Introduction
Autism spectrum disorder (ASD) refers to
neurodevelopmental disorders marked by significant challenges in
socialization, communication and behavior (1). A previous systematic review of 71
studies included sample sizes which were relatively large, ranging
from 465 to 50 million participants. Prevalence in these studies
ranged from 1.09/10,000 to 436/10,000, with a median majority of
100/10,000(2). Notably, the
reported prevalence of ASD among children has increased over time.
This may be attributable to several factors, including a broadening
of the diagnostic criteria, heightened public awareness of ASD and
its symptoms, and the enhanced availability of early interventions
and educational services tailored for children with ASD (3).
Sociodemographic factors, such as socio-economic
status, parental education and cultural background significantly
affect the development, diagnosis and management of ASD in
children. Studies from Australia and Bangladesh have highlighted
how parental education, occupation and cultural background
influence ASD diagnoses and access to services, emphasizing the
need for equitable healthcare policies and intervention programs
tailored to diverse needs (4,5).
Understanding these factors is essential for ensuring access to
support services for all children with ASD, regardless of
sociodemographic background.
Medical comorbidities are more common in children
with ASD than in the general population. For instance, children
with ASD are more likely to develop various neurological disorders,
including epilepsy, macrocephaly, migraines/headaches and
congenital abnormalities of the nervous system (6). Additionally, the risk of falls is
strongly prevalent in such children. This may be due to cognitive
and motor impairments that increase the risk of falls. The high
rate of non-fatal falls, the associated healthcare costs and the
significant risk of mortality (particularly as a result of head
injuries) render it essential to prioritize the prevention of
fall-related injuries in child safety efforts worldwide (7).
Numerous risk and protective factors for falls among
children have been reported, including sociodemographic
characteristics, maternal psychiatric disorders, and child
psychological and behavioral issues (8). A previous study employing
multivariate logistic regression analyzes identified significant
predictors of falls, such as an age <3 years, neurological
diagnosis (including epilepsy), dependency in activities of daily
living, physical developmental delay and multiple usage of
fall-risk-increasing drugs (9).
Antipsychotic medications are the agents most critically studied as
treatments for reducing symptoms. However, such medications can
increase the risk of falls due to syncope, sedation, slowed
reflexes, loss of balance and impaired psychomotor function
(9). Moreover, the administration
of antipsychotic medications requires careful monitoring due to
associated safety concerns and the potential for extended
utilization (10).
Interventions in general predominantly focus on
reducing ASD-specific symptoms, mitigating concurrent issues, and
enhancing overall quality of life (11). Notably, early interventions
demonstrate considerable efficacy, significantly improving outcomes
across domains (12). In Saudi
Arabia, children begin treatment at 3.3 years of age, whereas in
the USA, treatment is commenced at 2.2 years of age, indicating
delayed intervention in Saudi Arabia. Utilizing an online survey
methodology with a sample size of ~200 participants, a study
conducted >6 years prior highlighted the need for a
comprehensive investigation into the prevalence of ASD and related
services within the Saudi community (13).
This underscores the necessity of identifying and
implementing suitable interventions tailored to children with ASD
from different age groups, thus ensuring timely and effective
support mechanisms. In Saudi Arabia, to the best of our knowledge,
no study has yet evaluated the pediatric risk of falls among
children with ASD. To fill this gap in the research literature, the
present study examined the ASD profile through an analysis of
sociodemographic variables, the type of medications children with
ASD receive, and the presence of comorbidities. The present study
also conducted a correlational analysis to evaluate the risk of
falls among different age groups.
Patients and methods
Study participants
The sample size was determined using G*Power
software (http://www.gpower.hhu.de/). A priori
power analysis for a two-tailed correlation indicated that the
minimum sample size needed to yield a statistical power of 0.95
with an α value of 0.05 and a medium effect size (Cohen's d=0.5) is
134. For an independent samples Student's t-test, a minimal sample
size of 210 is required. Furthermore, a minimum of 172 participants
are required for a linear regression model with 10 predictor
variables, while 66 participants are required for a repeated
measures analysis of variance (ANOVA). The sample for the present
study comprised 250 autistic children attending the Psychology
Clinic at King Khalid University Hospital (KSUM) in Riyadh, Saudi
Arabia. This hospital operates under King Saud University.
Therefore, the sample size was appropriate. The sample included
children diagnosed with ASD from January, 2015 to the end of
October, 2023. All the children had received multidisciplinary
evaluations, including diagnostic, cognitive and behavioral
assessments.
Study design and procedure
A retrospective cohort study was designed using a
healthcare digital record system known as electronic medical record
(EMR) systems to collect the data from KSUM. Ethical approval for
the study was granted by the Institutional Review Board at King
Saud University in Riyadh, Saudi Arabia (Ref. E-22-7451 no.
23/0175/IRB), with an issue date of March 2, 2023. The ethics
committee granted a waiver of written informed consent.
Measurements and patient
demographics
The demographic variables collected from EMR systems
included geographical regions of Saudi Arabia (Riyadh and other
regions), current age categories in three groups: Early (3-6
years), middle (7-12 years) and late (13-17 years), age at first
diagnosis, body mass index (BMI), sex (female or male), education
(public school with/without mixed classes, disability/ASD center,
others) and parents' knowledge of ASD.
Statistical analysis
The descriptive statistics included frequencies and
percentages of survey responses for categorical variables, as well
as the mean (M) and standard deviation (SD) values for continuous
data. Spearman's (RS) correlation analyses were
performed to examine the correlation between age and the number of
medications the participants received. As a sensitivity analysis, a
repeated measures analysis of variance (ANOVA) was conducted to
examine whether the number of antipsychotic and non-antipsychotic
medications taken (repeated measurement) was dependent on the
participants' age (early, middle or late childhood). The current
medications reported in the study are depicted in Data S1. In addition, supplementary the
categorization of diseases reported in children with autism is
demonstrated in Table SI and
Data S2. The effect size was
assessed using partial eta-square (η2p),
while a Bonferroni post hoc test was performed to evaluate
significant differences between particular samples.
The total study sample was divided into two groups
in terms of risk of falls, using the cut score of 12 on the Humpty
Dumpty Falls Scale (HDFS). The group with a lower risk of falls
(HDFS <12) included 176 children with ASD, whereas the group
with a higher risk of falls (HDFS ≥12) comprised 74 children with
ASD. These two groups were then compared using a Mann-Whitney U
test. The following dependent variables (considered as continuous
or ordinal data) were examined: Age at first diagnosis, current
age, BMI, number of diagnoses, number of comorbidities and number
of medications taken per person, including the number of
antipsychotics, non-antipsychotics and vitamins. Rank biserial
correlation (RBC) was performed to assess the effect size for the
Mann-Whitney U test. In addition, the total sample was divided into
three groups according to age stages during childhood: Early
(children between 3 and 6 years of age), middle (children between 7
and 12 years of age) and late (adolescents between 13 and 17 years
of age). As a sensitivity analysis, Pearson's χ2 test of
independence or Fisher's exact test were then conducted to examine
associations between pediatric risk of falls (lower vs. higher) and
the categorical variables of age, sex, education status, region of
Saudi Arabia, and parent's self-reported knowledge of ASD (answered
as either yes or no). The Phi (φ) statistic was used to assess the
effect size for bi-categorical variables (i.e., sex, region, and
knowledge), while Cramer's V was used to determine the effect size
for multi-categorical variables (i.e., age and education status) in
the χ2 test.
Finally, the contribution of demographic variables
to the risk of falls among children with ASD was examined using
linear regression. The following predictor variables were included
in the regression model: Age at first diagnosis, current age, BMI,
sex, education status, parents' knowledge about ASD, number of
diagnoses, number of comorbidities, number of antipsychotics,
non-antipsychotics and vitamins taken. Tolerance was >0.25
(ranging from 0.48 to 0.97) and the variance inflation factor (VIF)
was <3 (ranging from 1.03 to 2.19), suggesting that
multicollinearity was not an issue in the multiple regression
model. All statistical analyses were performed using JASP version
0.18.3.0 software for Windows (https://jasp-stats.org). A value of P<0.05 was
considered to indicate a statistically significant difference.
Results
Characteristics of the study
sample
The demographic characteristics of the study
participants are presented in Table
I. The mean age of first ASD diagnosis was seven years, whereas
the mean current age of participants was twelve years. In terms of
sex differences, the majority of the participants were male (74.4%)
and the remainder (25.6%) were female. The average BMI was 19. The
majority of the patients with ASD were males, had attended some
schools or rehabilitation centers and resided in Riyadh. In the
majority of the families, both parents took care of the children,
and the majority of parents had knowledge about ASD. The majority
of the children had been diagnosed with ASD, and were usually
diagnosed once. Almost 39% of the children had another health
condition, usually took one medication, and often did not take any
vitamins. The study sample was divided according to the HDFS. The
group with low pediatric risk of falls (HDFS scores <12)
prevailed over those who met the criteria for a high risk of falls
(HDFS scores ≥12).
 | Table ICharacteristic of the study
participants (n=250). |
Table I
Characteristic of the study
participants (n=250).
| Variable | Range/code | M/n | SD/% |
|---|
| Age at first
diagnosis | 0-15 | 7.27 | 3.4 |
| Current age | 3-22 | 11.65 | 3.85 |
|
Early
(3-6) | 0 | 30 | 12 |
|
Middle
(7-12) | 1 | 114 | 45.6 |
|
Late
(13-17) | 2 | 106 | 42.4 |
| Body mass index
(BMI) | 8.33-42.58 | 18.56 | 5.57 |
| Sex | 0-1 | 0.75 | 0.44 |
|
Female | 0 | 64 | 25.6 |
|
Male | 1 | 186 | 74.4 |
| Education
statusa | 0-1 | 0.57 | 0.5 |
|
Public
school with/without mixed classes | 1 | 71 | 28.4 |
|
Disability
and autism center | 2 | 67 | 26.8 |
|
Other | 3 | 4 | 1.6 |
|
Not
mentioned | 4 | 108 | 43.2 |
| Region of Saudi
Arabia | | | |
|
Riyadh | 0 | 181 | 72.4 |
|
Other
regions | 1 | 69 | 27.6 |
| Parents' knowledge
about autism | 0-1 | 0.28 | 0.45 |
|
Yes | 0 | 180 | 72 |
|
No | 1 | 70 | 28 |
| Current
diagnosis | | | |
|
Atypical
autism | 7 | 2.8 | |
|
Childhood
autism | 39 | 15.6 | |
|
Autism | 204 | 81.6 | |
| No. of
diagnoses | 1-3 | 1.22 | 0.45 |
|
One | 1 | 199 | 79.6 |
|
Two | 2 | 47 | 18.8 |
|
Three | 3 | 4 | 1.6 |
| No. of
comorbidities | 0-3 | 1.29 | 1 |
|
No | 0 | 59 | 23.6 |
|
One | 1 | 97 | 38.8 |
|
Two | 2 | 55 | 22.0 |
|
Three | 3 | 39 | 15.6 |
| No. of current
medications taken per person | 0-5 | 1.96 | 1.36 |
| No. of
antipsychotic drugs | 0-4 | 1.24 | 0.98 |
| No. of
non-antipsychotic drugs | 0-5 | 0.72 | 1.12 |
| No. of vitamins
taken | 0-3 | 0.64 | 0.88 |
| Humpty Dumpty Falls
Scale (HDFS) | 2-18 | 10.66 | 1.79 |
| Pediatric risk of
falls | 0-1 | 0.3 | 0.46 |
|
Low (HDFS
<12) | 0 | 176 | 70.4 |
|
High (HDFS
≥12) | 1 | 74 | 29.6 |
Prevalence and type of
comorbidity
A diagnosis of ASD was reported in 82% of the
participants, among whom childhood ASD was detected in 15.6% and
atypical ASD in 2.8%. In the study sample, the majorty of the
children with ASD (76.4%) reported a comorbidity (Table I). One additional disease (apart
from ASD) was found in 38.8% of the children, two coexisting
diseases in 22%, and three in 15.6% of the childrern (Table I). The prevalence of particular
types of coexisting diseases is presented in Table II. The most common was ADHD (46%
of the total sample), followed by intellectual disabilities
(18.4%), epilepsy (17.6%), genetic conditions (9.2%), global
developmental delay (6.4%), asthma (6.4%) and metabolic disorders
(6%). Other types of diseases were less frequent. The
categorization of particular diseases is presented in Data S2.
 | Table IIFrequency of occurrence of various
types of comorbidity in the sample (n=250). |
Table II
Frequency of occurrence of various
types of comorbidity in the sample (n=250).
| Type of
comorbidity | No. of
participants | % |
|---|
| ADHD | 115 | 46.0 |
| Anxiety
disorder | 5 | 2.0 |
| Asthma | 16 | 6.4 |
| Cardiovascular
disease | 3 | 1.2 |
| Constipation | 3 | 1.2 |
| Epilepsy | 44 | 17.6 |
| Genetic
condition | 23 | 9.2 |
| Global
developmental delay | 16 | 6.4 |
| Hematological
disease | 3 | 1.2 |
| Infection | 1 | 0.4 |
| Intellectual
disability | 46 | 18.4 |
| Metabolic
disorder | 15 | 6.0 |
| Obesity | 3 | 1.2 |
| Other neurological
diseases | 10 | 4.0 |
| Others | 15 | 6.0 |
| Respiratory
disorders | 6 | 2.4 |
Type of medications taken depending on
age
On average, the participants currently took two
medications (M=1.96, SD=1.36), the number of which ranged from 0 to
5 per child (Table I).
Specifically, the majority of children used one medication (n=102,
40.8%), followed by two medications (n=56, 22.4%), three
medications (n=34, 13.6%), four medications (n=20, 8.0%), and five
medications (n=19, 7.6%). In total, 19 children (7.6%) reported not
using any medication. The frequency with which particular types of
medications were currently taken per child is presented in Table III. Participants took more
antipsychotic medications (M=1.24, SD=0.98, range 0-4) than
non-antipsychotics (M=0.72, SD=1.12, range 0-5) and vitamins
(M=0.64, SD=0.88, range 0-3).
 | Table IIINo. of particular types of
medications taken currently per child. |
Table III
No. of particular types of
medications taken currently per child.
| | Antipsychotics |
Non-antipsychotics | Vitamins |
|---|
| No. of
medications | No. of
participants | % | No. of
participants | % | No. of
participants | % |
|---|
| 0 | 56 | 22.4 | 153 | 61.2 | 144 | 57.4 |
| 1 | 112 | 44.8 | 47 | 18.8 | 67 | 26.7 |
| 2 | 54 | 21.6 | 26 | 10.4 | 26 | 10.4 |
| 3 | 22 | 8.8 | 16 | 6.4 | 14 | 5.6 |
| 4 | 6 | 2.4 | 6 | 2.4 | | |
| 5 | | | 2 | 0.8 | | |
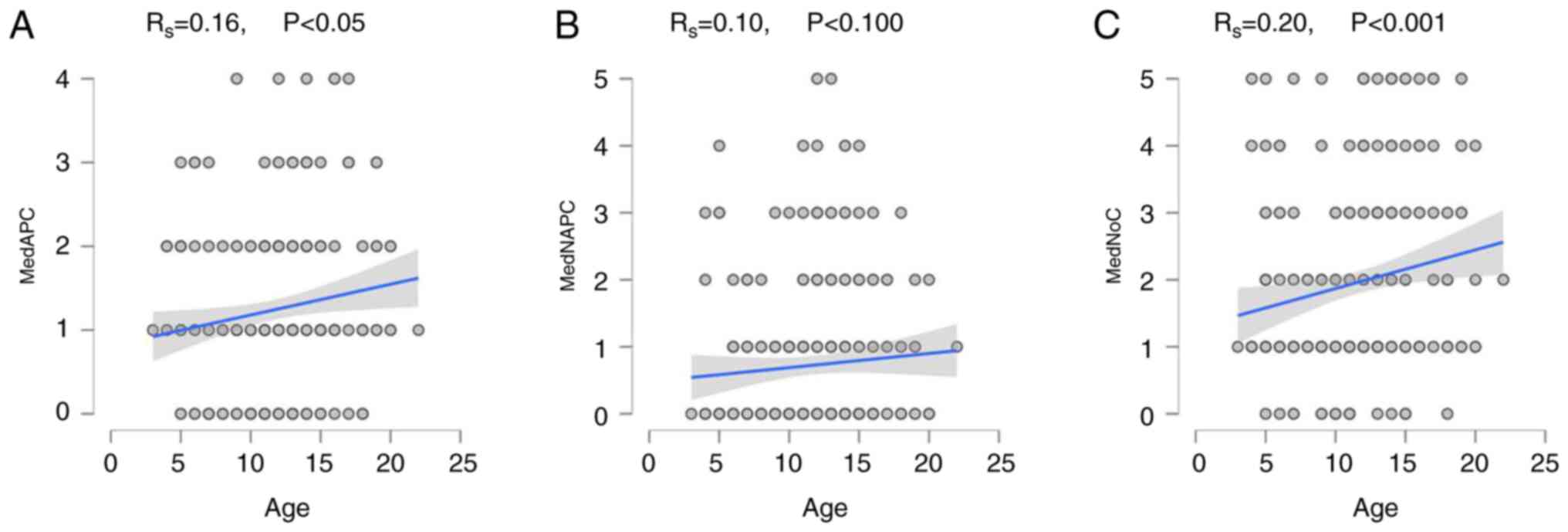
The correlation between age and the current number
of medications taken was examined using Spearman's correlation
analysis (Fig. 1). The results
revealed that the age of the children with ASD positively
correlated with the total number of medications taken
(RS=0.20, P<0.001) and antipsychotic medications used
(RS=0.16, P<0.05). Non-significant correlations were
found between age and non-antipsychotic medication use
(RS=0.10, P=0.10).
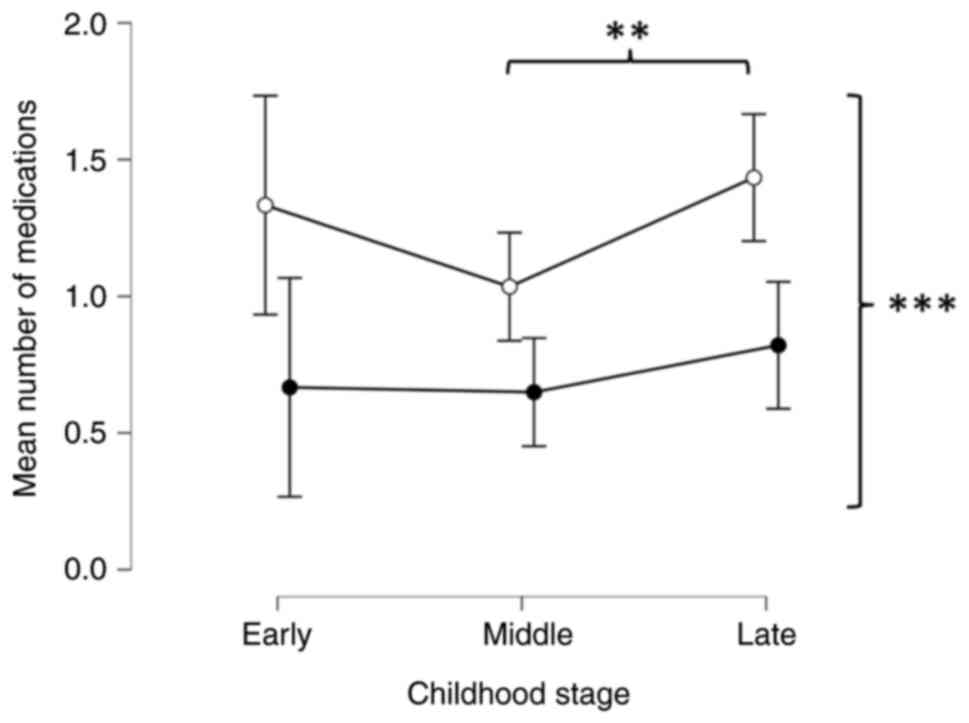
A repeated measures ANOVA was then conducted with
the type of medication (antipsychotic, non-antipsychotic) as a
dependent variable (repeated measures) and the three categories of
age during childhood (early, middle, and late) as a factor. A
significant difference was found between the mean number of
antipsychotic and non-antipsychotic medications taken
[F(1,247)=21.15, P< 0.001, η2p=0.08)]. A
Bonferroni post hoc test revealed that children with ASD used
significantly more antipsychotic medications than non-antipsychotic
(ΔM=0.56, SE=0.12, t=4.60, P<0.001). A significant effect was
also found for childhood stages [F(2,247)=4.98, P=0.008,
η2p=0.04]. A Bonferroni post hoc test
revealed that children in the middle stage took fewer medications
on average than adolescents (ΔM=-0.29, SE=0.09, t=-3.15, P=0.005).
There was no interaction effect between type of medication and age
[F(2,247)=0.71, P=493, η2p=0.01)].
Differences in the mean number of antipsychotic and
non-antipsychotic medications across ages are presented in Fig. 2.
Differences between children at high
and low risk of falls in terms of demographic variable
A Mann-Whitney U test was conducted to assess the
differences between children at lower and higher risk of falls for
the following continuous or ordinal variables: age of first
diagnosis, current age, BMI, number of diagnoses, number of
comorbidities and number of medications taken per child, including
the number of antipsychotics, non-antipsychotics, and vitamins
(Table IV). Significant
differences were found between these groups in terms of first
diagnosis and current age. In particular, participants at higher
risk of falls were diagnosed <6 years of age, whereas those at
lower risk were diagnosed at ~8 years of age. Similarly, younger
children (mean age, 10 years) had a higher risk of falls than older
children (mean age, 12 years). The differences in BMI, number of
diagnoses, comorbidity and medications taken per child were not
significant.
 | Table IVMann-Whitney U test for examining the
differences between children at a high and low risk of falls in
demographic continuous or ordinal variables. |
Table IV
Mann-Whitney U test for examining the
differences between children at a high and low risk of falls in
demographic continuous or ordinal variables.
| | Low risk
(n=176) | High risk
(n=74) | |
|---|
| Variable | M | SD | M | SD | U test | P-value | RBC |
|---|
| Age at first
diagnosis | 7.84 | 3.39 | 5.93 | 3.02 | 8632.0 |
<0.001 | 0.33 |
| Current age | 12.43 | 3.65 | 9.78 | 3.67 | 9082.5 |
<0.001 | 0.40 |
| Body mass index
(BMI) | 18.92 | 5.71 | 17.69 | 5.14 | 7359.5 | 0.071 | 0.15 |
| No. of
diagnoses | 1.24 | 0.48 | 1.16 | 0.37 | 6923.0 | 0.261 | 0.06 |
| Comorbidity | 1.33 | 1.01 | 1.22 | 0.97 | 6917.0 | 0.418 | 0.06 |
| No. of
medications | 1.90 | 1.32 | 2.11 | 1.46 | 5987.0 | 0.294 | 0.00 |
|
Antipsychotics | 1.26 | 0.94 | 1.20 | 1.07 | 6818.0 | 0.535 | 0.05 |
|
Non-antipsychotics | 0.65 | 1.04 | 0.91 | 1.27 | 5865.0 | 0.156 | -0.10 |
|
Vitamins | 0.62 | 0.87 | 0.70 | 0.92 | 6228.5 | 0.542 | -0.04 |
As regards categorical variables, the analyses
identified significant associations between pediatric risk of falls
and age (Table V). Among the
children who were at a higher risk of falls, those at an early age
(60%) were more susceptible than their counterparts in middle
childhood (34%) and adolescents (16%). However, the effect size was
small (P<0.001, φ=31).
 | Table VAnalysis of the associations between
pediatric risk of falls and categorical demographic variables. |
Table V
Analysis of the associations between
pediatric risk of falls and categorical demographic variables.
| | Low risk
(n=176) | High risk
(n=74) | |
|---|
| Variable | Categories | No. of
participants | % | No. of
participants | % | χ2 | df | P | φ/V |
|---|
| Age | Early (3-6
years) | 12 | 40.0 | 18 | 60.0 | 23.82 | 2 |
<0.001 | 0.31 |
| | Middle (7-12
years) | 75 | 65.8 | 39 | 34.2 | | | | |
| | Late (13-17
years) | 89 | 84.0 | 17 | 16.0 | | | | |
| Sex | Female | 51 | 79.7 | 13 | 20.3 | 3.56 | 1 | 0.059 | 0.12 |
| | Male | 125 | 67.2 | 61 | 32.8 | | | | |
| Education
status | Public school | 51 | 71.8 | 20 | 28.2 | 6.76a | 3 | 0.152 | 0.15 |
| | Disability/autism
center | 52 | 77.6 | 15 | 22.4 | | | | |
| | Other | 4 | 100.0 | 0 | 0.0 | | | | |
| | Not mentioned | 69 | 63.9 | 39 | 36.1 | | | | |
| Region | Riyadh | 130 | 71.8 | 51 | 28.2 | 0.64 | 1 | 0.425 | 0.05 |
| | Other regions | 46 | 66.7 | 23 | 33.3 | | | | |
| Parents'
knowledge | Yes | 133 | 73.9 | 47 | 26.1 | 3.76 | 1 | 0.053 | 0.12 |
| | No | 43 | 61.4 | 27 | 38.6 | | | | |
Logistic regression analysis of
pediatric risk of falls
Linear regression analysis was performed for
pediatric risk of falls, assessed using the HDFS as the dependent
variable. The predictors were age at first diagnosis, current age,
BMI, sex, education status, parents' knowledge about ASD, number of
diagnoses, number of comorbidities, number of antipsychotics and
non-antipsychotics taken (Table
VI). The regression model explained 23% of the pediatric risk
of falls variance [R=0.48, R2=0.23, F(10,238)=6.92,
P<0.001]. However, only two variables predicted a high risk of
falls in children with ASD: A lower current age of the child
(β=-0.34, P<0.001) and being male (β=0.21, P<0.001).
 | Table VILinear regression analysis of
pediatric risk of falls. |
Table VI
Linear regression analysis of
pediatric risk of falls.
| | 95% CI | Collinearity |
|---|
| Independent
variables | b | SE | β | t | P-value | LL | UL | Tolerance | VIF |
|---|
| (Intercept) | 12.30 | 0.63 | | 19.61 | <0.001 | 11.06 | 13.53 | | |
| Age at first
diagnosis | -0.06 | 0.04 | -0.12 | -1.46 | 0.145 | -0.15 | 0.02 | 0.48 | 2.10 |
| Current age | -0.16 | 0.04 | -0.34 | -3.96 | <0.001 | -0.23 | -0.08 | 0.46 | 2.19 |
| Body mass index
(BMI) | -0.01 | 0.02 | -0.04 | -0.56 | 0.578 | -0.05 | 0.03 | 0.84 | 1.19 |
| Sex | 0.86 | 0.24 | 0.21 | 3.64 | <0.001 | 0.40 | 1.33 | 0.97 | 1.03 |
| Education
status | -0.03 | 0.08 | -0.02 | -0.31 | 0.754 | -0.19 | 0.14 | 0.91 | 1.11 |
| Parents' knowledge
of autism | 0.15 | 0.24 | 0.04 | 0.64 | 0.524 | -0.31 | 0.61 | 0.93 | 1.08 |
| No. of
diagnoses | 0.03 | 0.12 | 0.02 | 0.23 | 0.818 | -0.21 | 0.26 | 0.74 | 1.35 |
| No. of
comorbidities | 0.02 | 0.23 | 0.01 | 0.10 | 0.923 | -0.44 | 0.48 | 0.94 | 1.07 |
| No. of
antipsychotics taken | 0.06 | 0.11 | 0.03 | 0.54 | 0.590 | -0.16 | 0.28 | 0.88 | 1.14 |
| No. of
non-antipsychotics taken | 0.10 | 0.11 | 0.06 | 0.92 | 0.357 | -0.11 | 0.31 | 0.71 | 1.42 |
Discussion
The present study identified an association between
the age of children and the total number of medications taken and
antipsychotic medications used. Furthermore, the findings indicated
a significant association between the risk of falls and age. The
results of logistic regression analysis suggested that multiple
factors, including a lower current age and the male sex, predict
the risk of falls. Among the health conditions that were comorbid
with ASD, the results revealed that ASD conditions have a high
comorbidity burden with a significant co-occurrence of ADHD,
followed by intellectual disabilities and epilepsy. Overall,
comorbidity profiles were present in almost 80% of ASD cases. This
reflects the fact that comorbidity is an emerging health concern in
ASD (14). Notably, the high
comorbidity profile associated with ASD is a confounding factor in
elucidating the pathological mechanisms of ASD and is the
foundation of ASD heterogeneity. It has been previously proposed
that ASD can be categorized into essential and complex ASD, the
latter of which refers to individuals who have a greater number of
seizures and lower intellectual capabilities (15).
Presenting with a comorbidity is linked to poorer
health outcomes and elevated healthcare needs among children
diagnosed with ASD, including, but not restricted, to management by
different clinical disciplines, economic burden, and coordinating
clinical, behavioral and pharmacological management (16). Identifying and characterizing the
number of health comorbidities is essential in mapping ASD cases as
it aids in treatment and prognosis (17). A comprehensive understanding of
comorbidities generally improves health metrics and quality of life
(18).
The comorbidity of ADHD and ASD is, however, well
recognized. In a previous study, utilizing a cross-sectional study
design, the co-occurrence of both conditions was evident in almost
50% of the study sample which comprised more than three thousand
children with ASD (19). In a
meta-analysis study, it was found that compared to adolescents,
children with ASD exhibited a higher prevalence of ADHD and
sleep-related issues (20).
However, the comorbidity of ASD-ADHD continues to be a subject of
debate (21). Furthermore, both
ASD and ADHD are described separately in the Diagnostic and
Statistical Manual of Mental Disorders version 5 (DSM-5).
Nevertheless, both similarities and differences between them were
included (22), indicating a
potential recognition of ASD-ADHD in future versions of DSM. Our
findings align with existing literature and highlight the existence
of a clinically distinct subgroup of ASD-ADHD (19,21,23).
Therefore, moving forward and establishing characteristic
diagnostic and management strategies is paramount.
A previous study also indicated that the rate of
antipsychotics taken in children with ASD is high (24). According to a previous
meta-analysis, the rate is expected to reach 1 adolescent with ASD
in every 10 adolescents treated with antipsychotics. This could be
driven by the fact that aggression, irritability (25) and other psychiatric conditions are
commonplace in ASD (26). Evidence
extracted from a systematic review and meta-analysis revealed that
antipsychotics engender a significant clinical improvement in
children with ASD compared to adults (27). The present study found that the age
of the children and the total number of medications taken were
positively associated. In support of these findings, previous
studies have indicated that increases in age correlate with the
number of medicines used (28-30).
For instance, a significant association between age and treatment
was found in a report utilizing the Simons Simplex Collection
(29).
The present study also identified an association
between the age at first diagnosis and the risk of falls among
children with ASD. Specifically, those at a higher risk of falls
were diagnosed with their condition <6 years of age, while those
at a lower risk received their diagnosis at ~8 years of age. In
general, the risk of falls and fall-related consequences were
reported to be higher in younger children than in older ones.
Specifically, it was found that there were ~20 fall-related deaths
in children <5 years of age and 10 fall-related deaths in
children aged between 5 and 9 years (31).
Herein, a significant association was also found
between the age at first diagnosis and the risks of falls. This
could be driven by the fact that a younger age at first diagnosis
is linked to severe behavioral symptoms, including aggression and
tantrums (32). In line with this
finding, a significant number of toddlers diagnosed with ASD <4
years of age present with more complex medical conditions (33). Alongside this, the time of
diagnosis is also clinically relevant (34).
One of the ASD-associated symptoms is motor
dysfunction. Hypotonia was documented to have prevailed in 50% of
ASD cases in a retrospective study conducted at the New Jersey
Medical School autism center. Notably, this functional reduction in
muscle tone was found to be improved in older ASD cases (35). Supporting these findings, the risks
of falls are reduced as age increases. In support of this, a recent
qualitative study demonstrated that children with ASD are prone to
accidental injuries. These injuries were associated with risk
factors, including comorbidity of other conditions (36). Another report indicated that the
most common accidental injury in ASD was a mechanical fall, which
was documented in 44% of the study sample (37). According to the World Health
Organization, falls account for >600,000 deaths each year, and
it is the second leading cause of mortality (38). Yet, the defined characterizations
of motor dysfunction consequences, detection, and interventions
have not been well investigated in ASD (39).
The prevalence of ASD differs regionally. For
example, in some USA states such as Pennsylvania and California, it
can reach around 50 cases per 1,000 children. Other states could be
estimated to be 15 per 1,000 children (40). On the other hand, ASD is estimated
at 9.4 per 1,000 children in Korea (41). Even there are regional differences
in the documented ASD cases, the fact that it is comorbid with ADHD
and linked to an elevated rate of falls is consistent. The data of
the present study enhance existing knowledge regarding the
association between the pediatric risk of falls and younger age and
the comorbidities of ASD and ADHD. The present study found that in
the Saudi population, the comorbidity of ASD-ADHD was consistent
with previous findings in Taiwanese (42), English (43) and Korean populations (44). In line with this, the elevated risk
of falls was recognized to be linked to ASD in different
populations (8,45).
The associated ASD-ADHD comorbidity and risk of
falls are predominant in different cultures, providing insights
that enrich global understandings and recognition of ASD-associated
conditions and consequences. It underscores the significance of
raising parents' awareness of the risks of falls, considering that
sometimes falls are not reported to the healthcare system (46). It further highlights the need to
establish an early intervention in younger ASD children to reduce
the health burden and improve clinical safety in ASD children at
the global level.
The present study has several clinical implications.
Firstly, it highlights the heterogeneity of ASD and its association
with severe consequences such as risk of falls. Thus, it is
recommended that healthcare professionals establish policies aimed
at raising awareness and educating families about the risk of falls
in younger individuals with ASD, particularly those who are taking
antipsychotics, and implement these educational workshops to be
mandatory appointments/sessions with healthcare professionals,
whether under a family care unit or primary healthcare clinic.
Secondly, as the association is significant, the findings affirm
ASD-ADHD comorbidity, and thus the need to establish characteristic
diagnostic and management strategies is paramount.
The present study however, also has certain
limitations, which should be mentioned. The present study provides
evidence regarding the current status of treatment and
comorbidities of children with ASD. The children's comorbidity
burden and treatment patterns were characterized. The present study
also conducted a correlation analysis to evaluate the risks of
falls among different age groups using observational data on 250
patients with ASD from routine clinical practice at KSUMC. However,
the present study has a number of limitations that need to be
addressed. Firstly, the sample size was relatively small. Although
multiple EMR studies have been published with a similar sample size
range (47,48), 250 is appropriate if statistically
robust conclusions are to be drawn. It is therefore recommended
that these findings be replicated using a larger sample size.
Furthermore, the present study was a single-center report, thus
rendering it necessary to expand these findings using a multicenter
study design (49,50). Additionally, the present study
focused on the pharmacological treatment approach. Indeed, it is
widely acknowledged that a majority of children with ASD take
pharmacological treatment (11).
However, ASD is also managed using behavioral and pharmacological
treatment strategies (51).
Furthermore, the findings report the current status of the number
of medications taken; however, no history of the number of
medications taken was obtained. In addition, although
pharmacological treatment was characterized, compliance was not
investigated. Moreover, in any follow-up, further adjustment of
diverse covariance is required for the multifactorial features of
ASD, ASD management, comorbidity and the risk of falls.
In conclusion, ASD is increasingly being recognized
as a significant and growing public health concern. It places a
substantial socio-economic burden upon families. The findings of
the present study confirm existing evidence regarding the link
between the pediatric risk of falls and a younger age.
Additionally, the present study confirmed the comorbidity of ASD
and ADHD, emphasizing the need to identify ASD-ADHD in the future
as a clinical subgroup of developmental disorders. These results
will also encourage healthcare practitioners to increase parental
awareness of the risks of falls in young autistic children.
Supplementary Material
Data S1
Data S2
Categorization of particular
additional diseases reported in children with autism (n=250).
Acknowledgements
The authors express their gratitude to the College
of Pharmacy Research Center and the Deanship of Scientific Research
at King Saud University for their continuous support, the provision
of research facilities and infrastructure, administrative
assistance, and encouragement throughout the duration of this
study.
Funding
Funding: Financial funding was provided by the King Abdul-Aziz
City for Science and Technology, General Directorate for Fund and
Grants to King Saud University to implement the study (Project no.
5-21-01-001-0015).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
MAA, TKA and AMR conceptualized the study and were
involved in the study methodology. AMR was involved in the formal
analysis. HMA and SAA were involved in the investigative aspects of
the study. HAA, SAA and AMR were involved in data curation. MAA and
TKA confirm the authenticity of all the raw data. HAA, SAA, TKA and
AMR were involved in the writing and preparation of the original
draft of the manuscript. TKA, MAA and AMR were involved in the
writing, reviewing and editing of the manuscript. MAA and TKA
supervised the study. MAA was involved in project administration.
All authors have read and agreed to the published version of the
manuscript.
Ethics approval and consent to
participate
Ethical approval was granted by the Institutional
Review Board at King Saud University in Riyadh, Saudi Arabia (Ref.
E-22-7451 no. 23/0175/IRB); issue date, March 2, 2023. A waiver of
written informed consent was granted by the ethics committee.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cervera GR, Romero MGM, Mas LA and Delgado
FM: Intervention models in children with autism spectrum disorders.
In: Autism Spectrum Disorders. Tim W (ed). IntechOpen, Rijeka, p7,
2011.
|
|
2
|
Zeidan J, Fombonne E, Scorah J, Ibrahim A,
Durkin MS, Saxena S, Yusuf A, Shih A and Elsabbagh M: Global
prevalence of autism: A systematic review update. Autism Res.
15:778–790. 2022.PubMed/NCBI View
Article : Google Scholar
|
|
3
|
Hyman SL, Levy SE and Myers SM: Council on
Children with Disabilities, Section on Developmental and Behavioral
Pediatrics. Identification, evaluation, and management of children
with autism spectrum disorder. Pediatrics.
145(e20193447)2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hussain A, John JR, Dissanayake C, Frost
G, Girdler S, Karlov L, Masi A, Alach T and Eapen V: Sociocultural
factors associated with detection of autism among culturally and
linguistically diverse communities in Australia. BMC Pediatr.
23(415)2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Faruk MO, Rahman MS, Rana MS, Mahmud S,
Al-Neyma M, Karim MS and Alam N: Socioeconomic and demographic risk
factors of autism spectrum disorder among children and adolescents
in Bangladesh: Evidence from a cross-sectional study in 2022. PLoS
One. 18(e0289220)2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Pan PY, Bölte S, Kaur P, Jamil S and
Jonsson U: Neurological disorders in autism: A systematic review
and meta-analysis. Autism. 25:812–830. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Craig F, Castelnuovo R, Pacifico R, Leo R
and Trabacca A: BIM Falls Study Group*. Falls in hospitalized
children with neurodevelopmental conditions: A cross-sectional,
correlational study. Rehabil Nurs. 43:335–342. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
DiGuiseppi C, Levy SE, Sabourin KR, Soke
GN, Rosenberg S, Lee LC, Moody E and Schieve LA: Injuries in
children with autism spectrum disorder: Study to explore early
development (SEED). J Autism Dev Disord. 48:461–472.
2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Shin HJ, Kim YN, Kim JH, Son IS and Bang
KS: A pediatric fall-risk assessment tool for hospitalized
children. Child Health Nurs Res. 20:215–224. 2014.
|
|
10
|
Malone RP and Waheed A: The role of
antipsychotics in the management of behavioural symptoms in
children and adolescents with autism. Drugs. 69:535–548.
2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Jonkman KM, Back E and Begeer S:
Predicting intervention use in autistic children: Demographic and
autism-specific characteristics. Autism. 27:428–442.
2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lee McIntyre L and Zemantic PK: Examining
services for young children with autism spectrum disorder: Parent
satisfaction and predictors of service utilization. Early Child
Educ J. 45:727–734. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Alnemary FM, Aldhalaan HM, Simon-Cereijido
G and Alnemary FM: Services for children with autism in the Kingdom
of Saudi Arabia. Autism. 21:592–602. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ahmedani BK and Hock RM: Health care
access and treatment for children with co-morbid autism and
psychiatric conditions. Soc Psychiatry Psychiatr Epidemiol.
47:1807–1814. 2012.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Miles JH, Takahashi TN, Bagby S, Sahota
PK, Vaslow DF, Wang CH, Hillman RE and Farmer JE: Essential versus
complex autism: Definition of fundamental prognostic subtypes. Am J
Med Genet A. 135:171–180. 2005.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Casanova MF, Frye RE, Gillberg C and
Casanova EL: Editorial: Comorbidity and autism spectrum disorder.
Front Psychiatry. 11(617395)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Rim SJ, Kwak K and Park S: Risk of
psychiatric comorbidity with autism spectrum disorder and its
association with diagnosis timing using a nationally representative
cohort. Res Autism Spectr Disord. 104(102134)2023.
|
|
18
|
Butterly EW, Hanlon P, Shah ASV, Hannigan
LJ, McIntosh E, Lewsey J, Wild SH, Guthrie B, Mair FS, Kent DM, et
al: Comorbidity and health-related quality of life in people with a
chronic medical condition in randomised clinical trials: An
individual participant data meta-analysis. PLoS Med.
20(e1004154)2023.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Gordon-Lipkin E, Marvin AR, Law JK and
Lipkin PH: Anxiety and mood disorder in children with autism
spectrum disorder and ADHD. Pediatrics.
141(e20171377)2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Micai M, Fatta LM, Gila L, Caruso A,
Salvitti T, Fulceri F, Ciaramella A, D'Amico R, Del Giovane C,
Bertelli M, et al: Prevalence of co-occurring conditions in
children and adults with autism spectrum disorder: A systematic
review and meta-analysis. Neurosci Biobehav Rev.
155(105436)2023.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Hours C, Recasens C and Baleyte JM: ASD
and ADHD comorbidity: What are we talking about? Front Psychiatry.
13(837424)2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
American Psychiatric Association (APA):
Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR).
APA, Washington, DC, 2013.
|
|
23
|
Miller M, Austin S, Iosif AM, de la Paz L,
Chuang A, Hatch B and Ozonoff S: Shared and distinct developmental
pathways to ASD and ADHD phenotypes among infants at familial risk.
Dev Psychopathol. 32:1323–1334. 2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Rast JE, Anderson KA, Roux AM and Shattuck
PT: Medication use in youth with autism and
attention-deficit/hyperactivity disorder. Acad Pediatr. 21:272–279.
2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Park SY, Cervesi C, Galling B, Molteni S,
Walyzada F, Ameis SH, Gerhard T, Olfson M and Correll CU:
Antipsychotic use trends in youth with autism spectrum disorder
and/or intellectual disability: A meta-analysis. J Am Acad Child
Adolesc Psychiatry. 55:456–468.e4. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Posey DJ, Stigler KA, Erickson CA and
McDougle CJ: Antipsychotics in the treatment of autism. J Clin
Invest. 118:6–14. 2008.PubMed/NCBI View
Article : Google Scholar
|
|
27
|
Deb S, Roy M, Limbu B, Akrout Brizard B,
Murugan M, Roy A and Santambrogio J: Randomised controlled trials
of antipsychotics for people with autism spectrum disorder: A
systematic review and a meta-analysis. Psychol Med. 53:7964–7972.
2023.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Houghton R, Ong RC and Bolognani F:
Psychiatric comorbidities and use of psychotropic medications in
people with autism spectrum disorder in the United States. Autism
Res. 10:2037–2047. 2017.PubMed/NCBI View
Article : Google Scholar
|
|
29
|
Mire SS, Raff NS, Brewton CM and
Goin-Kochel RP: Age-related trends in treatment use for children
with autism spectrum disorder. Res Autism Spect Disord.
15-16:29–41. 2015.
|
|
30
|
Xu G, Strathearn L, Liu B, O'Brien M,
Kopelman TG, Zhu J, Snetselaar LG and Bao W: Prevalence and
treatment patterns of autism spectrum disorder in the United
States, 2016. JAMA Pediatr. 173:153–159. 2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Gill AC and Kelly NR: Falls and
fall-related injuries in children: Prevention.
UpToDate®, 2025. https://www.uptodate.com/contents/falls-and-fall-related-injuries-in-children-prevention.
Accessed November 23, 2024.
|
|
32
|
Sicherman N, Charite J, Eyal G, Janecka M,
Loewenstein G, Law K, Lipkin PH, Marvin AR and Buxbaum JD: Clinical
signs associated with earlier diagnosis of children with autism
Spectrum disorder. BMC Pediatr. 21(96)2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Kim SH, Macari S, Koller J and Chawarska
K: Examining the phenotypic heterogeneity of early autism spectrum
disorder: Subtypes and short-term outcomes. J Child Psychol
Psychiatry. 57:93–102. 2016.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Wiggins LD, Baio J and Rice C: Examination
of the time between first evaluation and first autism spectrum
diagnosis in a population-based sample. J Dev Behav Pediatr. 27 (2
Suppl):S79–S87. 2006.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Ming X, Brimacombe M and Wagner GC:
Prevalence of motor impairment in autism spectrum disorders. Brain
Dev. 29:565–570. 2007.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Morgan CH, Mercier A, Stein B, Guest KC,
O'Kelley SE and Schwebel DC: A qualitative analysis of
unintentional injuries in autism spectrum disorder. J Autism Dev
Disord: Jan 27, 2025 (Epub ahead of print).
|
|
37
|
Jones V, Ryan L, Rooker G, Debinski B,
Parnham T, Mahoney P and Shields W: An exploration of emergency
department visits for home unintentional injuries among children
with autism spectrum disorder for evidence to modify injury
prevention guidelines. Pediatr Emerg Care. 37:e589–e593.
2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
World Health Organization (WHO): Falls
Fact Sheet. WHO, Geneva, 2021. https://www.who.int/news-room/fact-sheets/detail/falls.
|
|
39
|
Zampella CJ, Wang LAL, Haley M, Hutchinson
AG and de Marchena A: Motor skill differences in autism spectrum
disorder: A clinically focused review. Curr Psychiatry Rep.
23(64)2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Shaw KA, Williams S, Patrick ME,
Valencia-Prado M, Durkin MS, Howerton EM, Ladd-Acosta CM, Pas ET,
Bakian AV, Bartholomew P, et al: Prevalence and early
identification of autism spectrum disorder among children aged 4
and 8 years-autism and developmental disabilities monitoring
network, 16 sites, United States, 2022. MMWR Surveill Summ.
74:1–22. 2025.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Yoo SM, Kim KN, Kang S, Kim HJ, Yun J and
Lee JY: Prevalence and premature mortality statistics of autism
spectrum disorder among children in Korea: A nationwide
population-based birth cohort study. J Korean Med Sci.
37(e1)2022.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Chen MH, Wei HT, Chen LC, Su TP, Bai YM,
Hsu JW, Huang KL, Chang WH, Chen TJ and Chen YS: Autistic spectrum
disorder, attention deficit hyperactivity disorder, and psychiatric
comorbidities: A nationwide study. Res Autism Spect Disord. 10:1–6.
2015.
|
|
43
|
Simonoff E, Pickles A, Charman T, Chandler
S, Loucas T and Baird G: Psychiatric disorders in children with
autism spectrum disorders: Prevalence, comorbidity, and associated
factors in a population-derived sample. J Am Acad Child Adolesc
Psychiatry. 47:921–929. 2008.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Kim MJ, Park I, Lim MH, Paik KC, Cho S,
Kwon HJ, Lee SG, Yoo SJ and Ha M: Prevalence of
attention-deficit/hyperactivity disorder and its comorbidity among
Korean children in a community population. J Korean Med Sci.
32:401–406. 2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Florence C, Simon T, Haegerich T, Luo F
and Zhou C: Estimated lifetime medical and work-loss costs of fatal
injuries-United States, 2013. MMWR Morb Mortal Wkly Rep.
64:1074–1077. 2015.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Shmueli D, Razi T, Almog M, Menashe I and
Mimouni Bloch A: Injury rates among children with autism spectrum
disorder with or without attention-deficit/hyperactivity disorder.
JAMA Netw Open. 8(e2459029)2025.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Al-Amoosh HHS, Al-Amer R, Alamoush AH,
Alquran F, Atallah Aldajeh TM, Al Rahamneh TA, Gharaibeh A, Ali AM,
Maaita M and Darwish T: Outcomes of COVID-19 in pregnant women: A
retrospective analysis of 300 cases in Jordan. Healthcare (Basel).
12(2113)2024.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Spencer RA, Spencer SEF, Rodgers S,
Campbell SM and Avery AJ: Processing of discharge summaries in
general practice: A retrospective record review. Br J Gen Pract.
68:e576–e585. 2018.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Jo D: The interpretation bias and trap of
multicenter clinical research. Korean J Pain. 33:199–200.
2020.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Seifirad S and Alquran L: The bigger, the
better? When multicenter clinical trials and meta-analyses do not
work. Curr Med Res Opin. 37:321–326. 2021.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Höfer J, Hoffmann F and Bachmann C: Use of
complementary and alternative medicine in children and adolescents
with autism spectrum disorder: A systematic review. Autism.
21:387–402. 2017.PubMed/NCBI View Article : Google Scholar
|