Introduction
The extraction of mandibular impacted third molars,
a routine outpatient surgery performed by oral and maxillofacial
surgeons, is associated with common complications, such as trismus,
pain and infection (1). The most
severe cases of trismus usually occur at 2 days post-operatively.
The primary causes include elevation of flap beyond the external
oblique ridge, low-grade infection following local anesthesia and
repeated stimulation of the medial pterygoid muscle (inferior
alveolar nerve block), as well as other causes (2). The symptom of trismus is alleviated
by the post-operative local injection of dexamethasone (3,4).
Generally, trismus is gradually alleviated or disappears within
approximately 1 to 2 weeks post-operatively; however, in very rare
cases, trismus persists for >1 month. The present study reports
the case of a patient who exhibited trismus for 45 days following
mandibular third molar extraction. The patient received local and
systemic anti-inflammatory treatment, as well as incision and
drainage therapy under local anesthesia. Furthermore, the factors
associated with the occurrence and development of trismus were also
analyzed, and appropriate management strategies are discussed in
order to provide an effective treatment method for affected
patients, as well as to prevent the occurrence of trismus in the
future.
Case report
Initial presentation and
treatment
A 30-year-old male patient visited the Department of
Oral and Maxillofacial Surgery, the Stomatological Hospital,
Southern Medical University (Guangzhou, China) for the treatment of
edema and pain around the crown of the left third molar that had
lasted for >6 months. Informed consent was obtained from the
patient for his participation in the study and for publishing the
relevant clinical data. A clinical examination revealed that tooth
38 had partly erupted and was covered by a distal gingiva flap,
which was slightly red and swollen. The surface caries of tooth 38
extended to the dentin layer and were accompanied by transient
sensitivity to cold stimulation. There were no abnormalities in
terms of probing, percussion, mobility, or mouth opening; panoramic
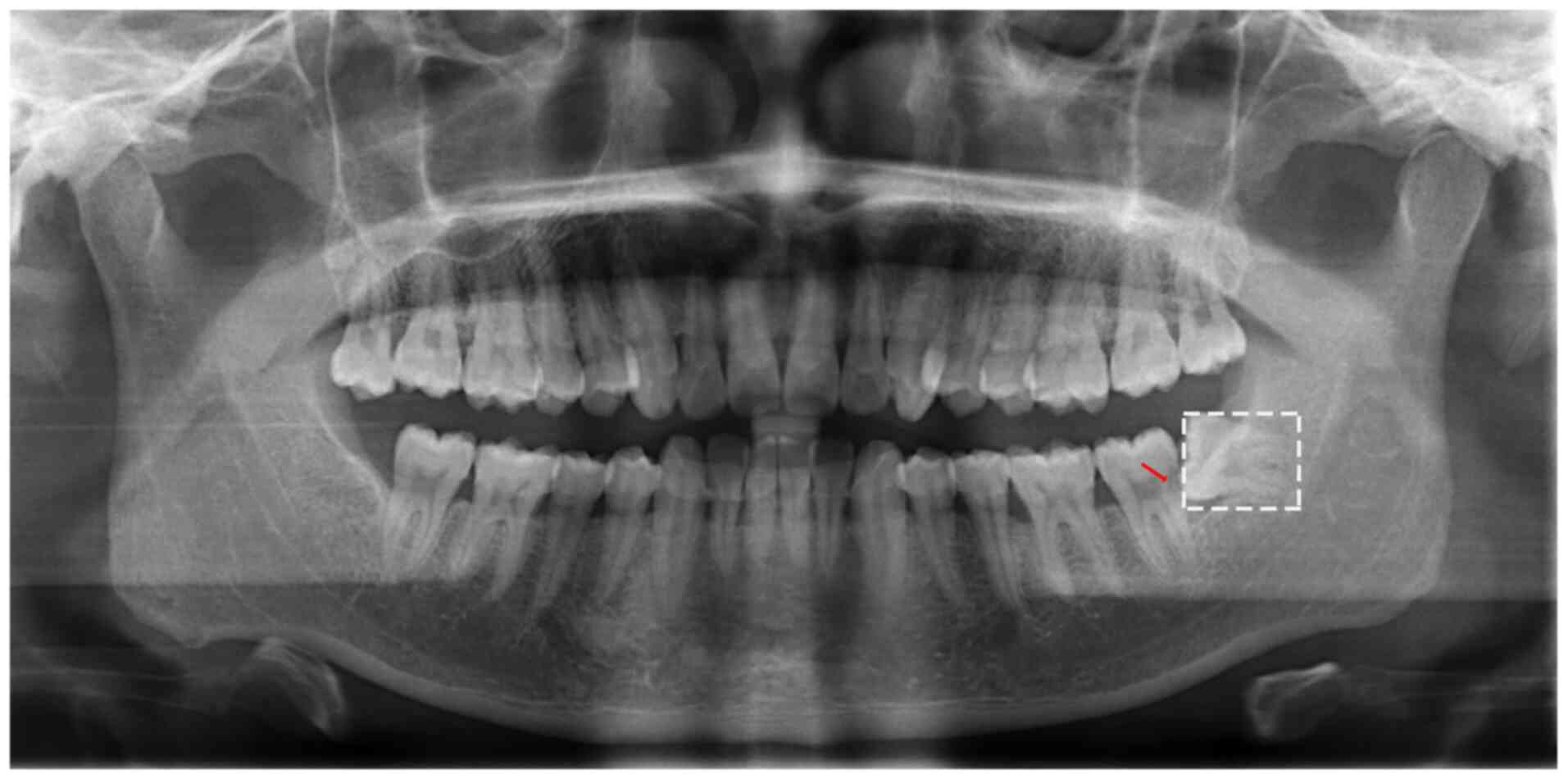
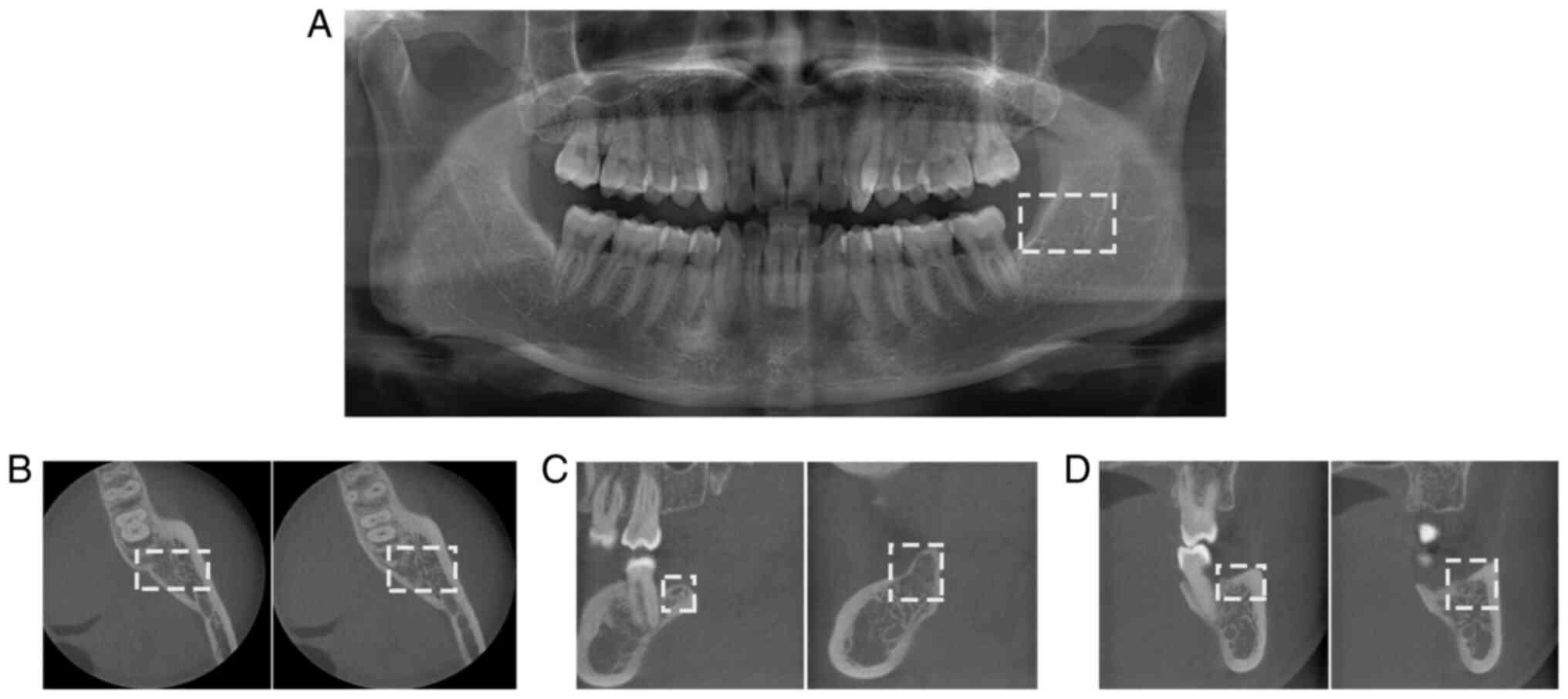
X-ray imaging revealed the mesioangular impaction of tooth 38
(Fig. 1, white rectangular region)
and distocervical low density in the area of tooth 37 (Fig. 1, red arrow). On the day of the
initial visit, according to the guidelines for the treatment of
mandibular third molars, patient symptoms are designated as present
and attributable to the third molar (5), the extraction of the affected tooth
was performed following iodophor disinfection in the area of tooth
38. Under inferior alveolar nerve block and infiltration anesthesia
(methylpiperazine hydrochloride/epinephrine), the flap was turned
and a dynamic bone drilling system was used to separate the crown
from the root. Thus, tooth 38 was extracted and the alveolar fossa
was scraped to remove inflamed tissue. Normal saline was used to
rinse the socket and the wound was closed with tight stitching to
achieve hemostasis. During the surgery, both the tooth and lingual
bone plate was removed together as the tooth root was adhered to
the lingual bone plate. The extraction procedure lasted for
approximately 30 min; the patient was instructed to take
anti-inflammatory (0.375 g cefaclor sustained-release tablets) and
detumescence (0.75 mg dexamethasone tablets) drugs for 3 days
post-operatively.
Occurrence of trismus
At 8 days post-operatively, the patient returned for
a routine follow-up. A clinical examination revealed slight trismus
(the distance of the incisal edges between the upper and lower
incisor was approximately 28 mm). No obvious edema or pain were
observed in the surgical area and normal wound healing was
observed. The sutures were removed following iodophor disinfection
and the wound was cleaned with normal saline. The patient was
instructed to perform mouth-opening training with a hot compress
and physiotherapy. Finally, the patient was provided oral hygiene
education and asked to return for clinical follow-up when he
experienced discomfort mainly due to slight trismus.
At 30 days post-operatively, the patient presented
with trismus which had not disappeared; it had gradually worsened
after self-opening training. A clinical examination revealed that
the wound in the area of tooth 38 was covered with food residue;
the surrounding soft tissue was red and swollen. There was no sign
of pyorrhea in the area of tooth 38. The buccal mucosa was swollen
and a sensation of motion was not obvious. The extent of mouth
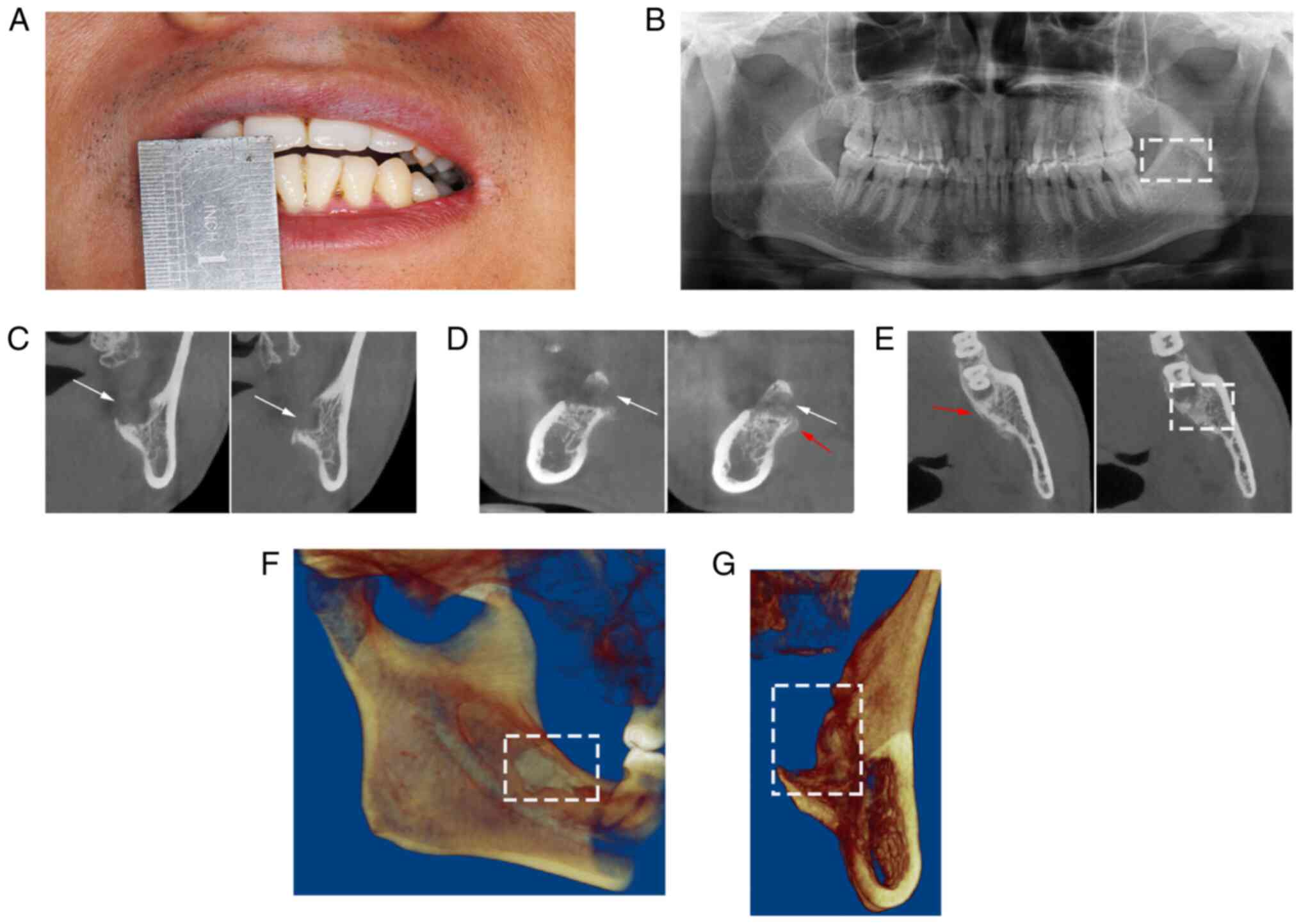
opening was approximately 2 mm (Fig.
2A), indicating more severe trismus; this was accompanied by
slight pain under the left jaw on palpation of swollen lymph nodes.
No obvious abnormalities were observed in a routine blood
examination (Table I). Panoramic
X-ray imaging demonstrated reduced bone density in the left
mandible (Fig. 2B, white
rectangular region) and tight occlusion of anterior teeth without a
gap. Cone beam computed tomography (CBCT) could not clearly discern
the repair to bone in the alveolar fossa of tooth 38 (Fig. 2C-E). The lingual bone plate in the
root tip area was missing (Fig. 2C
and D, white arrows) and the
3-dimensional reconstruction of the CBCT images also revealed the
absence of the lingual bone plate (Fig. 2F and G, white rectangular region); moreover,
obvious lamellar periosteal hyperplasia was present in the
corresponding area (Fig. 2D and
E, red arrows). Some areas of the
lingual bone plate were slightly rough (Fig. 2E, white rectangular region), and
the soft tissue gap was difficult to discern in the bottom of the
left side of the mouth. These radiological features indicated the
marginal osteomyelitis of the left mandible. As the sensation of
motion was not obvious and the patient exhibited severe trismus, no
surgery could be performed inside the mouth. Therefore, the
following local treatment was applied: The area of tooth 38 was
cleaned with hydrogen peroxide and normal saline; subsequently,
systemic anti-inflammatory treatment was administered intravenously
for 3 days (Table II).
 | Table IRoutine blood examination results. |
Table I
Routine blood examination results.
| Parameter | Value | Reference range | Unit |
|---|
| White blood cell
count | 7.6 | 3.5-9.5 | 109/l |
| Lymphocyte count | 2.4 | 0.8-4.0 | 109/l |
| Neutrophil count | 0.3 | 0.1-1.5 | 109/l |
| Neutrophilic
granulocyte count | 4.9 | 2.0-7.0 | 109/l |
| Percentage of
lymphocytes | 32.2 | 20.0-40.0 | % |
| Percentage of
neutrophils | 3.8 | 3.0-15.0 | % |
| Percentage of
neutrophilic granulocytes | 64.0 | 50.0-70.0 | % |
| Red blood cell
count | 5.04 | 4.30-5.80 |
1012/l |
| Hemoglobin level | 159 | 130-175 | g/l |
| Hematocrit level | 45.6 | 40.0-54.0 | % |
| Mean corpuscular
volume | 90.5 | 80.0-100.0 | fl |
| Mean corpuscular
hemoglobin | 31.5 | 27.0-34.0 | pg |
| Concentration of mean
corpuscular hemoglobin | 348 | 320-360 | g/l |
| Red blood cell
distribution width, coefficient of variation | 12.9 | 11.0-16.0 | % |
| Red blood cell
distribution width, standard deviation | 42.5 | 35.0-56.0 | % |
| Platelet count | 174 | 125-350 | 109/l |
| Mean platelet
volume | 8.2 | 6.5-12.0 | fl |
| Platelet distribution
width | 15.7 | 9.0-17.0 | fl |
| Plateletcrit
level | 0.142 | 0.108-0.282 | fl |
 | Table IIDetails of systemic anti-inflammatory
treatment administered intravenously for 3 days. |
Table II
Details of systemic anti-inflammatory
treatment administered intravenously for 3 days.
| Treatment | Dose | Frequency | Days |
|---|
| 0.9% sodium chloride
injection | 100 ml | Twice daily | 3 |
| Clindamycin phosphate
for injection | 0.6 g | Twice daily | 3 |
| 5% glucose and sodium
chloride injection | 250 ml | Once daily | 3 |
| Vitamin C
injection | 2 g | Once daily | 3 |
| Dexamethasone
phosphate sodium injection | 5 mg | Once daily | 3 |
| Ornidazole and sodium
chloride injection | 0.5 g | Once daily | 3 |
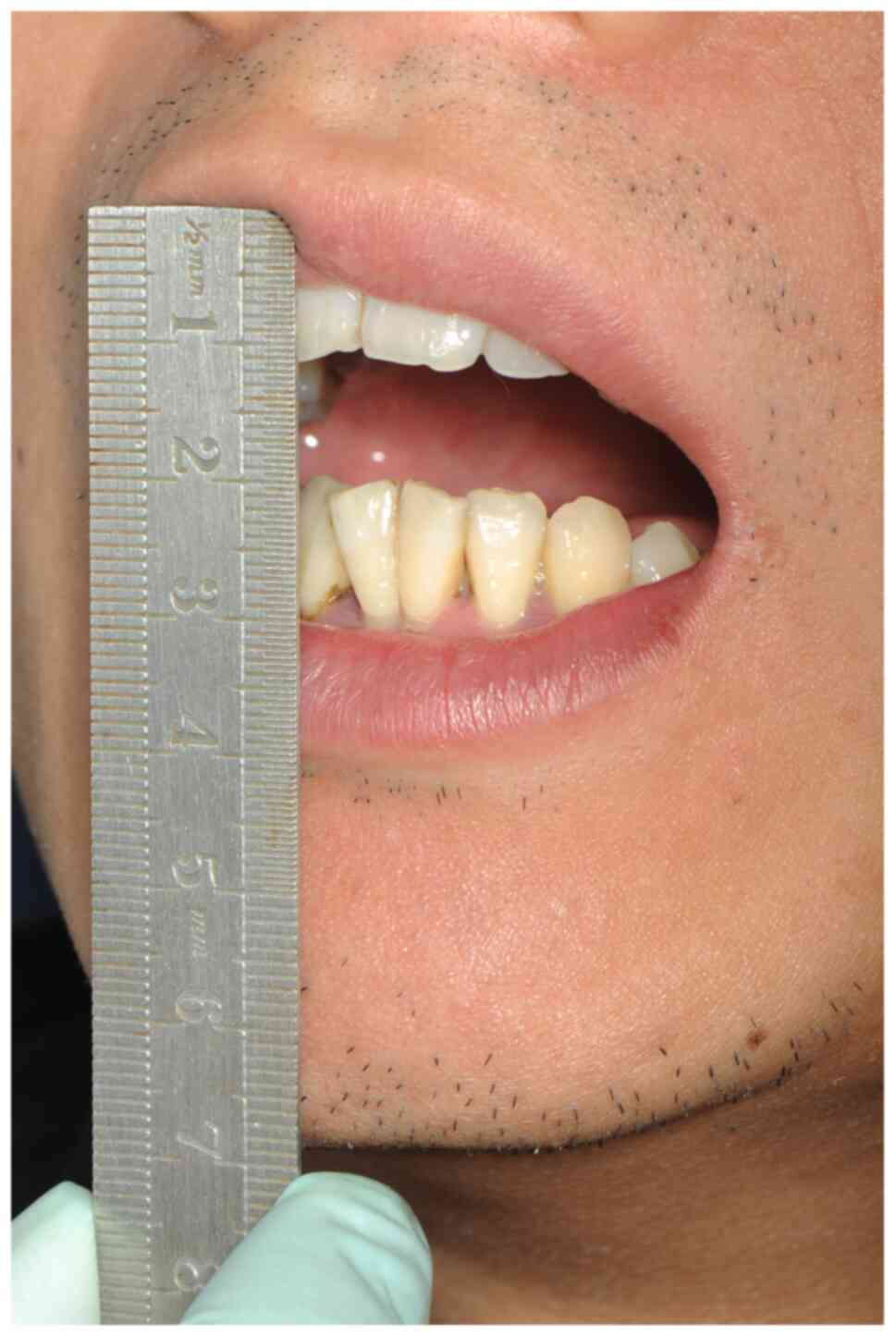
Following 3 days of systemic anti-inflammatory
treatment, there was a slight improvement in the trismus symptom of
the patient; edema and pain had faded in the left submandibular
region, and the extent of mouth opening was approximately 10 mm
(Fig. 3). There was an obvious
motion sensation in the area of tooth 38, although no evacuation
from the periodontium or other fistulas was observed. Under local
infiltration anesthesia with methylpiperazine
hydrochloride/epinephrine, the oral mucosa in the area of tooth 38
was treated with incision and drainage, causing discharge of a
large volume of bloody exudate. Inflammatory tissue was scraped
from the wound; considerable volumes of ornidazole and sodium
chloride injection, as well as normal saline, were used to clean
and wash the wound in an alternating manner.
Resolution of trismus
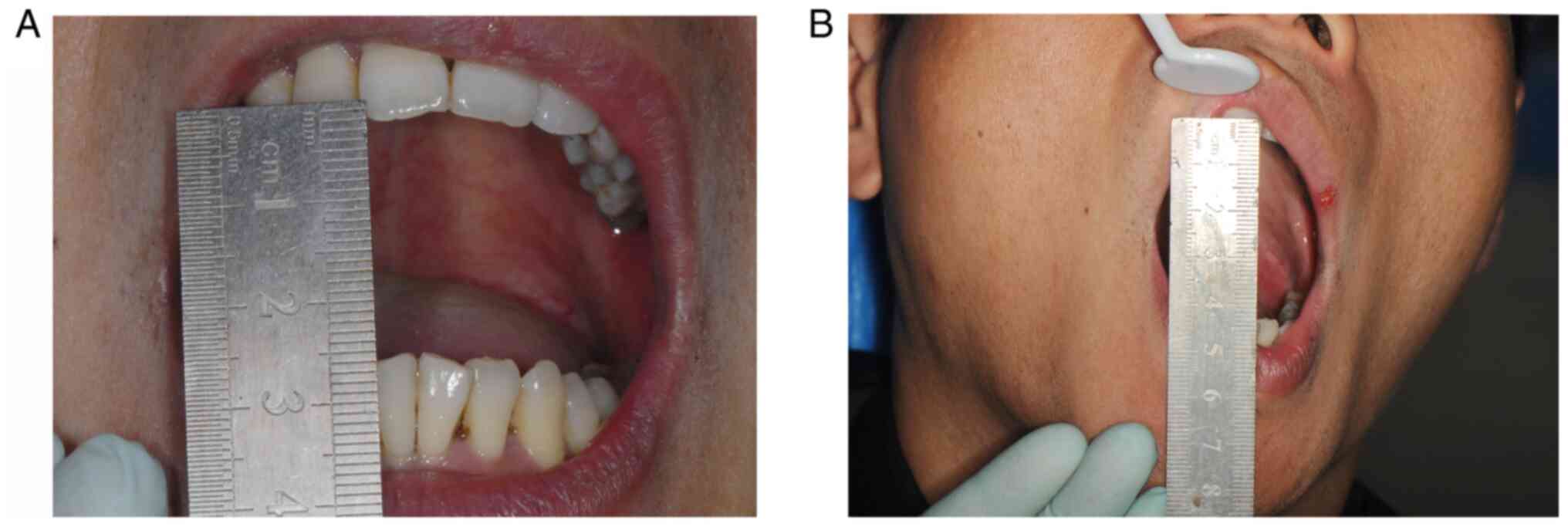
At 42 days post-operatively, the patient returned
for follow-up and presented alleviation of trismus. The extent of
mouth opening was approximately 25 mm, indicating slight trismus
(Fig. 4A). The soft tissue
demonstrated healing without any sign of pain after palpation. An
occlusal pad was placed to achieve compulsory mouth opening; the
extent of passive mouth opening was approximately 38 mm (Fig. 4B). At 1 year post-operatively, the
patient presented no discomfort. No obvious abnormalities were
found in clinical examination. Panoramic X-ray imaging (Fig. 5A, white rectangular region) and
CBCT (Fig. 5B-D, white rectangular
regions) revealed new bone formation in the alveolar fossa within
the area of tooth 38.
Discussion
The extraction of third molars can easily lead to
tissue injury, inflammation and other post-operative complications,
among which trismus is one of the most common (1). It is closely related to
post-operative edema, and is typically substantially alleviated or
disappeared within 1 to 2 weeks post-operatively. A number of
factors may contribute to the onset of trismus. For example, during
the extraction of mandibular third molar from the buccal side, the
muscle tendon may be severed; this painful stimulus causes muscle
protection, which results in trismus (2). Moreover, during inferior alveolar
nerve block anesthesia, masticatory muscle spasms may be caused by
incomplete disinfection and infection. Brooke (6) reported that multiple needle
injections during anesthesia may cause inflammation in that area,
while the stretching of intraoral muscles and muscle spasms may be
elicited by the use of narcotic drugs. However, the symptoms of
progressive trismus in the patient presented herein were not
greatly affected by the above factors.
Early during the course of the disease, the patient
of the present study exhibited mild trismus. However, this did not
receive extensive monitoring as it was presumed to be related to
postoperative edema and anxiety. However, when more severe trismus
was observed in combination with marginal osteomyelitis, the
attending physician intervened with a treatment plan for management
of marginal osteomyelitis. Due to the delayed diagnosis by the
attending physician, the disease treatment was delayed, which
affected the patient's post-operative recovery and daily
activities. Based on the intraoperative findings, the absence of
the lingual bone plate in the apical region was presumed to be the
main cause of marginal osteomyelitis. It was hypothesized that the
following was the possible cause of trismus: An infection after
tooth extraction spreads along the lingual space of the mandible.
Inflammatory mediators can cause irritation associated with muscle
tendon attachment to the mandibular ramus and the anterior section
of the medial pterygoid muscle, thereby resulting in masticatory
muscle spasms that lead to trismus.
For the patient in the present study, at 33 days
post-operatively, the surgeon performed incision and drainage in
the area of tooth 38 to eliminate a large amount of bloody exudate.
The progressive trismus was presumed to result from long-term
contact between low-toxicity inflammatory exudate and the muscle
tendon. Tight suturing had been performed at the end of surgery.
Notably, the inflammatory exudate could not drain with sufficient
speed; thus, it spread along the lingual space of the mandible and
interacted with the medial pterygoid muscle, which caused fascial
space infection associated with marginal mandibular osteomyelitis.
Treatment of chronic osteomyelitis has been a major focus in the
field of maxillofacial surgery; the main sources of chronic
osteomyelitis include odontogenic infection and tooth
extraction-related infection (7).
Bamberger encouraged the use of systemic antibiotic treatment for 4
weeks post-operatively to manage chronic osteomyelitis; using this
approach, surgical treatment was suggested to be unnecessary
(8). By contrast, Baur et
al (7) reported that surgical
treatment was generally more effective than single drug treatment;
moreover, conservative drug treatment often leads to multiple
recurrences of chronic osteomyelitis. For the patient presented
herein, the incision and drainage in the area of tooth 38 achieved
ideal results by combination with drug treatment; this was
potentially due to the fact that the patient was a young adult with
robust overall health and the drainage of inflammatory exudate was
performed relatively rapidly. Importantly, long-term follow-up was
necessary for our patient.
Tolstunov et al (9) found that the thickness of the lingual
bone plate of mesial or horizontal impacted mandibular third molars
was thinner than that of vertical impacted mandibular third molars;
thus, they stated that the lingual bone plate should be protected
during tooth extraction procedures. Lang et al (10) reported that the post-operative use
of antibiotics could effectively reduce the incidence of infection.
If tooth extraction causes extensive trauma and a large volume of
blood is lost, a drainage strip should be placed in the wound for 1
day to prevent infection. This approach also may aid reducing
postoperative edema of the patient's cheek. However, some studies
have demonstrated that when the mandibular third molar is tilted to
the lingual side, less post-operative inflammation will occur when
the lingual approach is used to remove the lingual bone plate,
compared with the buccal approach; thus, edema and pain will be
significantly reduced (11,12).
Accordingly, during the extraction of impacted third mandibular
molars, protection of the soft and hard tissues around the buccal
and lingual sides should be prioritized and trauma should be
minimized to avoid unnecessary injury. When fracture or loss of a
lingual bone plate occurs, close monitoring should be performed
during follow-up to ensure timely management of symptoms.
In conclusion, the extraction of an impacted
mandibular third molar is a very common oral surgery procedure.
During the surgery, the surgical area should be protected, and
careful assessment is necessary regarding fracture or loss of the
lingual bone plate. Effective drainage of inflammatory exudates
should be performed to prevent muscle spasms and trismus caused by
chronic contact with low-toxicity inflammatory exudates.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Sun Yat-Sen
Scientific Research Launch Project (grant no. YXQH201901), the
Natural Science Foundation of Guangdong Province, China (grant no.
2018A0303130106 and 2018A030313759).
Availability of data and materials
The data used during the present study are available
from the corresponding author on reasonable request.
Authors' contributions
YZ, PZ, BJ, ZW and ZZ conceived the case report,
wrote the initial manuscript and reviewed the final manuscript. JX,
QC, LN, ZW and ZZ interpreted and created the clinical and
radiographic images, and reviewed the final manuscript. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The patient provided informed consent for his
involvement in the present study.
Patient consent for publication
The patient provided informed consent for the
publishing of the relevant clinical data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bui CH, Seldin EB and Dodson TB: Types,
frequencies, and risk factors for complications after third molar
extraction. J Oral Maxillofac Surg. 61:1379–1389. 2003.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Balakrishnan G, Narendar R, Kavin T,
Venkataraman S and Gokulanathan S: Incidence of trismus in
transalveolar extraction of lower third molar. J Pharm Bioallied
Sci. 9 (Suppl 1):S222–S227. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Gülnahar Y and Kupeli I: Effect of
preemptive intravenous ibuprofen on postoperative edema and trismus
in third molar tooth extraction: A randomized controlled study. J
Dent Anesth Pain Med. 18:161–167. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Li C, Men Y and Li L: Discrepancies on
dexamethasone for trismus after third molar extraction. Oral Surg
Oral Med Oral Pathol Oral Radiol. 117(253)2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Steed MB: The indications for third-molar
extractions. J Am Dent Assoc. 145:570–573. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Brooke RI: Postinjection trismus due to
formation of fibrous band. Oral Surg Oral Med Oral Pathol.
47:424–426. 1979.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Baur DA, Altay MA, Flores-Hidalgo A, Ort Y
and Quereshy FA: Chronic osteomyelitis of the mandible: Diagnosis
and management-an institution's experience over 7 years. J Oral
Maxillofac Surg. 73:655–665. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Bamberger DM: Diagnosis and treatment of
osteomyelitis. Compr Ther. 26:89–95. 2000.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Tolstunov L, Brickeen M, Kamanin V,
Susarla SM and Selvi F: Is the angulation of mandibular third
molars associated with the thickness of lingual bone? Br J Oral
Maxillofac Surg. 54:914–919. 2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Lang MS, Morrow AJ, Gonzalez ML and Dodson
TB: Do postoperative antibiotics decrease the frequency of
inflammatory complications following third molar removal? J Oral
Maxillofac Surg. 74:e33–e34. 2016.
|
|
11
|
Singh V, Alex K, Pradhan R, Mohammad S and
Singh N: Techniques in the removal of impacted mandibular third
molar: A comparative study. Eur J Gen Dent. 2:25–30. 2013.
|
|
12
|
Yang TJ, Li Y and Zhu HY: Removal of
lingual bone plate in the extraction of lower wisdom teeth. J Oral
Maxillofac Surg. 24(63)2014.
|