Introduction
Playing a sport can provide benefits, such as an
improvement in physical and mental health. It not only helps in
stress reduction, but also inculcates teamwork and communication
skills. However, sports-related injuries are a global health
concern. For instance, the wrist or hand (28%) are the most common
sites of injury in children aged 5 to 18 years, followed by the
head or face (22%) and the ankle or foot (18%) (1). Orofacial injuries can occur in
athletes who engage in fast-paced sports involving close contact
with their body, with dental injuries being the commonest of such
injuries (2). Of note, one out of
five of these traumatic dental injuries are sustained to the
permanent teeth. These incidents can have profound consequences on
the social and psychological well-being of the patient (3). Maxillary anterior teeth, followed by
mandibular anterior teeth are more frequently injured compared with
posterior teeth. Individuals with class II division I malocclusion,
increased overjet and incompetent lips are more prone to trauma
(4). Dental fractures can be
classified based on the fracture level and pulpal involvement, as
enamel infractions, uncomplicated crown fractures (fractures of
enamel-dentin not involving pulp), complicated crown fractures
(fractures of enamel-dentin with pulp exposure), crown-root and
root fractures (5). The incidence
of complicated crown root fractures ranges from 2-13% and
uncomplicated crown fractures represent 28-44% of traumatised
teeth. The causes of such fractures range from contact sports to
domestic abuse, falls, fights and vehicular accidents (6). Ensuring that the form and
functionality of the tooth are restored is crucial for the success
of restorative planning. Treatment options vary from simple
composite restoration to fragment reattachment procedures (7). Restoring fractured teeth has become
more predictable owing to the advances made in material science and
in preparation techniques. Moreover, the procedure for fragment
reattachment has become streamlined owing to breakthroughs in
adhesive dentistry. The prognosis depends on the bonding of the
viable fragment and its adaptability to the rest of the tooth.
Patients have embraced fragment reattachment for its aesthetic
rehabilitation benefits, while maintaining the form, contour,
alignment, translucence, surface texture and position of the tooth.
This minimally invasive and affordable procedure provides
additional benefits, including the maintenance of proximal contact,
reduced chair time and a positive psychological response (7,8).
Preserving pulpal vitality is crucial for the
long-term prognosis of traumatised teeth. Utilising the vital pulp
therapy (VPT) interventions that are currently accessible is
therefore essential to the management of traumatised teeth. Direct
pulp capping, partial (Cvek) pulpotomy, and full pulpotomy are
interventions depending on the extent of pulp exposure (9,10).
Dental trauma-related pulp exposures typically involve less
microbiological contaminants and reduced exposure duration,
enhancing the chances of healing. A recent study reported high
success rates of VPT interventions for the treatment of traumatised
vital permanent teeth (11). The
current International Association of Dental Traumatology (IADT)
2020 guidelines advocate for partial pulpotomy or pulp capping as
the preferred line of treatment for teeth with complicated crown
fractures, with coronal fragment reattachment recommended when the
fragment is available (3).
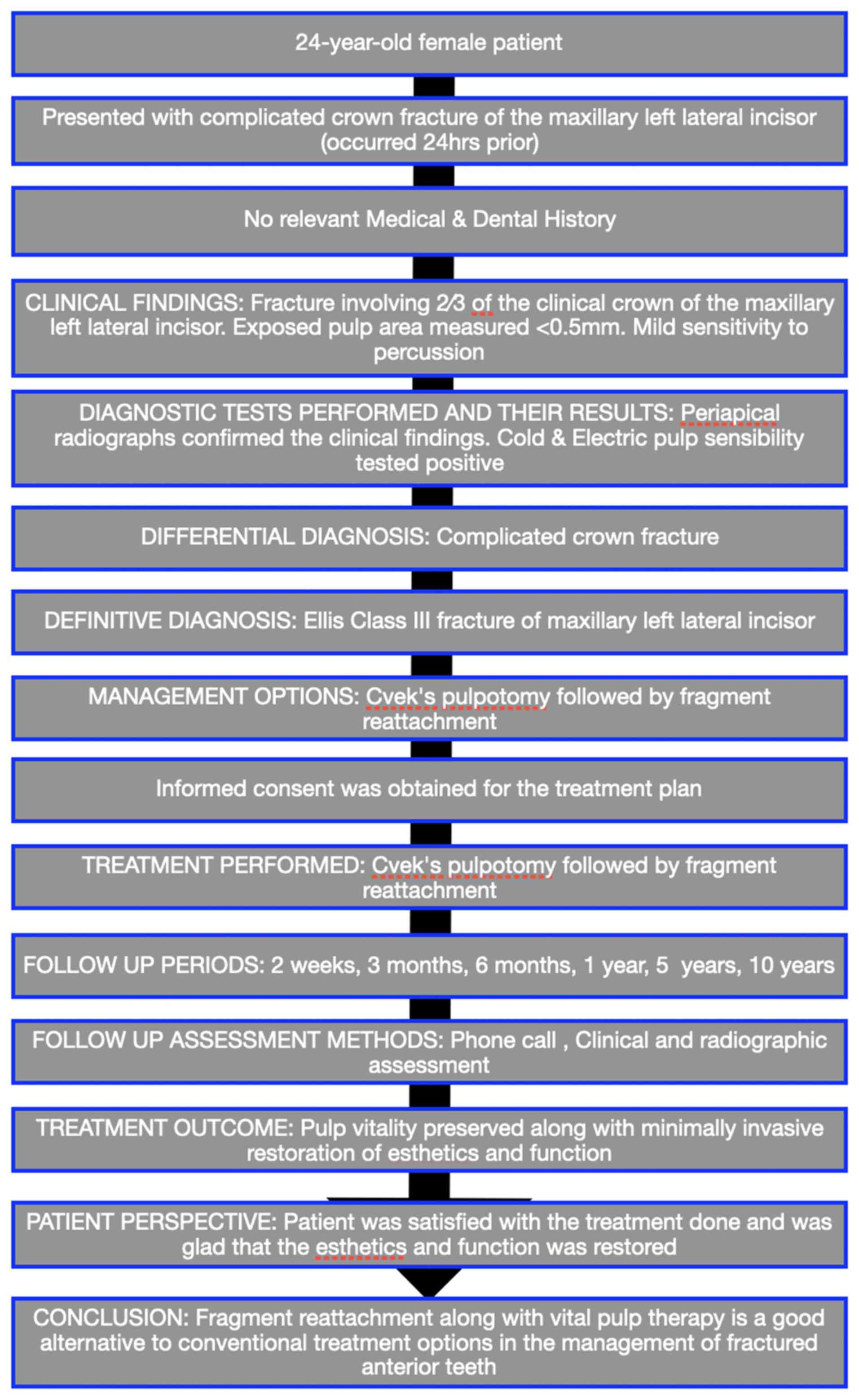
The present case report outlines a treatment for a
complicated crown fracture, focusing on biological tissue
preservation and minimal intervention principles. The management
protocol involved Cvek pulpotomy for pulp preservation and adhesive
bonding for reattaching the fracture fragment during restorative
treatment.
Case report
A 24-year-old female patient presented to the
Department of Conservative Dentistry and Endodontics, A.B Shetty
Memorial Institute of Dental Sciences (ABSMIDS), Nitte (Deemed to
be University) (Mangalore, India), with a complicated crown
fracture of the maxillary left lateral incisor that had occurred 24
h prior during sports activities. Consent for publication was
obtained from the patient. The patient did not report any relevant
medical or dental history. Extraoral assessment revealed no signs
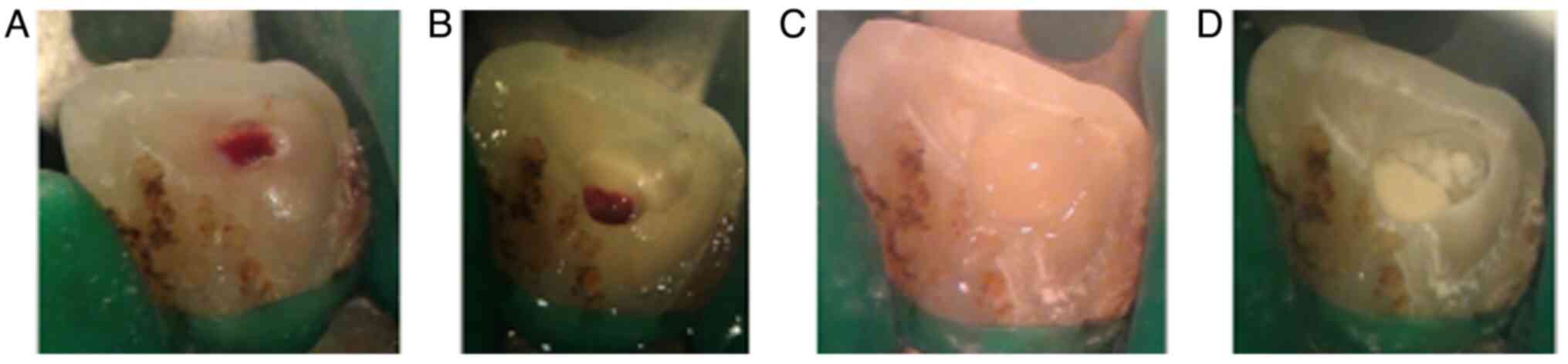
of soft tissue injury. Intraoral examination demonstrated an Ellis
class III fracture involving 2⁄3 of the clinical crown of the
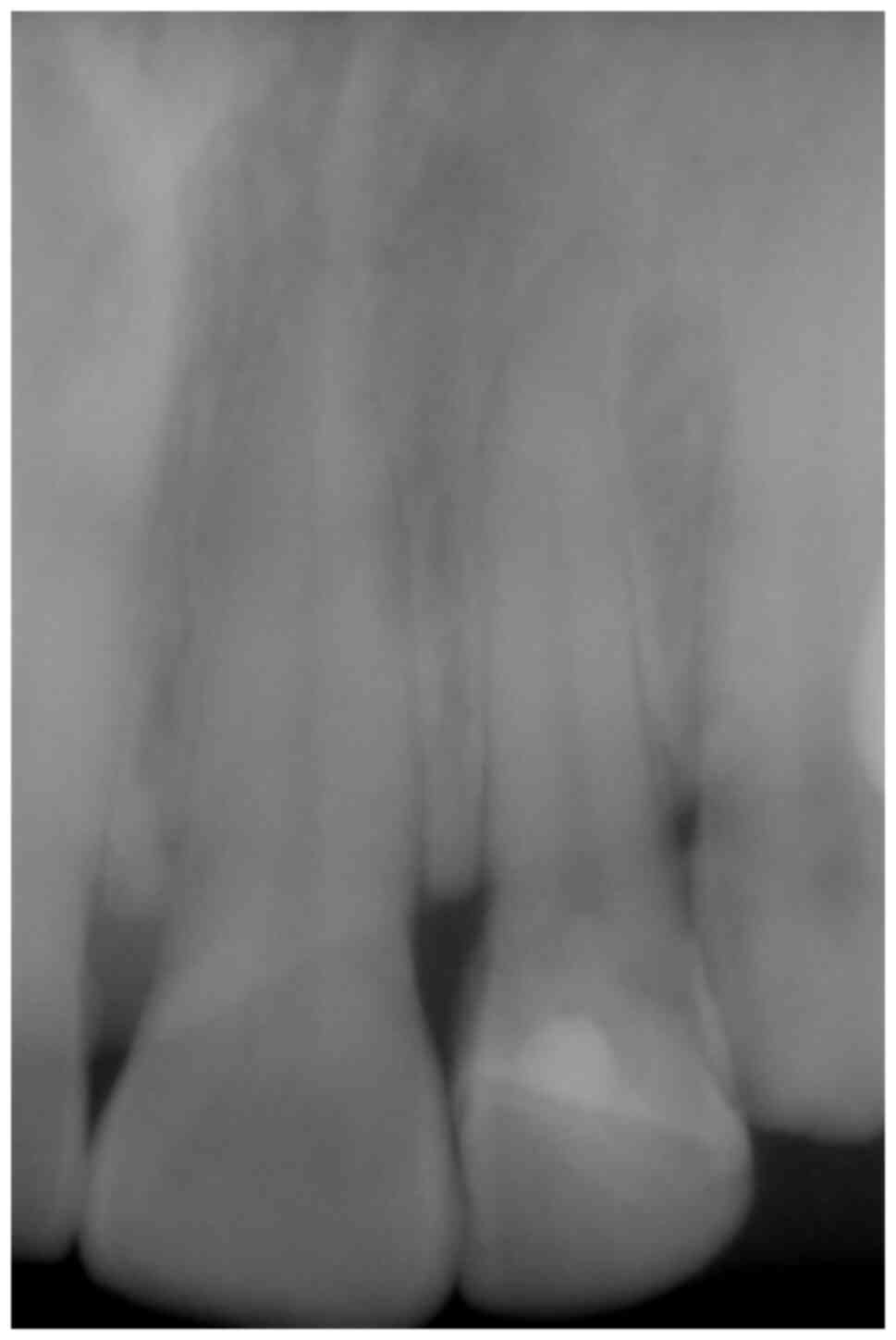
maxillary left lateral incisor (Fig.
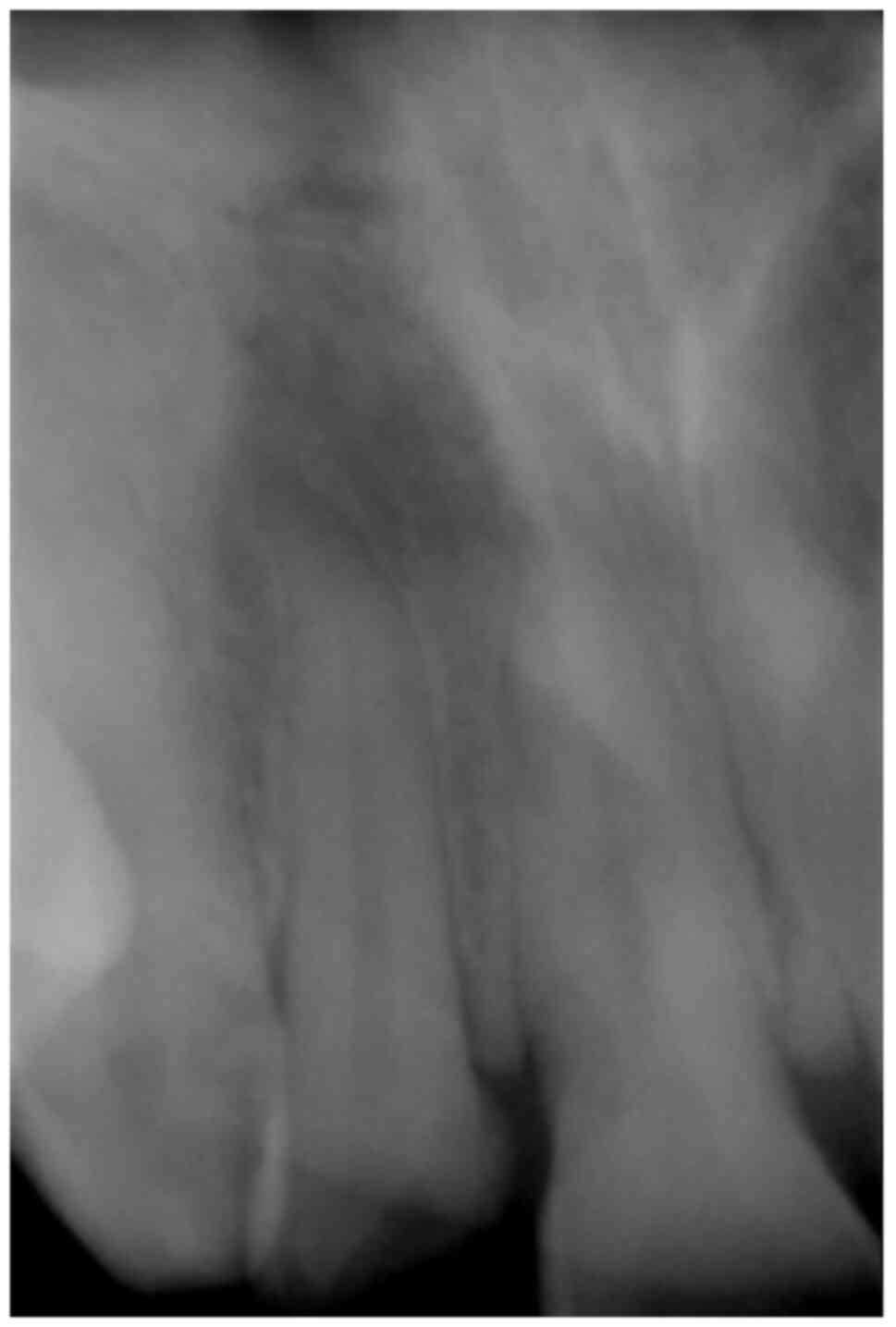
1). Periapical radiographs revealed mature apices with no
evidence of root fractures or peri-radicular injury (Fig. 2). The maxillary left central
incisor exhibited a craze line upon transillumination (Fig. 3). The exposed pulp area on the
maxillary left lateral incisor measured ~2 mm with a positive
electric pulp sensibility test, indicating reversible pulpitis. A
diagnosis of a complicated crown fracture with pulp exposure was
made. The patient reported mild symptoms, including sensitivity to
percussion (Table I).
 | Table IThe results of the diagnostic
sensibility tests of the patient. |
Table I
The results of the diagnostic
sensibility tests of the patient.
| Tooth no. | Cold | Electric pulp
tester | Percussion |
Transillumination | Mobility |
|---|
| 21 | Normal | Response | Normal | Craze line noted | Within physiological
limits |
| 22 | Normal | Response | Mild tenderness | Normal | Within physiological
limits |
| 23 | Normal | Response | Normal | Normal | Within physiological
limits |
The treatment objectives focused on preserving pulp
vitality along with the restoration of function and aesthetics. The
selected comprehensive plan incorporated the Cvek pulpotomy
(3,12) using Biodentine™
(Septodont USA) to treat the pulp and reattachment of the available
tooth fracture using resin composite. A consent form was signed by
the patient following the approval of the proposed protocol and
treatment was immediately initiated. Pre-procedural radiographs,
sensibility assessment, and try-in of fragments aided treatment
planning. The fragment was maintained in saline solution to prevent
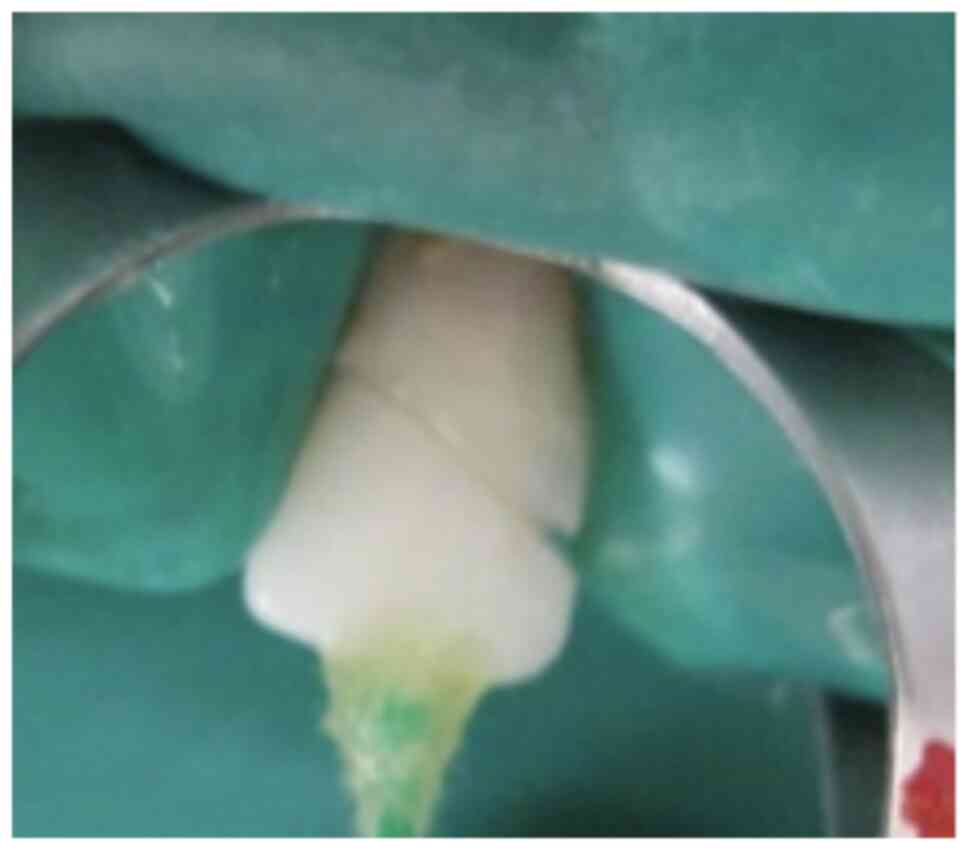
dehydration of the dentin. Following isolation under rubber dam, ~2
mm of the coronal pulp was amputated using a sterile spoon
excavator (EXC18, HuFriedyGroup) and the pulpal floor was treated
with sodium hypochlorite to arrest the bleeding.
Biodentine™ (Septodont USA) was placed followed by a
Glass ionomer cement (GlasIonomer FX Ultra, Shofu Dental India)
seal (Fig. 4). The fractured
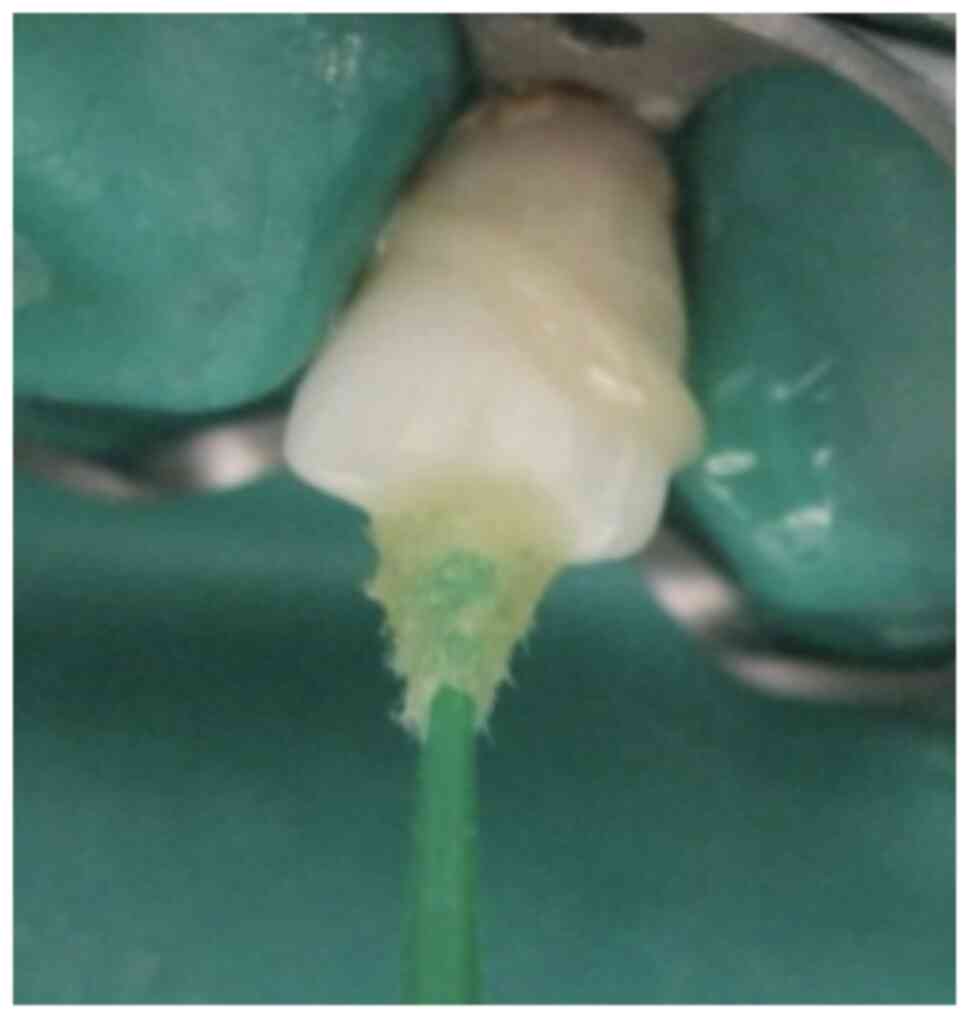
fragment was bonded to the tooth by etching with 37% phosphoric
acid gel (Prime Dental Products Pvt. Ltd.) (Fig. 5) followed by the application of
bonding agent (Adper Single Bond 2, 3M ESPE). The remaining coronal
tooth fragment was etched and bonded as well to receive the
fragment, which was reattached using flowable nanocomposite (Endure
Flow, Septodont USA) (Fig. 6,
Fig. 7 and Fig. 8). The patient was unable to attend
regular follow-ups due to distance constraints, as the patient
worked in another country. Thus, follow-ups were made via telephone
inquiries. However, the patient visited the dental clinic after 10
years for a regular check-up. At the 10-year follow-up, the
reattached fragment exhibited excellent retention with desired
aesthetics. A clinical examination revealed normal soft tissues,
tooth form/contour and crown coloration, with no signs of fracture
(Fig. 9). Periapical radiographs
at the 10-year follow-up revealed a distinct dentin bridge with
maintained pulp space with no signs of periapical radiolucency
(Fig. 10). Sensibility tests were
within normal limits. A comprehensive evaluation of adjacent
hard/soft tissues did not reveal any pathology. Clinical
photographs attested to the natural appearance of the reattached
tooth segment. Based on multiple assessments over the 10-year
period, the tooth was deemed to have a favourable prognosis
regarding continued pulp vitality and periapical health without the
need for further treatment (Table
II). The combined approach integrating adhesive techniques with
vital pulp treatment demonstrated a successful long-term outcome in
the management of a complicated crown fracture in an anterior
maxillary tooth (Fig. 11)
 | Table IIThe timeline of the case in the
present study. |
Table II
The timeline of the case in the
present study.
| Time | Event |
Diagnosis/outcome |
|---|
| 0 | Patient visited the
clinic; history, clinical and radiographic examination | Complicated crown
fracture in relation to maxillary left lateral incisor |
| 0 | Cvek pulpotomy
followed by the fragment reattachment procedure | |
| +2 weeks | 1st follow-up (Phone
inquiry) | No pain, swelling
(symptom-free), reattached fragment intact |
| +3 months | 2nd follow-up (Phone
inquiry) | No pain, swelling
(symptom-free), reattached fragment intact |
| +6 months | 3rd follow-up (Phone
inquiry) | No pain, swelling
(symptom-free), reattached fragment intact |
| +1 year | 4th follow-up (Phone
inquiry) | No pain, swelling
(symptom-free), reattached fragment intact |
| +5 year | 5th follow-up (Phone
inquiry) | No pain, swelling
(symptom-free), reattached fragment intact |
| +10 year | 6th follow-up
(clinical and radiographic assessment) | Symptom free,
electric pulp test: Positive response, reattached fragment intact
and no discolouration noted |
Discussion
Traumatic crown fractures in anterior teeth causing
pulp exposure are distressing injuries requiring prompt care,
particularly in young patients. Unlike caries exposures, traumatic
cases tend to have a better prognosis due to the lack of bacteria.
Treatment options for such pulp exposures include direct pulp
capping or partial/full pulpotomy, depending on extent of
inflammation, root development stage and vascular supply. Although
the time between injury and treatment along with exposure size can
influence outcomes, studies have demonstrated that partial
pulpotomy can be successful, despite delays if the infected pulp is
removed (13,14). Exposures >1 mm where treatment
is delayed beyond 24 h are managed more effectively with Cvek
pulpotomy involving the removal of 1-2 mm inflamed pulp until
healthy tissue is reached (12).
Partial pulpotomy preserves coronal pulp tissue with a greater
healing capacity. The remaining crown pulp can maintain physiologic
dentin formation, strengthening the tooth (9,10).
For pulp capping, calcium hydroxide has been the
preferred material due to its antibacterial alkaline pH that
supports healing and hard tissue formation. However, it requires
technique sensitivity, can be difficult to apply, and lacks
cost-effectiveness of contemporary alternatives (15). Currently, mineral trioxide
aggregate (MTA) and Biodentine are preferred over calcium hydroxide
for VPT in primary and permanent teeth (16). Although effective, an adverse
effect of MTA is potential tooth discoloration due to the
radiopacifier, bismuth oxide, in grey and white formulations.
Biodentine can also stain teeth, although seemingly less than MTA
(17).
Material selection, including the adhesive strategy
(etch type) and resin (conventional, flowable, pre-heated, etc.)
also markedly affect the success (7,8,18).
Flowable composites are suitable when adaptation and interfacial
gaps are minimal (19).
Maintaining fragment hydration is also critical, as moisture loss
reduces bond strength (20). In
the case presented herein, the reattachment was performed using a
total-etch single bottle adhesive and flowable composite owing to
excellent fracture adaptation. Storing fragments in saline
prevented dehydration and related discoloration. The decision to
perform partial pulpotomy considered the time from injury to
treatment, the age of the patient, root status and marginal fit of
fragments that assured pulp dressing retention. Hence, Biodentine
was applied as the capping agent. At the 10-year follow-up, there
was no evidence of coronal or reattachment line discolouration. The
teeth exhibited normal sensibility with no periapical pathosis
signs/symptoms indicating success.
Advances made in restorative materials, tooth
preparation designs and bonding protocols have enabled predictable
restoration of fractured teeth using various approaches tailored to
factors, such as economics, age and oral status. Proper occlusal
rehabilitation following trauma is vital for stomatognathic
function, facial symmetry, speech, swallowing and preventing
dental/skeletal discrepancies over time. Here, the own fragments of
the patient were reattached, unlike more invasive veneers or
crowns. Numerous techniques and materials to reattach fragments
exist, with some researchers promoting additional tooth preparation
to increase fracture resistance compared to bonding alone (21). However, there is evidence to
indicate that no preparation or only chamfering still retains
adequate strength (8). Ultimately,
there is no consensus on an ideal reattachment technique with
choice depending on fracture and marginal adaptation quality
(7,22).
In conclusion, as demonstrated in the case described
in the present study, fragment reattachment in conjugation with VPT
stands out as a favourable alternative to traditional treatment
approaches for the management of fractured anterior teeth. This
method is straightforward, minimally invasive, and ensures both
effective retention of the fragment and pleasing aesthetics, all
while preserving the integrity of the pulp tissue.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Data sharing is not applicable to this article as no
datasets were generated or analyzed during the current study.
Authors' contributions
PS conceptualized the study and was involved in the
clinical analysis of the patient. MP was involved in the curation
of the patient's data. RB was involved in the writing and
preparation of the original draft of the manuscript, performed the
treatment procedure, obtained medical images, as well as in the
reviewing and editing of the manuscript. All authors have reviewed,
and read and approved the final manuscript.
Ethics approval and consent to
participate
Informed consent had been obtained from the patient
following the explanation of the treatment outcomes.
Patient consent for publication
Informed consent had been obtained from the patient
for the publication of the present case report and any related
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Taylor BI and Attia MW: Sports-related
injuries in children. Acad Emerg Med. 7:1376–1382. 2000.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Emerich K and Kaczmarek J: First aid for
dental trauma caused by sports activities: State of knowledge,
treatment and prevention. Sports Med. 40:361–366. 2010.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Bourguignon C, Cohenca N, Lauridsen E,
Flores MT, O'Connell AC, Day PF, Tsilingaridis G, Abbott PV, Fouad
AF, Hicks L, et al: International association of dental
traumatology guidelines for the management of traumatic dental
injuries: 1. Fractures and luxations. Dent Traumatol. 36:314–330.
2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Jones LC: Dental trauma. Oral Maxillofac
Surg Clin North Am. 32:631–638. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
DiAngelis AJ, Andreasen JO, Ebeleseder KA,
Kenny DJ, Trope M, Sigurdsson A, Andersson L, Bourguignon C, Flores
MT, Hicks ML, et al: Guidelines for the management of traumatic
dental injuries: 1. Fractures and luxations of permanent teeth.
Pediatr Dent. 38:358–368. 2016.PubMed/NCBI
|
|
6
|
Levin L, Day PF, Hicks L, O'Connell A,
Fouad AF, Bourguignon C and Abbott PV: International association of
dental traumatology guidelines for the management of traumatic
dental injuries: General introduction. Dent Traumatol. 36:309–313.
2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Garcia FCP, Poubel DLN, Almeida JCF,
Toledo IP, Poi WR, Guerra ENS and Rezende LVML: Tooth fragment
reattachment techniques-A systematic review. Dent Traumatol.
34:135–143. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Bruschi-Alonso RC, Alonso RCB, Correr GM,
Alves MC, Lewgoy HR, Sinhoreti MAC, Puppin-Rontani RM and
Correr-Sobrinho L: Reattachment of anterior fractured teeth: Effect
of materials and techniques on impact strength. Dent Traumatol.
26:315–322. 2010.PubMed/NCBI View Article : Google Scholar
|
|
9
|
European Society of Endodontology (ESE)
developed by. Duncan HF, Galler KM, Tomson PL, Simon S, El-Karim I,
Kundzina R, Krastl G, Dammaschke T, Fransson H, et al: European
society of endodontology position statement: Management of deep
caries and the exposed pulp. Int Endod J. 52:923–934.
2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Duncan HF: Present status and future
directions-vital pulp treatment and pulp preservation strategies.
Int Endod J. 55 (Suppl 3):S497–S511. 2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Krastl G, Weiger R, Ebeleseder K and
Galler K: Present status and future directions: Endodontic
management of traumatic injuries to permanent teeth. Int Endod J.
55 (Suppl 4):S1003–S1019. 2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Bimstein E and Rotstein I: Cvek
pulpotomy-revisited. Dent Traumatol. 32:438–442. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Matoug-Elwerfelli M, ElSheshtawy AS,
Duggal M, Tong HJ and Nazzal H: Vital pulp treatment for
traumatized permanent teeth: A systematic review. Int Endod J.
55:613–629. 2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Qudeimat MA, Alyahya A and Hasan AA:
Mineral trioxide aggregate pulpotomy for permanent molars with
clinical signs indicative of irreversible pulpitis: A preliminary
study. Int Endod J. 50:126–134. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Mohammadi Z and Dummer PMH: Properties and
applications of calcium hydroxide in endodontics and dental
traumatology. Int Endod J. 44:697–730. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Parirokh M, Torabinejad M and Dummer PMH:
Mineral trioxide aggregate and other bioactive endodontic cements:
An updated overview-part I: Vital pulp therapy. Int Endod J.
51:177–205. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Pednekar A, Ataide I, Fernandes M, Lambor
R and Soares R: Spectrophotometric analysis of coronal
discolouration induced by ProRoot MTA, biodentine and MTA repair HP
used for pulpotomy procedures. Eur Endod J. 6:189–196.
2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Pereira RV, Tabata LF, Rosemberg ET,
Ribeiro APD, Poubel DLDN and Garcia FCP: Fragment reattachment or
direct restoration? An in vitro study. Dent Traumatol. 39:257–263.
2023.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Farik B, Munksgaard EC, Andreasen JO and
Kreiborg S: Fractured teeth bonded with dentin adhesives with and
without unfilled resin. Dent Traumatol. 18:66–69. 2002.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Madhubala A, Tewari N, Mathur VP and
Bansal K: Comparative evaluation of fracture resistance using two
rehydration protocols for fragment reattachment in uncomplicated
crown fractures. Dent Traumatol. 35:199–203. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Stellini E, Stomaci D, Stomaci M, Petrone
N and Favero L: Fracture strength of tooth fragment reattachments
with postpone bevel and overcontour reconstruction. Dent Traumatol.
24:283–288. 2008.PubMed/NCBI View Article : Google Scholar
|
|
22
|
de Sousa APBR, França K, de Lucas Rezende
LVM, do Nascimento Poubel DL, Almeida JCF, de Toledo IP and Garcia
FCP: In vitro tooth reattachment techniques: A systematic review.
Dent Traumatol. 34:297–310. 2018.PubMed/NCBI View Article : Google Scholar
|