Introduction
The ongoing coronavirus disease 2019 (COVID-19)
pandemic has significantly affected social, economic, educational
and political systems (1,2). Social and economic impacts were
identified in each country (3).
Global measures to prevent the spread of COVID-19, such as school
closures and the cancelation of public gatherings, substantially
reduced the movement of the population at both the local and
national levels (4,5). Healthcare services experienced an
increase in workload due to the high incidence of patients with
COVID-19(6), apart from changes in
patient presentation at emergency departments. For instance,
changes in societal behaviors due to lockdowns and restrictions
have led to fewer vehicle-related emergencies (7). However, psychological stress caused
by the measures to prevent the spread of COVID-19 has been reported
in numerous countries (8-10).
Patients who required emergency department consultations were more
likely to need acute hospital care (11,12).
Despite these findings, the impact of COVID-19 on
emergency transport remains unclear. Studies conducted in Japan
have associated the pandemic with increased intervals between
patient collection and arrival at an emergency department (13), as well as the amount of time
required to respond to and arrive at scenes (13,14).
However, little is known about changes in emergency transport
according to conditions.
Emergency transportation is often required for
febrile urological conditions, such as acute pyelonephritis
(15) and urinary tract infections
(UTIs) (16). However, fever is a
primary symptom of COVID-19 infection (17); thus, its manifestation in a patient
requiring emergency care can prolong the wait for a response and
admission, even when patients do not have severe acute respiratory
syndrome coronavirus 2 (SARS-CoV-2) infection (18). A previous study on the association
between COVID-19 and urological diseases found a decrease in the
number of patients treated with antibiotics; however, there was no
evidence of an increase in complications, such as pyelonephritis
(19). The impact of COVID-19 on
urology services has been examined (20-24);
however, the effects of the pandemic on the emergency transport
time for patients with urological diseases remain unclear.
The present study aimed to determine the impact of
lockdown restrictions on the time required to transport patients
with urological diseases with fever to the hospital during the
early stages of the COVID-19 pandemic.
Patients and methods
Study design and setting
Japan has a national fire and ambulance service
provided by local governments and funded by taxpayers. It is
available free of charge to anyone, anytime, anywhere, by calling
the emergency telephone number 119. The municipal government
oversees the management of fire departments. The National Fire and
Disaster Management Agency, Ministry of Internal Affairs and
Communications, and Prefectural Governments provide guidance and
advice to municipal fire departments. The present study was
conducted in Kochi City, Japan, which is the largest metropolitan
area in Kochi Prefecture, with an estimated population of 320,000
individuals. Kochi Prefecture had 15 fire departments in 2021, and
Kochi City had a fire brigade headquarters and 10 fire/ambulance
stations.
Data sources
The present retrospective, observational study
analyzed information downloaded from the public Kochi-Iryo-Net
database that was established in 2015 as part of the Kochi
prefectural emergency medical and disaster information system
(https://www.kochi-iryo.net/) (25). The database contains information
about fire and ambulance dispatches and crew details, dates and
times of calls, destination medical institutions, and distance
between patients from the fire department. Upon arrival at the
destination (medical institution), an attending doctor recorded
pertinent information regarding institution names, locations where
patients were collected, types and degrees of conditions or urgency
in the institutional medical record database. The Kochi Prefectural
Government then integrated this information into the Kochi-Iryo-Net
database. The data that support the findings of the present study
are available from the Kochi Prefecture database. However, these
data are not publicly available. However, these data are not
publicly available as they report the surveillance conducted by
Kochi Prefecture Healthcare Policy Division Department for
monitoring emergency medical care. The requirement for written
informed consent from the selected participants was waived by the
Ethical Review Committee of Kochi University School of Medicine in
2020 (No. 2020-116) due to the retrospective, observational nature
of the study. The present study was approved by and complied with
the Ethical Guidelines for Medical and Biological Research
Involving Human Subjects of the Ministry of Education, Culture,
Sports, Science and Technology; Ministry of Health, Labour and
Welfare; Ministry of Economy, Trade and Industry, and the
Declaration of Helsinki (2013 amendment).
Variables
The duration of the chaotic and quarantine periods
was an exposure factor, and the outcome was urological disease.
Other variables comprised sex, age (0-69, 70-79 and ≥80 years) and
disease severity (mild, moderate, severe and fatal). Disease
severity was defined as fatal, severe, moderate, mild, or other
when mortality was confirmed at the time of the initial diagnosis,
or by hospitalization for >3, <3 weeks, no diagnosis by a
physician, and not diagnosed by a or transported to other
locations, respectively.
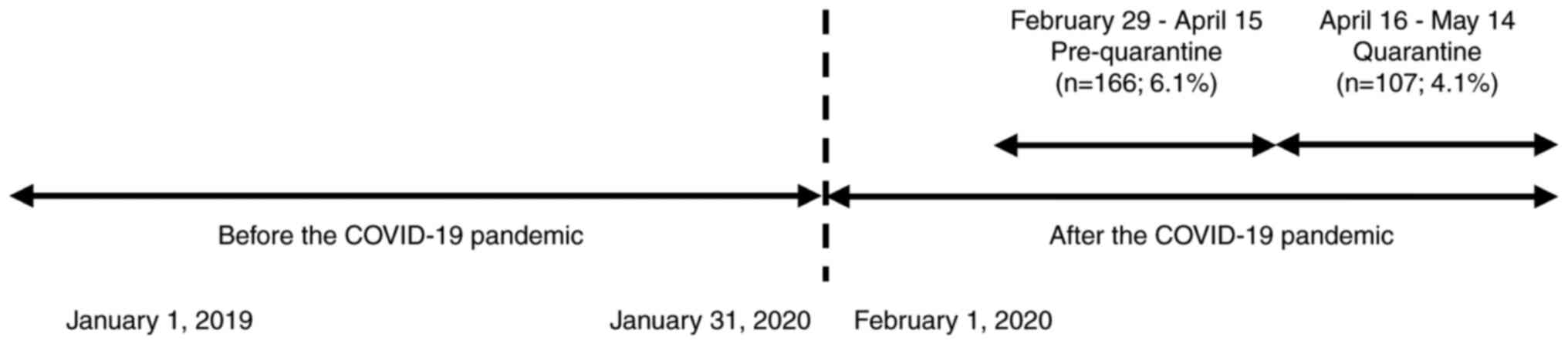
An overview of the data collection and analyzed time
frames is presented in Fig. 1.
Data were collected between January 1, 2019 and December 31, 2020.
The new coronavirus infection became a designated infectious
disease on February 1, 2020. Thus, data were defined as
pre-pandemic from January 1, 2019 to January 31, 2020. Data were
analyzed after the pandemic between February 1, 2020 and December
31, 2020. The pre-quarantine period was defined as when the first
patient was diagnosed with COVID-19 on February 29, 2020 and a
state of emergency was initially declared in Kochi Prefecture on
April 15, 2020. Quarantine began on April 16 and lasted until May
14, 2020.
Information about patients entered into the
Kochi-Iryo-Net database had to contain disease classifications and
up to three specified injuries or diseases. Patients with
urological diseases with pyelonephritis or UTIs were further
classified as having fever (n=1,255), and all others were
classified as not having a fever (n=1,556). According to previous
research, the annual incidence of hospitalization due to urinary
tract stones in Japan is estimated at 6.8 males and 12.4 females
per 10,000 individuals in the population (26).
Statistical analysis
The elapsed time between an incoming telephone call
and the moment when an ambulance arrived at a hospital was defined
as the total transport time and was compared before and after the
start of the COVID-19 pandemic. After verifying the normality of
the data with the Shapiro-Wilk test, between-group differences in
total transport time were analyzed using the Mann-Whitney U-test.
Categorical variables were analyzed using Chi-squared tests. If the
expected frequencies were too low (>20% of the cells had an
expected count of <5), Fisher's exact tests were conducted
instead of the Chi-squared tests. Bivariate associations before and
after the COVID-19 pandemic started were assessed using simple
linear and multiple regression analyses. Values with two-tailed
P<0.05 were considered to indicate statistically significant
differences. All data were analyzed using Stata/MP v.16.0
(StataCorp LLC.).
Results
The present study limited the analysis to patients
with urological diseases between 2019 and 2020, who were listed in
the Kochi-Iryo-Net database. Among these patients, 10 patients with
a transport time >1,000 min (n=10) were excluded from the study
as previously described (27); the
transport time exceeding 1,000 min usually does not exceed 180 min
one-way, even if the patient was transported from the eastern or
western edge of Kochi Prefecture to the center of the prefecture.
Although there were rare cases in which the transport time was
extended due to disease, the time exceeding 1,000 min was
considered an anomaly due to an error in the entry of the transport
time. Data derived from 2,811 transported patients were finally
analyzed.
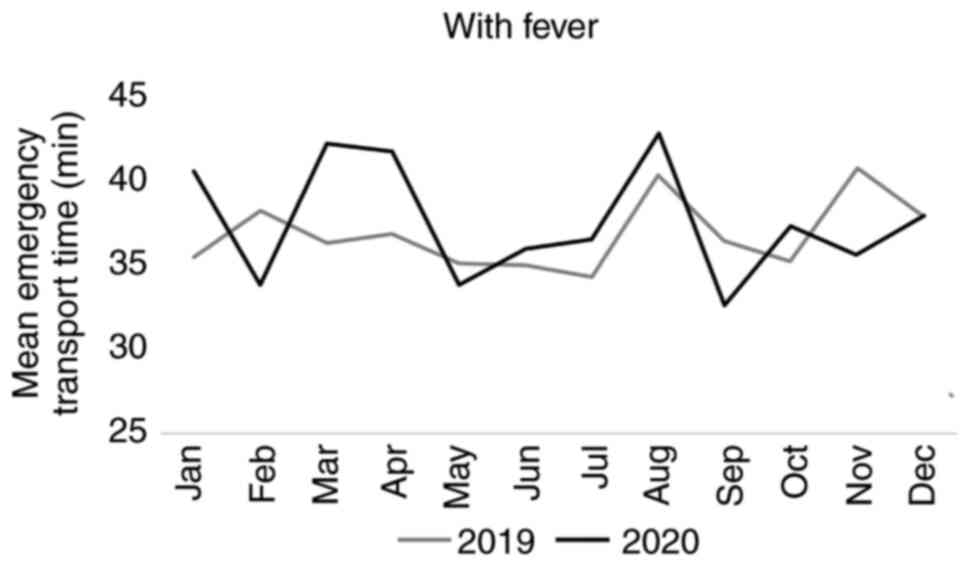
As illustrated in Fig.
2, the emergency transport time was the long during March and
April, 2020 for patients with urological diseases with fever during
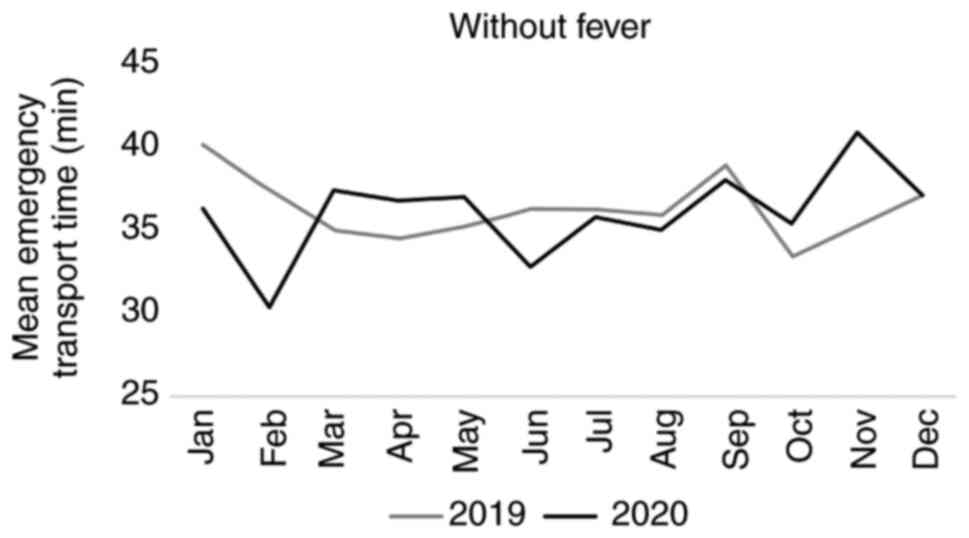
the entire study period compared to 2019. As shown in Fig. 3, the amount of time required to
deliver patients with urological diseases without fever in the case
of an emergency to a hospital during 2019 and 2020 did not markedly
vary throughout the study period.
Of the total number of patients with urological
diseases (n=2,811) included in the present study, 1,255 patients
had urologic diseases with fever, and 1,556 patients had no fever.
The pre-quarantine (February 29 to April 15, 2020) and quarantine
(April 16 to May 14, 2020) demographics of the patients are
presented in Table I. It was found
that 75 (45.2%), 91 (54.8%) at pre-quarantine, and 49 (45.8%) and
58 (54.2%) patients during quarantine with urological diseases with
and without fever, respectively, were transported by an ambulance
during these respective time periods.
 | Table IDemographic characteristics of the
patients throughout the COVID-19 pandemic. |
Table I
Demographic characteristics of the
patients throughout the COVID-19 pandemic.
| Characteristic | All 2,811; n
(%) | Pre-quarantine 166
(60.8), n (%) | Quarantine 107
(39.2), n (%) | P-value |
|---|
| Sex | | | | |
|
Male | 1,507 (53.6) | 83 (50.0) | 63 (58.9) | 0.36a |
|
Female | 1,304 (46.4) | 83 (50.0) | 44 (41.1) | |
| Age (years) | | | | |
|
0-69 | 764 (27.2) | 39 (23.5) | 29 (27.1) | 0.55a |
|
70-79 | 645 (23.0) | 45 (27.1) | 28 (26.2) | |
|
≥80 | 1,402 (49.9) | 82 (49.4) | 50 (46.7) | |
| Severity | | | | |
|
Mild | 898 (32.0) | 55 (33.1) | 33 (30.8) | 0.96b |
|
Moderate | 1,329 (47.3) | 78 (47.0) | 54 (50.5) | |
|
Severe | 563 (20.0) | 33 (19.9) | 19 (17.8) | |
|
Death | 6 (0.2) | 0 (0.0) | 0 (0.0) | |
|
Other | 15 (0.5) | 0 (0.0) | 1 (0.9) | |
| Fever with
urological disease | | | | |
|
No
fever | 1,556 (55.4) | 91 (54.8) | 58 (54.2) | 0.96a |
|
Feverc | 1,255 (44.7) | 75 (45.2) | 49 (45.8) | |
As demonstrated in Table II, the mean duration of emergency
transport was longer for patients with urological diseases with
fever than without fever before, compared with during the
quarantine period and after the COVID-19 pandemic began.
 | Table IIMean emergency transport time (min)
in 2020 during the pre-quarantine and quarantine periods. |
Table II
Mean emergency transport time (min)
in 2020 during the pre-quarantine and quarantine periods.
| Patients with
urological diseases, n=2,811 | Pre-quarantine |
P-valuea | Quarantine |
P-valuea |
|---|
| No fever, n=1,556
(55.4%) | 37.4 (14.1) | 0.12 | 36.8 (12.9) | 0.81 |
| Fever, n=1,255
(44.7%) | 41.9 (17.2) | | 37.7 (14.6) | |
The results of simple linear and multiple regression
analyses are presented in Table
III. The mean pre-quarantine transport times were significantly
associated with fever [β=5.35; 95% confidence interval (CI),
1.69-9.01; P<0.05] and remained significant after adjusting for
sex, age and urgency (β=5.57; 95% CI, 1.93-9.21; P<0.05).
 | Table IIISimple linear and multiple regression
analyses of the mean duration of emergency transport of patients
with urological diseases. |
Table III
Simple linear and multiple regression
analyses of the mean duration of emergency transport of patients
with urological diseases.
| | | 95% CI | | | 95% CI | |
|---|
| Time point | β | SE | Lower value | Upper value | P-value | βa | SE | Lower value | Upper value | P-value |
|---|
| Pre-quarantine | | | | | | | | | | |
|
No
fever | 1.25 | 1.79 | -2.26 | 4.76 | 0.49 | 1.18 | 1.79 | -2.33 | 4.69 | 0.51 |
|
Fever | 5.35 | 1.87 | 1.69 | 9.01 | <0.05 | 5.57 | 1.86 | 1.93 | 9.21 | <0.05 |
| Quarantine | | | | | | | | | | |
|
No
fever | 0.61 | 2.22 | -3.74 | 4.95 | 0.79 | 0.68 | 2.21 | -3.66 | 5.02 | 0.76 |
|
Fever | 0.83 | 2.29 | -3.66 | 5.32 | 0.72 | 0.72 | 2.28 | -3.76 | 5.19 | 0.75 |
Discussion
The present study examined the impact of the
COVID-19 pandemic on the amount of time required for an ambulance
to transport patients with urological diseases with or without
fever in the case of an emergency in Kochi Prefecture, Japan. A
significant pre-quarantine increase was observed in the emergency
transport time for patients with urological diseases with fever.
Urological diseases are adversely affected by even a 5-min delay,
and longer waits for emergency transport can delay the appropriate
and timely administration of treatment, as well as subsequent
dispatches (28). Each fire
station in Kochi Prefecture usually has two ambulances, and if a
station is unable to respond to an emergency, an ambulance from a
neighboring station will be dispatched. The survival of patients
with serious illnesses is associated with prompt transport
(29). To the best of our
knowledge, this is the first study to find longer transport times
during the spread of COVID-19 in a rural area in Japan.
This longer time was attributed to the
implementation of infection control measures that were not
previously required (30).
Currently, these measures include hand disinfection, wearing
protective clothing and mandatory reports of suspected infections
(28,31). Other factors that likely
contributed to the increased duration of emergency transport
include the similarity between fever caused by a febrile urological
state and COVID-19 (17,32,33),
as well as delays caused by searching for a hospital that was
appropriately equipped, willing to admit a patient with suspected
COVID-19 and had a free bed. Numerous hospital beds were reserved
for or were occupied by patients with COVID-19(34).
The COVID-19 pandemic also changed the consultation
policies of urologists, according to the findings of cue-expedited
transport of patients with urological diseases (23,24,35).
The frequency of admissions with urological complaints decreased,
the pattern of referrals changed, the length of hospital stays
decreased, more patients were discharged against medical advice,
and the number of patients with irreversible urological
complications or complications requiring surgery due to deferred
treatment increased (35). Ansari
et al (36) suggested that
specific medical centers that could provide emergency services
should be selected. Such measures are certainly useful, although
they are difficult to implement in rural areas such as Kochi
Prefecture, where medical resources are limited, in contrast to
large cities, such as Tokyo and Osaka, which have ample medical
facilities. Even if such a system were developed, it is important
to recognize that its functionality is likely to change during a
period of social turmoil, such as a pandemic, as noted herein.
The measures implemented to prevent or reduce the
spread of COVID-19, including self-quarantine, have had various
effects on emergency care. Of course, the vast number of patients
infected with COVID-19 severely strained medical services; however,
the overall number of patients presenting at emergency departments
decreased in numerous parts of the world (36-38).
The various preventive measures implemented during the pandemic did
not affect emergency medical services in six US level I trauma
centers (39). Notably, the spread
of COVID-19 affected the mortality of patients who were transported
by ambulance in Osaka, Japan (40).
It is considered that the significant difference
between patients who had urological diseases with and without fever
should be noted.
Symptoms and infection status related to COVID-19
became confusing and stressful, particularly during the early
stages of the pandemic when limited information was available
(41-43).
An urgent need emerged in Japan to create a process that would not
strain the medical system (44,45).
During this period, individuals tended to avoid medical clinics and
hospitals due to fear of SARS-CoV-2 infection (46,47),
and patients with mild symptoms and those who were younger
(48,49) tended to not use emergency services
(50-52).
The period analyzed in the present study was a precursor to the
subsequent major pandemic. The Ministry of Health, Labour and
Welfare notified each prefecture that medical institutions
accepting Class II infectious diseases would accept patients with
COVID-19. On March 11, 2020, the Headquarters for the Promotion of
Countermeasures against Infectious Diseases Caused by the New Type
of Coronavirus, the Ministry of Health, Labour and Welfare,
released guidelines regarding the treatment of persons with
suspected COVID-19(53). A new
system was established in Kochi Prefecture on April 22, 2020. This
included establishing a second medical institution that would
accept persons with COVID-19 due to an increase in the demand to
care for infected patients (53).
It is considered that this system was responsible for the
difference in transport times between the pre-quarantine and
quarantine periods. The process that allocated patients with fever
to designated medical institutions may have resulted in the smooth
transportation of febrile patients with urological diseases after
May, 2020. The present study did not identify confusion caused by
circulating information about COVID-19, but rather uncovered the
reason for the difference in the transport time between the
pre-quarantine and quarantine periods.
The present study had certain limitations, which
should be mentioned. The strength of the present study was the use
of a large data set that accurately captured the number of patients
transported throughout Kochi Prefecture. The medical record
management system from which the dataset was obtained was designed
to capture all relevant data upon the dispatch of emergency
transportation. However, as the information related to the
transportation service was entered by ambulance crews in real-time,
the possibility of entering erroneous or misleading data into the
database cannot be eliminated. For example, in some data-entry
fields, a range of descriptions for the same illness can be entered
that is dependent on the discretion of the person inputting the
data (e.g., ‘pyelonephritis’ vs. ‘acute pyelonephritis’).
Currently, the classification of injuries and diseases is performed
in a selective format with a check item; however, it is necessary
to make modifications, such as using ICD-10 codes instead of a
descriptive format for the accurate registration of injury and
disease names.
Moreover, the information was manually entered into
the database via a tablet computer in each ambulance. This can lead
to data entry errors, such as using a 12-h instead of a 24-h clock,
resulting in data indicating that transport lasted for >1 day.
Transport time is an important topic in the field of emergency
care; therefore, future improvements to the system are required to
address erroneous data input, such as the simplification of entry
items, the standardization of entry formats, or a system of
double-checks. In Japan, the operation of such a system is
performed on a prefectural basis, and a separate document is
submitted to the Fire and Disaster Management Agency of the
Ministry of Internal Affairs and Communications, which has
jurisdiction over firefighting, to ascertain the number of
emergency cases transported. It is hoped that the same system can
be operated in all prefectures in Japan in the future.
Emergency medical service teams consider a case to
be difficult to accept ‘after four or more calls for acceptance to
medical institutions’ or ‘more than 30 min have elapsed since their
arrival at the scene’(54).
However, since the dataset used for the analysis did not include
any information about the above, it could not be confirmed whether
the patients who were transported by emergency medical services
over a long period of time were difficult to accept. The ability to
categorize ‘difficult to accept’ may further clarify how the field
was disrupted during this period. Another limitation is that the
body temperature of febrile patients with urological diseases could
not be verified. Additionally, the data were from only one of 47
Japanese prefectures; thus, the present findings may not be
generalizable to other prefectures. The aging rate in Kochi
Prefecture is 35.8%, which is higher than the national average of
28.8% and the second highest in Japan. The percentage of the
population aged ≥65 years in the total population of Kochi
Prefecture is one in three of the prefecture's residents. As for
the current situation of regional medical care in Kochi Prefecture,
there are few large hospitals, and there is a lack of facilities to
accept seriously ill patients. Of note, ~70% of the population of
Kochi Prefecture is concentrated in the center where the medical
school is located, while ~80% of physicians and nurses are
concentrated. Doctors and hospitals responsible for regional
medical care accept many patients with limited personnel and
facilities (54). Therefore, they
are unable to provide highly specialized medical care, and
maintaining the medical system in mountainous areas is a challenge.
While Japan is aging and its population is becoming increasingly
concentrated in one area, it is considered that the changes that
occurred in Kochi Prefecture, which has such regional challenges,
suggest that similar confusion will occur in contingencies that
occur in other prefectures in the future.
Delayed emergency transport is a life-threatening
situation for patients. In the future, the authors aim to use data
to confirm what types of occurrences increase transport times and
what types of diseases tend to do so and to compare these data with
data from other prefectures in Japan regarding emergency transport
times.
The present study revealed that the measures,
restrictions, lockdowns and lifestyle changes that limited the
spread of COVID-19 affected emergency transport time in one
prefecture in Japan during the quarantine period. Particularly, the
increase in transport duration was significant for patients with
urological diseases with fever. These results suggested that
similar delays may occur in future events when patients may develop
symptoms akin to those of a disease that causes a pandemic.
Acknowledgements
The authors would like to express their great
appreciation to the personnel of the fire departments in Kochi
Prefecture for their great efforts in collecting the data. The
authors also extend their thanks to the officials of Kochi
Prefecture for providing the data. The authors would also like
thank the Kochi University School of Disaster and Emergency
Medicine and the Kochi Prefecture Department of Health Policy for
providing insight and expertise to facilitate interpretation.
Funding
Funding: No funding was received.
Availability of data and materials
The data supporting the present findings are under
license from Kochi Prefecture and are not publicly available. The
dataset is surveillance conducted by Kochi Prefecture Healthcare
Policy Division Department, for monitoring emergency medical care
and is not publicly available, although use may be permitted after
ethical review.
Authors' contributions
MMinami was involved in the conceptualization and
methodology of the study, and in the writing the original draft of
the manuscript. MMiyauchi and ME were involved in the study
methodology. KI and KN were involved in the study methodology, and
supervised the study. MMinami and ME confirm the authenticity of
all the raw data. All authors (MMinami, MMiyauchi, ME, AK, HF, SA,
TK, KI, NS and KN) were involved in the interpretation of and in
reporting the findings of the study. All authors were involved in
the conceptualization of the study, contributed to, and have read
and approved the final version of the manuscript.
Ethics approval and consent to
participate
An opt-out recruitment was adopted to obtain consent
in the present study on the Kochi-Iryo-Net's website. There was no
objection from participants to use or provide the required
information. This study was approved by the Ethical Review
Committee of Kochi University School of Medicine in 2020 (no.
2020-116). The present study was approved by and complied with the
Ethical Guidelines for Medical and Biological Research Involving
Human Subjects of the Ministry of Education, Culture, Sports,
Science and Technology; Ministry of Health, Labour and Welfare;
Ministry of Economy, Trade and Industry, and the Declaration of
Helsinki (2013 amendment).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ayittey FK, Dhar BK, Anani G and Chiwero
NB: Gendered burdens and impacts of SARS-CoV-2: A review. Health
Care Women Int. 41:1210–1225. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Okuyama J, Seto S, Fukuda Y, Funakoshi S,
Amae S, Onobe J, Izumi S, Ito K and Imamura F: Mental health and
physical activity among children and adolescents during the
COVID-19 pandemic. Tohoku J Exp Med. 253:203–215. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Backhaus I, Hoven H, Di Tecco C, Iavicoli
S, Conte A and Dragano N: Economic change and population health:
Lessons learnt from an umbrella review on the Great Recession. BMJ
Open. 12(e060710)2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Bou-Karroum L, Khabsa J, Jabbour M, Hilal
N, Haidar Z, Abi Khalil P, Khalek RA, Assaf J, Honein-AbouHaidar G,
Samra CA, et al: Public health effects of travel-related policies
on the COVID-19 pandemic: A mixed-methods systematic review. J
Infect. 83:413–423. 2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Onyeaka H, Anumudu CK, Al-Sharify ZT,
Egele-Godswill E and Mbaegbu P: COVID-19 pandemic: A review of the
global lockdown and its far-reaching effects. Sci Prog.
104(368504211019854)2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kayastha SR, Parajuli B, Basi A and
Shrestha D: Orthopaedic services during nationwide COVID-19
lockdown: Dhulikhel Hospital, Kathmandu University hospital
experience and review of literature. Kathmandu Univ Med J (KUMJ).
18:29–35. 2020.PubMed/NCBI
|
|
7
|
Sutherland M, McKenney M and Elkbuli A:
Vehicle related injury patterns during the COVID-19 pandemic: What
has changed? Am J Emerg Med. 38:1710–1714. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Almeida M, Shrestha AD, Stojanac D and
Miller LJ: The impact of the COVID-19 pandemic on women's mental
health. Arch Womens Ment Health. 23:741–748. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Dubey S, Biswas P, Ghosh R, Chatterjee S,
Dubey MJ, Chatterjee S, Lahiri D and Lavie CJ: Psychosocial impact
of COVID-19. Diabetes Metab Syndr. 14:779–788. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Irwin M, Lazarevic B, Soled D and Adesman
A: The COVID-19 pandemic and its potential enduring impact on
children. Curr Opin Pediatr. 34:107–115. 2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Golinelli D, Campinoti F, Sanmarchi F,
Rosa S, Beleffi M, Farina G, Tampieri A, Fantini MP, Giostra F and
Santi L: Patterns of emergency department visits for acute and
chronic diseases during the two pandemic waves in Italy. Am J Emerg
Med. 50:22–26. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Reschen ME, Bowen J, Novak A, Giles M,
Singh S, Lasserson D and O'Callaghan CA: Impact of the COVID-19
pandemic on emergency department attendances and acute medical
admissions. BMC Emerg Med. 21(143)2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ageta K, Naito H, Yorifuji T, Obara T,
Nojima T, Yamada T, Tsukahara K, Yakushiji H and Nakao A: Delay in
emergency medical service transportation responsiveness during the
COVID-19 pandemic in a minimally affected region. Acta Med Okayama.
74:513–520. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Katayama Y, Kiyohara K, Kitamura T,
Hayashida S and Shimazu T: Influence of the COVID-19 pandemic on an
emergency medical service system: A population-based, descriptive
study in Osaka, Japan. Acute Med Surg. 7(e534)2020.PubMed/NCBI View
Article : Google Scholar
|
|
15
|
Belyayeva M and Jeong JM: Acute
pyelonephritis. In: StatPearls. StatPearls Publishing, Treasure
Island, FL, 2021.
|
|
16
|
Boissier R, Savoie PH and Long JA:
Epidemiology of urological emergencies in France. Prog Urol.
31:945–955. 2021.PubMed/NCBI View Article : Google Scholar : (In French).
|
|
17
|
Al Maqbali M, Al Badi K, Al Sinani M,
Madkhali N and Dickens GL: Clinical features of COVID-19 patients
in the first year of pandemic: A systematic review and
meta-analysis. Biol Res Nurs. 24:172–185. 2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kim HS, Jang TC, Kim GM, Lee SH, Ko SH and
Seo YW: Impact of the coronavirus disease 2019 outbreak on the
transportation of patients requiring emergency care. Medicine
(Baltimore). 99(e23446)2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
van de Pol AC, Boeijen JA, Venekamp RP,
Platteel T, Damoiseaux RAMJ, Kortekaas MF and van der Velden AW:
Impact of the COVID-19 pandemic on antibiotic prescribing for
common infections in the netherlands: A primary care-based
observational cohort study. Antibiotics (Basel).
10(196)2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Cacciamani GE, Shah M, Yip W, Abreu A,
Park D and Fuchs G: Impact of Covid-19 on the urology service in
United States: Perspectives and strategies to face a pandemic. Int
Braz J Urol. 46 (Suppl 1):S207–S214. 2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Feng D, Liu S, Bai Y, Tang Y, Han P and
Wei W: Management of urology during COVID-19 pandemic: A
perspective from Sichuan Province, China. Int J Surg. 81:115–121.
2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Castellani D, Ragonese M, Di Rosa M,
Marzio V, Di Gianfrancesco L, Bassi P, De Dominicis M, Dellabella M
and Antonucci M: An Italian multicenter analysis of emergency
admissions and treatment of upper tract urolithiasis during the
lockdown and reopening phases of the COVID-19 pandemic: Are we
ready for a second wave of the outbreak? Int J Urol. 28:950–954.
2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Georgiou M, Ridzuan-Allen A, Chamsin A,
Siddiqui Z, Tolofari S, Ejikeme C, Jones R, Napier-Hemy TP, Rotas
S, Hughes KE, et al: Emergency urology procedures during the
COVID-19 pandemic in the UK: A 3-month prospective study. Urologia.
90:407–414. 2023.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Rajwa P, Przydacz M, Krajewski W, Kuffel
B, Zapala P, Krzywon A, Cortez AJ, Dybowski B, Stamirowski R,
Jarzemski M, et al: Changing patterns of urologic emergency visits
and admissions during the COVID-19 pandemic: A retrospective,
multicenter, nationwide study. Arch Med Sci. 17:1262–1276.
2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Minami M, Kidokoro K, Eitoku M, Kawauchi
A, Miyauchi M, Suganuma N and Nishiyama K: Acute effect of the
COVID-19 pandemic on emergency transportation due to acute
alcoholic intoxication: A retrospective observational study.
Environ Health Prev Med. 26(98)2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Sako A, Yasunaga H, Matsui H, Fushimi K,
Yanai H, Gu Y and Ohmagari N: Hospitalization for urinary tract
infections in Japan, 2010-2015: A retrospective study using a
national inpatient database. BMC Infect Dis.
21(1048)2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Hanaki N, Yamashita K, Kunisawa S and
Imanaka Y: Effect of the number of request calls on the time from
call to hospital arrival: A cross-sectional study of an ambulance
record database in Nara prefecture, Japan. BMJ Open.
6(e012194)2016.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Lawn S, Roberts L, Willis E, Couzner L,
Mohammadi L and Goble E: The effects of emergency medical service
work on the psychological, physical, and social well-being of
ambulance personnel: A systematic review of qualitative research.
BMC Psychiatry. 20(348)2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Colnaric J, Bachir R and El Sayed M:
Association between mode of transportation and outcomes in
penetrating trauma across different prehospital time intervals: A
matched cohort study. J Emerg Med. 60:460–470. 2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Li C, Sotomayor-Castillo C, Nahidi S,
Kuznetsov S, Considine J, Curtis K, Fry M, Morgan D, Walker T,
Burgess A, et al: Emergency clinicians' knowledge, preparedness and
experiences of managing COVID-19 during the 2020 global pandemic in
Australian healthcare settings. Australas Emerg Care. 24:186–196.
2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Jefferson T, Del Mar CB, Dooley L, Ferroni
E, Al-Ansary LA, Bawazeer GA, van Driel ML, Jones MA, Thorning S,
Beller EM, et al: Physical interventions to interrupt or reduce the
spread of respiratory viruses. Cochrane Database Syst Rev.
11(CD006207)2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Kamble P, Daulatabad V, John N and John J:
Synopsis of symptoms of COVID-19 during second wave of the pandemic
in India. Horm Mol Biol Clin Investig. 43:97–104. 2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Ding FM, Feng Y, Han L, Zhou Y, Ji Y, Hao
HJ, Xue YS, Yin DN, Xu ZC, Luo S, et al: Early fever is associated
with clinical outcomes in patients with coronavirus disease. Front
Public Health. 9(712190)2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Caminiti C, Maglietta G, Meschi T,
Ticinesi A, Silva M and Sverzellati N: Effects of the COVID-19
epidemic on hospital admissions for non-communicable diseases in a
Large Italian university hospital: A descriptive case-series study.
J Clin Med. 10(880)2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Castoldi L, Solbiati M, Costantino G and
Casiraghi E: Variations in volume of emergency surgeries and
emergency department access at a third level hospital in Milan,
Lombardy, during the COVID-19 outbreak. BMC Emerg Med.
21(59)2021.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Ansari Jafari A, Javanmard B, Rahavian A,
Rafiezadeh AR, Borumandnia N, Hojjati SA, Hosseininia SM and Karami
H: Impact of COVID-19 pandemic on emergency department referrals
with urologic complaints; a retrospective cross-sectional study.
Arch Acad Emerg Med. 10(e37)2022.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Flamm A, Lee A and Mencl F: COVID-19: A
comprehensive analysis of the pandemic's effect on an emergency
department. Disaster Med Public Health Prep. 8:1–4. 2021.PubMed/NCBI View Article : Google Scholar : (Epub ahead of
print).
|
|
38
|
Frumer M, Aharony SM, Shoshany O, Kedar D,
Baniel J and Golan S: Trends in urological emergencies in the Era
of COVID-19. Int Braz J Urol. 47:997–1005. 2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Jarvis S, Salottolo K, Berg GM, Carrick M,
Caiafa R, Hamilton D, Banton K, Lieser M and Bar-Or D: Examining
emergency medical services' prehospital transport times for trauma
patients during COVID-19. Am J Emerg Med. 44:33–37. 2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Nakao S, Masui J, Katayama Y, Kitamura T
and Matsuoka T: Impact of coronavirus disease 2019 on the mortality
of patients who received emergency transportation: A
population-based cross-sectional study. Acute Med Surg.
10(e813)2023.PubMed/NCBI View
Article : Google Scholar
|
|
41
|
Clemente-Suárez VJ, Navarro-Jiménez E,
Simón-Sanjurjo JA, Beltran-Velasco AI, Laborde-Cárdenas CC,
Benitez-Agudelo JC, Bustamante-Sánchez Á and Tornero-Aguilera JF:
Mis-Dis information in COVID-19 health crisis: A narrative review.
Int J Environ Res Public Health. 19(5321)2022.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Theberath M, Bauer D, Chen W, Salinas M,
Mohabbat AB, Yang J, Chon TY, Bauer BA and Wahner-Roedler DL:
Effects of COVID-19 pandemic on mental health of children and
adolescents: A systematic review of survey studies. SAGE Open Med.
10(20503121221086712)2022.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Na L, Yang L, Mezo PG and Liu R: Age
disparities in mental health during the COVID19 pandemic: The roles
of resilience and coping. Soc Sci Med. 305(115031)2022.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Honda C, Sumikawa Y, Yoshioka-Maeda K,
Iwasaki-Motegi R and Yamamoto-Mitani N: Confusions and responses of
managerial public health nurses during the COVID-19 pandemic in
Japan. Public Health Nurs. 39:161–169. 2022.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Kagiyama N, Komatsu T, Nishikawa M, Hiki
M, Kobayashi M, Matsuzawa W, Daida H, Minamino T, Naito T, Sugita
M, et al: Impact of a telemedicine system on work burden and mental
health of healthcare providers working with COVID-19: A multicenter
pre-post prospective stu. JAMIA Open. 5(ooac037)2022.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Riera R, Bagattini ÂM, Pacheco RL, Pachito
DV, Roitberg F and Ilbawi A: Delays and disruptions in cancer
health care due to COVID-19 pandemic: Systematic review. JCO Glob
Oncol. 7:311–323. 2021.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Kriegmair MC, Speck T, Schneider AW,
Volkmer B and Michel MS: Urological care in practices and clinics
during the corona virus pandemic in Germany. Urologe A. 60:318–330.
2021.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
48
|
Dopfer C, Wetzke M, Zychlinsky Scharff A,
Mueller F, Dressler F, Baumann U, Sasse M, Hansen G, Jablonka A and
Happle C: COVID-19 related reduction in pediatric emergency
healthcare utilization-a concerning trend. BMC Pediatr.
20(427)2020.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Kostopoulou E, Gkentzi D, Papasotiriou M,
Fouzas S, Tagalaki A, Varvarigou A and Dimitriou G: The impact of
COVID-19 on paediatric emergency department visits. A one-year
retrospective study. Pediatr Res. 91:1257–1262. 2022.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Müller F, Hummers E, Jablonka A, Schmidt T
and Noack EM: Impact of the COVID-19 lockdown on emergency medical
service operations. Notf Rett Med. 25:341–347. 2022.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
51
|
Yamamoto A, Kuriyama A and Ikegami T:
Validity of a five-level prehospital triage system in Japan: A
cohort study. Am J Emerg Med. 45:329–334. 2021.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Sekine I, Uojima H, Koyama H, Kamio T,
Sato M, Yamamoto T, Fukaguchi K, Fukui H and Yamagami H: Impact of
non-pharmaceutical interventions for the COVID-19 pandemic on
emergency department patient trends in Japan: A retrospective
analysis. Acute Med Surg. 7(e603)2020.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Kochi Prefecture new coronavirus
infectious disease notification. https://www.pref.kochi.lg.jp/soshiki/131301/2020021900446.html.
Accessed February 13.
|
|
54
|
The Current State of Medical Care in Kochi
Prefecture and Future Responses, 2024. Retrieved February 24,.
2024, from https://www.mhlw.go.jp/file/05-Shingikai-12401000-Hokenkyoku-Soumuka/0000096877.pdf.
|