Introduction
Infectious spondylodiscitis (IS) is an inflammation
of both the vertebrae and vertebral discs, extending towards the
adjacent structures and resulting in the deterioration of the
affected locations (1). Vertebral
osteomyelitis is a rare occurrence, the incidence of which is ~2.4
cases per 100,000 individuals, and increasing with age (from 0.3
per 100,000 individuals aged ≤20 years to 6.5 per 100,000
individuals aged ≥70 years) (2,3).
There are two types of IS: Pyogenic and
granulomatous (tuberculous, brucellar, fungal and parasitic)
(4-6).
Currently, tuberculosis accounts for ~24% of cases, while the
majority of cases are pyogenic (5). Moreover, IS may have an acute,
subacute, or chronic clinical course (7).
IS is characterized by an insidious onset and
non-specific symptoms, such as back pain, fever, general malaise,
weakness and weight loss. Due to the lack of specific symptoms, an
early diagnosis is difficult and is often delayed by several weeks
or even months (1). Diabetes,
malnutrition, steroid therapy, rheumatic diseases and spinal
surgery are risk factors for IS, whereas an older age worsens the
prognosis (1,7,8).
Pathogens can infect the spine via three routes: By
hematogenous spread, by direct external inoculation, or by spread
from contiguous tissues (4). The
most frequent route is the arterial one, which allows the seeding
of infection from primary localizations to the spine (4,9).
Pyogenic spondylodiscitis preferentially affects the lumbar spine
(60%), followed by the thoracic (30%) and cervical spine (10%). The
involvement of posterior elements of vertebrae is very rarely
encountered in pyogenic spondylodiscitis, while it is more common
with tuberculous and fungal spondylodiscitis (1,2,4-12).
From the literature, it is evident that there is an
increased rate of primary and secondary bacterial infections during
the COVID-19 pandemic (13-18).
The present study is a case series study of 6 cases of pyogenic
spondylodiscitis. The present study aimed to describe the prevalent
etiology, together with clinical characteristics and main
complications of the condition.
Patients and methods
A specific time span was selected for a
retrospective evaluation. From January 1 to June 30, 2022, all case
of spondylodiscitis admitted at the Infectious Disease Unit of the
Garibaldi Hospital in Catania (Italy) were included. Their medical
history, comorbidities, location of spondylodiscitis, time spent in
hospital, age, pre-admittance treatment, possible causes of illness
and clinical, laboratory and microbiology diagnosis were collected.
To confirm the diagnosis of spondylodiscitis and exclude other
causes, original radiographs, computed tomography images (CT), with
CT-guided needle aspiration, magnetic resonance imaging (MRI) and
transesophageal echocardiogram (TEE) images were evaluated. A
measure of the pain intensity of the patients was performed using a
numerical rating scale (NRS), which ranged from 0 (lowest pain
intensity) to 10 (highest pain intensity). All the patients were
>18 years of age and signed a general written informed consent
for study purposes upon admission. This research was conducted
according to the Declaration of Helsinki. It was approved as a
retrospective minimally invasive experimental study by the
Provincial Review Board of Messina on June 29, 2020, with the
protocol no. 63/20 bis. During the 6-month time span, 6 consecutive
cases entered the Unit of Infectious Diseases of the ‘Garibaldi’
Hospital in Catania, Italy for clinical management.
Case 1
A 53-year-old male with a medical history of
thyroidectomy, monoclonal gammopathy and cutaneous leishmaniasis
presented with fever and back pain radiating to the chest, lasting
for 1 month. Upon admission to the ward, the patient was in good
condition, apart from intense lower back pain, mostly on the left
side. His blood pressure (BP) was 150/100 mmHg, his heart rate (HR)
64 bpm, oxygen saturation (SpO2) was 99% in ambient air
(AA) and his body temperature was 36.5˚C. A physical examination
(PE) of the chest revealed physiological breath sounds, rhythmic
heart activity and a 2/6 systolic murmur to the centrum cordis. A
blood cell count analysis revealed a white blood cell (WBC) count
of 6,400/µl, C-reactive protein (CRP) levels of 12 mg/l (normal
values, ≤5 mg/l) and an erythrocyte sedimentation rate (ESR) of 88
mm/h. During the admission, Wright's sero-diagnosis was performed
to detect any contact with Brucella spp., which yielded
negative results, and an interferon-gamma release assay (IGRA;
QuantiFERON®, Qiagen GmbH), which yielded weak positive
results. Blood and needle aspiration cultures yielded negative
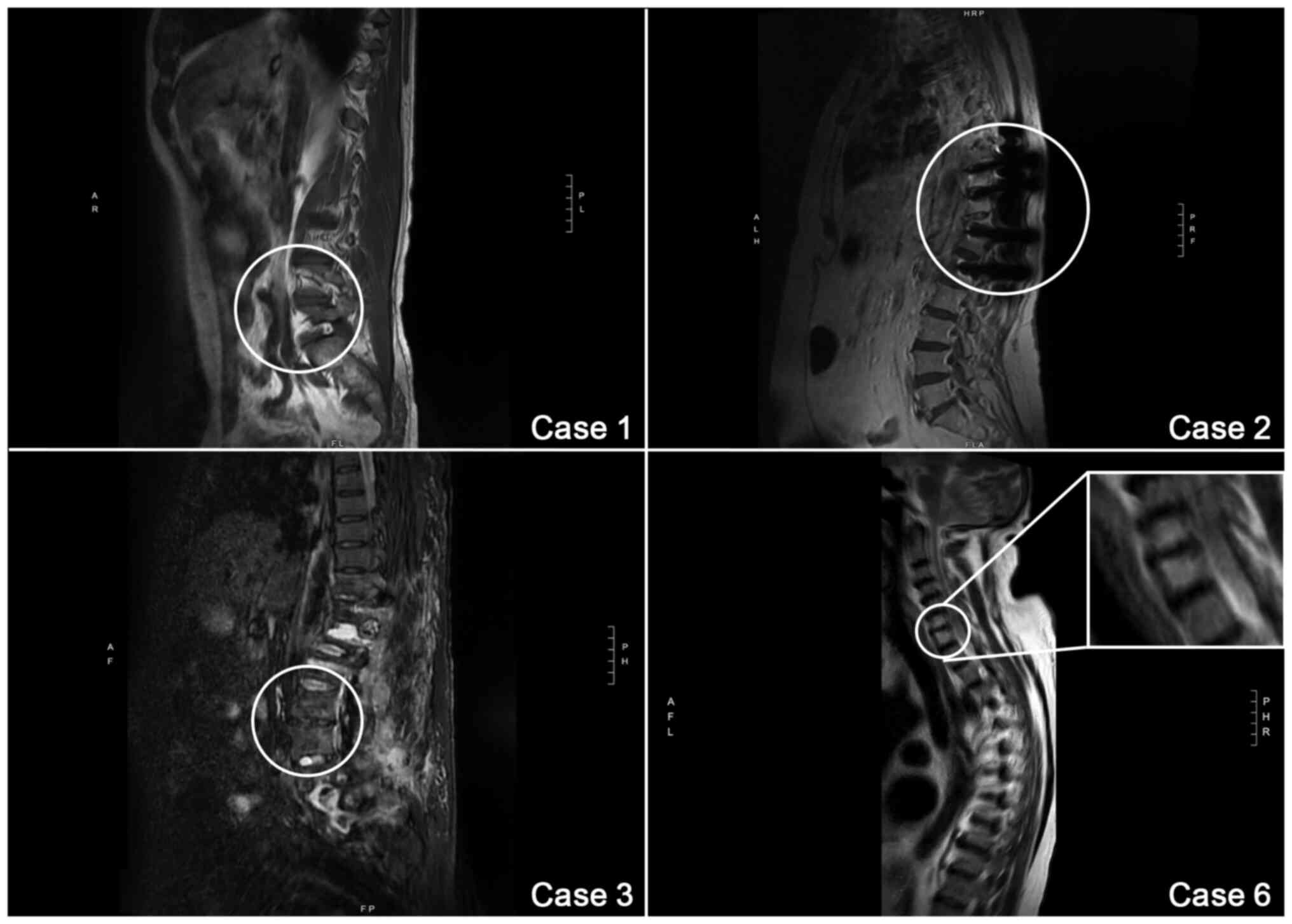
results. The first MRI of the spine, carried out on the 7th day
since admission, revealed a spondylitis (D7-D8) and a collection of
fluids inside the spinal canal (D4-D8) (Fig. 1, case 1). An antibiotic therapy
with intravenous (i.v.) teicoplanin at 12 mg/kg four times a day
(qid) and i.v. Fosfomycin at 4 g qid was commenced. Despite
antibiotic therapy, a fever (body temperature, >37.5˚C) was
observed on the 17th, and 33rd day since the admission. The patient
underwent another MRI on the 33rd day since the admission, which
revealed a slight improvement of the vertebral inflammation and the
abscess. On the 36th day since the admission, a transthoracic
echocardiogram (TTE) revealed the presence of three rounded
hyperechogenic formations: The first one (maximum diameter, 8x6 mm)
was on the posterior flap of the mitral valve, the second one
(maximum diameter, 6x3 mm) was on the front flap and the third one
(maximum diameter, 7x6 mm) was on the free margin of the coronary
cusp of the aortic valve. Therefore, he underwent a TEE which only
confirmed the presence of two small endocarditic formations on a
coronary cusp of the aortic valve, with the mitral valve free from
endocarditic formations. A diagnosis of infectious endocarditis was
then made. Therapy with gentamicin at 3 mg/kg qid was commenced,
according to the European Society for Cardiology (ESC) guidelines
(19), and teicoplanin was
replaced with daptomycin at 12 mg/kg qd iv. Therapeutic drug
monitoring (TDM) for gentamicin was performed. Following the
appearance of a skin rash, the antibiotic treatment was terminated.
Teicoplanin, gentamicin and fosfomycin were commenced again after a
48-h wash-out. The patient was treated for a total of 68 days with
teicoplanin and Fosfomycin, and 15 days of gentamycin. At 3 days
after gentamicin treatment was terminated, he underwent a TTE which
revealed scarring on the aortic valve and a mild valvular
insufficiency. After 68 days from the admission, a re-evaluation
with an MRI revealed a marked regression of the spondylodiscitis
images. On day 83, his blood count revealed a WBC count of 4,100/µl
(neutrophils, 49.4%). His CRP level was 1.9 mg/l and the ESR was 17
mm/h. The patient was discharged on day 92.
Case 2
A 73-year-old female, affected by arterial
hypertension, underwent a D9-L1 arthrodesis for a T11 inveterate
fracture in 2020. She came to our attention as an outpatient for
persisting back pain. She had also undergone an MRI of the spine
which revealed inflammatory lesions at the D8-D9 level, compatible
with spondylodiscitis by superinfection (Fig. 1, case 2).
Upon admission to the ward, the patient was in good
general condition. Her BP was 150/70 mmHg, her HR was 92 bpm and
SpO2 was 95% in AA. She complained of hyposthenia in the
lower limbs, which indicated non-elicitable tendon reflexes. A
blood count analysis revealed a WBC count of 7,400/µl, a CRP level
of 310.9 mg/l, and an ESR of 65 mm/h. Wright's sero-diagnosis and
IGRA tests yielded negative results. Both blood cultures and a
CT-guided needle aspiration of the vertebral location revealed
infection with resistant Staphylococcus aureus. The results
of the MRI of the spine was affected by ferromagnetic artifacts of
the previously positioned vertebral stabilization system.
Therefore, she underwent a CT scan of the spine which revealed an
alteration of the D8-D9 soma. The patient underwent a TTE and TEE
on the 19 and 25th day of hospitalization, respectively. These
imaging tests did not reveal any endocardial vegetation. Antibiotic
therapy with daptomycin at 8 mg/kg qid (i.v.) and rifampicin at 10
mg/kg twice a day (bid; i.v.) was commenced. Treatment with
meropenem at 1 g three times a day (tid; i.v.) was added based on
the antibiogram due to a mild increase in CRP levels, for a total
of 40 days. A consulting neurosurgeon gave no indication of surgery
and suggested to mobilize the patient with a back brace. She also
underwent kinesiotherapy daily for neuromuscular reinforcement. The
patient was discharged on day 58 in good general condition. She
continued the antibiotic treatment with rifampicin at 450 mg bid,
doxycycline at 100 mg bid and cefixime 400 mg at qid for an
additional 28 days.
Case 3
A 73-year-old female, presented to the Infectious
Diseases Unit of the ‘Garibaldi’ Hospital in Catania, affected by
diabetes mellitus type 2, arterial hypertension, dyslipidemia,
depressive syndrome, post-thyroidectomy hypothyroidism. She had
undergone an arthrodesis of thoracic and lumbar vertebrae in 2015
and 2017. Following a surgical wound dehiscence, the prosthetic
material used for the arthrodesis was removed and cultured,
revealing infection with methicillin-resistant Staphylococcus
aureus (MRSA) and Enterococcus faecalis. Therefore, she
was admitted to the infectious disease ward to undergo antibiotic
treatment. Upon admission, she was feverish, but in a good overall
condition; her BP was 110/60 mmHg, her HR was 75 bpm, her
SpO2 was 96% in AA and her body temperature was 38.0˚C.
A PE highlighted a fistula formation on the surgical scar. Blood
tests revealed a WBC count of 9,000/µl, CRP levels of 45.2 mg/l and
an ESR of 89 mm/h. Serial blood testing and imaging were performed
during the admission. An MRI of the spine revealed the presence of
a subfascial and paravertebral fluid collection going from L4 to
L5, also flanking the metallic bone fixators from D12 to S1
(Fig. 1, case 3). A CT of the
spine revealed a continuity solution of ~13 cm in the skin and
subcutaneous tissue of the lumbar region with hyper dense material
inside. Moreover, this area was surrounded by partially colliquated
tissue up to the fascial plane. Based on the sensitivity test
performed on a culture, a targeted antibiotic therapy with
teicoplanin at 10 mg/kg qid and doxycycline at 100 mg bid for 28
days, and gentamicin at 3 mg/kg qid for 14 days was commenced.
Following a neurosurgical consultation, the need for debridement
surgery of the fistula and surrounding tissue was highlighted;
however, succumbed due to sepsis following surgical
debridement.
Case 4
A 55-year-old male, whose clinical history revealed
recurrent dental abscesses, complained of lower back pain for ~1
month following a fall. He had undergone antalgic therapy with no
benefit. Therefore, he referred to the emergency department of
another hospital, where he was diagnosed with lumbar sciatica. For
the persistence of the symptomatology, he underwent an MRI of the
spine at an external outpatient clinic, which highlighted
spondylodiscitis in L1-L2 with lysis of the anterior cortical
profile, and an abscess in front of the vertebral soma from T10 to
L2. Upon admission to the Infectious Diseases Unit of the
‘Garibaldi’ Hospital in Catania he was in a fair general condition,
complaining of lower back pain (visual analogue scale, 7) with
functional limitation. His BP was 120/90 mmHg, his HR was 85 bpm,
his SpO2 was 97% in AA and his temperature was 37.2˚C.
Blood tests revealed a WBC count of 11,800/µl (neutrophils, 81.9%),
CRP levels of 139.7 mg/l and an ESR of 89 mm/h. Wright's
sero-diagnosis yielded negative results. The patient underwent a
CT-guided aspiration of a vertebral abscess. Pus culture revealed
the presence of MRSA, while a blood culture revealed the presence
of mixed flora, with methicillin-susceptible Staphylococcus
aureus and Pseudomonas aeruginosa. On the 8 and 25th day
he underwent a TTE and TEE, respectively to exclude endocarditic
formations of the valve systems. He had several sudden high fever
peaks (maximum body temperature, 38.5˚C). The fever disappeared
soon after the commencement of empirical antibiotic therapy with
teicoplanin at 12 mg/kg qd, levofloxacin at 750 mg qd and
fosfomycin at 4 g qid. The empirical antibiotic therapy regimen was
selected according to the patient's medical history and imaging
tests. Since the antimicrobial sensitivity tests revealed that the
etiological agent was sensitive to all the antimicrobials used for
the empirical treatment, the therapy was not changed. The patient
underwent this treatment for a total of 42 days. At the time of
discharge, blood tests revealed a WBC count of 4,300/µl CRP levels
of 9.7 mg/l and an ESR of 14 mm/h. The patient was then discharged
in a good general condition with a lumbar back brace, according to
the suggestion of the neurosurgeon. He continued antibiotic
treatment with doxycycline at 100 mg bid and levofloxacin at 750 mg
qid for a further 28 days. The second spine CT, performed at the
end of the treatment, revealed the disappearance of the abscess and
residual spondylosis in L1-L2.
Case 5
An 83-year-old male, affected by bradycardia treated
in 2020 with a bicameral pacemaker (PM), prostate cancer diagnosed
in 2019 for which he underwent radiotherapy, and carrier of a left
knee prosthesis, underwent an orthopedic evaluation at a private
practice, and an X-ray of the spine, pelvis and hip with evidence
of advanced spondylarthrosis in L3-L4, L5-S1, due to the appearance
of sudden sacroiliac pain ~4 months prior to hospitalization. For
his history of prostate cancer, upon the advice of the orthopedist,
he underwent a total body scintigraphy. The examination revealed
hyperaccumulation of radiopharmaceuticals in the lumbar vertebrae,
due to dystrophic-degenerative pathology. His oncologist then
suggested therapy with cortisone and non-steroidal
anti-inflammatory drugs. Pain reappeared upon the end of the
treatment. Therefore, he referred to the emergency department of
another hospital in Catania and was admitted to the neurosurgery
ward. During this admission, he was diagnosed with lumbar sciatica
and left lumbosacral spondylar disco-arthrosis and was then
discharged with an antalgic therapy based on morphine-like drugs.
He had to terminate the antalgic treatment due to the appearance of
drowsiness. As the lower back pain persisted, he underwent an MRI
of the lumbosacral spine at a private practice, which revealed
spondylar-discopathy L3-L4, L4-L5 and L5-S1 with bilateral
abscesses in the context of the psoas muscles. Upon admission to
the Infectious Diseases Unit of the ‘Garibaldi’ Hospital in
Catania, he was in good general clinical conditions. Vital
parameters were good: His BP was 120/50 mmHg, his HR was 80 bpm,
his SpO2 was 98% in AA and his temperature was 36.5˚C.
An empirical antibiotic therapy with teicoplanin at 12 mg/kg/die
and rifampicin at 12 mg/kg/die was commenced after obtaining
samples for blood cultures. Due to the accessory diagnostic
hypothesis of endocarditis, he underwent a TTE on the 3rd day of
admission. The examination revealed the presence of a formation on
the left aortic cusp and a thickening of the other cusps
attributable to endocarditic vegetations projecting in the left
ventricle and determining moderate aortic insufficiency. After 2
days, a TEE was performed, which confirmed the presence of three
mobile vegetations, one in each aortic cusp, and two vegetations on
the anterior mitral flap, while the electro-catheter of the PM was
free from vegetations. Therefore, gentamicin at 3 mg/Kg qid was
added to the treatment regimen and was administered for 17 days on
TDM. On the 11th day since the admission, a CT of the spine
revealed lumbo-arthrosis with osteophytes bridge and at the level
of L3-L4 and L4-L5 bone lysis and structural alteration of the
lithic type. From the blood cultures a methicillin-resistant
Staphylococcus sciuri was isolated. The bacteria tested
sensitive for empirical antibiotic treatment, which did not require
any adjustments.
On the 30th day of hospitalization, the patient
exhibited dyspnea and a sensation of thoracic constriction. An ECG
was performed, and the troponin curve was raised. After performing
a coronary angiography, which revealed an occlusion of ~90% of the
right coronary artery, he underwent a percutaneous transluminal
coronary angioplasty with the placement of two stents. After 7 days
in a cardiological environment for post-treatment observation, the
patient returned to the authors' ward to continue treatment for IS.
He underwent 56 days of treatment with rifampicin 12 mg/kg/die and
teicoplanin 12 mg/kg/die. However, on the 60th day since the
admission, the patient discharged himself against medical
advice.
Case 6
A 73-year-old male, affected by diabetes mellitus,
obesity, previous cancer of the anal-rectal joint for which he
underwent chemo- and radiotherapy with resulting actinic phimosis,
dyslipidemia and arterial hypertension, referred to the Emergency
Department of the ‘Garibaldi’ Hospital in Catania for the
appearance of cervicalgia, hypotonia and mild functional impotence
of the upper limb, reporting a recent infection of the inner ear.
He was bedridden following a left femur fracture which occurred 7
months prior to admission. He was first admitted at the Internal
Medicine Ward of the ‘Garibaldi’ Hospital, where he underwent a CT
scan of the cervical spine. The examination revealed a protrusion
of the intervertebral discs between C4-C5 and C5-C6, and the
presence of posterior marginal-somatic osteophytes in C3-C4, C5-C6
and C6-C7. He also underwent an MRI of the column, which revealed
the presence of fluid collections in the anterior epidural
intra-rachides and in the left paramedian paravertebral tissues
(Fig. 1, case 6). Blood culture
analysis yielded positive results for Streptococcus
agalactiae. A specific antibiotic therapy was commenced with
levofloxacin at 750 mg qid, and he was transferred to the
Infectious Diseases Unit of the ‘Garibaldi’ Hospital in Catania.
Upon admission, he was in a good general condition with a BP of
125/70 mmHg, a HR of 60 bpm, a SpO2 of 96% in AA, a body
temperature of 36.6˚C, hemo glucocose test resulted 230 mg/dl.
Blood test analyses revealed a WBC count of 8,730/µLl a CRP level
of 226.8 mg/l and an ESR of 55 mm/h. Wright's sero-diagnosis
yielded negative results, as IGRA did. A TTE was performed,
excluding infectious endocarditis. Treatment with rifampicin at 600
mg bid (i.v.) and teicoplanin at 600 mg bid was commenced, in
addition to levofloxacin 750 mg/die for a total of 28 days. A
contrast cervical MRI revealed that the anterior epidural
intra-rachides collection extended from C4 to D1 and highlighted
the presence of a second collection in front of the C6-C7 cervical
vertebral bodies. A consulting neurosurgeon ruled out the chance of
a surgical approach and recommended the use of a cervical
collar.
Results
The median age of the included patients in the
present study was 63 years [interquartile range (IQR), 59.5-75],
with a male to female ratio of 2:1. The median interval between the
onset of symptoms and admission was 6 months (IQR, 1.9-10.5).
The risk factors predisposing to spondylodiscitis
are presented in Table I. The most
frequent localization of spondylodiscitis observed in the patients
in the present case series was the lumbar spine (in 3 cases, 50%),
the thoracic spine in 2 cases (33.3%) and the cervical spine in 1
case (16.7%). In the 5 cases in which it was possible to isolate
the pathogenic microorganism, a targeted and specific therapy was
carried out, while in the remaining case, a broad-spectrum
empirical therapy was set up.
 | Table IDemographic data of the patients in
the present case series. |
Table I
Demographic data of the patients in
the present case series.
| Case no. | Sex | Age, years | Predisposing
factors |
|---|
| 1 | Male | 53 | Thyroidectomy,
gammopathy, cutaneous leishmaniosis |
| 2 | Female | 73 | Spine surgery
D9-L1 |
| 3 | Female | 73 | Spine surgery
D12-L5, diabetes mellitus, hypothyroidism |
| 4 | Male | 55 | Recurrent dental
abscesses |
| 5 | Male | 83 | Carrier of
pacemaker, radiotherapy for prostate cancer |
| 6 | Male | 73 | Diabetes mellitus,
obesity, rectal cancer chemo- and radiotherapy |
CT scan was used as the selected radiological
analysis tool for all patients for monitoring epidural and
paraspinal abscesses, and at diagnosis, in patients who could not
undergo an MRI. All patients had radiographic findings of
intervertebral disc space narrowing with the erosion of the
vertebral endplate and the collapse of the vertebral bodies at the
infectious level. Moreover, 1 patient (16.7%) had epidural abscess,
2 patients (33%) had paraspinal abscess accumulation, 1 patient had
both paraspinal and epidural abscesses (16%) and 1 patient had no
abscesses (16%).
A TTE was performed in all patients with
non-post-surgical spondylodiscitis. In 2 cases, the suspicion of
infectious endocarditis was raised, and the diagnostic procedure
continued with the TEE, confirming the infectious endocarditis. In
one of the 2 cases, methicillin-resistant Staphylococcus
sciuri was isolated in the blood, while in the other case, it
was not possible to detect the pathogen.
The median length of the hospital duration was 41.5
days (IQR, 32.8-54.0). All patients received parenteral
antibiotics, and the median duration of antimicrobial therapy was
55.0 days (IQR, 30.0-64.3). In addition, 1 patient underwent
surgical treatment.
Positivity in the IGRA test required a
rifampicin-sparing antibiotic treatment. All patients received a
combination therapy of at least two antibiotics for
spondylodiscitis, and in cases of associated infectious
endocarditis, gentamicin was added for a duration of 14 days. In
total, 5 out of the 6 patients received teicoplanin in combination
with rifampicin (2/5 patients) or fosfomycin (2/5 patients) or
doxycycline (1/5). In 2 cases, and particularly those with a
microbiological isolate, levofloxacin was used. Along with
antimicrobial therapy, pain management was carried out. The drug
dosages were progressively decreased, with the reduction of the
pain. In 1 case, surgical treatment was necessary to remove
infected fixation materials.
A total of 3 patients, following clinical
improvement and the results of laboratory data, were discharged
with oral therapy and 2 patients were transferred to other
departments for further treatment; 1 patient succumbed due to
sepsis following surgical debridement.
Discussion
In the present case-series, the most frequent cause
of spondylodiscitis was haematogenic dissemination, as reported in
the literature. The majority of patients with spondylodiscitis have
at least one of the risk factors, such as old age, diabetes, an
immunocompromised state, steroid therapy, infection in other foci,
history of spinal surgery (20-22).
No association was observed with urinary tract infections, although
some studies have reported such an association (3,4,21,23).
The clinical symptoms of spondylodiscitis are
associated with the affected region, with back pain being the first
symptom to appear, as observed in the cases described herein and in
literature, and this may be followed by neurological deficits, such
as muscle weakness, numbness and paralysis, which are often
misdiagnosed as overload disorders of the spine, delaying the
correct diagnosis. In the majority of cases, the disease affects
the lumbar region, followed by the thoracic and cervical region. In
all the cases in the present case series, pain radiated from the
spine to the upper or lower limbs, depending on the localization of
damage (3,7,24).
Usually, post-operative spondylodiscitis has a more acute onset,
with symptoms appearing from days to few weeks after the procedure
and being led by pain. This delay is related to the development of
inflammatory tissue in the intervertebral space, and pain increases
over time (7). It is important to
always consider vertebral osteomyelitis in patients complaining of
back pain, whose ESR is increased. As vertebral osteomyelitis is a
localized infection, fever may be absent, particularly in elderly
patients, and when there is no sign of a concurrent bloodstream
infection (22).
Microbiological isolates are of utmost importance to
pass from an empiric treatment to a targeted one. Moreover, if
there is no sign of any concurrent life-threatening infection, it
has been suggested to begin an antimicrobial treatment with i.v.
antibiotics on the basis of microbial identification and
sensitivity tests (2,12). As reported in the literature, the
most frequently isolated bacterium in spondylodiscitis is
Staphylococcus aureus followed by Enterobacteriaceae
(4,7,12,22,24).
The present case series confirms the data reported in the
literature. In fact, following the exclusion of tuberculosis and
brucellosis infections, the authors were able to isolate at least a
microorganism in 5 cases, and the most common was
Staphylococcus spp. When there are no positive blood
cultures, a bone biopsy must be performed to identify the agent
responsible for vertebral osteomyelitis and to select an
appropriate therapy (11,22). Although in the present case series
it was not possible to perform the bone biopsy, the abscess was
drained, where possible, following evaluation by the interventional
radiologist, and the collected liquid was placed in culture. The
most frequent reasons for a negative culture on a bone biopsy or on
material of aspiration, or on blood culture, are sampling errors
and prior antibiotic therapy (22).
As reported in other studies, an MRI has the highest
definition of paravertebral and epidural spaces, and it allows for
the early detection of vertebral osteomyelitis and the assessment
of any compression of neural elements, with high sensitivity and
specificity (3,8,25-27).
The use of a CT scan with contrast may be an alternative when
searching for bone destruction, in order to plan a spinal biopsy
and surgery (6). However, a CT
scan has a lower sensitivity and specificity than an MRI, and it
should only be preferred when an MRI is contraindicated (7). In the present study, all patients
underwent an MRI upon admission to the ward and were followed-up
with an MRI or CT scan at the end of the treatment period. Nuclear
medicine is becoming increasingly used for the diagnosis of
infectious diseases (28,29). Abnormal metabolic activity can be
highlighted with high sensitivity using gallium-67 citrate and
technetium-99m radioisotopes. These techniques have a ~94%
sensitivity in the diagnosis of discitis and are particularly
useful in detecting early disease. However, false negative results
have been observed, particularly in elderly patients. It is
suggested that the most probable cause may be regional ischemia;
therefore, a negative result does not offer a definitive exclusion.
18F-Fluorodeoxyglucose PET has been increasingly used to localize
vertebral abnormalities and monitor response to treatment (25,30).
The treatment of spondylodiscitis is highly
variable, depending on the team of physicians and local
preferences, although some therapeutic guidelines are available.
This results in high outcome variability (5,30).
It has been established that bone is a difficult-to-treat tissue,
since a number of antibiotics are not able to reach adequate
concentrations in it. Fluoroquinolones, clindamycin and rifampicin
achieve excellent levels in bone; β-lactam antibiotics and
glycopeptides achieve moderate levels, whereas aminoglycosides
concentrate poorly in bone (25).
When treatment cannot be delayed, particularly in febrile patients
with suspected dissemination of the infection, empiric
antimicrobial therapy should be selected among those drugs active
against Staphylococci, including MRSA, Streptococci
and Gram-negative bacilli. Usually, these regimens include
vancomycin plus a cephalosporin active on Gram-negative bacilli. In
the case of allergy or intolerance, daptomycin and a quinolone may
be included (11). In Italy,
teicoplanin, a glycopeptide with a higher tolerance and easier
handling than vancomycin is also available and has been approved
for use in acute bacterial skin and skin structure infections, bone
and joint infections, community-acquired and healthcare-acquired
pneumonia, complicated urinary tract infections and infectious
endocarditis (31). The
availability of this drug allowed for the use of vancomycin for the
patients described herein. In the present case series, teicoplanin
was often combined with rifampicin, an anti-staphylococcal
antibiotic with an excellent penetration into the bone. In
addition, fosfomycin (i.v.) was also used in complicated cases.
Fosfomycin exhibits good activity against Gram-positive and
Gram-negative microorganisms, even on multidrug-resistant strains,
and it also reaches a good concentration in bone (32-34).
However, only a limited number of studies on the use of this drug
for osteomyelitis are available (35-37).
Conservative treatment for non-specific spondylodiscitis consists
of 6 to 12 weeks of antibiotic treatment (i.v.), which may be
combined with bed rest and/or an orthosis. Conservative treatment
is the treatment of choice in the majority of the cases.
Antibiotics are administered (i.v.) for at least 2-4 weeks and then
orally (2,5,10,21,25).
A high risk of treatment failure is associated with a shorter
antibiotic (i.v.) course. The decision to discontinue the treatment
should be dependent on patient improvement, CRP and ESR
normalization (7).
However, as previously observed, there are no
updated guidelines for the duration and selection of antibiotic
therapy (4,7,25,38).
In the present case series, the i.v. therapy had to be terminated
before the lower limit of 6 weeks only in 1 case due to the patient
leaving the hospital. The other cases were treated intravenously
for >4-6 weeks, and even continued with oral therapy as their
clinical conditions dramatically improved, allowing discharge.
Patients should use a brace, corset, or lumbar
support belt. The immobilization of the affected segment is of
utmost importance in conservative therapy, since adequate
immobilization replace prolonged bed rest, improving the quality of
life of the patients from the first days of treatment. For the
cervical spine, immobilization can be achieved using a collar or
halo-fixator. For the mid-thoracic spine, a reclining brace is
sufficient (2).
In some cases, targeted antimicrobial treatment is
not sufficient and surgical debridement and stabilization is
required. The decision to use a surgical approach should be made on
the basis of clinical signs, such as the presence or signs of roots
in the MRI, spinal cord or dura mater compression, mechanical
instability or spinal deformity due to bone destruction or severe
deformity, and intractable pain (5,6).
Clinically unsuccessful medical treatment, for example in a patient
with persisting pain, may also be an indication for surgery
(6,39). Finally, surgical treatment is
necessary if the antimicrobial treatment does not stop the
progression of the disease. Surgery consists of removing the
mechanical cause of pain; therefore, decompression of neural
structures or drainage of abscesses are the most frequent
procedures (3,4,7).
Surgery is associated with a high operative risk, particularly in
elderly patients; therefore, a conservative approach should be
preferred, particularly if clinical symptoms and destruction of the
spine are mild, or when the operative risk appears too high
(21).
The present study had some limitations. Due to the
retrospective design, some important clinical characteristics may
not have been recorded. Moreover, the duration of i.v. antibiotic
treatment was selected on a case-by-case basis according to
clinical, microbiological and laboratory resolution. Moreover, it
was not possible to perform a bone biopsy for microbiological
diagnosis. The strength of the present study is the through the
description of diverse cases, which are all included in the
‘spondylodiscitis’ category, but present a detailed overview of
different aspects of the same disease.
In conclusion, the present study describes six
different cases of spondylodiscitis. This infectious disease is
difficult to diagnose, due to its confusing clinical
characteristics; the cases described herein demonstrate that it
must be always considered as a differential diagnosis in a patient
with back pain and increased levels of inflammatory markers. It is
also important to investigate the simultaneous presence of
abscesses, as well as endocarditis, as both can be either the
result or the cause of an infectious spondylodiscitis. Antibiotic
therapy should be i.v., and it should be carried out for at least 6
weeks, starting from an empirical therapy. A take-home message of
this article is related to the short time during which an otherwise
rare occurrence was observed in such a high prevalence. The
diagnostic delays and lack of specialized cures, due to the
COVID-19 pandemic, have led to the misdiagnosis of primary
infections causing the occurrence of secondary spondylodiscitis.
Possibly, due to the persistent status of emergency, even more rare
diseases presenting with a high prevalence may be observed in the
future.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MC, AM, BSC and GN conceptualized the study. BSC and
GN supervised the study. MC and BB were involved in project
administration and in formal analysis. BB, AEC, EP, LT, CM, EVR,
LL, RR, AZ and RB were involved in clinical and laboratory
investigations. MC, BB, AEC, EP, LT, CM, EVR, LL, RR, AZ and RB
were involved in data curation. BB, MC and AM were involved in the
writing and preparation of the original draft. MC, AM, BSC and GN
were involved in the writing, reviewing and editing of the
manuscript. All authors have read and approved the final
manuscript. MC, AM, and BSC confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
The present study was conducted according to the
Declaration of Helsinki. It was approved as a retrospective
minimally invasive experimental study by the Provincial Review
Board of Messina on June 29th, 2020, with the protocol no. 63/20
bis. Patients signed a written informed consent to the use of their
data for research.
Patient consent for publication
Patients signed a written informed consent to the
use of their data for research and publication purposes upon
admission.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Homagk L, Marmelstein D, Homagk N and
Hofmann GO: SponDT (spondylodiscitis diagnosis and treatment):
Spondylodiscitis scoring system. J Orthop Surg Res.
14(100)2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Zarghooni K, Röllinghoff M, Sobottke R and
Eysel P: Treatment of spondylodiscitis. Int Orthop. 36:405–411.
2012.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Cebrián Parra JL, Saez-Arenillas Martín A,
Urda Martínez-Aedo AL, Soler Ivañez I, Agreda E and Lopez-Duran
Stern L: Management of infectious discitis. Outcome in one hundred
and eight patients in a university hospital. Int Orthop.
36:239–244. 2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Gouliouris T, Aliyu SH and Brown NM:
Spondylodiscitis: Update on diagnosis and management. J Antimicrob
Chemother. 65 (Suppl 3):iii11–iii24. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Rutges JPHJ, Kempen DH, van Dijk M and
Oner FC: Outcome of conservative and surgical treatment of pyogenic
spondylodiscitis: A systematic literature review. Eur Spine J.
25:983–999. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Guerado E and Cerván AM: Surgical
treatment of spondylodiscitis. An update. Int Orthop. 36:413–420.
2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Garkowski A, Zajkowska A, Czupryna P,
Lebkowski W, Letmanowski M, Gołębicki P, Moniuszko A, Ustymowicz A,
Pancewicz S and Zajkowska J: Infectious spondylodiscitis-a case
series analysis. Adv Med Sci. 59:57–60. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Cheung WY and Luk KDK: Pyogenic
spondylitis. Int Orthop. 36:397–404. 2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Zimmerli W: Clinical practice. Vertebral
osteomyelitis. N Engl J Med. 362:1022–1029. 2010.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Li YD, Wong CB, Tsai TT, Lai PL, Niu CC,
Chen LH and Fu TS: Appropriate duration of post-surgical
intravenous antibiotic therapy for pyogenic spondylodiscitis. BMC
Infect Dis. 18(468)2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Berbari EF, Kanj SS, Kowalski TJ,
Darouiche RO, Widmer AF, Schmitt SK, Hendershot EF, Holtom PD,
Huddleston PM III, Petermann GW, et al: 2015 2015 Infectious
diseases society of America (IDSA) clinical practice guidelines for
the diagnosis and treatment of native vertebral osteomyelitis in
adults. Clin Infect Dis. 61:e26–e46. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yee DKH, Samartzis D, Wong YW, Luk KDK and
Cheung KMC: Infective spondylitis in Southern Chinese: A
descriptive and comparative study of ninety-one cases. Spine (Phila
Pa 1976). 35:635–641. 2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ceccarelli M, Marino A, Pulvirenti S, Coco
V, Busà B, Nunnari G and Cacopardo BS: Bacterial and fungal
co-infections and superinfections in a cohort of COVID-19 patients:
Real-life data from an italian third level hospital. Infect Dis
Rep. 14:372–382. 2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Bartoletti M, Pascale R, Cricca M, Rinaldi
M, Maccaro A, Bussini L, Fornaro G, Tonetti T, Pizzilli G,
Francalanci E, et al: Epidemiology of invasive pulmonary
aspergillosis among COVID-19 intubated patients: A prospective
study. Clin Infect Dis. (ciaa1065)2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Scott H, Zahra A, Fernandes R, Fries BC,
Thode HC Jr and Singer AJ: Bacterial infections and death among
patients with Covid-19 versus non Covid-19 patients with pneumonia.
Am J Emerg Med. 51:1–5. 2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Marino A, Campanella E, Stracquadanio S,
Ceccarelli M, Zagami A, Nunnari G and Cacopardo B: Corynebacterium
striatum bacteremia during SARS-CoV2 infection: Case Report,
Literature review, and clinical considerations. Infect Dis Rep.
14:383–390. 2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Temperoni C, Caiazzo L and Barchiesi F:
High prevalence of antibiotic resistance among opportunistic
pathogens isolated from patients with COVID-19 under mechanical
ventilation: Results of a single-center study. Antibiotics (Basel).
10(1080)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Garcia-Vidal C, Sanjuan G, Moreno-García
E, Puerta-Alcalde P, Garcia-Pouton N, Chumbita M, Fernandez-Pittol
M, Pitart C, Inciarte A, Bodro M, et al: Incidence of co-infections
and superinfections in hospitalized patients with COVID-19: A
retrospective cohort study. Clin Microbiol Infec. 27:83–88.
2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Habib G, Lancellotti P, Antunes MJ,
Bongiorni MG, Casalta JP, Del Zotti F, Dulgheru R, El Khoury G,
Erba PA, Iung B, et al: 2015 ESC guidelines for the management of
infective endocarditis: The task force for the management of
infective endocarditis of the European society of cardiology (ESC).
Endorsed by: European association for cardio-thoracic surgery
(EACTS), the European association of nuclear medicine (EANM). Eur
Heart J. 36:3075–3128. 2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bhavan KP, Marschall J, Olsen MA, Fraser
VJ, Wright NM and Warren DK: The epidemiology of hematogenous
vertebral osteomyelitis: A cohort study in a tertiary care
hospital. BMC Infect Dis. 10(158)2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Sobottke R, Röllinghoff M, Zarghooni K,
Zarghooni K, Schlüter-Brust K, Delank KS, Seifert H, Zweig T and
Eysel P: Spondylodiscitis in the elderly patient: Clinical mid-term
results and quality of life. Arch Orthop Trauma Surg.
130:1083–1091. 2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Torda AJ, Gottlieb T and Bradbury R:
Pyogenic vertebral osteomyelitis: Analysis of 20 cases and review.
Clin Infect Dis. 20:320–328. 1995.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Mylona E, Samarkos M, Kakalou E,
Fanourgiakis P and Skoutelis A: Pyogenic vertebral osteomyelitis: A
systematic review of clinical characteristics. Semin Arthritis
Rheu. 39:10–17. 2009.PubMed/NCBI View Article : Google Scholar
|
|
24
|
McHenry MC, Easley KA and Locker GA:
Vertebral osteomyelitis: Long-term outcome for 253 patients from 7
Cleveland-area hospitals. Clin Infect Dis. 34:1342–1350.
2002.PubMed/NCBI View
Article : Google Scholar
|
|
25
|
Cottle L and Riordan T: Infectious
spondylodiscitis. J Infect. 56:401–412. 2008.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Varma R, Lander P and Assaf A: Imaging of
pyogenic infectious spondylodiskitis. Radiol Clin North Am.
39:203–213. 2001.PubMed/NCBI View Article : Google Scholar
|
|
27
|
An HS and Seldomridge JA: Spinal
infections: Diagnostic tests and imaging studies. Clin Orthop Relat
Res. 444:27–33. 2006.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Love C and Palestro CJ: Nuclear medicine
imaging of bone infections. Clin Radiol. 71:632–646.
2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Censullo A and Vijayan T: Using nuclear
medicine imaging wisely in diagnosing infectious diseases. Open
Forum Infect Dis. 4(ofx011)2017.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Gasbarrini A, Boriani L, Nanni C,
Zamparini E, Rorato G, Ghermandi R, Salvadori C, Allegri V,
Bandiera S, Barbanti-Brodano G, et al: Spinal infection
multidisciplinary management project (SIMP): From diagnosis to
treatment guideline. Int J Immunopathol Pharmacol. 24 (Suppl
2):S95–S100. 2011.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Pan A, Lorenzotti S and Zoncada A:
Registered and investigational drugs for the treatment of
methicillin-resistant Staphylococcus aureus infection.
Recent Pat Antiinfect Drug Discov. 3:10–33. 2008.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Marino A, Stracquadanio S, Ceccarelli M,
Zagami A, Nunnari G and Cacopardo B: Oral fosfomycin formulation
for acute bacterial prostatitis; a new role for an old molecule: A
case report and brief literature review. World Acad Sci J.
4(26)2022.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Marino A, Stracquadanio S, Campanella E,
Munafò A, Gussio M, Ceccarelli M, Bernardini R, Nunnari G and
Cacopardo B: Intravenous fosfomycin: A potential good partner for
cefiderocol. Clinical experience and considerations. Antibiotics
(Basel). 12(49)2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Marino A, Stracquadanio S, Bellanca CM,
Augello E, Ceccarelli M, Cantarella G, Bernardini R, Nunnari G and
Cacopardo B: Oral fosfomycin formulation in bacterial prostatitis:
New role for an old molecule-brief literature review and clinical
considerations. Infect Dis Rep. 14:621–634. 2022.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Poeppl W, Tobudic S, Lingscheid T,
Plasenzotti R, Kozakowski N, Georgopoulos A and Burgmann H:
Efficacy of fosfomycin in experimental osteomyelitis due to
methicillin-resistant ssylococcus aureus. Antimicrob Agents
Chemother. 55:931–933. 2011.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Morata L and Soriano A: The role of
fosfomycin in osteoarticular infection. Rev Esp Quimioter. 32
(Suppl 1):S30–S36. 2019.PubMed/NCBI
|
|
37
|
Thabit AK, Fatani DF, Bamakhrama MS,
Barnawi OA, Basudan LO and Alhejaili SF: Antibiotic penetration
into bone and joints: An updated review. Int J Infect Dis.
81:128–136. 2019.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Silber JS, Anderson DG, Vaccaro AR,
Anderson PA and McCormick P: NASS. Management of postprocedural
discitis. Spine J. 2:279–287. 2002.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Chen WH, Jiang LS and Dai LY: Surgical
treatment of pyogenic vertebral osteomyelitis with spinal
instrumentation. Eur Spine J. 16:1307–1316. 2007.PubMed/NCBI View Article : Google Scholar
|