Introduction
Multiple myeloma (MM) is a B-cell neoplasm
characterized by the clonal proliferation of plasma cells that
develops due to the presence of genetic changes and the interaction
of plasma cells with the bone marrow microenvironment (1). The improvement in the overall
survival (OS) and progression-free survival (PFS) rates of patients
with MM due to the application of specific immunomodulators and
proteasome inhibitors has been based on risk stratification
(2,3). Chromosomal abnormalities, including
t(4;14), t(14;16), t(14;20), amp1q21 and del 17p have been shown to
be associated with a poor prognosis. the revised international
staging system (R-ISS) is based on a combination of cytogenetic
aberrations detected by fluorescence in situ hybridization
(FISH), ISS (international staging system, a combination of albumin
and β2-microglobulin) and lactate dehydrogenase (LDH). R-ISS is
accepted as the prognostic scoring system for patients with MM.
However, patients with MM have highly variable prognoses and a
meticulous evaluation of their prognosis is required for optimal
treatment strategies to be administered (2,3).
Afram et al (4) indicated that the performance status
may be useful in determining the prognosis of patients. Cai et
al (5) suggested that a high albumin-to-globulin ratio was
associated with an improved survival time (5). Qian et al (6) and Chen et al (7) indicated that a high percentage of
abnormal plasma cells in the bone marrow were highly associated
with a poor prognosis. Qian et al (6) also demonstrated that a high serum
calcium level was a poor prognostic factor for OS.
Several studies have examined the expression levels
of certain inflammatory factors and have suggested that these
factors (8-10)
exerted adverse effects on the survival rate of patients with MM.
These inflammatory factors include the platelet count (PLT), the
neutrophil-to-lymphocyte ratio (NLR), the platelet-to-lymphocyte
ratio (PLR), the monocyte-to-lymphocyte ratio (MLR) and C-reactive
protein (CRP) levels. Previous studies, such as those of Zhang
et al (8), Liu et al
(9), Kim et al (10), Szudy-Szczyrek et al
(11) and Zuo et al
(12) suggested that a high NLR
was an adverse prognostic factor. However, no consensus has yet
been reached on the cut-off value used for the diagnosis of MM.
Recently, Gui et al (13)
and Solmaz et al (14)
identified that a high PLR was a significant factor for a poor
survival time.
Several studies have investigated the combination of
several prognostic indicators to provide a system equivalent to the
ISS or R-ISS. Kim et al (10) identified that the multiple
prognostic index (MPI) value included NLR, PLT and CRP for patients
with MM. Liu et al (9)
identified application of IPSI (inflammatory prognostic score
index), which included the following parameters: NLR, platelet
count and red blood cell distribution width (RDW).
Since 2005, ISS (with albumin and β2-microglobulin)
has been applied for the prognosis of patients with symptomatic MM
from 17 institutions (15). It is
a simple and easy-to-use prognostic indicator; however, it was
developed prior to the use of the new regimen. In August 2015, the
International Myeloma Working Group (IMWG) published the R-ISS. It
is a system that was established by the development of additional
biomarkers in MM, including ISS, LDH and cytogenetic analysis.
R-ISS was developed based on clinical and laboratory data following
the evaluation of chromosomal abnormalities by FISH [high-risk
includes the following markers: t(4;14), t(14;16) and del 17 p,
standard-risk without these chromosomal abnormalities] from
patients with a new diagnosis of MM who were treated with new drugs
(immunomodulatory agents or proteasome inhibitors) (16). Therefore, it is suitable for the
prognosis of patients treated with new drugs. However, this
indicator requires technical expertise, has a high cost and
requires a long period of analysis. Therefore, it is necessary to
propose tools that are simple, cost- and time-effective and
suitable for a new regimen.
To facilitate the stratification of the risk of
patients with MM using the simple factors, the present study was
conducted to determine the influence of the combined prognostic
index (CPI), which included the serum calcium levels, the NLR and
the PLT, on the survival rates of patients with MM.
Patients and methods
Patients
From January, 2015 to April, 2019, 111 patients with
de novo MM, according to the criteria of IMWG 2014, were
enrolled in the present study at the Center of Hematology and Blood
Transfusion, Bach Mai Hospital, Hanoi, Vietnam (17). The study protocol was approved by
the Ethical Committee in Hanoi Medical University (no. 187).
Patient consent was waived by the committee as the present study
was a retrospective observational study.
Screening tests
Prior to treatment, all patients were evaluated by
the Eastern Cooperative Oncology Group performance status (PS)
(18). The percentage of bone
marrow plasma cells, the hemoglobin levels, the NLR, PLT, as well
as the serum albumin, β2-microglobulin and calcium levels were
assessed to evaluate the pre-chemotherapy patient status and the
prognostic risk.
Treatment
All patients were treated with chemotherapy
including the following regimens: The MPT protocol, which included
melphalan-prednisone-thalidomide for patients ≥65 years of age, the
VCD protocol, which included
bortezomib-cyclophosphamide-dexamethasone or the VTD protocol,
which included bortezomib-thalidomide-dexamethasone for patients
<65 years of age.
Definitions
The stage classification was defined according to
the ISS (16). The response to the
remission induction therapy was evaluated according to the IMWG
2016 response criteria (19).
Statistical analysis
The following prognostic factors were subjected to
univariate analysis: PS, the percentage of bone marrow plasma
cells, hemoglobin levels, ISS stage, platelet count, NLR and serum
calcium levels. The optimal cut-off value of PS (score 2) was
determined as described in study by Kim et al (10). The optimal cut-off value of a high
percentage of bone marrow plasma cells (30%) and a low hemoglobin
level (<100 g/l) were determined according to the study of Qian
et al (6). The optimal
cut-off value for low PLT (<150x109/l) was determined
according to the study of Kim et al (10). The present study carefully
considered and selected a PLT cut-off value of 150x109/l
instead of 100x109/l according to the study of Jung
et al (20). However, a
higher level of alert is required when assessing patient prognosis.
The receiver operating characteristic curve was performed
separately for the determination of the NLR and the serum calcium
levels to obtain a predictive value for OS. The cut-off value of
NLR was 2.245, whereas the cut-off value of the serum calcium
levels was 2.665 mmol/l. OS was calculated using the Kaplan-Meier
method. Univariate analysis of prognostic factors for OS was
performed using the log-rank test with the following variables: PS
(score 2), high percentage of bone marrow plasma cells (30%), low
hemoglobin levels (<100 g/l), high NLR (2.245), low PLT
(<150x109/l), high serum calcium levels (2.665
mmol/l), and stage ISS. P<0.05 was considered to indicate a
statistically significant difference. The variables that indicated
statistically significant differences in the univariate analysis
were included as prognostic factors in the multivariate analysis.
Multivariate analysis of prognostic factors for OS was performed
using the Cox proportional hazards method. Statistical analysis was
performed using SPSS 25 software. P<0.05 was considered to
indicate a statistically significant difference.
Results
Clinical data
At diagnosis, 111 patients were included in the
present study, of whom 55 were males (M:F ratio, 0.98). The
characteristics of the patients are presented in Tables I and II.
 | Table ICharacteristics of the patients
included in the present study. |
Table I
Characteristics of the patients
included in the present study.
| Characteristic | No. of patients
(n=111) | Percentage |
|---|
| Sex | | |
|
Male | 55 | 49.5 |
|
Female | 56 | 50.5 |
| ISS stage | | |
|
I | 10 | 9 |
|
II | 27 | 24.3 |
|
III | 74 | 66.3 |
| Age, years (mean,
60; min, 32; max, 84) | | |
|
<65
years | 80 | 72.1 |
|
≥65
years | 31 | 27.9 |
 | Table IILaboratory indices of the patients
included in the study. |
Table II
Laboratory indices of the patients
included in the study.
| Characteristic | Minimum | Maximum | Mean | Standard
deviation |
|---|
| Hemoglobin
(g/l) | 39.00 | 136.00 | 87.5721 | 21.93982 |
| WBC
(x109/l) | 1.47 | 59.93 | 7.8307 | 6.11695 |
| Platelet
(x109/l) | 37.00 | 626.00 | 213.8559 | 92.44338 |
| NLR | .54 | 19.53 | 2.6394 | 2.37388 |
| Urea (mmol/l) | 2.50 | 32.70 | 10.5464 | 6.78404 |
| Creatinine
(mmol/l) | 43.00 | 1,073.00 | 196.3036 | 196.81591 |
| AST (U/l) | 12.00 | 143.00 | 30.0800 | 18.95692 |
| ALT (U/l) | 6.00 | 228.00 | 28.1109 | 29.51206 |
| Albumin (g/l) | 17.30 | 51.00 | 32.3649 | 7.33865 |
| LDH (U/l) | 89.00 | 756.00 | 201.4048 | 114.21689 |
| B2M (µg/ml) | 1.70 | 91.80 | 11.7759 | 13.54150 |
| Ferritin
(ng/ml) | 46.40 | 7,180.00 | 892.9460 | 928.97367 |
| Calcium
(mmol/l) | 1.09 | 3.94 | 2.3539 | .44654 |
| Bone marrow count
(x109/l) | 5.56 | 258.58 | 58.0596 | 54.77775 |
| Plasma cells in
bone marrow (%) | 2.00 | 86.00 | 27.8018 | 19.52798 |
Prognostic factors of survival
Univariate analysis was performed to assess the OS.
The data indicated that a PS ≥2 (P=0.004), a high percentage of
bone marrow plasma cells (P=0.004), a high NLR (P=0.015), a low
platelet count (P=0.025), high serum calcium levels (P=0.001) and
the stage of ISS (P=0.002) were prognostic factors, which were
significantly associated with a poor prognosis (Table III). Multivariate analysis for OS
indicated that a high percentage of bone marrow plasma cells
(P=0.047), a high NLR (P=0.042), a low PLT (P=0.025) and high serum
calcium levels (P=0.015) were independent and significant
prognostic factors for the survival of the patients with MM
(Table III).
 | Table IIIPrognostic factors included in the
survival analysis. |
Table III
Prognostic factors included in the
survival analysis.
| | Univariate
analysis | Multivariate
analysis |
|---|
| Factor | OS (months) | P-value (log-rank
test) | HR | 95% CI | P-value (Cox
analysis) |
|---|
| Performance
status | | | | | |
|
0-1 | 45.948 | 0.004 | | | |
|
≥2 | 32.615 | | | | |
| Bone marrow plasma
cells (%) | | | | | |
|
<30 | 40.529 | 0.004 | 1 | | 0.047 |
|
≥30 | 31.815 | | 1.951 | 1.010-3.766 | |
| NLR | | | | | |
|
<2.245 | 41.344 | 0.015 | 1 | | 0.042 |
|
≥2.245 | 31.296 | | 2.001 | 1.025-3.905 | |
| Platelet count
(x109/l) | | | | | |
|
≥150 | 39.834 | 0.025 | 1 | | 0.025 |
|
<150 | 29.698 | | 2.105 | 1.096-4.046 | |
| Calcium levels
(mmol/l) | | | | | |
|
<2.665 | 40.492 | 0.001 | 1 | | 0.015 |
|
≥2.665 | 26.241 | | 2.173 | 1.166-4.050 | |
| ISS | | | | | |
|
ISS1 | 50.400 | 0.002 | | | |
|
ISS2 | 40.885 | | | | |
|
ISS3 | 33.524 | | | | |
Establishment of CPI
Multivariate analysis demonstrated that high serum
calcium levels (2.665 mmol/l), high NLR (2.245) and low platelet
count (<150x109/l) were independent and significant
adverse prognostic factors and were included in the CPI. The
criteria for scoring of the CPI were based on the presence of each
risk factor. The patients with high calcium levels (2.665 mmol/l),
a high NLR (2.245) and a low PLT (<150x109/l)
demonstrated a score of 1. Based on the scores obtained, the CPI
was formed, in which the patients were grouped into a low-risk
group (0-1 points), an intermediate-risk group (2 points) and a
high-risk group (3 points). Although the results of the
multivariate analysis indicated that the high percentage of the
bone marrow plasma cells was an independent and significant
prognostic factor for patient OS, this parameter was not included
in the plasma cell index of the CPI, since the objective of the
present study was to provide a simple and easy-to-use index that
could be applied in the peripheral blood samples of the
patients.
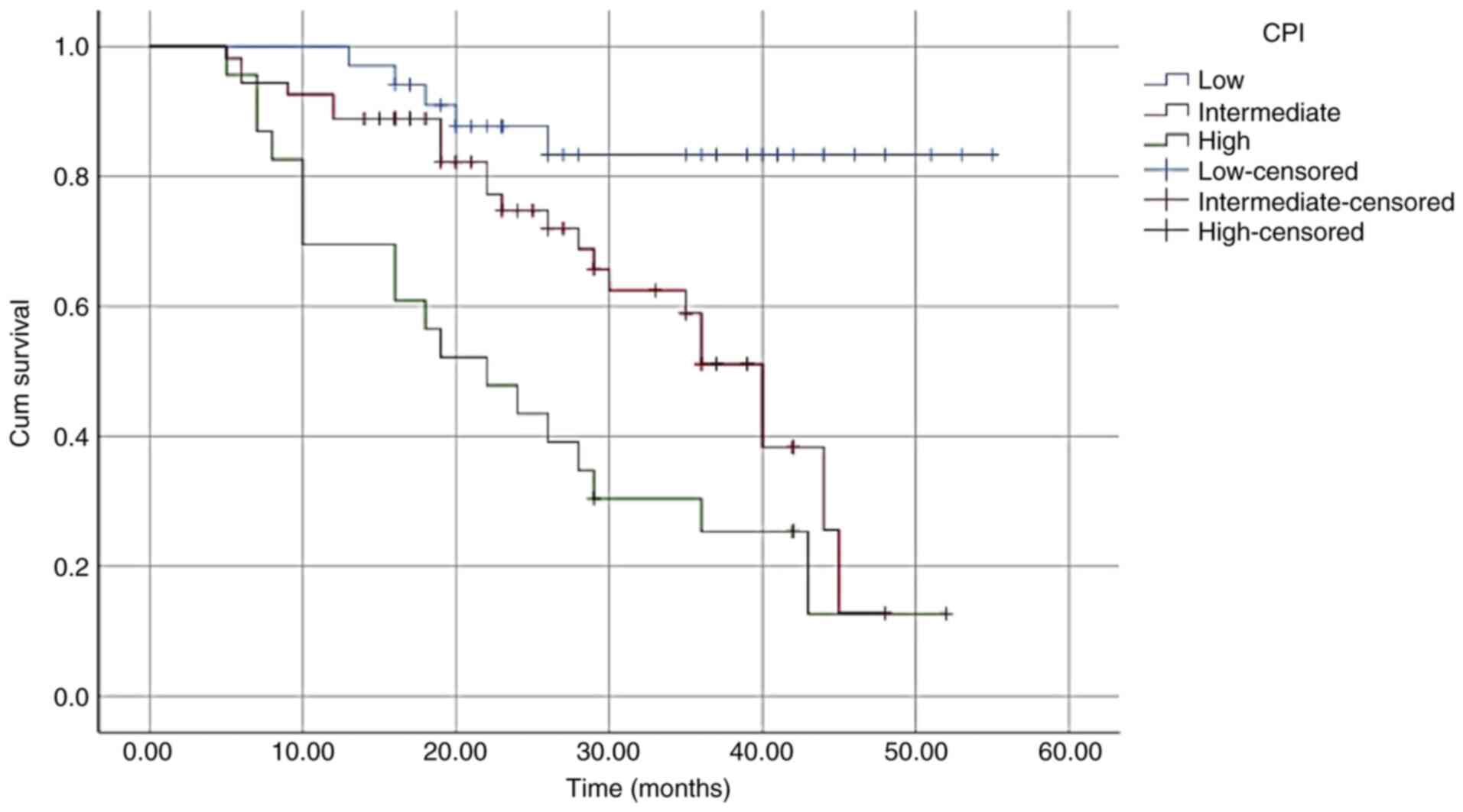
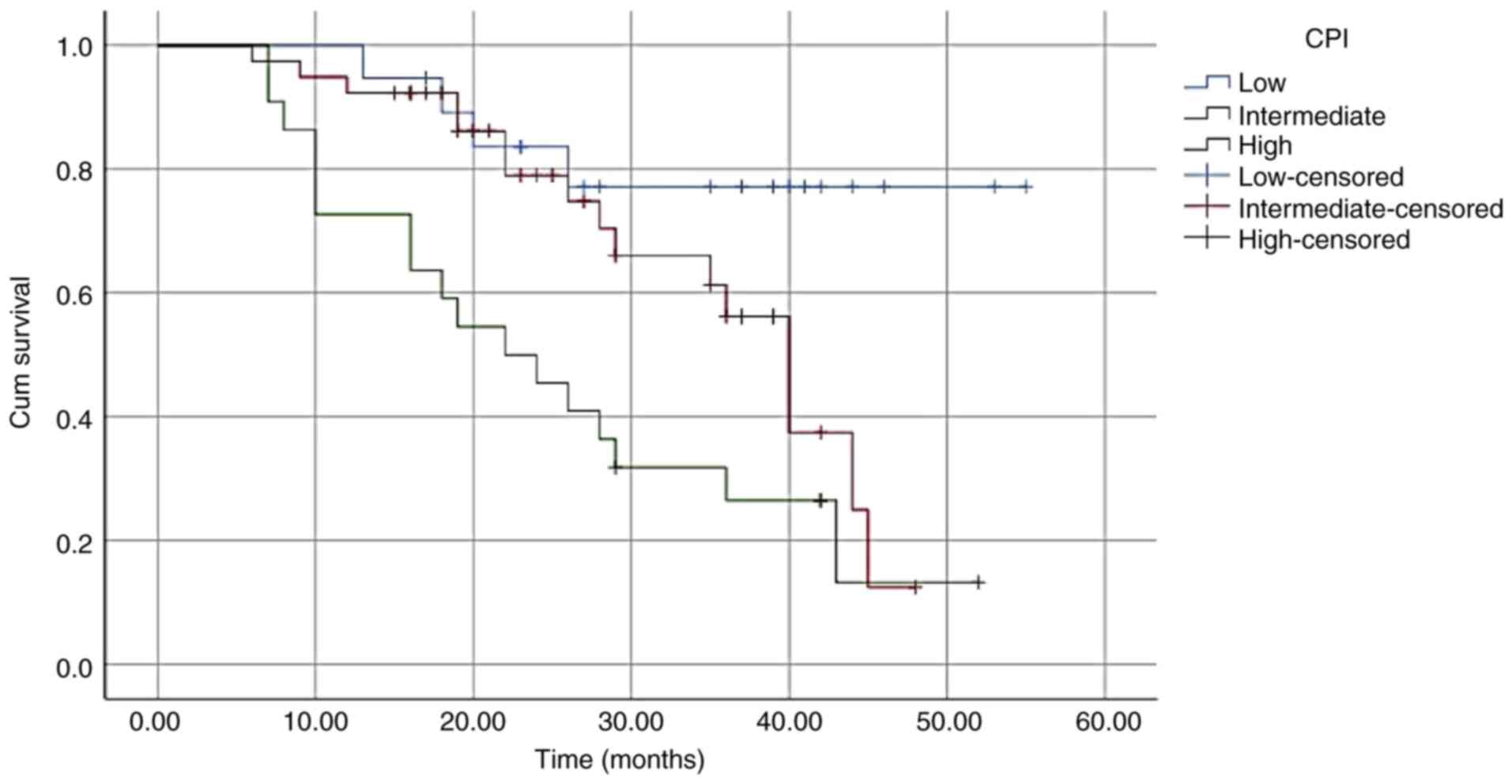
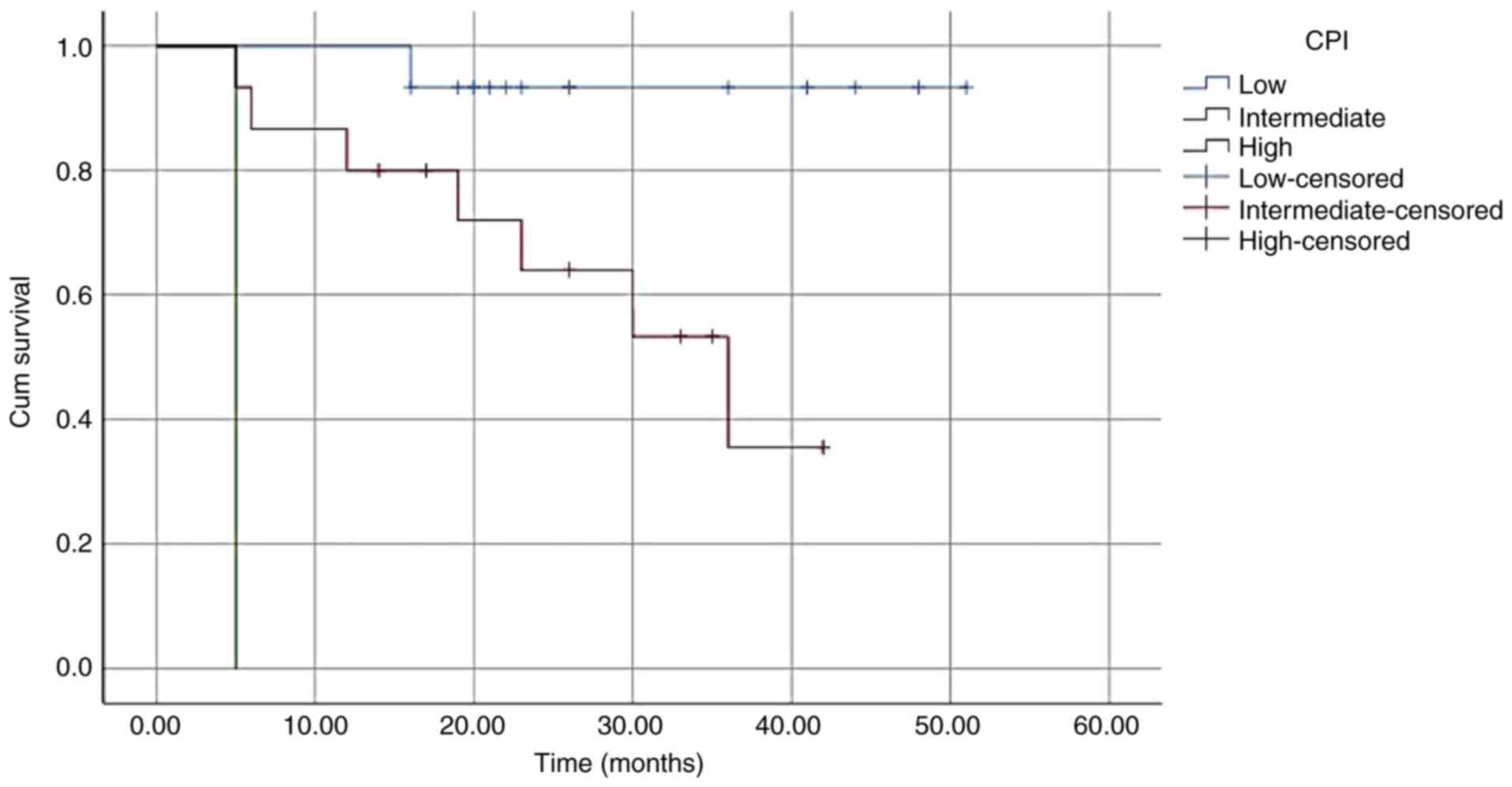
Role of CPI in survival analysis
Univariate analysis demonstrated that significant
associations were noted between the three CPI groups (P<0.001;
Table IV and Fig. 1). Multivariate analysis suggested
that the CPI was an independent prognostic factor for OS
[intermediate-risk group: Hazard ratio (HR), 3.244; 95% confidence
interval (CI), 1.213-8.679; high-risk group: HR, 4.290; 95% CI,
2.180-8.443; P<0.001; Table
IV]. This level of significance was also observed in the
subgroups that were divided according to age (≥ or <65 years)
and to the percentage of bone marrow plasma cells (≥ or <30%;
Table V, Fig. 2, Fig.
3, Fig. 4 and Fig. 5).
 | Table IVCPI used in the survival
analysis. |
Table IV
CPI used in the survival
analysis.
| | Univariate
analysis | Multivariate
analysis |
|---|
| Factor | OS (months) | P-value (log-rank
test) | HR | 95% CI | P-value (Cox
analysis) |
|---|
| CPI | | | | | |
|
Low-risk | 49.048 | <0.001 | 1 | | <0.001 |
|
Intermediate-risk | 34.009 | | 3.244 | 1.213-8.679 | |
|
High-risk | 24.960 | | 4.290 | 2.180-8.443 | |
| Bone marrow plasma
cells (%) | | | | | |
|
<30 | 40.529 | 0.004 | 1 | | 0.009 |
|
≥30 | 31.815 | | 2.270 | 1.228-4.196 | |
 | Table VOS determined according to the CPI in
the groups of plasma cell percentage and age. |
Table V
OS determined according to the CPI in
the groups of plasma cell percentage and age.
| Factor | CPI | OS (months) | P-value |
|---|
| Plasma cell count,
<30% | Low | 51.429 | 0.001 |
| | Intermediate | 34.785 | |
| | High | 31.757 | |
| Plasma cell count,
≥30% | Low | 38.662 | <0.001 |
| | Intermediate | 33.797 | |
| | High | 17.545 | |
| Age <65
years | Low | 46.912 | 0.001 |
| | Intermediate | 35.119 | |
| | High | 25.867 | |
| Age ≥65 years | Low | 48.667 | <0.001 |
| | Intermediate | 29.427 | |
| | High | 5.000 | |
Discussion
Hypercalcemia is noted in several cancer types,
inflammatory conditions and specific diseases, which are usually
caused by increased bone resorption due to increased osteoclast
activity (21). During the
development of MM, the increased osteoclastic bone resorption is
caused by cytokines (receptor activator of the nuclear factor-κB
ligand, macrophage inflammatory protein-1α and tumor necrosis
factors) that are oversecreted by myeloma or other types of cells
in the bone marrow microenvironment (22). Secondly, patients with MM often
have impaired renal function and increased renal tubular calcium
reabsorption. Therefore, this causes an elevation in serum calcium
levels (22).
Several studies have focused on the prognostic value
of the serum calcium levels in patients with MM. Zagouri et
al (23) suggested that
hypercalcemia was related to a two-fold increase in the risk of
early mortality. Similarly, Cheng et al (24) indicated a statistically significant
difference in the mortality rate between the groups of patients
with serum calcium levels > or <2.44 mmol/l. Qian et
al (6) suggested that a high
serum calcium level of 2.75 mmol/l was a poor prognostic factor for
OS. The present study demonstrated that a high serum calcium level
of 2.665 mmol/l was also an independent adverse prognostic factor
for OS.
Recent studies have investigated the application of
various inflammatory factors as prognostic indices in patients with
MM. Inflammatory factors have a substantial impact on the tumor
microenvironment and in tumor progression; therefore, they are
related to the prognosis of patients with malignant diseases
(25). Inflammation-related
indices derived from peripheral blood cells, including NLR, PLR and
MLR, are considered prognostic biomarkers (8).
The majority of the studies have agreed on the
prognostic value of NLR. Zhang et al (8), Liu et al (9), Kim et al (10), Szudy-Szczyrek et al
(11) and Zuo et al
(12) suggested that a high NLR
was an adverse prognostic factor; however, no consensus was
reported on its cut-off value (8-12).
These cut-off values ranged from 2 to 3.1 (9-12).
The data of the present study indicated that a high NLR (2.245) was
an independent prognostic factor for a poor survival rate of
patients with MM.
Platelets are an important factor involved in the
development of inflammation. Multiple inflammatory elements are
present in platelets, which can activate innate immune cells and
stimulate the endothelium. Platelets interact with leukocytes and
support their interaction with the vessel wall, which enables their
migration to the tissues (26). In
various cancer types, platelets protect metastatic cancer cells
from surveillance by natural killer (NK) cells. They also reduce
the beneficial effects of immunotherapy (27). Therefore, the role of platelets in
the prognosis of MM is very complex. An increase or decrease in
platelet levels has been considered to be a poor prognostic factor
for MM. Previous studies by Liu et al (9) and Kim et al (10) have demonstrated that a low platelet
count (<150x109/l) is a poor prognostic factor in MM.
The current study also indicated similar results. In contrast to
these findings, Jung et al (20) considered a value below
100x109/l to be used as a prognostic factor for MM.
However, a higher level of alert is required when assessing patient
prognosis. A recent study by Mellors et al (28) indicated that following two cycles
of chemotherapy treatment with novel agents, patients with MM and
thrombocytopenia (<150x109/l) exhibited worse OS and
PFS survival rates than those of patients who maintained a platelet
count ≥150x109/l.
The combination of the prognostic factors can be
used to establish an accurate prognostic system. This has been a
challenge for several studies that have investigated MM (9,10,15,16).
In addition to the successful prognostic systems that have been
recognized for several years, such as the ISS or the R-ISS, novel
valuable systems are currently investigated, notably those that
exhibit potential applications with novel treatment regimens.
Kim et al (10) demonstrated that the MPI value
included the following parameters: NLR, platelet count and CRP for
patients with MM. The MPI applies to conventional chemotherapy, as
well as to novel agents (10). Liu
et al (9) identified the
value of IPSI including the following parameters: NLR, PLT and RDW.
IPSI supports the use of ISS by further dividing the subgroups at
each disease stage (9). The
present study focused on providing a prognostic scale (CPI) that
combines simple pathological factors. Serum calcium levels may be
an indicator of the tumor growth. The NLR is an inflammatory marker
that affects the tumor microenvironment and tumor progression.
Platelets protect cancer cells from NK cells and may reverse the
effects of immunotherapy. These indices are easy to evaluate and
not expensive. Furthermore, the CPI was also applicable to all
subgroups of patients regardless of the percentage of bone marrow
plasma cells (≥30 or <30%) and the age (≥65 or <65
years).
The present study exhibits certain limitations.
Firstly, it was not performed on a group of patients who had
received autologous stem cell transplantation. Secondly, this was
merely an initial research study and additional studies with a
larger number of patients who will be treated with novel drugs need
to be conducted in the future.
In conclusion, the present study demonstrates that
the CPI, which comprises high serum calcium levels, a high NLR and
a low PLT, can be used as an independent prognostic factor for
patients with MM. The combination of the prognostic factors can be
used to establish an accurate prognostic system. As it is the
result of a combination of factors, it is more predictive than
using each factor individually. Moreover, the usage is also very
simple and convenient.
Acknowledgements
The authors would like to thank Dr Duc Anh Nguyen,
from the Hanoi Obstetrics and Gynecology Hospital, Hanoi, Vietnam,
for his efforts in supporting the research. The present study was
carried out at the Center of Hematology and Blood Transfusion, Bach
Mai Hospital, Hanoi, Vietnam.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MPV conceived the study. MPV and VTH designed the
study. VTH, PTP and HV were involved in data collection and
processing. MPV, VTH, PTP and HV were involved in data analysis and
interpretation, as well as in the literature search. MPV was
involved in the writing of the manuscript. MPV and VTH confirm the
authenticity of the all raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The study protocol was approved by the Ethical
Committee in Hanoi Medical University (no. 187). Patient consent
was waived by the committee as the present study was a
retrospective observational study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that have no competing
interests.
References
|
1
|
Fairfield H, Falank C, Avery L and Reagan
MR: Multiple myeloma in the marrow: Pathogenesis and treatments.
Ann N Y Acad Sci. 1364:32–51. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Wallington-Beddoe CT and Mynott RL:
Prognostic and predictive biomarker developments in multiple
myeloma. J Hematol Oncol. 14(151)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Bustoros M, Mouhieddine TH, Detappe A and
Ghobrial IM: Established and novel prognostic biomarkers in
multiple myeloma. Am Soc Clin Oncol Educ Book. 37:548–560.
2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Afram G, Gran C, Borg Bruchfeld J, Wagner
AK, Hussein A, Alici E and Nahi H: Impact of performance status on
overall survival in patients with relapsed and/or refractory
multiple myeloma: Real-life outcomes of daratumumab treatment. Eur
J Haematol. 105:196–202. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Cai Y, Zhao Y, Dai Q, Xu M, Xu X and Xia
W: Prognostic value of the albumin-globulin ratio and
albumin-globulin score in patients with multiple myeloma. J Int Med
Res. 49(300060521997736)2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Qian J, Jin J, Luo H, Jin C, Wang L, Qian
W and Meng H: Analysis of clinical characteristics and prognostic
factors of multiple myeloma: A retrospective single-center study of
787 cases. Hematology. 22:472–476. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chen R, Zhang X, Gao C, Luan C, Wang Y and
Chen B: Treatment and prognostic factors for survival in newly
diagnosed multiple myeloma patients with bortezomib and
dexamethasone regimen: A single Chinese center retrospective study.
Cancer Manag Res. 9:373–380. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zhang X, Duan J, Wen Z, Xiong H, Chen X,
Liu Y, Liao K and Huang C: Are the derived indexes of peripheral
whole blood cell counts (NLR, PLR, LMR/MLR) clinically significant
prognostic biomarkers in multiple myeloma? A systematic review and
meta-analysis. Front Oncol. 11(766672)2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Liu S, Shi J, Guo H, Xu F, Wei M, Sun K
and Chen Y: Prognostic significance of the inflammatory index-based
scoring system in patients preliminarily diagnosed with multiple
myeloma in the bortezomib-based chemotherapy era. Cancer Manag Res.
11:9409–9420. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kim DS, Yu ES, Kang KW, Lee SR, Park Y,
Sung HJ, Choi CW and Kim BS: Myeloma prognostic index at diagnosis
might be a prognostic marker in patients newly diagnosed with
multiple myeloma. Korean J Intern Med. 32:711–721. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Szudy-Szczyrek A, Mlak R, Mielnik M,
Szczyrek M, Nowaczyńska A, Homa-Mlak I, Zmorzyński S, Kuśmierczuk
K, Sompor J, Filip A, et al: Prognostic value of pretreatment
neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in
multiple myeloma patients treated with thalidomide-based regimen.
Ann Hematol. 99:2881–2891. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zuo H, Zhai L, Liu X, Gao H and Xu P:
Prognostic significance of neutrophil-lymphocyte ratio in multiple
myeloma patients. Transl Cancer Res. 7:88–96. 2018.
|
|
13
|
Gui L, Wang F, Shi J and Chen B: The
significance of inflammatory markers in the prognosis of newly
diagnosed multiple myeloma patients. Blood. 136 (Suppl
1)(S15)2020.
|
|
14
|
Solmaz S, Uzun O, Acar C, Sevindik OG,
Piskin O, Ozsan HG, Demirkan F, Undar B, Alacacioglu A, Ozcan MA
and Alacacioglu I: Is the platelet-to-lymphocyte ratio a new
prognostic marker in multiple myeloma? J Lab Physicians.
10:363–369. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Greipp PR, San Miguel J, Durie BG, Crowley
JJ, Barlogie B, Bladé J, Boccadoro M, Child JA, Avet-Loiseau H,
Kyle RA, et al: International staging system for multiple myeloma.
J Clin Oncol. 23:3412–3420. 2005.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Palumbo A, Avet-Loiseau H, Oliva S,
Lokhorst HM, Goldschmidt H, Rosinol L, Richardson P, Caltagirone S,
Lahuerta JJ, Facon T, et al: Revised international staging system
for multiple myeloma: A report from international myeloma working
group. J Clin Oncol. 33:2863–2869. 2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Rajkumar SV: Multiple myeloma: 2016 Update
on diagnosis, risk-stratification, and management. Am J Hematol.
91:719–734. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Azam F, Latif MF, Farooq A, Tirmazy SH,
AlShahrani S, Bashir S and Bukhari N: Performance status assessment
by using ECOG (eastern cooperative oncology group) score for cancer
patients by oncology healthcare professionals. Case Rep Oncol.
12:728–736. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Garderet L, D'Souza A, Jacobs P, van
Biezen A, Schönland S, Kroeger N, Morris C and Hari P: Response
assessment in myeloma: Practical manual on consistent reporting in
an era of dramatic therapeutic advances. Biol Blood Marrow
Transplant. 23:1193–1202. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Jung SH, Cho MS, Kim HK, Kim SJ, Kim K,
Cheong JW, Kim SJ, Kim JS, Ahn JS, Kim YK, et al: Risk factors
associated with early mortality in patients with multiple myeloma
who were treated upfront with a novel agents containing regimen.
BMC Cancer. 16(613)2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Deftos LJ: Hypercalcemia in malignant and
inflammatory diseases. Endocrinol Metab Clin North Am. 31:141–158.
2002.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Oyajobi BO: Multiple
myeloma/hypercalcemia. Arthritis Res Ther. 9 (Suppl
1)(S4)2007.PubMed/NCBI View
Article : Google Scholar
|
|
23
|
Zagouri F, Kastritis E, Zomas A, Terpos E,
Katodritou E, Symeonidis A, Delimpasi S, Pouli A, Vassilakopoulos
TP, Michalis E, et al: Hypercalcemia remains an adverse prognostic
factor for newly diagnosed multiple myeloma patients in the era of
novel antimyeloma therapies. Eur J Haematol. 99:409–414.
2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Cheng J, Zhang W, Zhao Y, Li X, Lv R, Li H
and Chen J: Association of serum calcium levels with renal
impairment and all-cause death in Chinese patients with newly
diagnosed multiple myeloma: A cross-sectional, longitudinal study.
Nutr Metab (Lond). 18(19)2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Greten FR and Grivennikov SI: Inflammation
and cancer: Triggers, mechanisms and consequences. Immunity.
51:27–41. 2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Arman M, Payne H, Ponomaryov T and Brill
A: Role of Platelets in Inflammation. Intechopen, 2015. https://www.intechopen.com/chapters/48530.
|
|
27
|
Karachaliou N, Pilotto S, Bria E and
Rosell R: Platelets and their role in cancer evolution and immune
system. Transl Lung Cancer Res. 4:713–720. 2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Mellors P, Binder M, Buadi FK, Lacy MQ,
Gertz MA, Dispenzieri A, Hayman SR, Kapoor P, Gonsalves WI, Hwa Y,
et al: Development of thrombocytopenia and survival outcomes in
newly diagnosed multiple myeloma. Blood. 132 (Suppl
1)(S1902)2018.
|