Introduction
Penile abscess is a rare and uncommon urological
condition with various known etiologies, including idiopathic
causes, complications from endourologic procedures such as
cavernoscopy, penile injections, instrumentation, trauma,
gonorrhea, tuberculosis, priapism and the hematogenous spread of
distant infections (1).
Clinically, penile abscesses typically present with painful
erections and localized swelling, potentially leading to severe
complications. The most frequently reported microorganisms include
Bacteroides, Fusobacteria, Streptococci and
Staphylococcus aureus (2).
Complications associated with penile abscess include penile
curvature, fibrosis and the spread of infection to adjacent or
distant anatomical regions, potentially resulting in fistula
formation. Prompt identification and timely intervention are
essential for preventing these complications, even in the absence
of clearly identifiable precipitating factors (3).
Several imaging modalities, including computed
tomography (CT), magnetic resonance imaging (MRI), cavernosography
and ultrasonography (US) ARE utilized to diagnose and manage penile
abscesses (4). Treatment
strategies are typically determined by the severity and etiology of
the infection. While systemic antibiotic therapy and surgical
incision and drainage remain the mainstays of treatment, some
studies suggest successful outcomes using aspiration techniques
guided by imaging, particularly MRI and US (2,5). Two
previous studies demonstrated favorable outcomes in the treatment
of penile abscess, emphasizing the importance of understanding its
etiologies, clinical presentation, and management options (1,6). The
present systematic review aimed to provide a comprehensive overview
of penile abscess and its complications, topics that were seldom
discussed in the existing literature, and to enhance clinical
knowledge among healthcare professionals involved in diagnosing and
managing this rare urologic condition.
Data and methods
The present systematic review was conducted in
accordance with the Preferred Reporting Items for Systematic
Reviews and Meta-Analyses (PRISMA) 2020 guidelines (7).
Database search
A comprehensive electronic search was performed
using the PubMed, ScienceDirect, Web of Science, the Cochrane
Central Register of Trials (CENTRAL) databases, and the Cumulated
Index to Nursing and Allied Health Literature (CINAHL) using the
following key words: ‘penile’ OR ‘penis’ OR ‘corpus cavernosum’ AND
‘abscess’ OR ‘suppuration’ OR ‘infection’. The search included
studies published up to December 10, 2023. Only peer-reviewed
studies involving adult human subjects (aged ≥18 years of age) and
published in the English language were considered. All identified
articles were imported into Mendeley Reference Manager, and
duplicates were removed through both digital and manual processes.
The resulting articles were then exported to Microsoft Excel for
title and abstract screening, followed by full-text review.
Study selection
The present systematic review primarily focused on
case report analyses. A total of two independent reviewers screened
the titles and abstracts to determine their eligibility. Studies
were included if they met all of the following criteria: i)
Reported cases of corpus cavernosum or penile abscess; ii)
described either conservative or surgical treatment; iii) detailed
complications, treatment methods and clinical outcomes; iv) were
published in peer-reviewed journals; and v) were available in
English. Studies were excluded if they were non-English, lacked
full-text access, were review articles, letters to the editor, or
conference abstracts, or had irrelevant content. Abstracts without
sufficient methodological or clinical details were also excluded.
Disagreements during the selection process were resolved through
discussion.
Data extraction
Data from each included study were independently
extracted by two authors (FFP and RN) using a standardized data
extraction form. Extracted variables included the first author's
name, year of publication, study location, study design, patient
demographics, etiology of the abscess, clinical features, treatment
modalities, outcomes and reported complications. Any disagreements
between reviewers were resolved through discussion, with a third
author acting as an arbitrator if necessary.
Integration of results
The extracted data were synthesized qualitatively
due to the limited number of cases and the heterogeneity of study
designs, underlying etiologies, clinical presentations,
interventions, diagnostic approaches, and outcome measures. A
quantitative meta-analysis was not feasible under these
conditions.
Evaluation of the risk of biases
Each included study was assessed for quality using
the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for
Case Reports (8). Two independent
reviewers (FFP and RN) performed the assessments, and any
discrepancies were resolved through discussion. The checklist
consisted of eight items, and studies meeting at least five
criteria were deemed to be of acceptable quality and included in
the final synthesis.
Results
Record inclusion
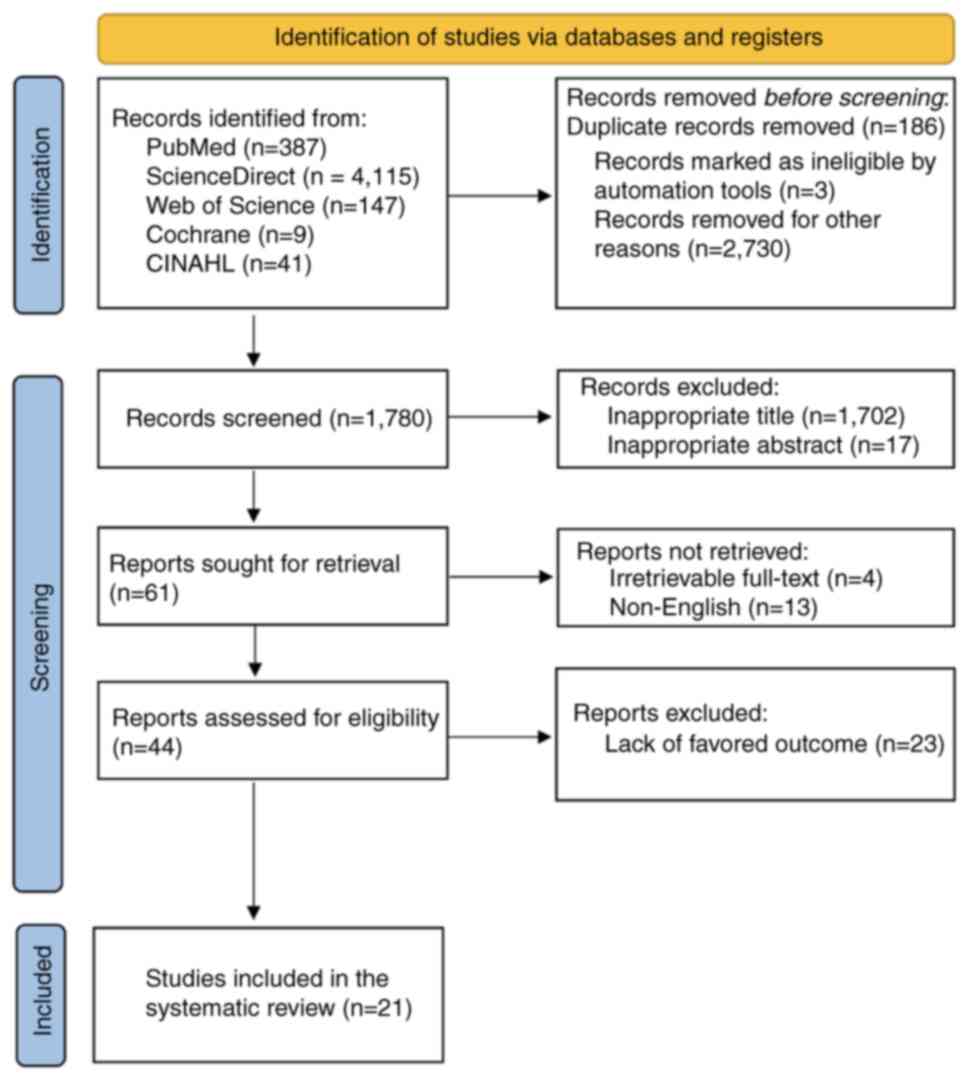
A total of 4,699 records were identified through the
initial database search. Following the removal of 186 duplicate
entries, 4,513 studies remained for screening. After reviewing
1,780 entries, 1,702 titles and 17 abstracts were excluded. In
addition, 17 articles were not retrievable due to inaccessible full
texts (n=4) or non-English language (n=13). Subsequently, 44
articles were assessed for full eligibility, of which 21 case
report studies were ultimately included in the present systematic
review. The PRISMA flow diagram (Fig.
1) illustrates the selection process and reasons for
exclusion.
Evaluating risk of bias
The initial criterion assessed was patient
demographics, which included sex, age, and in some cases, race, all
of which were reported in the included studies. However, three
studies omitted patient histories and chronological timelines. All
21 studies fulfilled the third criterion, which required a clear
description of the patients' clinical presentation. Of note, two
studies lacked sufficient details regarding diagnostic procedures
and their findings. The fifth criterion assessed the explanation of
intervention and treatment procedures; all studies addressed this,
although some only briefly.
A total of 18 studies provided sufficient
post-treatment follow-up, reporting pain relief and abscess
resolution, while three studies lacked such information. Unexpected
events or complications were not described in two of the case
reports, which constituted the seventh criterion. The final
criterion evaluated whether the case report included lessons
learned or clinical implications; 14 studies fulfilled this
requirement. Overall, the majority of case reports contained
adequate information on patient demographics, clinical history,
diagnostic approaches and outcomes. Based on the JBI checklist, all
21 studies were determined to be of acceptable quality and were
included in the present systematic review (2,4,9-27)
(Table I).
 | Table IQuality assessment of the included
studies based on JBI criteria. |
Table I
Quality assessment of the included
studies based on JBI criteria.
| | Criteria | |
|---|
| First author, year
of publication | Patient demographic
characteristics | Patient history
presented as timeline | Current clinical
condition | Diagnostic tests or
assessment methods and the results | Intervention(s) or
treatment procedure(s) | Post-intervention
clinical condition | Adverse events
(harms) or unanticipated events | Takeaway
lessons | Overall
appraisal | (Refs.) |
|---|
| Dugdale, 2013 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Include | (2) |
| Brennan, 2013 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Include | (4) |
| Charles, 2009 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Include | (9) |
| Dempster, 2013 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Include | (10) |
| Ehara, 2007 | ✓ | - | ✓ | ✓ | ✓ | ✓ | ✓ | - | Include | (11) |
| Frank, 1999 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | - | Include | (12) |
| Gore, 2020 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Include | (13) |
| Hidaka, 2022 | ✓ | ✓ | ✓ | - | ✓ | ✓ | ✓ | ✓ | Include | (14) |
| Jinga, 2012 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Include | (15) |
| Kachare, 2022 | ✓ | - | ✓ | ✓ | ✓ | ✓ | - | - | Include | (16) |
| Kızılkan, 2018 | ✓ | ✓ | ✓ | ✓ | ✓ | - | ✓ | ✓ | Include | (17) |
| Lazarou, 2019 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Include | (18) |
| Minagawa, 2015 | ✓ | ✓ | ✓ | ✓ | ✓ | - | ✓ | ✓ | Include | (19) |
| Moussa, 2019 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | - | - | Include | (20) |
| Paladino, 2014 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Include | (21) |
| Sagar, 2005 | ✓ | ✓ | ✓ | - | ✓ | ✓ | ✓ | - | Include | (22) |
| Sater, 1989 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | - | Include | (23) |
| Shamloul, 2006 | ✓ | - | ✓ | ✓ | ✓ | ✓ | ✓ | - | Include | (24) |
| Tüzel, 2015 | ✓ | ✓ | ✓ | ✓ | ✓ | - | ✓ | ✓ | Include | (25) |
| Wang, 2023 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Include | (26) |
| Yamagishi,
2021 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Include | (27) |
Evidence synthesis
Table II
summarizes the characteristics of the 21 included case reports,
each involving one adult patient diagnosed with corpus cavernosum
or penile abscess. The studies were distributed across five
continents: Europe (n=7), Asia (n=7), USA and South America (n=5),
Africa (n=1) and Australia (n=1). The age of the patients ranged
from 19 to 75 years. In general, the most prevalent presenting
symptoms mentioned in the included studies were penile pain and
edema. The included studies reported several etiologies for penile
abscess. As regards the cause of penile abscess, five included
studies indicated either spontaneous or idiopathic penile abscesses
(4,10,11,22,23).
whereas other studies reported the association of penile abscess
with a different etiology, including priapism (14,26),
penile injection (15,17,24),
oral sex and periodontal abscess (9), genital trauma (18), immunocompromised condition
(16,20,25),
erectile dysfunction (2),
hematological spread of distal infections (12), or other pathologies in the urethra
and corpus cavernosum (13,19,27).
The most common causal organisms were Staphylococcus and
Streptococci. Negative culture was reported in several
studies (10,14,19,27),
whereas one case report did not mention the causative organisms
(23).
 | Table IIDescription of the characteristics of
the included studies. |
Table II
Description of the characteristics of
the included studies.
| First author, year
of publication | Country | Study design | Age, years | Etiology | Imaging | Pathogenic
bacteria | Treatment |
Outcomes/complications | (Refs.) |
|---|
| Dugdale, 2013 | USA | Case report | 48 | Erectile
dysfunction | CT scan | Streptococcus
anginosus and Streptococcus constellatus | Surgical incision
and drainage + systemic antibiotic | Recurrent abscess,
erectile dysfunction | (2) |
| Brennan, 2013 | Ireland | Case report | 56 | Idiopathic | MRI | Streptococcus
constellatus and Streptococcus intermedius | Surgical incision
and drainage + systemic antibiotic | Penile deviation
(ipsilateral chordee) | (4) |
| Charles, 2009 | France | Case report | 46 | Oral sex,
periodontal abscess | US and MRI | Streptococcus
constellatus and Peptostreptococcus | Surgical incision
and drainage + systemic antibiotic | Erectile
dysfunction | (9) |
| Dempster, 2013 | UK | Case report | 32 | Idiopathic | US | Negative
culture | Open cavernostomy
and debridement + systemic antibiotic | Erectile
dysfunction, need for implantation of prosthesis | (10) |
| Ehara, 2007 | Japan | Case report | 54 | Idiopathic | MRI |
Methicillin-resistant Staphylococcus
aureus | Surgical incision
and drainage + systemic antibiotic | Recurrent abscess
leading to total penectomy and perineal urethrostomy | (11) |
| Frank, 1999 | USA | Case report | 59 | Intraabdominal
abscess | CT scan | Enterococcus
sp. | Bilateral
corporotomy + systemic antibiotic | Recurrent abscess,
pubic osteomyelitis, erectile dysfunction | (12) |
| Gore, 2020 | USA | Case report | 34 | Perforation of
urethral diverticulum | CT scan | Peptoniphilus
asaccharolyticus and Corynebacterium sp. | Bilateral corporal
cavernostomies + systemic antibiotic | Necrotic tissue
development, erectile dysfunction | (13) |
| Hidaka, 2022 | Brazil | Case report | 42 | Ischemic
priapism | - | Negative
culture | Surgical incision
and drainage + systemic antibiotic | Erectile
dysfunction, need for implantation of prosthesis | (14) |
| Jinga, 2012 | Romania | Case report | 49 | Papaverine
injection | US | Klebsiella
sp. | Surgical incision
and drainage + systemic antibiotic | Urethrocutaneous
fistula | (15) |
| Kachare, 2022 | India | Case report | 40 | Type 2 diabetes
mellitus | US | Acinetobacter
sp. | US-guided puncture
and drainage + systemic antibiotic | Resolution of
penile abscess | (16) |
| Kızılkan, 2018 | Turkiye | Case report | 45 | Papaverine
injection | MRI | Staphylococcus
aureus | Surgical incision
and drainage + systemic antibiotic | Erectile
dysfunction, need for implantation of prosthesis | (17) |
| Lazarou, 2019 | Greece | Case report | 37 | Sexual trauma | US and MRI | Streptococcus
intermedius, Prevotella bivia, Peptostreptococcus
micros, Fusobacterium spp., and Actinomyces
meyeri | Surgical incision
and drainage + systemic antibiotic | Erectile
dysfunction | (18) |
| Minagawa, 2015 | Japan | Case report | 75 |
Xantho-granulomatous granuloma in the
corpus cavernosum | US and CT scan | Negative
culture | CT-guided
percutaneous drainage + systemic antibiotic total penectomy and
urethral perineal fistula formation | Painful penile
symptoms | (19) |
| Moussa, 2019 | Lebanon | Case report | 60 | Type 2 diabetes
mellitus | MRI | Staphylococcus
aureus | US-guided
aspiration drainage + systemic antibiotic | Resolution of
penile abscess | (20) |
| Paladino, 2014 | Brazil | Case report | 23 | After Winter's
procedure | CT scan | Multisensitive
coagulase-negative Staphylococci | Needle aspiration
puncture drainage + systemic antibiotic | Erectile
dysfunction, need for implantation of prosthesis | (21) |
| Sagar, 2005 | UK | Case report | 19 | Idiopathic | - | Staphylococcus
aureus | Surgical incision
and drainage + systemic antibiotic | Penile deviation
(chordee) | (22) |
| Sater, 1989 | Belgium | Case report | 38 | Idiopathic | CT scan | Not reported | Surgical incision
and drainage + systemic antibiotic | Erectile
dysfunction, penile deviation | (23) |
| Shamloul, 2006 | Egypt | Case report | 53 | Intracavernous
injection of PGE1 | US | Bacteroides
sp. | Drainage and
debridement of cavernous body + systemic antibiotic | Penile
deviation | (24) |
| Tüzel, 2015 | Turkiye | Case report | 38 | Chronic anabolic
androgenic steroid abuse | US | Staphylococcus
epidermidis | Surgical incision
and drainage + systemic antibiotic | Penile
deviation | (25) |
| Wang, 2023 | Australia | Case report | 50 | Ischemic
priapism | US and MRI | Prevotella
bivia and Streptococcus anginosus | Surgical incision
and drainage + systemic antibiotic | Recurrent abscess,
erectile dysfunction | (26) |
| Yamagishi,
2021 | Japan | Case report | 64 | Urethral stricture,
catheter placement | MRI | Negative
culture | Surgical incision
and drainage + systemic antibiotic | Penile
deviation | (27) |
In addition to CT scan imaging, the majority of the
included studies reported the use of MRI and US as imaging
modalities to assess penile abscess cases. However, due to resource
limitations, two studies assessed the condition based solely on
clinical presentation (14,22).
As regards treatment options, the majority of cases were managed
with surgical incision and drainage accompanied by systemic
antibiotics, although the duration of treatment varied.
Furthermore, two studies described the use of ultrasound-guided
drainage and puncture for penile abscesses (16,20),
while one study reported a case of percutaneous drainage guided by
CT scan (19).
Overall, during the follow-up period, all studies
documented positive therapeutic outcomes, defined by abscess
resolution and the alleviation of clinical symptoms. Erectile
dysfunction was reported as the most frequent complication
following incision and drainage, as shown in 19 patients that
exhibited post-operative complications (9,10,12-14,17-19,21,23,26).
This condition often necessitated prosthesis insertion. In addition
to ED, 5 patients reported the occurrence of chordee or penile
deviation following surgery (4,22,24,25,27),
followed by recurrent abscess (2,11,12,26),
urethrocutaneous fistula (15) and
painful penile symptoms (19),
However, two studies found that the penile abscess resolved without
any complications, indicating that ultrasound-guided aspiration
drainage may have been beneficial in reducing postoperative risks
(16,20). Detailed information of the
characteristics of the included studies is provided in Table II.
Discussion
The most prevalent symptoms of penile abscess, a
rare urological illness, are painful erections and localized penile
swelling. Although the causes of penile abscess vary, they are
often linked to injections, disseminated infections and penile
trauma. Furthermore, numerous occurrences of spontaneous penile
abscess are described without an underlying cause or inciting
event. Primary, secondary and idiopathic penile abscesses are
distinguished based on their etiology. While secondary abscesses
are associated with perianal, perineal, or intra-abdominal
abscesses and/or hematogenous diffusion, primary abscesses were
associated with intracavernosal injection, penile trauma and
iatrogenic causes (2). Physical
examinations occasionally reveal inguinal lymphadenopathy or
scrotal abscesses. As the etiology of penile abscess could be
linked to perianal abscess, digital rectal examination are
recommended to be performed methodically (28). Additionally, the presentation of
tuberculosis-related penile abscess is typically more progressive
and ‘silent’ (the presentation of tuberculosis-related penile
abscess is not easily noticeable or symptomatic until the condition
becomes more severe or advanced. It typically progresses without
clear or prominent symptoms until it reaches a more critical stage)
(29,30).
The variety of organisms cultivated from abscess
swabs reflect the diverse etiologies of penile abscess. The
following organisms have been isolated in various case reports:
Staphylococcus aureus, Escherichia coli, Mycobacterium
tuberculosis, Prevotella bivia, Streptococcus anginosus,
Streptococcus constellatus and Streptococcus
intermedius. The most frequently implicated species in penile
abscess, as reported by Dugdale et al (2) are Staphylococcus aureus,
Streptococcus, Bacteroides and Fusobacteria (2). Apart from infection, penile abscesses
are also associated with diabetes mellitus (16,20)
and other forms of immunosuppression due to steroid abuse (25). As demonstrated in a previous study,
it remains unclear whether the corpora cavernosa is resistant to
the hematogenous spread of infection (22). However, there have been a few
accounts, including one regarding a case in which the hematogenous
dispersion of dental caries was reported to result in penile
abscess (9,31). Of note, two distinct
microbiological scenarios have been identified. When abscesses have
a localized origin, the causative organisms are usually
skin-related (Staphylococcus aureus, Staphylococcus
epidermidis). Under certain conditions, these microbes act as
opportunistic pathogens, despite being part of the normal
microflora (2,5). By contrast, when no clear portal of
bacterial entry is identified, the primary pathogens originate from
dental commensal flora (9).
In the past, aspiration and clinical examination
served as the primary diagnostic methods for penile abscess.
However, with the advancement of medical technology, various
imaging modalities, such as CT scans, US and MRI, are utilized to
confirm the diagnosis (32). The
majority of studies included in the present systematic review
reported that MRI and US were used to evaluate penile abscess
cases. Among these, US served as the main imaging technique
(33), given its noninvasive
nature and the ability to perform bedside procedures including
simultaneous abscess drainage. When moderate cases were assessed
with extracranial doppler with color US, findings included
significant hyperemia of the cavernous bodies, thickened mucosa,
increased echogenicity of subcutaneous tissues and heterogeneous
hypoechoic areas. In severe cases, B-mode US has revealed anechoic
or hypoechoic collections with sediment and poorly defined margins
(34). CT scans, although less
frequently used due to radiation and low soft tissue contrast,
assist in drainage guidance, abscess localization and the
evaluation of adjacent structure involvement. When contrast agents
are administered, CT scans reveal fluid accumulation, occasional
air bubbles, perilesional fat edema and wall hyperemia. MRI, when
available, provides superior soft tissue contrast and allows for
surgical planning, tissue plane characterization, and the exclusion
of other pelvic or perineal infection foci. On an MRI, penile
abscesses exhibit a low signal intensity on T1-weighted images and
high signal intensity on T2-weighted images, with rim enhancement
following gadolinium administration (35). CT or MRI assess disease extension
to the perineum, abdominal wall, fascial planes and buttocks.
Nonetheless, it is suggested that the selection of imaging modality
should be tailored to individual cases due to the lack of consensus
on the most appropriate approach for this rare presentation.
Management options for penile abscess consist of
intravenous antibiotic therapy combined with either open surgical
incision and drainage (11) or
radiologically guided needle aspiration (32). Antibiotic therapy is ideally based
on culture and sensitivity results, although empirical therapy is
frequently initiated. Despite the appeal of conservative treatment,
the surgical approach, although invasive and associated with
complications, remains the primary choice due to the risk of
recurrence with incomplete evacuation (2). Surgical drainage is performed in
cases that develop spontaneously or are exacerbated by trauma,
disseminated infection, or failed conservative therapy. This
approach enables the simultaneous treatment of the abscess and its
underlying cause. Additionally, it allows surgeons to assess
anatomical damage (1).
Several studies reported the use of broad-spectrum
antibiotics as first-line therapy, particularly ceftriaxone,
vancomycin and piperacillin-tazobactam (2). These were often administered
intravenously and were selected based on either empirical judgment
or microbial culture results. Treatment duration ranged from 7 to
14 days in the majority of cases. However, due to the nature of
case reports, detailed dosing information was inconsistently
provided, limiting standardized interpretation of efficacy across
cases. However, some cases were successfully managed using less
invasive interventional techniques, such as image-guided aspiration
and antibiotics (16,20). Image-guided needle aspiration,
performed under local anesthesia, minimizes tissue trauma and
reduced the risk of postoperative complications like fibrosis
(32). Among these, US-guided
coaxial puncture and rinsing has emerged as a promising method
(3), owing to its simplicity,
cost-effectiveness and minimal equipment requirements. The
real-time monitoring capability of US enables the accurate
visualization of the abscess cavity throughout treatment. The
coaxial aspiration/flushing technique has proven to be particularly
effective for superficial subcutaneous abscesses. However, in cases
involving deep abscesses seen in preoperative imaging, this method
is deemed insufficient for complete evacuation and washout. Thus,
open incision and drainage remain the gold standard for thorough
debridement and concurrent pathology assessment (3,16,33).
Close post-operative monitoring is emphasized regardless of the
treatment method. For instance, Ehara et al (11) reported a case of a 54-year-old
patient who underwent open surgical drainage for a cavernosal
abscess; however, 3 weeks later, the patient developed a recurrent
abscess caused by methicillin-resistant Staphylococcus
aureus, requiring total penectomy
In addition to therapeutic strategies, several
underlying risk factors have been observed to increase patient
susceptibility to penile abscess. These include diabetes mellitus,
long-term immunosuppressive therapy, poor hygiene, sexually
transmitted infections and intracavernosal injections. Conditions,
such as uncontrolled diabetes and systemic immunosuppression may
compromise host defense mechanisms, allowing bacterial invasion and
abscess formation. The awareness and management of these risk
factors are essential for both prevention and early intervention
(1-4,6,12,15).
Post-operative complications, such as penile
curvature, fibrosis and erectile dysfunction have been reported,
although the majority of patients have been shown to regain normal
anatomy and erectile function. The present systematic review
identified secondary fibrosis and resultant penile deviation, as
well as erectile dysfunction as the most common sequelae. Compared
to US-guided aspiration, these complications occurred more
frequently following open surgical drainage. Consequently, some
patients required penile prosthesis or further surgical
intervention to manage these issues (22). In one case of cavernositis, the
patient presented within 36 h of symptom onset and did not
experience erectile dysfunction after drainage. This case, as
reported by Shamloul et al (24), suggested that early intervention
may preserve erectile function by limiting cavernosal necrosis and
fibrosis.
Erectile dysfunction remains a potential
complication, particularly in cases of delayed treatment or
surgical trauma (20). Although
its precise pathogenesis remains unclear, it is considered to
involve multiple mechanisms including fibrosis, penile curvature
and impaired vascular supply. In the majority of cases, fibrosis
and curvature do not require correction, although they could
significantly affect erectile quality (1). Additional contributors to erectile
dysfunction include impaired blood flow, nerve injury, hormonal
disturbances and tissue pathology (36). Venous occlusion and endothelial
dysfunction also play a role (37). Given the complex integration of
neurologic, vascular and hormonal systems required for erectile
function, further investigations are warranted to clarify the exact
mechanisms linking penile abscess to erectile dysfunction (38). Thus, further research and clinical
assessment are necessary to fully understand the specific
mechanisms of erectile dysfunction following a penile abscess.
The present systematic review represents, to the
best of our knowledge, the first comprehensive synthesis of
complications and outcomes associated with penile abscess.
Nonetheless, it was limited by the nature of the included
literature, which consisted entirely of case reports and case
series. Additionally, the restriction to English-language studies
reduced the pool of eligible publications. Conducting multicenter
research in this field remains challenging due to the clinical
complexity and rarity of such cases. The limited sample size also
constituted a major limitation of the present systematic
review.
In conclusion, in the present systematic review,
case reports on the clinical outcomes and complications of penile
abscesses were synthesized and analyzed. Although several
complications were reported, as reported in the included studies
generally demonstrated favorable clinical outcomes, despite the
inherent risk of postoperative complications. Early diagnosis and
prompt treatment remained the key to successful management.
Given the predominance of systemic antibiotics and
surgical drainage in current management, these modalities continue
to serve as a reliable therapeutic backbone. Broad-spectrum
antibiotics, such as ceftriaxone, vancomycin and
piperacillin-tazobactam are commonly used, either empirically or
guided by culture results. In the majority of the reported cases,
antibiotics were administered intravenously with a duration ranging
from 7 to 14 days, depending on the clinical response. However,
detailed information on dosage was inconsistently reported across
case studies, limiting definitive conclusions on optimal
therapeutic regimens. these modalities continue to serve as a
reliable therapeutic backbone. However, less invasive techniques,
such as image-guided aspiration, have exhibited encouraging results
in reducing postoperative complications and preserving erectile
function. Therefore, incorporating these approaches into clinical
decision-making may enhance patient outcomes and reduce the need
for extensive interventions. Patients should be closely monitored
post-operatively for adverse effects, particularly erectile
dysfunction and penile deviation, which were the most commonly
reported complications. These findings should be applied with
caution in clinical practice. As regards adverse effects, erectile
dysfunction and penile deviation were the most commonly reported
complications.
Additionally, the awareness of patient-specific risk
factors, such as diabetes mellitus, immunosuppressive conditions
and a history of intracavernosal injection, may help clinicians
identify vulnerable individuals and implement early preventative or
therapeutic measures.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
FFP, SS and RN conceived and designed the study. BS,
DHH and MHW were involved in the methods (search and selection).
FFP, RN and MHW were involved in the analysis of the results and
conclusions. SS and DHH were involved in manuscript preparation. FF
and RN confirm the authenticity of all the raw data. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Garcia C, Winter M, Chalasani V and Dean
T: Penile abscess: A case report and review of literature. Urol
Case Rep. 2:17–19. 2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Dugdale CM, Tompkins AJ, Reece RM and
Gardner AF: Cavernosal abscess due to streptococcus anginosus: A
case report and comprehensive review of the literature. Curr Urol.
7:51–56. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Yuan Y, Meng L, Wang R, Zhang Z, Yang J,
Zhang X, Xu J, Meng Y, Zhang W and Liu C: Ultrasound-guided
puncture and drainage for penile abscess: Case report and review of
the literature. Radiol Case Rep. 18:1796–1808. 2023.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Brennan J, O'kelly F and Quinlan DM: A
case of spontaneous abscess of the corpus cavernosum. Scand J Urol.
47:534–536. 2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kropman RF, de la Fuente RB, Venema PL and
van Imhoff WL: Treatment of corpus cavernosum abscess by aspiration
and intravenous antibiotics. J Urol. 150:1502–1503. 1993.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lee LT, Hon SA, Chuah J, Tee YJ and
Ibrahim SO: Spontaneous base of penile abscess successfully treated
by transperineal incision and drainage: A case report. Proceedings
of Singapore Healthcare. 31:2022.
|
|
7
|
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. BMJ. 372(n71)2021.PubMed/NCBI View
Article : Google Scholar
|
|
8
|
Chapter 7: Systematic reviews of etiology
and risk. In: JBI Manual for Evidence Synthesis. JBI, 2020.
|
|
9
|
Charles T, Roy C, Lang H, Jacqmin D and
Hansmann Y: Abscess of corpus cavernosum following a fellatio or a
periodontal infection. Curr Urol. 3:217–219. 2009.
|
|
10
|
Dempster NJ, Maitra NU, McAuley L, Brown M
and Hendry D: A unique case of penile necrotizing fasciitis
secondary to spontaneous corpus cavernosal abscess. Case Rep Urol.
2013(576146)2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ehara H, Kojima K, Hagiwara N, Phuoc NB
and Deguchi T: Abscess of the corpus cavernosum. Int J Infect Dis.
11:553–554. 2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Frank I and Lieber M: Gas containing
cavernous abscess secondary to an intra-abdominal abscess. J Urol.
162:1382–1383. 1999.PubMed/NCBI
|
|
13
|
Gore TC, Schepcoff A and Sorresso D:
Corpus cavernosum abscess secondary to traumatic perforation of
urethral diverticulum. Cureus. 12(e7032)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kyoshi Hidaka A, Murata Hayashi R, Chahade
Sibanto Simões G, Simões AGS and Paladino JR Jr: Corpus cavernosum
abscess: A case report. Urol Case Rep. 43(102118)2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Jinga V and Iconaru V: Penile abscess and
urethrocutaneous fistula following intracavernous injection: A case
report. J Sex Med. 9:3270–3273. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kachare M, Alamgir K and Mane N:
Periurethral abscess in corpus spongiosum diagnosed on
ultrasonography. J Med Ultrasound. 30:135–137. 2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kızılkan Y, Duran MB and Peşkircioğlu ÇL:
Penile abscess due to intracavernosal injection: A case report. J
Urological Surg. 5:214–216. 2018.
|
|
18
|
Lazarou L, Berdempes M, Markopoulos T,
Kostakopoulos N, Spyropoulos K and Mitsogiannis I: A case of
cavernosal abscess after neglected penile fracture and bacteremia.
Urol Ann. 11(328)2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Minagawa T, Kato H, Ogawa T, Uehara T and
Ishizuka O: Usefulness of sonourethrography for penile abscess as a
result of xanthogranulomatous granuloma in the corpus cavernosum of
an adult: A case report. Int J Urol. 22:788–790. 2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Moussa M and Abou Chakra M: Spontaneous
cavernosal abscess: A case report and review of literature. J Surg
Case Rep. 2019(rjz108)2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Paladino JR, Nascimento FJ, Gromatsky C
and Pompeo ACL: Corpus cavernosum abscess after Winter procedure
performance. BMJ Case Rep. 2014(bcr2013202089)2014.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Sagar J, Sagar B and Shah DK: Spontaneous
Penile (cavernosal) abscess: Case report with discussion of
aetiology, diagnosis, and management with review of literature.
ScientificWorldJournal. 5:39–41. 2005.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Sater AA and Vandendris M: Abscess of
corpus cavernosum. J Urol. 141(949)1989.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Shamloul R and Kamel I: Early treatment of
cavernositis resulted in erectile function preservation. J Sex Med.
3:320–322. 2006.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Tüzel E: Spontaneous corpus cavernosum
abscess in a healthy man using Long-term androgenic anabolic
steroids. World J Mens Health. 33:36–38. 2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Wang H, Dhar A and Wang A: Corpora
cavernosum abscess and corporoglanular fistula following penile
shunts for ischemic priapism. Urol Case Rep.
47(102341)2023.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Yamagishi A, Kurokawa M, Nishida H, Konno
T and Tsuchiya N: Prednisolone treatment is effective for an
idiopathic penile abscess: A case report and review. Am J Case Rep.
22(e933618)2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Weizberg M, Gillett BP and Sinert RH:
Penile discharge as a presentation of perirectal abscess. J Emerg
Med. 34:45–47. 2008.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Murali TR and Raja NS: Cavernosal cold
abscess: A rare cause of impotence. Br J Urol. 82:929–930.
1998.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Köksal T, Kadioğlu A, Tefekli A, Usta M,
Beşişik A and Erol B: Spontaneous bacterial abscess of bilateral
cavernosal bodies. BJU Int. 84:1107–1108. 1999.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Fernandez N, Chavarriaga J and Pérez J:
Complete corporeal preservation clitoroplasty: New insights into
feminizing genitoplasty. Int Braz J Urol. 47:861–867.
2021.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Thanos L, Tsagouli P, Eukarpidis T,
Mpouhra K and Kelekis D: Computed Tomography-guided drainage of a
corpus cavernosum abscess: A minimally invasive successful
treatment. Cardiovasc Intervent Radiol. 34:217–219. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Bertolotto M, Pavlica P, Serafini G, Quaia
E and Zappetti R: Painful penile induration: Imaging findings and
management. RadioGraphics. 29:477–493. 2009.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Roberto L, Silvestro C, Lucia D, Umberto
B, Antonella C and Daniele M: A rare case of a spontaneous abscess
of the corpus cavernosum: The role of contrast-enhanced ultrasound
in diagnosis and post-therapeutic follow-up. J Ultrasound.
24:567–572. 2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Kickuth R, Adams S, Kirchner J, Pastor J,
Simon S and Liermann D: Magnetic resonance imaging in the diagnosis
of Fournier's gangrene. Eur Radiol. 11:787–790. 2001.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Mirone V, Fusco F, Cirillo L and
Napolitano L: Erectile dysfunction: From pathophysiology to
clinical assessment. In: Practical Clinical Andrology. Springer
International Publishing, Cham, pp25-33, 2023.
|
|
37
|
Hsieh CH, Hsieh JT, Chang SJ, Chiang IN
and Yang SSD: Penile venous surgery for treating erectile
dysfunction: Past, present, and future perspectives with regard to
new insights in venous anatomy. Urol Sci. 27:60–65. 2016.
|
|
38
|
Chaudhari F, Ali A and Balyan P:
Mechanisms and therapeutic opportunities in erectile dysfunction
for advanced glycation end products (AGEs). J Exp Clin Med.
40:390–400. 2023.
|