Introduction
Traditional herbal medicine has provided clinical
benefits to patients with coronavirus 2019 (COVID-19) in China
(1-3).
Several herbal formulas are encouraged for use in the treatment of
COVID-19 in the latest version of the diagnosis and treatment
protocol for novel coronavirus pneumonia (Trial Version 7) released
by the National Health Commission of China (4). One of these is Jinhua Qinggan granule
(JHQGG), which was formulated specifically for the treatment of
H1N1 influenza in the 2009-2010 pandemic (5-7).
JHQGG contains 12 herbal components, namely Jinyin hua
(Lonicerae Japonicae Flos, honeysuckle), Shigao (Gypsum
fibrosum moles, Gypsum fibrosum), Ma huang (Ephedra herba,
Ephedra), Kuxing ren (Amygdalus Communis Vas, Armeniacae Semen
Amarum), Huangqin (Scutellariae Radix, Scutellaria
baicalensis), Lianqiao (Forsythiae Fructus, Fructus
forsythiae), Zhebeimu (Fritillariae thunbergii Bulbus,
Thunberg Fritillary Bulb), Zhimu (Anemarrhenae Rhizoma, Rhizoma
Anemarrhenae), Niubangzi (Fructus Arctii, Arctii Fructus), Qinghao
(Artemisia annua L., Artemisiae annua herba), Bohe
(Menthae Herba, Menthae haplocalycis Herba) and
Gancao (Licorice, Liquorice), that exert medicinal effects on
symptoms of respiratory viral infection. Previous preclinical
studies have demonstrated that JHQGG reduces pulmonary lesions and
mortality in mice infected with the H1N1 influenza virus (5). Clinical studies have also
demonstrated that JHQGG reduces the duration of fever and
alleviates respiratory symptoms in patients with H1N1 influenza
(5,6).
On the basis of its therapeutic efficacy for
influenza, JHQGG has been recommended for use in patients
clinically suspected of COVID-19 infection to prevent disease onset
(8-11).
In randomized controlled trials on patients with COVID-19, the
combined administration of JHQGG with Western medicine was shown to
significantly promote viral clearance, ameliorate respiratory
symptoms, shorten the recovery time from pneumonia and relieve
psychological anxiety compared with the administration of Western
medicine alone (8-11).
Recent network pharmacological analyses have identified a large
number of active natural compounds contained in the herbal
ingredients of JHQGG, including rutin, luteolin, wogonin,
myricetin, quercetin, ursolic acid, chrysoeriol and glabridin
(12,13). These compounds interact with a wide
variety of target proteins and modulate the complex webs of
signaling and metabolic pathways associated with immune regulation,
anti-inflammation, and protection from oxidative stress and tissue
injury (12,13). Several active compounds also have
the potential to directly inhibit severe acute respiratory syndrome
coronavirus 2 (SARS-CoV-2) infection by downregulating angiotensin
I converting enzyme 2, the viral entry receptor (13).
Although network pharmacological studies have
provided in silico predictions on the possible
compound-target and target-function networks modulated by JHQGG
(12,13), there is limited information
available on the in vivo immunological mechanisms underlying
the prophylactic and therapeutic benefits of JHQGG against
COVID-19. To obtain insight into this issue, the present study
examined the acute effects of JHQGG on hematological and
immunological parameters.
Subjects and methods
Subjects and inclusion/exclusion
criteria
Since JHQGG has been recommended for use in
individuals clinically suspected of COVID-19 infection under
medical observation to prevent disease onset, the present study
employed uninfected individuals as subjects in a single-arm trial.
Participants were recruited through the University Hospital Medical
Information Network-Clinical Trials Registry (UMIN-CTR) website,
the authors' clinical website (https://takanawa-clinic.com/), announcements in an
e-mail newsletter and personal contacts. Individuals who met all
the following inclusion criteria were enrolled in the trial: Adults
between the ages of 20 and 70, and having negative RT-PCR and
IgM/IgG antibody tests for SARS-CoV-2 at study entry. Individuals
were excluded from the trial if they met any of the following
exclusion criteria: Were pregnant or breastfeeding; had duplicate
enrollment in other clinical trials; a history of infectious
diseases within the prior 6 months; a current or past history of
chronic inflammatory or immune-related diseases, or malignancies; a
history of drug use within the past 6 months; had any underlying
conditions associated with a higher risk of COVID-19 infection,
including hypertension, cardiovascular disease, cerebrovascular
disease, diabetes, obesity (body mass index ≥30), chronic
obstructive pulmonary disease and chronic kidney disease.
Administration of JHQGG
JHQGG was kindly provided by Dr Hugh Wang,
Juxiechang (Beijing) Pharmaceutical Co., Ltd. The subjects were
instructed to take a packet (5 g) orally 40 min their lunchtime
meal in accordance with the administration protocol of the Chinese
official guideline (4). This dose
is known to be effective for the treatment of influenza (6).
Hematological, biochemical and
cytokine analyses
To examine the acute hematological and immunological
effects of JHQGG, peripheral blood samples were obtained from each
subject immediately prior to and at 1 h following the
administration of JHQGG. Hematological and blood biochemical tests
were outsourced to SRL, Inc. Plasma cytokine levels were quantified
using the V-PLEX Proinflammatory Panel 1 Human kit (K15049D-1; Meso
Scale Diagnostics) and the Human IL-18 ELISA kit (ab215539; Abcam).
The primary outcome measure was changes in the plasma levels of
inflammatory-related cytokines [interleukin (IL)-6, IL-1β, IL-18,
IL-12, IL-2, IL-8, IL-10, interferon (IFN)-γ and tumor necrosis
factor (TNF)-α] at 1 h after the JHQGG ingestion compared with the
baseline levels. The secondary outcome measure was changes in
hematological parameters (as listed in Table I) at 1 h after the JHQGG ingestion
compared with baseline levels.
 | Table IAlterations in hematological
parameters and cytokine levels in subjects administered JHQGG. |
Table I
Alterations in hematological
parameters and cytokine levels in subjects administered JHQGG.
| | Pre-JHQGG
administration | Post-JHQGG
administration | |
|---|
| Measurements | Median | (IQR) | Median | (IQR) | Z value | P-value | r value |
|---|
| Complete blood
count | | | | | | | |
|
Red blood
cell count (x104/µl) | 454 | (419-468) | 457 | (416-469) | 1.26 | 0.206 | 0.298 |
|
Hemoglobin
(g/dl) | 13.5 | (12.3-14.4) | 13.6 | (12.2-14.0) | 1.60 | 0.111 | 0.376 |
|
Hematocrit
(%) | 41.0 | (36.5-43.7) | 40.6 | (36.2-42.8) | 2.06 |
0.0394a | 0.486 |
|
MCV
(fl) | 90.7 | (88.2-94.7) | 90.3 | (87.8-95.4) | 2.30 |
0.0216a | 0.542 |
|
MCH
(pg) | 30.1 | (29.4-31.5) | 30.3 | (29.5-31.7) | 0.166 | 0.868 | 0.0392 |
|
MCHC
(%) | 33.2 | (32.6-33.7) | 33.4 | (32.9-33.7) | 1.58 | 0.115 | 0.372 |
|
White blood
cell count (/µl) | 6200 | (5730-6680) | 6450 | (6030-6780) | 1.11 | 0.265 | 0.263 |
|
Platelet
count (x104/µl) | 24.4 | (22.1-28.7) | 24.7 | (22.7-28.3) | 0.214 | 0.831 | 0.0504 |
| White blood cell
differential | | | | | | | |
|
Neutrophils
(%) | 62.3 | (59.6-68.5) | 61.7 | (58.9-65.6) | 2.77 |
0.00561b | 0.653 |
|
Eosinophils
(%) | 1.10 | (0.850-2.08) | 1.05 | (0.725-2.38) | 0.0713 | 0.943 | 0.0168 |
|
Basophils
(%) | 0.450 | (0.300-0.575) | 0.500 | (0.325-0.600) | 0.431 | 0.666 | 0.102 |
|
Monocytes
(%) | 5.25 | (4.40-6.38) | 5.65 | (4.73-6.48) | 1.06 | 0.288 | 0.250 |
|
Lymphocytes
(%) | 29.1 | (23.6-32.9) | 29.9 | (25.3-33.0) | 2.82 |
0.00485b | 0.664 |
|
Neutrophil/lymphocyte
ratio | 2.24 | (1.82-2.97) | 2.08 | (1.79-2.52) | 2.72 |
0.00649b | 0.642 |
| Blood
biochemistry | | | | | | | |
|
AST
(U/l) | 16.5 | (15.0-19.5) | 16.0 | (14.3-18.8) | 0.00 | 1.00 | 0.00 |
|
ALT
(U/l) | 15.0 | (10.3-18.5) | 15.0 | (10.3-18.5) | 0.632 | 0.527 | 0.149 |
|
γ-GT
(U/l) | 14.0 | (12.3-21.0) | 14.0 | (13.0-21.0) | 1.51 | 0.132 | 0.355 |
|
LDH
(U/l) | 143 | (134-170) | 145 | (131-166) | 1.07 | 0.285 | 0.252 |
|
Albumin
(g/dl) | 4.70 | (4.50-4.88) | 4.65 | (4.53-4.90) | 0.206 | 0.837 | 0.0486 |
|
Urea
nitrogen (mg/dl) | 12.2 | (11.8-14.2) | 12.4 | (11.4-14.4) | 0.0237 | 0.981 | 0.00559 |
|
HDL
cholesterol (mg/dl) | 69.0 | (61.8-77.8) | 68.5 | (61.3-77.0) | 1.02 | 0.306 | 0.241 |
|
LDL
cholesterol (mg/dl) | 109 | (96.5-124) | 109 | (91.8-123) | 1.30 | 0.193 | 0.307 |
|
Triglycerides
(mg/dl) | 62.0 | (41.3-108) | 66.0 | (42.0-111) | 0.687 | 0.492 | 0.162 |
|
CRP
(mg/dl) | 0.0500 |
(0.0225-0.0875) | 0.0550 |
(0.0225-0.0875) | 1.61 | 0.107 | 0.380 |
| Cytokines | | | | | | | |
|
IFN-γ
(pg/ml) | 3.33 | (1.80-4.72) | 3.85 | (2.99-5.00) | 2.20 |
0.0268a | 0.518 |
|
IL-6
(pg/ml) | 1.40 | (0.731-3.31) | 0.988 | (0.690-1.59) | 2.96 |
0.00309b | 0.697 |
|
TNF-α
(pg/ml) | 2.49 | (2.01-3.55) | 2.63 | (2.29-3.39) | 0.893 | 0.393 | 0.210 |
|
IL-1β
(pg/ml) | 0.504 | (0.336-1.45) | 0.377 | (0.224-2.36) | 0.806 | 0.442 | 0.190 |
|
IL-18
(pg/ml) | 145 | (99.6-232) | 109 | (90.1-304) | 1.98 |
0.0483a | 0.467 |
|
IL-12
(pg/ml) | 0.262 | (0.106-0.452) | 0.330 | (0.185-0.472) | 1.02 | 0.325 | 0.241 |
|
IL-2
(pg/ml) | 0.280 | (0.0955-0.655) | 0.389 | (0.157-0.891) | 1.94 | 0.0539 | 0.457 |
|
IL-8
(pg/ml) | 448 | (105-1220) | 415 | (115-766) | 0.719 | 0.495 | 0.169 |
|
IL-10
(pg/ml) | 0.259 | (0.184-0.500) | 0.268 | (0.213-0.556) | 0.327 | 0.766 | 0.0770 |
Statistical analysis
No outliers were taken into account, and all
collected data from all patients (n=18) were subjected to
statistical analysis. The normality of the data was tested using
the Shapiro-Wilk test. On the basis of the results from the
normality test, the two-tailed Wilcoxon signed-rank test was
employed at the significance level (α) of 0.05 for subsequent
statistical analysis of the data. All statistical analyses were
performed using EZR version 1.53 (Saitama Medical Center, Jichi
Medical University, Saitama, Japan), which is a graphical user
interface for R (The R Foundation for Statistical Computing,
Vienna, Austria) (14). Post hoc
power analysis was performed using G*Power version 3.1.9.2(15). A P-value <0.05 was considered to
indicate a statistically significant difference.
Results
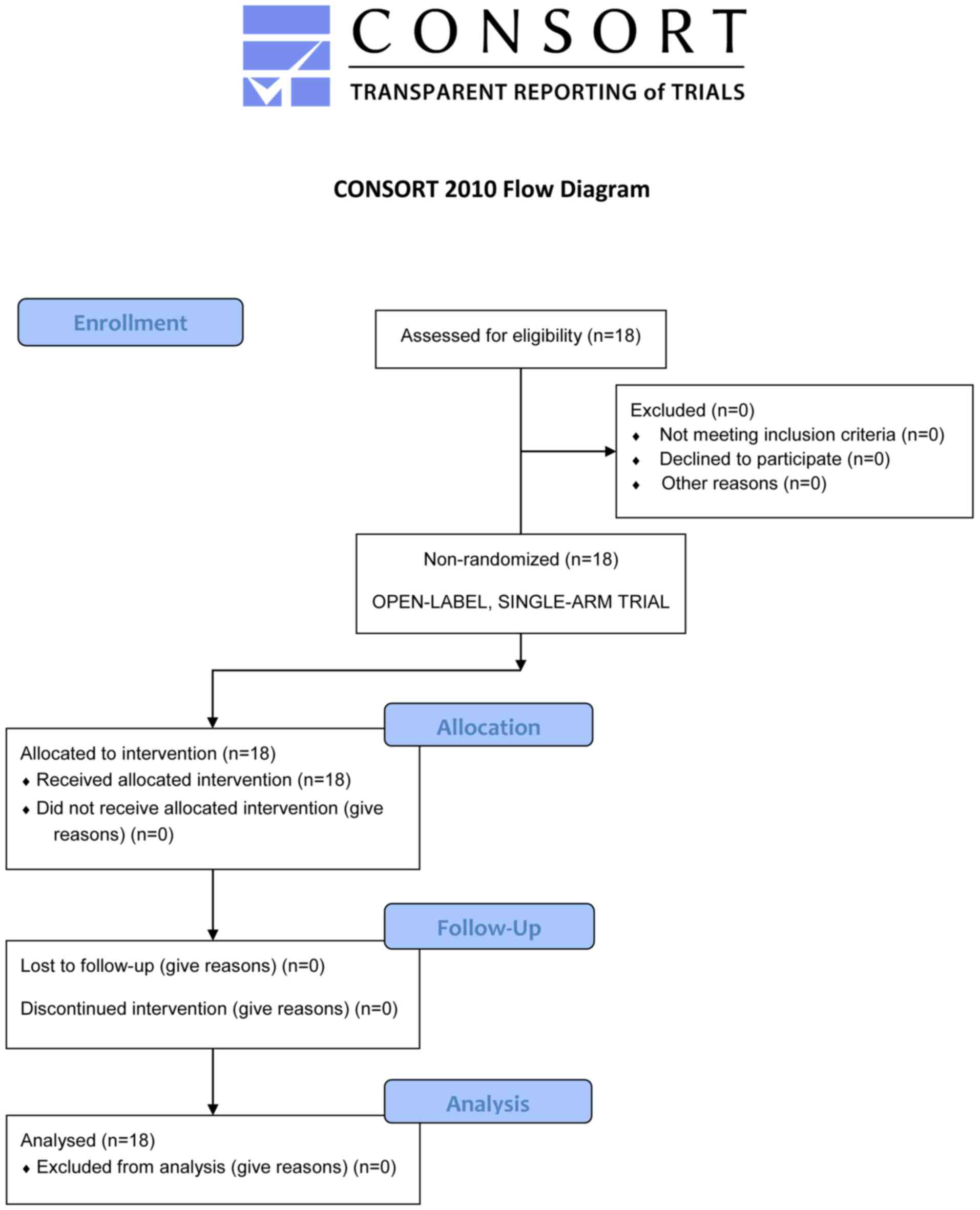
A total of 18 healthy volunteers were screened for
eligibility, found to be eligible and enrolled in the trial in the
present study (Fig. 1). These
subjects were the same as those that used in a previous study by
the authors on Qingfei Paidu decoction (QFPD) (16). JHQGG was administered to all the
enrolled participants from May 28-29, 2020 following a 2-week
washout period from the completion of the QFPD trial. Consequently,
18 subjects (5 males and 13 females; age range, 22-58 years; mean ±
SD, 33.8±10.7 years) completed the intervention, and the data were
subjected to statistical analysis (Fig. 1).
It was found that hematocrit levels (Z=2.06,
P=0.0394, r=0.486) and mean corpuscular volume (Z=2.30, P=0.0216,
r=0.542) were slightly altered within the reference ranges,
although there were no significant differences in the other
measurements of complete blood count and blood biochemistry between
pre- and post-JHQGG ingestion (Table
I). Notably, JHQGG intake induced a rapid decrease in the
proportion of neutrophils (Z=2.77, P=0.00561, r=0.653) and a
concomitant increase in the proportion of lymphocytes (Z=2.82,
P=0.00485, r=0.664), resulting in a significant decrease in the
neutrophil/lymphocyte ratio (NLR; Z=2.72, P=0.00649, r=0.642
(Table I). A decreased NLR was
observed in 13 (72.2%) out of the 18 subjects (Fig. 2).
In the blood cytokine analysis, the plasma levels of
IL-6 and IFN-γ were significantly decreased and increased,
respectively, compared with those in the pre-JHQGG ingestion (IL-6:
Z=2.96, P=0.00309, r=0.697; IFN-γ: Z=2.20, P=0.0268, r=0.518)
(Table I). The plasma IL-6 levels
were decreased in 14 (77.8%) subjects, and the plasma IFN-γ levels
were increased in 13 (72.2%) subjects (Fig. 2). A marginally significant decrease
was also found in the plasma IL-18 levels (Z=1.98, P=0.0483,
r=0.467) (Table I).
Post hoc two-tailed power analysis was performed
(significance level, α=0.05; sample size, n=18) and statistical
powers were obtained (1 - β) of 0.720 (neutrophils), 0.735
(lymphocytes), 0.706 (NLR), 0.775 (IL-6), 0.524 (IFN-γ) and 0.445
(IL-18) following the completion of the trial.
Discussion
Patients with severe COVID-19 infection present with
neutrophilia, lymphocytopenia and a resulting elevated NLR, which
are closely associated with poor clinical outcomes (17,18).
Extensive neutrophil infiltration into pulmonary capillaries and
the alveolar space has been observed in autopsy specimens from
patients with COVID-19(19).
Neutrophils stimulate alveolar macrophages to release
pro-inflammatory cytokines, such as IL-1β during respiratory viral
infection (20). Neutrophilia can
also cause the formation of excessive neutrophil extracellular
traps (NETs), which induce deregulated cytokine release,
respiratory failure, microthrombosis and oxidative stress-induced
tissue damage (19,21,22).
In the present study, JHQGG decreased the proportion of neutrophils
and increased that of lymphocytes within 1 h following ingestion,
yielding a significantly lower NLR. The rapid effects on the
proportions of neutrophils and lymphocytes may be suitable for
rebalancing immune cell dysregulation in patients with
COVID-19.
JHQGG contains various active pharmaceutical
ingredients, mainly rutin, luteolin, wogonin, myricetin, quercetin,
ursolic acid, chrysoeriol and glabridin (12,13).
There are only a limited number of studies available assessing the
pharmacokinetic properties of these representative active
ingredients in humans. The oral bioavailability values of the
active compounds are known to range from 3.20-46.43% (rutin, 3.20%;
myricetin, 13.75%; ursolic acid, 16.77%; chrysoeriol, 28.41%;
wogonin, 30.68%; luteolin, 36.16%; glabridin, 46.42%; and
quercetin, 46.43%) (12,13). By contrast, the time to peak blood
concentration (Tmax) of each active ingredient remains poorly
understood, apart from quercetin. As previously discussed (23), Erlund et al (24) demonstrated that the Tmax of oral
quercetin aglycone in healthy humans ranged from 1.9±1.2 to 4.9±2.1
h in a dose-dependent manner, and Graefe et al (25) demonstrated that the Tmax of oral
quercetin glycosides in humans was 0.7±0.2 to 0.3 h. Lee and
Mitchell (26) reported that the
Tmax of dietary quercetin from onion powder and apple peel powder
was 2.0±1.7 and 2.9±2.0 h in humans, respectively. To the best of
our knowledge, there are no studies available to date on the
pharmacokinetics of luteolin in humans; however, oral luteolin in
rats is known to be absorbed efficiently with a Tmax of 1.1 h
(27,28). Yasuda et al (29) also demonstrated that blood luteolin
levels rapidly increased at 0.5 h following the oral ingestion with
a Tmax of 1.0 h, as also previously discussed (27). As regards these data on oral
bioavailability and Tmax, the current setting of blood sampling (1
h following JHQGG ingestion) was considered to be appropriate for
the pilot study of the acute immunological effects of JHQGG.
There is a large body of evidence to indicate that
patients with COVID-19 have aberrantly increased blood levels of
pro-inflammatory cytokines and chemokines (30). In particular, IL-6 is known to be a
critical driver of complex immune dysregulation that causes the
excessive production of pro-inflammatory cytokines termed as the
'cytokine storm' and systemic hyperinflammation (31). The blood IL-6 level is positively
associated with the severity and mortality of patients with
COVID-19(32). IL-6 receptor
blockade using tocilizumab has been shown to reduce mortality and
the risk of mechanical ventilation in patients with severe COVID-19
infection (33). The network
pharmacological study by Niu et al predicted that several
natural compounds such as rutin, luteolin, quercetin and ursolic
acid, all of which are active ingredients of JHQGG, potentially
interact with IL-6 directly to downregulate its pro-inflammation
function (12). Considering the
critical role of IL-6 as an exacerbating factor for COVID-19, the
immunological activity of JHQGG to rapidly downregulate the blood
level of IL-6 indicates that it may be suitable for preventing
severe cases of infection and/or improving the severity of COVID-19
infection.
INF-γ is produced predominantly by type 1 helper T
(Th1) and natural killer (NK) cells and stimulates innate immunity
and inflammation, particularly through the activation of
macrophages and dendritic cells. In the present study, JHQGG
ingestion induced a slight, yet significant increase in the blood
level of INF-γ. This pro-inflammatory activity appears to be
contradictory to its clinical benefits against COVID-19. Notably,
IFN-γ is known to serve as a central mediator of a broad spectrum
of antiviral immunity by interfering with viral replication
directly, potentiating the effects of IFN-α/β, activating
Th1-dependent immune responses, and promoting the activation of the
MHC class I pathway (34,35). However, compared with type I IFNs,
the roles of IFN-γ in COVID-19 pathogenesis are more complex and
have been less clearly defined. Notably, several studies have
reported the impaired IFN-γ responses in patients with severe
COVID-19 infection (36-38).
Kim et al (36) reported
that the plasma levels of IFN-γ were significantly decreased in
patients in the intensive care unit (ICU), compared with
outpatients and patients with mild disease. In line with the
decrease in the levels of IFN-γ, the levels of IFN-γ-stimulated
genes, including HLA-A, HLA-B, HLA-DPA1,
HLA-DRA, β2M and CIITA, were downregulated,
particularly in patients in the ICU, as compared with outpatients
and convalescent patients (36).
Ruetsch et al (37)
demonstrated that the reduced production levels of IFN-γ by in
vitro-stimulated immune cells from patients with COVID-19 were
significantly associated with the increased disease severity and
the stimulated IFN-γ levels <15 IU/ml upon hospital admission
were significantly associated with a greater number of
complications during hospitalization. The multivariate-adjusted
logistic regression analysis by Hu et al (38) revealed that the circulating IFN-γ
levels were inversely associated with the risk of developing lung
fibrosis, inflammation-induced lung injury, in hospitalized
patients. Thus, the functional exhaustion of IFN-γ production and
the impairment of the downstream inflammatory responses are
pathologically associated with a severe disease course of COVID-19.
It was thus hypothesized that physiological, well-controlled, mild
pro-inflammatory conditions, such as the JHQGG-induced minimal
increase in INF-γ levels, may play protective roles against viral
infection and replication, although pathological, dysregulated
hyperinflammation leads to severe symptoms, such as the cytokine
storm and acute respiratory distress syndrome.
Patients with severe COVID-19 infection have
significantly lower numbers of CD4+ T-, CD8+
T- and NK cells, with a decreased capacity to produce IFN-γ, which
results in a decrease in IFN-γ production by CD4+
T-cells (39-41).
Similarly, in a previous study using IFN-γ-deficient mice, Kyuwa
and Sugiura (42) demonstrated
that IFN-γ and CD8+ T-cells were essential for the
clearance of murine coronavirus, a virus within the same genus
(betacoronavirus) as SARS-CoV-2. Previous studies have reported the
decreased plasma IFN-γ levels in patients with severe COVID-19
infection (36-38).
Furthermore, the reduced cytotoxic potential of CD4+ T-,
CD8+ T- and NK cells is IL-6-dependent, and cases with
severe COVID-19 infection have a higher IL-6/IFN-γ ratio than cases
with moderate infection (40,43).
The transfusion of COVID-19 convalescent plasma to patients with
severe infection has been shown to significantly decrease the
IL-6/IFN-γ ratio (44). Thus, the
ability of JHQGG to decrease IL-6 and increase IFN-γ levels may be
a suitable property for correcting the aberrantly elevated
IL-6/IFN-γ ratio.
The main limitations of the present study are the
small number of participants and the selection of uninfected
individuals as the study subjects. Since JHQGG has been recommended
for use in individuals clinically suspected of COVID-19 infection
under medical observation or asymptomatic patients to prevent
disease onset, uninfected individuals were employed as the study
subjects. The present study demonstrated that JHQGG significantly
up- and downregulated the plasma levels of IFN-γ and IL-6,
respectively. Further studies with larger cohorts of patients with
moderate to severe infection are thus essential to confirm the
conclusion in patients and determine generalizability. Randomized
controlled trials in patients with moderate to severe infection are
also essential to confirm whether cytokine responses to JHQGG are
sustained and whether they are associated with significant clinical
improvement. Further validation studies are also required to
determine whether the blood levels of JHQGG-derived compounds
increase at 1 h following oral administration. The present study
tried to measure the blood levels of representative active
ingredients of JHQGG before and after oral administration; however,
since some difficulties were encountered in finding optimal Liquid
chromatography-mass spectrometry conditions, such data could not be
obtained. In addition, since JHQGG contains 12 herbal components,
the quality control or batch-to-batch quality consistency poses a
great challenge in clinical practice.
In conclusion, the findings of the present study
suggest that the clinical benefits of JHQGG against COVID-19 are,
at least in part, associated with its rapid immunomodulatory
effects; JHQGG can rapidly decrease the blood levels of neutrophils
and IL-6, two critical exacerbating factors of COVID-19, and
increase the blood levels of lymphocytes and IFN-γ that are
essential for coordinated antiviral immune responses. JHQGG has
been recommended for use in suspected and asymptomatic cases of
COVID-19 to suppress disease onset, as per the Chinese official
clinical guideline (4).
Considering the rapid immunomodulatory effects on neutrophils,
lymphocytes, IFN-γ and IL-6, JHQGG may also be effective for
preventing disease progression in patients with moderate to severe
infection as an option of adjunctive pharmacotherapy against
COVID-19.
Acknowledgements
The authors would like to thank Dr Hugh Wang
[Juxiechang (Beijing) Pharmaceutical Co., Ltd.] for generously
providing Jinhua Qinggan granule and for his helpful advice for
clinical trial planning.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YK and TE were involved in the conceptualization and
methodology of the study, as well as in performing the experiments
and data collection, obtaining resources, data curation, reviewing
and editing of the manuscript, and project administration. KA, KK
and MM were involved in performing the experiments and data
collection, obtaining resources, and in the reviewing and editing
of the manuscript. TA was involved in the conceptualization of the
study, and in the reviewing and editing of the manuscript. TN was
involved in the conceptualization and methodology of the study, as
well as in formal analysis, and in the writing of the original
draft, as well as in the preparation and creation of the published
figures and tables. YK, TA and TN were also involved in study
supervision. YK and TN confirm the authenticity of all the raw
data. All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was carried out in accordance with
The Code of Ethics of the World Medical Association (Declaration of
Helsinki). All procedures were reviewed and approved by the Ethics
Committees of Takanawa Clinic (approval no. 2020-2). A signed
informed consent form was obtained from each participant prior to
inclusion in this study.
Patient consent for publication
Not applicable.
Competing interests
YK, KA, KK, MM and TE are employees of Takanawa
Clinic. TA and TN serve as research advisers to Takanawa Clinic and
receive advisory fees. The authors declare that there is no
conflict of interest between the study group and Juxiechang
(Beijing) Pharmaceutical Co., Ltd., the Chinese pharmaceutical
company that provided Jinhua Qinggan granule for the study.
References
|
1
|
Yang Y, Islam MS, Wang J, Li Y and Chen X:
Traditional Chinese medicine in the treatment of patients infected
with 2019-new coronavirus (SARS-CoV-2): A review and perspective.
Int J Biol Sci. 16:1708–1717. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Luo H, Gao Y, Zou J, Zhang S, Chen H, Liu
Q, Tan D, Han Y, Zhao Y and Wang S: Reflections on treatment of
COVID-19 with traditional Chinese medicine. Chin Med.
15(94)2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Zhao Z, Li Y, Zhou L, Zhou X, Xie B, Zhang
W and Sun J: Prevention and treatment of COVID-19 using Traditional
Chinese Medicine: A review. Phytomedicine.
85(153308)2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Wei PF: Diagnosis and treatment protocol
for novel coronavirus pneumonia (Trial Version 7). Chin Med J
(Engl). 133:1087–1095. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Tao Z, Yang Y, Shi W, Xue M, Yang W, Song
Z, Yao C, Yin J, Shi D, Zhang Y, et al: Complementary and
alternative medicine is expected to make greater contribution in
controlling the prevalence of influenza. Biosci Trends. 7:253–256.
2013.PubMed/NCBI
|
|
6
|
Li GQ, Zhao J, Tu ZT, Li JB, Liu QQ, Shi
LQ, Miao Q, Yuan HQ, Liu XQ, Long YY, et al: Treating influenza
patients of wind-heat affecting Fei syndrome by jinhua qinggan
granule: A double-blinded randomized control trial. Zhongguo Zhong
Xi Yi Jie He Za Zhi. 33:1631–1635. 2013.PubMed/NCBI(In Chinese).
|
|
7
|
Wu L, Chen Y, Ma Y, Yang Z, Yang N, Deng
W, Chen Y, Sun Y, Li Y and Lin L: Clinical practice guideline on
treating influenza in adult patients with Chinese patent medicines.
Pharmacol Res. 160(105101)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ang L, Song E, Lee HW and Lee MS: Herbal
medicine for the treatment of coronavirus disease 2019 (COVID-19):
A systematic review and meta-analysis of randomized controlled
trials. J Clin Med. 9(1583)2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Liu Z, Li X, Gou C, Li L, Luo X, Zhang C,
Zhang Y, Zhang J, Jin A, Li H, et al: Effect of Jinhua Qinggan
granules on novel coronavirus pneumonia in patients. J Tradit Chin
Med. 40:467–472. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wang J and Qi F: Traditional Chinese
medicine to treat COVID-19: The importance of evidence-based
research. Drug Discov Ther. 14:149–150. 2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Liu M, Gao Y, Yuan Y, Yang K, Shi S, Zhang
J and Tian J: Efficacy and safety of integrated traditional Chinese
and Western medicine for corona virus disease 2019 (COVID-19): A
systematic review and meta-analysis. Pharmacol Res.
158(104896)2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Niu WH, Wu F, Cao WY, Wu ZG, Chao YC and
Liang C: Network pharmacology for the identification of
phytochemicals in traditional Chinese medicine for COVID-19 that
may regulate interleukin-6. Biosci Rep: Jan 29, 2021 (Epub ahead of
print). doi: 10.1042/BSR20202583.
|
|
13
|
Niu W, Wu F, Cui H, Cao W, Chao Y, Wu Z,
Fan M and Liang C: Network pharmacology analysis to identify
phytochemicals in traditional Chinese medicines that may regulate
ACE2 for the treatment of COVID-19. Evid Based Complement Alternat
Med. 2020(7493281)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kanda Y: Investigation of the freely
available easy-to-use software ‘EZR’ for medical statistics. Bone
Marrow Transplant. 48:452–458. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Faul F, Erdfelder E, Lang AG and Buchner
A: G*Power 3: A flexible statistical power analysis program for the
social, behavioral, and biomedical sciences. Behav Res Methods.
39:175–191. 2007.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kageyama Y, Aida K, Kawauchi K, Morimoto
M, Ebisui T, Akiyama T and Nakamura T: Qingfei Paidu decoction, a
Chinese herbal medicine against COVID 19, elevates the blood levels
of pro inflammatory cytokines: An open label, single arm pilot
study. World Acad Sci J. 3(25)2021.
|
|
17
|
Liu J, Li S, Liu J, Liang B, Wang X, Wang
H, Li W, Tong Q, Yi J, Zhao L, et al: Longitudinal characteristics
of lymphocyte responses and cytokine profiles in the peripheral
blood of SARS-CoV-2 infected patients. EBioMedicine.
55(102763)2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Li X, Liu C, Mao Z, Xiao M, Wang L, Qi S
and Zhou F: Predictive values of neutrophil-to-lymphocyte ratio on
disease severity and mortality in COVID-19 patients: A systematic
review and meta-analysis. Crit Care. 24(647)2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Barnes BJ, Adrover JM, Baxter-Stoltzfus A,
Borczuk A, Cools-Lartigue J, Crawford JM, Dassler-Plenker J, Guerci
P, Huynh C, Knight JS, et al: Targeting potential drivers of
COVID-19: Neutrophil extracellular traps. J Exp Med.
217(e20200652)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Peiró T, Patel DF, Akthar S, Gregory LG,
Pyle CJ, Harker JA, Birrell MA, Lloyd CM and Snelgrove RJ:
Neutrophils drive alveolar macrophage IL-1β release during
respiratory viral infection. Thorax. 73:546–556. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zuo Y, Yalavarthi S, Shi H, Gockman K, Zuo
M, Madison JA, Blair C, Weber A, Barnes BJ, Egeblad M, et al:
Neutrophil extracellular traps in COVID-19. JCI Insight.
5(e138999)2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Laforge M, Elbim C, Frère C, Hémadi M,
Massaad C, Nuss P, Benoliel JJ and Becker C: Tissue damage from
neutrophil-induced oxidative stress in COVID-19. Nat Rev Immunol.
20:515–516. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Batiha GE, Beshbishy AM, Ikram M, Mulla
ZS, El-Hack ME, Taha AE, Algammal AM and Elewa YH: The
pharmacological activity, biochemical properties, and
pharmacokinetics of the major natural polyphenolic flavonoid:
Quercetin. Foods. 9(374)2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Erlund I, Kosonen T, Alfthan G, Mäenpää J,
Perttunen K, Kenraali J, Parantainen J and Aro A: Pharmacokinetics
of quercetin from quercetin aglycone and rutin in healthy
volunteers. Eur J Clin Pharmacol. 56:545–553. 2000.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Graefe EU, Wittig J, Mueller S, Riethling
AK, Uehleke B, Drewelow B, Pforte H, Jacobasch G, Derendorf H and
Veit M: Pharmacokinetics and bioavailability of quercetin
glycosides in humans. J Clin Pharmacol. 41:492–499. 2001.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Lee J and Mitchell AE: Pharmacokinetics of
quercetin absorption from apples and onions in healthy humans. J
Agric Food Chem. 60:3874–3881. 2012.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Wang Z, Zeng M, Wang Z, Qin F, Chen J and
He Z: Dietary luteolin: A narrative review focusing on its
pharmacokinetic properties and effects on glycolipid metabolism. J
Agric Food Chem. 69:1441–1454. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Chen T, Li LP, Lu XY, Jiang HD and Zeng S:
Absorption and excretion of luteolin and apigenin in rats after
oral administration of Chrysanthemum morifolium extract. J Agric
Food Chem. 55:273–277. 2007.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Yasuda MT, Fujita K, Hosoya T, Imai S and
Shimoi K: Absorption and metabolism of luteolin and its glycosides
from the extract of chrysanthemum morifolium flowers in rats and
Caco-2 cells. J Agric Food Chem. 63:7693–7699. 2015.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Cao X: COVID-19: Immunopathology and its
implications for therapy. Nat Rev Immunol. 20:269–270.
2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Giamarellos-Bourboulis EJ, Netea MG,
Rovina N, Akinosoglou K, Antoniadou A, Antonakos N, Damoraki G,
Gkavogianni T, Adami ME, Katsaounou P, et al: Complex immune
dysregulation in COVID-19 patients with severe respiratory failure.
Cell Host Microbe. 27:992–1000.e3. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Zhang X, Tan Y, Ling Y, Lu G, Liu F, Yi Z,
Jia X, Wu M, Shi B, Xu S, et al: Viral and host factors related to
the clinical outcome of COVID-19. Nature. 583:437–440.
2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Tleyjeh IM, Kashour Z, Damlaj M, Riaz M,
Tlayjeh H, Altannir M, Altannir Y, Al-Tannir M, Tleyjeh R, Hassett
L, et al: Efficacy and safety of tocilizumab in COVID-19 patients:
A living systematic review and meta-analysis. Clin Microbiol
Infect. 27:215–227. 2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Hoffmann HH, Schneider WM and Rice CM:
Interferons and viruses: An evolutionary arms race of molecular
interactions. Trends Immunol. 36:124–138. 2015.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Kang S, Brown HM and Hwang S: Direct
antiviral mechanisms of interferon-γ. Immune Netw.
18(e33)2018.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Kim MH, Salloum S, Wang JY, Wong LP, Regan
J, Lefteri K, Manickas-Hill Z, Gao C, Li JZ, Sadreyev RI, et al:
MGH COVID-19 Collection and Processing Team: Type I, II, and III
interferon signatures correspond to coronavirus disease 2019
severity. J Infect Dis. 224:777–782. 2021.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Ruetsch C, Brglez V, Crémoni M, Zorzi K,
Fernandez C, Boyer-Suavet S, Benzaken S, Demonchy E, Risso K,
Courjon J, et al: Functional exhaustion of type I and II
interferons production in severe COVID-19 patients. Front Med
(Lausanne). 7(603961)2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Hu ZJ, Xu J, Yin JM, Li L, Hou W, Zhang
LL, Zhou Z, Yu YZ, Li HJ, Feng YM, et al: Lower circulating
interferon-γ is a risk factor for lung fibrosis in COVID-19
patients. Front Immunol. 11(585647)2020.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Chen G, Wu D, Guo W, Cao Y, Huang D, Wang
H, Wang T, Zhang X, Chen H, Yu H, et al: Clinical and immunological
features of severe and moderate coronavirus disease 2019. J Clin
Invest. 130:2620–2629. 2020.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Mazzoni A, Salvati L, Maggi L, Capone M,
Vanni A, Spinicci M, Mencarini J, Caporale R, Peruzzi B, Antonelli
A, et al: Impaired immune cell cytotoxicity in severe COVID-19 is
IL-6 dependent. J Clin Invest. 130:4694–4703. 2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Zheng M, Gao Y, Wang G, Song G, Liu S, Sun
D, Xu Y and Tian Z: Functional exhaustion of antiviral lymphocytes
in COVID-19 patients. Cell Mol Immunol. 17:533–535. 2020.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Kyuwa S and Sugiura Y: Role of cytotoxic T
lymphocytes and interferon-γ in coronavirus infection: Lessons from
murine coronavirus infections in mice. J Vet Med Sci. 82:1410–1414.
2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Lagunas-Rangel FA and Chávez-Valencia V:
High IL-6/IFN-γ ratio could be associated with severe disease in
COVID-19 patients. J Med Virol. 92:1789–1790. 2020.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Acosta-Ampudia Y, Monsalve DM, Rojas M,
Rodríguez Y, Gallo JE, Salazar-Uribe JC, Santander MJ, Cala MP,
Zapata W, Zapata MI, et al: CP-COVID-19 group: COVID-19
convalescent plasma composition and immunological effects in severe
patients. J Autoimmun. 118(102598)2021.PubMed/NCBI View Article : Google Scholar
|