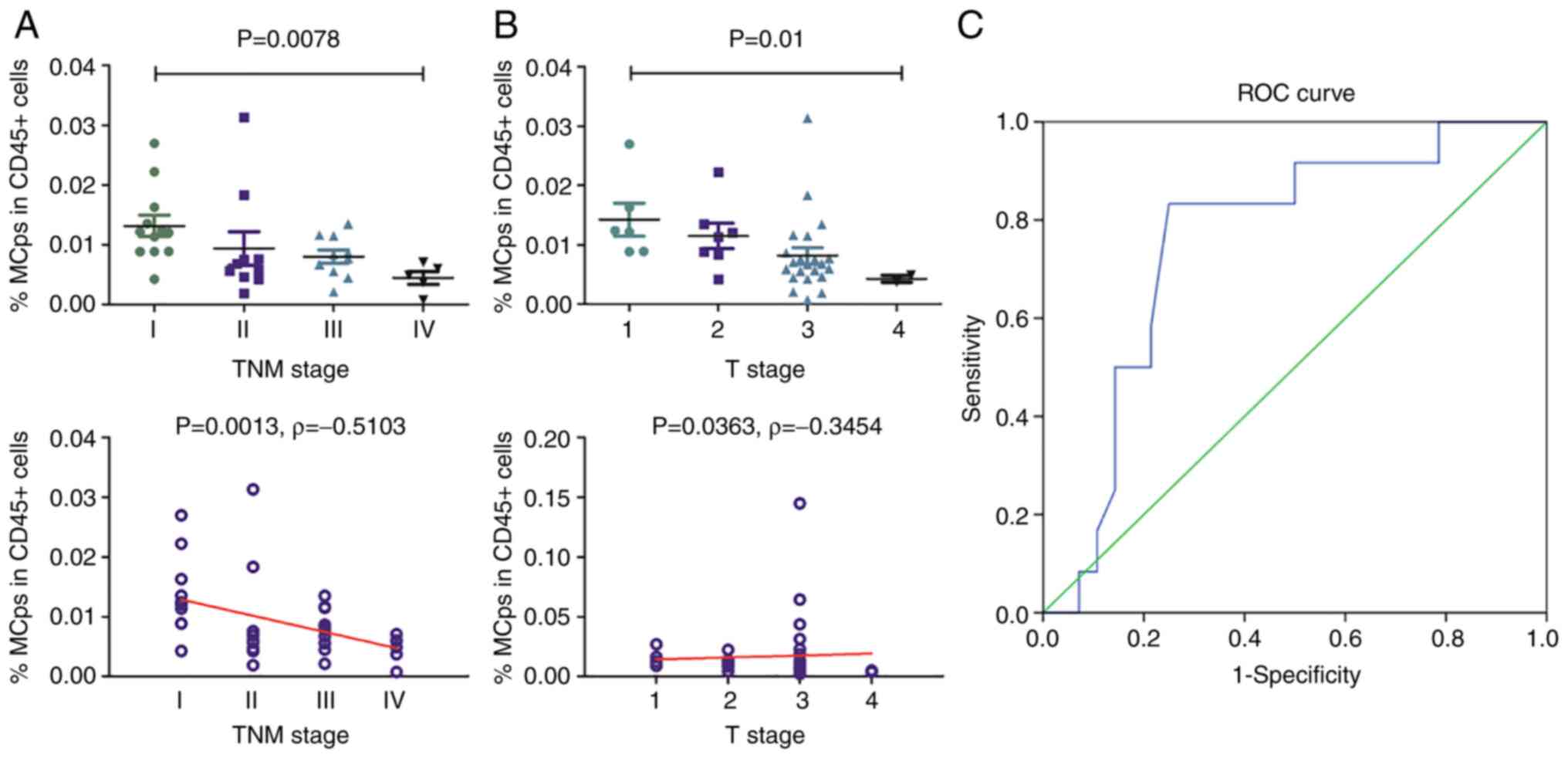
MCp frequency is related to CRC
progression
The relationship between MCp frequency and CRC
progression was analysed. It was revealed that the frequency of
circulating MCps was significantly associated with TNM stage
(P=0.0078; Fig. 2A) and the depth
of tumour invasion (P=0.01; Fig.
2B).
To assess whether MCps can be used for the
differentiation of CRC, receiver operating characteristic (ROC)
curves were plotted. It was identified that the frequency of
circulating MCps has certain reference value for the
differentiation of stage I CRC from other three stages of CRC
(P=0.011; AUC=0.756; Fig. 2C).
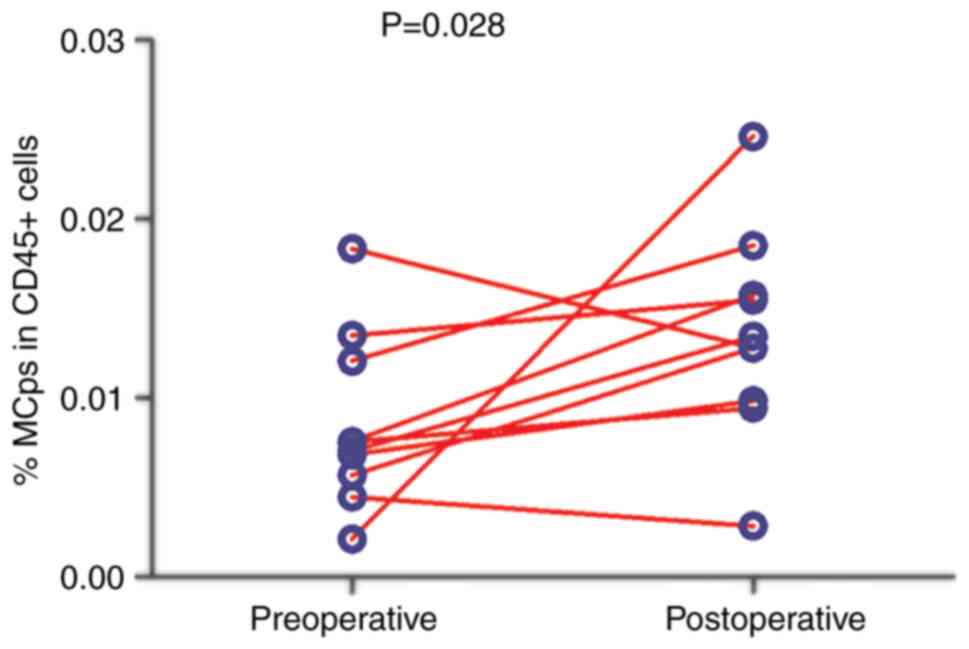
Frequency of circulating MCps in
patients with CRC following treatment
The effect of surgical treatment on circulating MCps
in patients with CRC was investigated. The preoperative and
postoperative (7 days after surgery) frequencies of circulating
MCps in 10 patients with CRC were compared. The frequency of
circulating MCps after treatment was significantly higher compared
with that before treatment (P=0.028; Fig. 3).
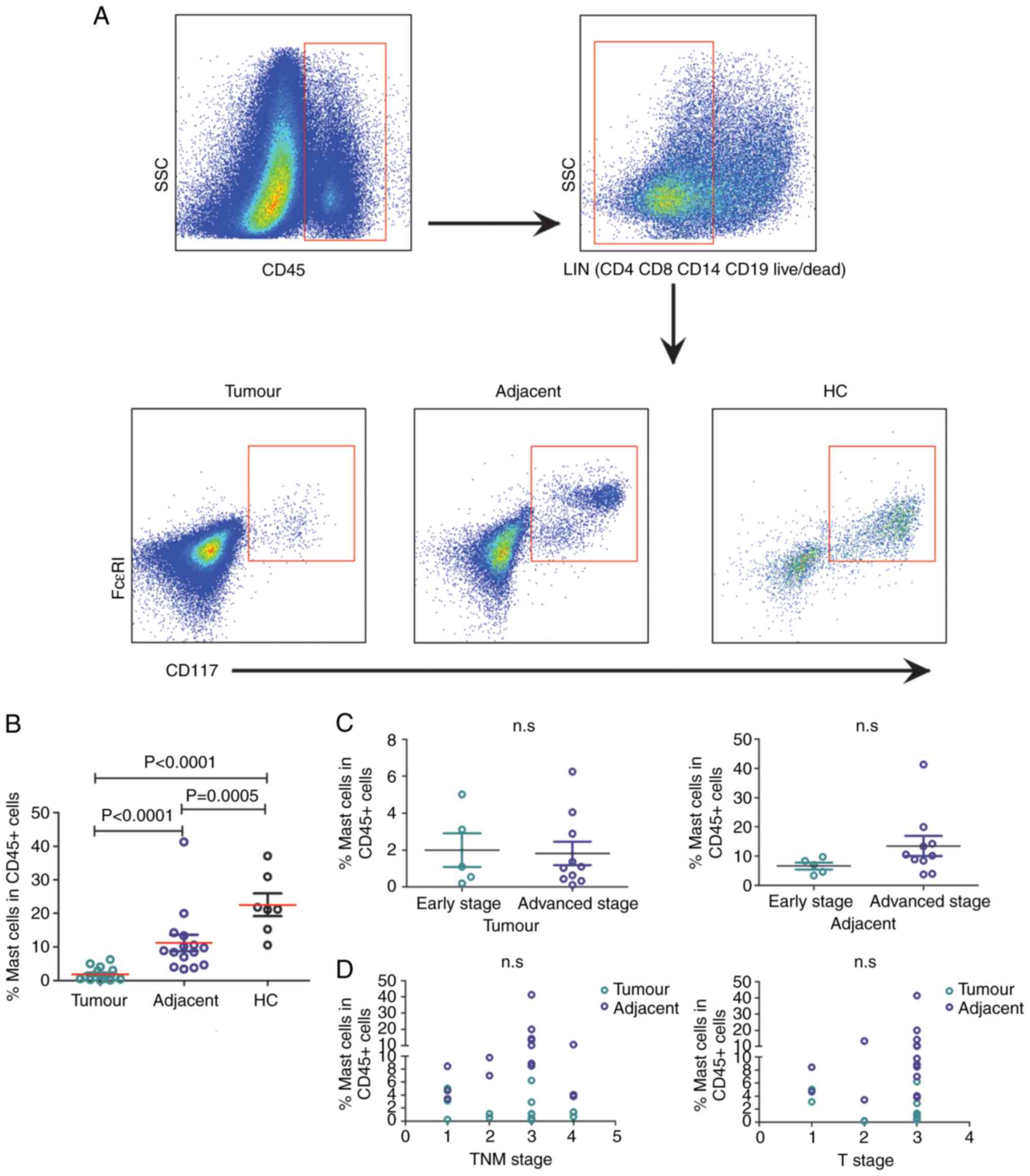
Frequency of mast cells infiltrating
tumour and adjacent normal tissues from patients with CRC
Finally, to explore whether the frequency of mast
cells in tissues changed during CRC progression, the percentage of
mast cells among the total CD45+ leukocyte population in
tumour and adjacent normal tissues from patients with CRC and HC
tissue was analysed using flow cytometry (Fig. 4A). Consistent with a previous study
(21), the frequency of mast cells
infiltrating in tumour tissue was significantly lower compared with
that in the adjacent normal tissue and HC tissue (both P<0.0001;
Fig. 4B). In addition, the
frequency of mast cells in adjacent normal tissue was significantly
lower compared with that in HC tissue (P=0.0005; Fig. 4B).
The frequency of mast cells in adjacent normal
tissue did not differ between early-stage and advanced-stage
patients (Fig. 4C). Additionally,
the frequency of mast cells in tumour and adjacent normal tissue
was not associated with T stage or TNM stage (Fig. 4D).
Discussion
By studying the phenotype, distribution and clinical
relevance of mast cells at different locations and in patients with
different stages of CRC, the present study comprehensively analysed
the characteristic changes in MCps and mast cells during CRC
progression from multiple perspectives. The data showed that the
frequency of circulating MCps was lower in patients with CRC and
was associated with TNM stage and T stage. This suggested that a
lower MCp level may reflect CRC progression. To the best of our
knowledge, this is the first study to systematically analyse the
changes of MCps and mast cells in the circulation and tissues of
patients with CRC.
Previous studies reported that interaction between
CRC cells and mast cells ultimately promotes tumour growth
(22,23). Mast cells can be divided into
immature circulating MCps and mature mast cells distributed in
tissues. MCps are direct precursors of mast cells in the peripheral
blood, and previous definitions of mast cell precursors have been
unclear (24,25). However, the definition of the
circulating MCp phenotype provides a new research direction
(6). The present results suggested
that age, sex and tumour location do not affect the frequency of
MCps in patients with CRC, but patients with CRC do have
significantly lower circulating MCp levels compared with HCs. More
importantly, patients with advanced-stage CRC were found to have
lower MCp levels compared with patients with early-stage CRC. With
increasing TNM stage and T stage, the proportion of circulating
MCps decreased significantly. It has been reported that a high
level of tumour stroma-infiltrating mast cells is an independent
unfavourable predictor in patients with muscle invasive bladder
cancer and biliary tract cancer (26,27).
Hence, it was concluded that the frequency of MCps may be an
independent indicator of aggressive CRC features in patients and,
in particular, may be used to distinguish early- and advanced-stage
patients with CRC.
Radical resection is the preferred treatment for the
majority of patients with CRC. A total of 10 patients with CRC were
followed up at 7 days following surgery, and it was observed that
after surgical treatment, the frequency of MCps increased
significantly. These data suggested that the frequency of MCps can
be used as an indicator to evaluate the effectiveness of
surgery.
Chronic low-grade inflammation is a hallmark of
cancer, and mast cells are an important part of this inflammation
(28). The role of mast cells in
the tissue microenvironment of CRC is an area of research interest.
A number of studies have suggested that the density of mast cells
is negatively correlated with disease outcomes in CRC (16–18,29),
whereas others hold the opposite view (30–32).
In addition to the influence of race (33), region (34) and other factors, such as age and
sex, we hypothesized that the method for detecting mast cells in
tissues may also be one of the reasons for this phenomenon. Mast
cells can be divided into tryptase-positive-only (MC T) and
tryptase-positive/chymase-positive (MC TC) subtypes depending on
the protease they contain. The subtype distribution also varies
according to the organ in which they are found (35). It was reported that in human CRC
tissues, the MC TC subtype accounts for ~75% of all mast cells.
Both mast cell types seem to serve an important role in CRC
pathogenesis (31). However,
previous studies on tumour mast cells mainly analysed the effect of
the MC T subtype on CRC prognosis (21,23).
In the present study, total mast cells were defined as
CD4−CD8−CD19−CD14−CD117+FcεRI+
(36) to investigate their
components and phenotypes in cancer tissues. Flow cytometry was
used to analyse the proportion of mature mast cells among
CD45+ leukocytes, and it was found that the frequency of
mast cells was highest in HC tissues, followed by adjacent normal
tissues and then tumour tissues, which was consistent with a
previous study (19). The
frequency of mast cells in both HC and adjacent normal tissues did
not reflect CRC progression.
In the present study, a lower frequency of
circulating MCps was observed in patients with CRC, particularly in
patients with advanced-stage disease. The frequency of MCps is
related to CRC progression, which may reflect aggressive CRC
features. Furthermore, according to the present data, the frequency
of mast cells in tissue did not reflect the severity of the
disease. There are certain limitations to the present study that
should be mentioned; for example, MC T and MC TC subtypes were not
detected by immunohistochemistry, thus total MC and MC T subtype
could not be compared simultaneously. The migration of MCps to the
intestine and the presence of mast cells in intestinal tissue after
surgery need to be further investigated. The present findings may
provide new insights into the role of mast cells in regulating CRC
processes.
Acknowledgements
We thank our colleagues at the First Hospital of
Jilin University (Changchun, China), they are Mr. Yue Yudong, M.M.,
for his help in sample collection, Ms. Lin Fangnan, M.M., for
discussions and Ms. Liu Jing, M.M., for assistance with FACS.
Funding
The present study was supported by The National Natural Science
Foundation of China (grant nos. 30972610, 81273240, 91742107 and
81570002), The National Key Research and Development Program (grant
nos. 2017YFC0910000 and 2017YFD0501300) and The Jilin Province
Science and Technology Agency (grant nos. JJKH20211164KJ,
JJKH20211210KJ, 20200403084SF, JLSWSRCZX2020-009, 20200901025SF,
20190101022JH, 2019J026, 20170622009JC, 2017C021, 2017J039,
SXGJXX2017-8, JJKH20180197KJ, DBXM154-2018 and
2018SCZWSZX-015).
Availability of data and materials
The datasets generated during and/or analysed during
the current study are available from the corresponding author upon
reasonable request.
Authors' contributions
All authors contributed to the study concept and
design as well as the interpretation of the data. PiZ, PeZ and RS
wrote the original draft and conducted the experiments. TT acquired
the samples and collated the data. YiJ wrote, reviewed and edited
the manuscript. AL and XH formally analysed and confirm the
authenticity of all the raw data. YaJ provided the resources, and
wrote, reviewed and edited the manuscript. All authors read and
approved the final manuscript and agree to be accountable for all
aspects of research in ensuring that the accuracy or integrity of
any part of the work are appropriately investigated and
resolved.
Ethics approval and consent to
participate
Written informed consent was obtained from each
participant. The experimental protocol was established according to
the guidelines of The Declaration of Helsinki and was approved by
the Human Ethics Committee of the First Hospital of Jilin
University (Changchun, China; approval no. 2018-464).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Keum N and Giovannucci E: Global burden of
colorectal cancer: Emerging trends, risk factors and prevention
strategies. Nat Rev Gastroenterol Hepatol. 16:713–732. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Galon J and Bruni D: Tumor Immunology and
tumor evolution: Intertwined histories. Immunity. 52:55–81. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
IJsselsteijn ME, Sanz-Pamplona R, Hermitte
F and de Miranda NFCC: Colorectal cancer: A paradigmatic model for
cancer immunology and immunotherapy. Mol Aspects Med. 69:123–129.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Schmitt M and Greten FR: The inflammatory
pathogenesis of colorectal cancer. Nat Rev Immunol. 21:653–667.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lv Y, Zhao Y, Wang X, Chen N, Mao F, Teng
Y, Wang T, Peng L, Zhang J, Cheng P, et al: Increased intratumoral
mast cells foster immune suppression and gastric cancer progression
through TNF-α-PD-L1 pathway. J Immunother Cancer. 7:542019.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hallgren J and Gurish MF: Mast cell
progenitor trafficking and maturation. Adv Exp Med Biol. 716:14–28.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dahlin JS, Malinovschi A, Öhrvik H,
Sandelin M, Janson C, Alving K and Hallgren J: Lin-CD34hi
CD117int/hi FcεRI+ cells in human blood constitute a rare
population of mast cell progenitors. Blood. 127:383–391. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Marone G, Galli SJ and Kitamura Y: Probing
the roles of mast cells and basophils in natural and acquired
immunity, physiology and disease. Trends Immunol. 23:425–427. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Maltby S, Khazaie K and McNagny KM: Mast
cells in tumor growth: Angiogenesis, tissue remodelling and
immune-modulation. Biochim Biophys Acta. 1796:19–26.
2009.PubMed/NCBI
|
|
10
|
Komi DEA and Redegeld FA: Role of mast
cells in shaping the tumor microenvironment. Clin Rev Allergy
Immunol. 58:313–325. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nagata M, Shijubo N, Walls AF, Ichimiya S,
Abe S and Sato N: Chymase-positive mast cells in small sized
adenocarcinoma of the lung. Virchows Arch. 443:565–573. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mangia A, Malfettone A, Rossi R, Paradiso
A, Ranieri G, Simone G and Resta L: Tissue remodelling in breast
cancer: Human mast cell tryptase as an initiator of myofibroblast
differentiation. Histopathology. 58:1096–1106. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ranieri G, Ammendola M, Patruno R, Celano
G, Zito FA, Montemurro S, Rella A, Di Lecce V, Gadaleta CD,
Battista De Sarro G and Ribatti D: Tryptase-positive mast cells
correlate with angiogenesis in early breast cancer patients. Int J
Oncol. 35:115–120. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Guo X, Zhai L, Xue R, Shi J, Zeng Q and
Gao C: Mast cell tryptase contributes to pancreatic cancer growth
through promoting angiogenesis via activation of angiopoietin-1.
Int J Mol Sci. 17:8642016. View Article : Google Scholar
|
|
15
|
Ammendola M, Sacco R, Sammarco G, Donato
G, Montemurro S, Ruggieri E, Patruno R, Marech I, Cariello M, Vacca
A, et al: Correlation between serum tryptase, mast cells positive
to tryptase and microvascular density in colo-rectal cancer
patients: Possible biological-clinical significance. PLoS One.
9:e995122014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gulubova M and Vlaykova T: Prognostic
significance of mast cell number and microvascular density for the
survival of patients with primary colorectal cancer. J
Gastroenterol Hepatol. 24:1265–1275. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Malfettone A, Silvestris N, Saponaro C,
Ranieri G, Russo A, Caruso S, Popescu O, Simone G, Paradiso A and
Mangia A: High density of tryptase-positive mast cells in human
colorectal cancer: A poor prognostic factor related to
protease-activated receptor 2 expression. J Cell Mol Med.
17:1025–1037. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Suzuki S, Ichikawa Y, Nakagawa K, Kumamoto
T, Mori R, Matsuyama R, Takeda K, Ota M, Tanaka K, Tamura T and
Endo I: High infiltration of mast cells positive to tryptase
predicts worse outcome following resection of colorectal liver
metastases. BMC Cancer. 15:8402015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Acikalin MF, Oner U, Topçu I, Yaşar B,
Kiper H and Colak E: Tumour angiogenesis and mast cell density in
the prognostic assessment of colorectal carcinomas. Dig Liver Dis.
37:162–169. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Amin MB, Gress DM, Meyer Vega LR, Edge SB,
Greene FL, Byrd DR, Brookland RK, Washington MK and Compton CC:
AJCC Cancer Staging Manual. 8th edition. Springer; New York, NY:
2017, View Article : Google Scholar
|
|
21
|
Xia Q, Wu XJ, Zhou Q, Jing-Zeng .Hou JH,
Pan ZZ and Zhang XS: No relationship between the distribution of
mast cells and the survival of stage IIIB colon cancer patients. J
Transl Med. 9:882011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yu Y, Blokhuis B, Derks Y, Kumari S,
Garssen J and Redegeld F: Human mast cells promote colon cancer
growth via bidirectional crosstalk: Studies in 2D and 3D coculture
models. Oncoimmunology. 7:e15047292018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gounaris E, Erdman SE, Restaino C, Gurish
MF, Friend DS, Gounari F, Lee DM, Zhang G, Glickman JN, Shin K, et
al: Mast cells are an essential hematopoietic component for polyp
development. Proc Natl Acad Sci USA. 104:19977–19982. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Dahlin JS and Hallgren J: Mast cell
progenitors: Origin, development and migration to tissues. Mol
Immunol. 63:9–17. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Drew E, Huettner CS, Tenen DG and McNagny
KM: CD34 expression by mast cells: Of mice and men. Blood.
106:1885–1887. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Liu Z, Zhu Y, Xu L, Zhang J, Xie H, Fu H,
Zhou Q, Chang Y, Dai B and Xu J: Tumor stroma-infiltrating mast
cells predict prognosis and adjuvant chemotherapeutic benefits in
patients with muscle invasive bladder cancer. Oncoimmunology.
7:e14743172018. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Bo X, Wang J, Suo T, Ni X, Liu H, Shen S,
Li M, Wang Y, Liu H and Xu J: Tumor-infiltrating mast cells predict
prognosis and gemcitabine-based adjuvant chemotherapeutic benefit
in biliary tract cancer patients. BMC Cancer. 18:3132018.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Varricchi G, Galdiero MR, Loffredo S,
Marone G, Iannone R, Marone G and Granata F: Are mast cells MASTers
in cancer? Front Immunol. 8:4242017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hu G, Wang S and Cheng P:
Tumor-infiltrating tryptase(+) mast cells predict unfavorable
clinical outcome in solid tumors. Int J Cancer. 142:813–821. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Mehdawi L, Osman J, Topi G and Sjölander
A: High tumor mast cell density is associated with longer survival
of colon cancer patients. Acta Oncol. 55:1434–1442. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Tan SY, Fan Y, Luo HS, Shen ZX, Guo Y and
Zhao LJ: Prognostic significance of cell infiltrations of
immunosurveillance in colorectal cancer. World J Gastroenterol.
11:1210–1214. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Nielsen HJ, Hansen U, Christensen IJ,
Reimert CM, Brünner N and Moesgaard F: Independent prognostic value
of eosinophil and mast cell infiltration in colorectal cancer
tissue. J Pathol. 189:487–495. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Curran T, Sun Z, Gerry B, Findlay VJ,
Wallace K, Li Z, Paulos C, Ford M, Rubinstein MP, Chung D and Camp
ER: Differential immune signatures in the tumor microenvironment
are associated with colon cancer racial disparities. Cancer Med.
10:1805–1814. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Xu K, Miao L, Chen W, Wu H, Gong Y, Tu X,
Gou W, Pan B, Qu C, Wu X and Wang B: Establishment of the reference
intervals of lymphocyte subsets for healthy Chinese Han adults and
its influencing factors. Ann Transl Med. 9:14952021. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Wernersson S and Pejler G: Mast cell
secretory granules: Armed for battle. Nat Rev Immunol. 14:478–494.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Huber M, Cato ACB, Ainooson GK, Freichel
M, Tsvilovskyy V, Jessberger R, Riedlinger E, Sommerhoff CP and
Bischoff SC: Regulation of the pleiotropic effects of
tissue-resident mast cells. J Allergy Clin Immunol. 144 (Suppl
4):S31–S45. 2019. View Article : Google Scholar : PubMed/NCBI
|