Introduction
Hydatid disease (HD), caused by the larval stage of
the tapeworm Echinococcus granulosus, is a zoonotic
infection with a diverse range of clinical presentations (1). Dogs are the definitive hosts of
Echinococcus granulosus, while livestock and rodents serve
as intermediate hosts. Humans can become incidental hosts when they
are infected by ingesting the eggs of Echinococcus species
(1,2). The lungs and liver are the most
commonly affected organs. However, extrapulmonary involvement can
occur in various locations due to the ability of the parasite to
disseminate through the hematogenous route. Uncommon sites of
involvement include the kidneys, pancreas, heart, brain, bones,
muscles, orbits, peritoneal cavity, chest wall, urinary bladder,
neck, thyroid and parotids (3-7).
The breasts are an exceptionally rare site for HD. Breast hydatid
cysts (BHCs) are unusual even in regions endemic for
Echinococcosis, where they represent only 0.27% of all HC
cases (1,2). Due to its low prevalence and mimicry
of more frequent breast pathologies, the diagnosis of BHC is
challenging (8).
In accordance with the CaReL guidelines (9), the present study describes the case
of an elderly female patient who presented with a longstanding BHC
masquerading as a slowly enlarging, painless mass.
Case report
Patient information
A 79-year-old female patient presented to Smart
Health Tower, Sulaymaniyah, Iraq) with a palpable, painless, slowly
enlarging lump in her left breast that had been present for the
past 20 years. She was multiparous with no history of smoking, and
her past medical and surgical histories were negative. She had no
fever, weight loss, night sweats, or chest pain. She resided in an
urban area, but had a history of having a pastoral lifestyle for a
number of years (>10 years) with daily close contact with
various farm animals, including sheep and cattle.
Clinical findings
Upon a physical examination, a palpable, non-tender,
well-defined, freely mobile mass was found in the lateral central
part of the left breast, ~40 mm in diameter. The physical
examination did not reveal any other notable findings.
Diagnostic assessment
A breast ultrasound (U/S) revealed (images not
available) a heterogeneous mass with internal layering and
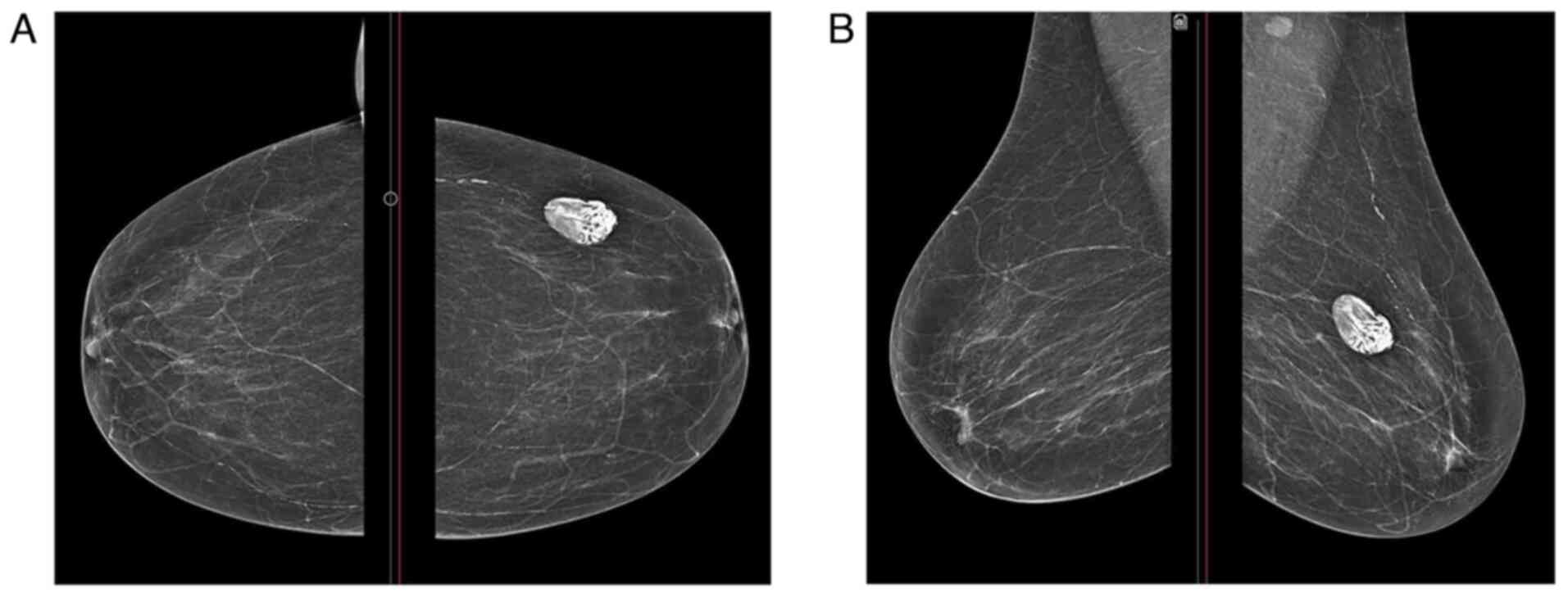
calcification, but no vascularity. A mammography (MMG) revealed a
circumscribed, hyperdense mass, measuring 35x23 mm, in the lateral
central part of the left breast. The radiological features were
suggestive of a calcified HC. The mammogram classified the mass as
BI-RAD 2 (Fig. 1). Based on
radiological findings and to minimize costs for the patient,
magnetic resonance imaging (MRI) and serology were not
performed.
Therapeutic intervention
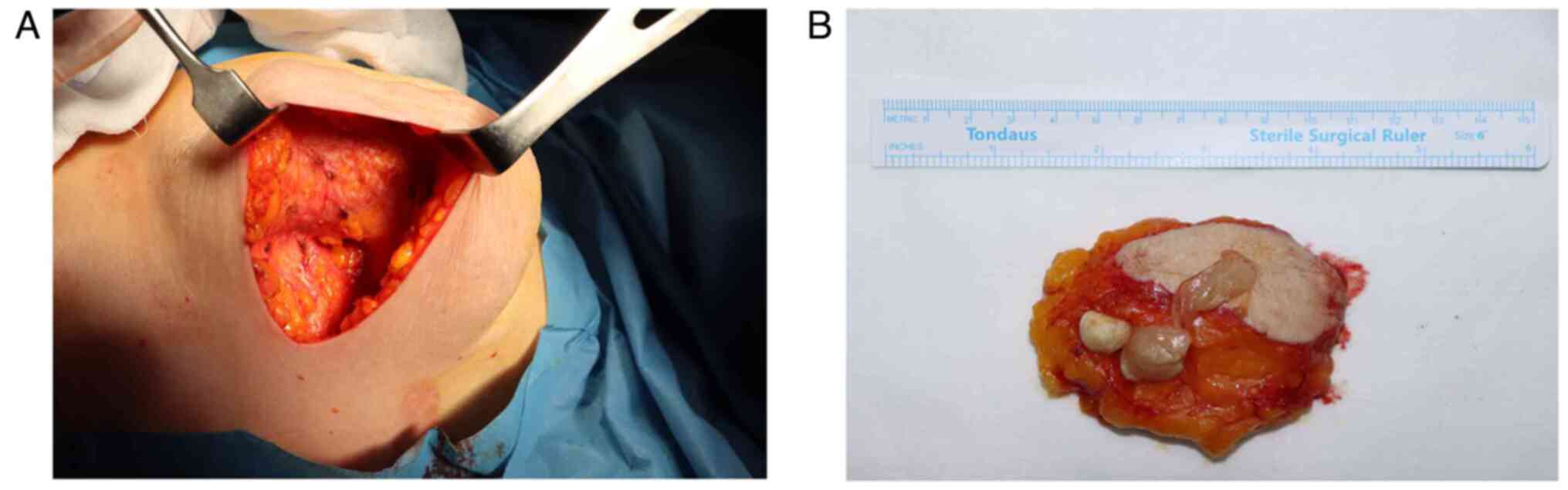
The patient underwent surgery to excise the mass.
The skin overlying the mass was marked for an elliptical incision.
The mass was then identified and carefully dissected free from the
surrounding breast tissue. Great care was taken to ensure the
complete excision of the mass, while avoiding the rupture of the
cyst wall. Hemostasis was achieved throughout the dissection using
electrocautery. The entire mass was removed intact without the
spillage of the contents of the cyst. The surgical cavity was
irrigated with sterile saline to remove residual debris (Fig. 2A). A drain was deemed unnecessary
due to the absence of visible bleeding and a clean surgical field.
The wound was closed in layers with absorbable sutures, followed by
the closure of the skin incision with subcuticular sutures for an
optimal cosmetic outcome. The cyst was ruptured during
post-resection manipulation (Fig.
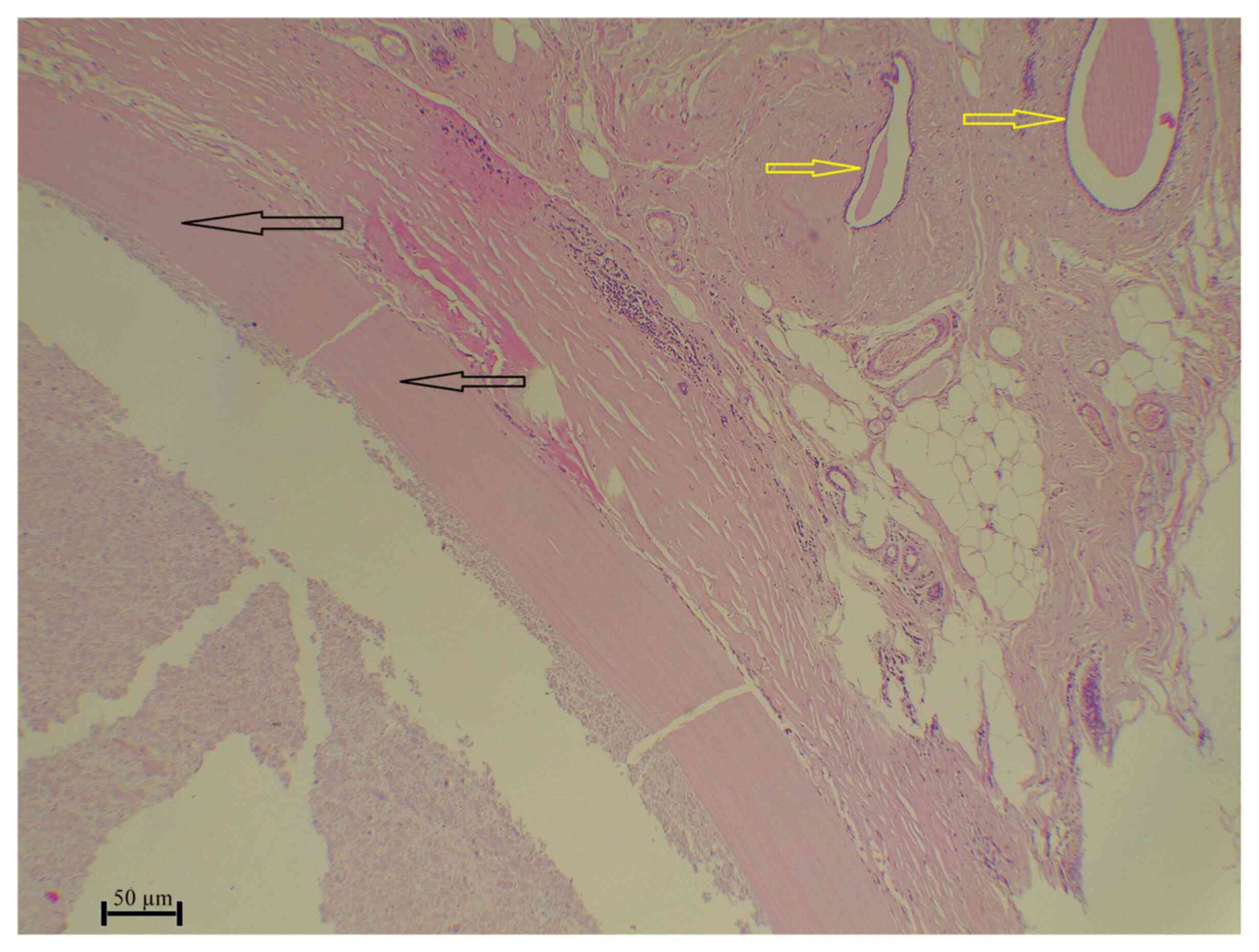
2B). A histopathological examination was performed on
5-µm-thick sections which were paraffin-embedded. The sections were
then fixed in 10% neutral-buffered formalin at room temperature for
24 h and stained with hematoxylin and eosin (H&E; Bio Optica
Co, Italy) for 1-2 min at room temperature. The sections were then
examined under a light microscope (Leica Microsystems GmbH). This
examination revealed benign breast ducts and lobules in a fibrous
stroma surrounding a well-defined cyst composed of an outer fibrous
layer and an inner lamellated, chitinous layer with calcification
and mixed inflammatory cell infiltration. This confirmed the
diagnosis of a calcified BHC (Fig.
3).
Follow-up and outcome
The post-operative period was uneventful, and the
patient reported no wound complications (Fig. 4). A U/S examination at the 4-month
follow-up (images not available) revealed no evidence of
recurrence.
Discussion
Echinococcus is a genus of tapeworms that
cause a parasitic disease in humans and animals known as
echinococcosis. Cystic echinococcosis is the most common of the
four main types of the disease, also known as HD. The larval stage
of Echinococcus granulosus is responsible for causing HD
(8). It is an endemic disease in a
number of areas, including the Mediterranean, South America, North
and East Africa, the Middle East, China, Australia and Russia
(10). It is primarily observed in
places where sheep and cattle are raised (11).
The Echinococcus life cycle requires a
definitive host and an intermediate host. Humans can become
intermediate hosts (8) when they
become accidentally infected by ingesting the eggs of the parasite,
which are shed in the feces of infected dogs (12). This can occur through close contact
with infected dogs, particularly when handwashing is omitted
following direct contact or when contaminated food or water is
ingested. The ingested eggs travel to the human intestines, where
they hatch and release oncospheres (1). These embryos then migrate through the
bloodstream to different organs, most commonly the liver (in 75% of
cases) and lungs (in 15% of cases), followed by other organs (in
10% of cases) (3,13). The embryos develop into HCs in
these organs, which can grow slowly over the years. The most
probable route for disseminating HD is the bowel lymphatics into
the systemic bloodstream (14).
The lymphatic pathways between the liver and breast
(Gerota's pathway) are a possible route for breast involvement by
HD (14). Herein, following a
literature review, it was found that the reported cases mostly
occurred between the ages of 30 and 50 years, usually presenting
with a history of a painless, slowly enlarging breast mass
(3,12,13).
A literature review was conducted to identify relevant reports on
BHC, filtered by the well-known predatory lists (15). The process involved a Google
Scholar search employing the ‘breast hydatid cyst’ as a key word.
In total, 13 reports on BHCs were identified from 2021 to 2024, of
which 11 reports were summarized in the present study (2,8,16-24).
Among these, rural residency was reported in 3 cases, with an age
range of 18 to 75 years and a mean age of 37.6 years. The majority
of these cases (90.9%) presented with a breast lump (Table I). In their systematic review,
Mutafchiyski et al (14)
reported that in a total of 52 cases of BHC, the duration of the
presentation ranged from 4 months to 19 years. The majority of
cases involved a single cyst, with only 2 cases having multiple
cysts (14). In a case series,
Tavakoli et al (10)
described 6 cases with symptom durations ranging from 8 months to 3
years, while Koc et al (13) reported a case with a longstanding
history before presentation, a finding similar to the case
presented herein. Among the reviewed cases that specified the
duration of presentation, this ranged from 2 to 36 months, with a
mean of 15.4 months. The left breast was the most frequently
affected side (72.7%), and the upper quadrant was the most commonly
involved region (54.5%). In the patient in the present case report,
the lesion was located in the lateral central portion of the left
breast.
 | Table ISummary of 11 case reports on breast
hydatid cysts in females from 2021 to 2024 identified in the
literature. |
Table I
Summary of 11 case reports on breast
hydatid cysts in females from 2021 to 2024 identified in the
literature.
| | Pre-operative
assessment | |
|---|
| First author | Country, year of
publication | Age, years | Laterality | Presen tation | Duration
(months) | Residency | Radiology | Location | Size (cm) | Axillary
lymphadenopathy | Biopsy | Other involved
organs | Management | Follow-up | Outcome | (Refs.) |
|---|
| Kassahun
Tadele | Ethiopia, 2022 | 18 | Left | Painless breast
lump | 24 | Rural | U/S | UQ | 5.5 | No | Granulo matous
inflammation | No | Surgery and
postoperative albendazole | 6 months | No recurrence | (2) |
| Al Sharei | Jordan, 2023 | 38 | Bilateral | Painless breast
lump | 2 | Rural | U/S, MMG | UOQ, upper
central | 2.3 | No | No | Liver | Pre-operative
albendazole and surgery | 3 months | No recurrence | (8) |
| Mesfin | Ethiopia, 2023 | 28 | Left | Breast pain | 12 | NA | U/S | LOQ | 3.8 | NA | No | No | Pre-operative
albendazole and surgery | NA | NA | (16) |
| Samsami | Iran, 2021 | 31 | Left | Painless breast
lump | 24 | NA | U/S | Axillary tail | 5 | NA | No | No | Surgery and
post-operative albendazole | One year | No recurrence | (17) |
| Alareqi | Yemen, 2021 | 23 | Left | Breast lump | 3 | NA | U/S, MMG | UOQ | 2.9 | Yes | Hydatid cyst | No | Albendazole and
antibiotics | NA | NA | (18) |
| Abu-Mandeel | Jordan, 2023 | 38 | Left | Painless breast
lump | 7 | NA | U/S, MMG | UOQ | 3.2 | No | No | Liver | Surgery and
post-operative albendazole | NA | No recurrence | (19) |
| Dattal | India, 2023 | 75 | Right | Painless breast
lump | NA | NA | U/S, MMG | Retro-areolar | 4 | No | Cellular
debris | No | Surgical
excision | NA | NA | (20) |
| Ines | Tunisia, 2022 | 50 | Left | Painless breast
lump | Few
yearsa | Rural | U/S, MMG, MRI | LQ | 7 | No | No | No | Pre-operative
albendazole and surgery | 6 months | No recurrence | (21) |
| Assefa | Ethiopia, 2022 | 28 | Left | Painless breast
lump | NA | NA | U/S | UOQ | 3.4 | No | Hydatid cyst | No | Surgical
excision | NA | NA | (22) |
| Mahmood | Pakistan, 2023 | 50 | Left | Painless breast
lump | 36 | NA | U/S, MMG | UOQ | 3.5 | No | Hydatid cyst | Liver | Albendazole | Lost to
follow-up | NA | (23) |
| Sharma | India, 2021 | 35 | Right | Painless breast
lump | NA | NA | U/S, MMG | NA | 4.2 | No | Simple cystic
lesion | No | Surgical
excision | NA | NA | (24) |
BHC can mimic a simple cyst, fibroadenoma, phyllodes
tumor, chronic abscess, or cancer (8,12).
Fibroadenomas have an excellent prognosis with minimal malignant
potential and may even regress spontaneously (25). BHC also exhibits a benign course
following resection; however, follow-up is recommended to monitor
for recurrence (26). By contrast,
breast carcinoma has a stage-dependent prognosis, with the 5-year
survival >99% in localized disease, yet decreasing to ~87% with
regional spread and ~32% with metastasis (27).
Generally, HC is an essential consideration in the
differential diagnosis of a palpable breast mass, particularly in
individuals from regions where HD is endemic (2). Therefore, a triple assessment is
valuable for excluding malignancy in any breast mass, including a
comprehensive history and physical examination, radiological
imaging and histopathological analysis (28). Clinically, HC appears as a firm,
mobile, often painless lump of variable size with a regular border
(1). Imaging may be helpful in the
diagnosis of breast HD, although it is usually not conclusive
(1,12). Breast U/S is the method of choice
for evaluating this type of cystic lesion. It has a sensitivity of
88-98% and a specificity of 95-100% (8,10).
Breast U/S can indicate a well-defined, sometimes lobulated mass
with mixed internal echoes, potentially containing both cystic and
solid areas. According to the classification presented in the study
by Gharbi et al (29), five
ultrasonographic features have been described: An uninoculated pure
fluid collection (type I); a fluid collection with a split wall
(type II); a multi-vesicular, multiseptated cyst with daughter
cysts (type III); a mass with a heterogeneous echo pattern (type
IV); and a mass with reflecting thick walls (type V). Types II and
III HC have more specific diagnostic imaging features than the
other types. MMG may illustrate a non-specific, well-circumscribed,
round, or oval-shaped mass with internal ring-shaped structures
(1). Calcifications within the
cyst wall or daughter cysts may be visualized (20). Upon imaging, the case in the
present study was found to have type IV features (a mass with a
heterogeneous echo pattern) according to the classification
presented in the study by Gharbi et al (29). However, fibroadenomas typically
appear as well-circumscribed, oval, or lobulated masses with
smooth, sharp margins on mammography and as uniformly hypoechoic,
circumscribed lesions on ultrasound (25). By contrast, invasive breast
carcinomas typically present as irregular or spiculated
high-density masses (often accompanied by microcalcifications) on
MMG and as angular, non-parallel hypoechoic lesions with posterior
acoustic shadowing on ultrasound (30,31).
A breast MRI can be a helpful tool for the diagnosis
of HC in the breast (13), as it
can provide more detailed information about the size, location and
characteristics of the cyst. A well-defined cystic lesion with a
smooth wall, perilesional edema (fluid build-up around the cyst),
daughter cysts (smaller cysts within the larger cyst), T1
hypo-intensity (dark signal on T1-weighted images), T2
hyperintensity (bright signal on T2-weighted images) and peripheral
rim enhancement (increased uptake of contrast dye along the rim of
the cyst) are the MRI findings that are suggestive of an HC
(10,20). Notably, these findings are not
specific to HCs and can also be observed in other breast lesions
(13). The results of a breast MRI
need to be interpreted in conjunction with other clinical
information, such as the medical history of the patient and the
results of the physical examination, in order to ensure an accurate
diagnosis. In their systematic review, Mutafchiyski et al
(14) reported that MRI was used
as a diagnostic modality in only a few cases. Among the 11 reviewed
cases in the present study, only 1 case had undergone a breast MRI
(21).
Fine needle aspiration cytology was previously
considered controversial in the pre-operative diagnosis of HC in
the case that the U/S examination suggested the disease, as it may
lead to spillage and anaphylactic reaction (10,24).
Recent literature, however, has concluded that the procedure may be
safe, fast and inexpensive (2,12,32).
The microscopic identification of the scolices or hooklets in the
fluid is required for the diagnosis (12,14).
Serological tests can be used for diagnosis, screening and
post-operative follow-up, including enzyme-linked immunosorbent
assay (ELISA), hydatid immunoelectrophoresis, latex agglutination
and an indirect hemagglutination test. The sensitivity of ELISA
ranges from 80-100%, and its specificity ranges from 88-96% for
hepatic cysts. The sensitivity of the test ranges from 50 to 56%
for lung HD and from 25 to 65% for HD of other organs (4). Since serological tests demonstrate
variable sensitivity in diagnosing HCs at different anatomical
sites, the development of a rapid and reliable serological assay
for extrapulmonary HC remains necessary (33). Therefore, U/S, MRI or MMG may help
rule out the presence of HC in the breast (13,21),
as in the case in the present study.
Surgical intervention, puncture aspiration injection
and re-aspiration, a ‘watch and wait’ approach, and chemotherapy
are the main treatment options for HC (4,8).
However, complete surgical excision is the best diagnostic and
therapeutic approach (14). By
contrast, fibroadenomas are usually observed or removed by local
excision if large or symptomatic, while invasive carcinomas require
oncologic surgery, often with additional radiotherapy,
chemotherapy, or hormonal therapy depending on stage and tumor
biology (25,34).
A definitive diagnosis of HC is often achieved
through a post-operative histopathological examination (8). HCs have a multilayered wall composed
of a laminated membrane and a germinal layer that produces
protoscoleces and daughter vesicles, typically accompanied by
surrounding fibrosis and inflammation (26). However, fibroadenomas are benign,
well-circumscribed tumors of stromal and ductal elements with
intact myoepithelial lining and no atypia (25). Breast carcinomas exhibit malignant
invasion beyond the basement membrane, characterized by nuclear
pleomorphism, increased mitotic activity, and disorganized growth
patterns (34). Preoperative
chemotherapeutic agents, such as albendazole, can reduce the
postoperative recurrence rate (2,3),
which ranges from 2 to 25% (3).
However, among the cases reviewed herein, only 3 cases used
pre-operative albendazole (8,16,21).
The mortality rate due to echinococcosis is very low, ranging
between 0.29 to 0.6% (4). Complete
surgical excision with intact borders followed by a course of
albendazole was the favored treatment in many studies (1,2,8,25).
Of the cases reviewed herein, 4 cases were administered
post-operative albendazole (2,17-19).
The current case underwent the complete surgical excision of the
cyst without postoperative complications. Histopathological
examination confirmed BHC. Following a 4-month follow-up, no
recurrence was reported. Further studies with larger sample sizes
and more robust designs are warranted to elucidate the mechanisms
underlying BHC occurrence.
In conclusion, BHC can remain asymptomatic for a
long period of time and may masquerade as a gradually enlarging,
painless breast mass.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
AMS and SHH were major contributors to the
conception of the study, as well as to the literature search for
related studies. HOAb, SL and BOH were involved in the literature
review, in the conception of the study and in the writing of the
manuscript. HOAl, KAA, RMA, FHF and SMA were involved in the
literature review, in the design of the study, in the critical
revision of the manuscript, and in the processing of the table and
figures. LRAP was the radiologist who performed the assessment of
the case. AMA was the histopathologist who performed the diagnosis
of the case. AMS, SL, BOH and HOAl were involved in the management
and monitoring of the case. AMS and SHH confirm the authenticity of
all the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for her participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
El Moussaoui K, Lakhdar A, Baidada A and
Kherbach A: Hydatid cyst of the breast: Case report. Int J Surg
Case Rep. 77:325–328. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kassahun Tadele A, Israel Korga T, Melis
Nisiro A and Abebe Ayele S: Rare case report on hydatid cyst of
breast. Pathol Lab Med Int. 14:33–36. 2022.
|
|
3
|
Cancelo MJ, Martín M and Mendoza N:
Preoperative diagnosis of a breast hydatid cyst using fine-needle
aspiration cytology: A case report and review of the literature. J
Med Case Rep. 6(293)2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sachar S, Goyal S and Sangwan S: Uncommon
locations and presentations of hydatid cyst. Ann Med Health Sci
Res. 4:447–452. 2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Hussein DM, Kakamad FH, Amin BJ, Baqi DH,
Tahir SH, Salih AM, Ali RK, Fattah FH, Ahmed GS, Abdalla BA, et al:
Hydatid cyst in the pulmonary artery; a meta-analysis. Barw Med J.
1:8–13. 2023.
|
|
6
|
Baba HO, Salih AM, Abdullah HO, Hassan HA,
Ali RK, Kakamad FH, Salih RQ and Hussein S: Primary hydatid cyst of
the posterior neck; a case report with literature review. Int J
Surg Open. 40(100449)2022.
|
|
7
|
Ali RM, Hawramy OHG, Esmaeil DA, Gharib
DT, Tahir SH, Ahmed DH, Ali AHH, Hussein KFH, Ali RE, Abdalla BA,
et al: Primary pancreatic hydatid cyst: A case report and a brief
review of the literature. World Acad Sci J. 6(49)2024.
|
|
8
|
Al Sharei A, Abu-Jeyyab M, Al-Khalaileh M,
Al-Awabdeh M, Al-Asbahi H, Al-Dwairy S and Al-Share M: Bilateral
hydatid cyst of the breast: A case report and review of the
literature. Ann Med Surg (Lond). 85:2981–2984. 2023.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Prasad S, Nassar M, Azzam AY,
García-Muro-San José F, Jamee M, Sliman RKA, Evola G, Mustafa AM,
Abdullah HQ, Abdalla B, et al: CaReL guidelines: A consensus-based
guideline on case reports and literature review (CaReL). Barw Med
J. 2:13–19. 2024.
|
|
10
|
Tavakoli M, Rastegar YF, Laein AF and
Farrokh D: Hydatid cyst of the breast: A case series and review of
the literature. Iran Red Crescent Med J. 20(e29972)2018.
|
|
11
|
Abdullah HO, Abdalla BA, Mohammed-Saeed
DH, Tahir SH, Fattah FH, Hassan SJ, Hamasalih HM, Amin BJH, Salih
AM, Noori SS, et al: A comprehensive study of pericardial hydatid
cyst: Systematic review and meta-data presentation. Barw Med J.
1:14–23. 2023.
|
|
12
|
Kumar A, Gaurav K, Chandra G, Tiwary AK,
Bhagat S and Sarawgi M: A rare case of isolated hydatid cyst of
breast. Int J Surg Case Rep. 7:115–118. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Koc A, Sarici IS, Vurdem UE, Karabiyik O
and Gumus UO: Unusual presentation of hydatid cyst in breast with
magnetic resonance imaging findings. Case Rep Med.
2017(6237435)2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Mutafchiyski VM, Popivanov GI, Tabakov MS,
Vasilev VV, Kjossev KT, Cirocchi R, Philipov AT, Vaseva VS,
Baitchev GT, Ribarov R and Konaktchieva MN: Cystic echinococcosis
of the breast-diagnostic dilemma or just a rare primary
localization. Folia Med (Plovdiv). 62:23–30. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Abdullah HO, Abdalla BA, Kakamad FH, Ahmed
JO, Baba HO, Hassan MN, Bapir R, Rahim HM, Omar DA, Kakamad SH, et
al: Predatory publishing lists: A review on the ongoing battle
against fraudulent actions. Barw Med J. 2:26–30. 2024.
|
|
16
|
Mesfin T, Sahiledengle B, Taha M, Nigusu
F, Seyoum K, Geta G, Ejigu N, Zenbaba D, Gomora D, Beressa G, et
al: Isolated breast hydatid cyst: A case report. Clin Case Rep.
11(e8183)2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Samsami M, Qaderi S, Bagherpour JZ and
Lucero-Prisno DE III: A case report of primary isolated
extrahepatic hydatid cyst of the soft tissues of the breast and
thigh. Int J Surg Case Rep. 79:475–478. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Alareqi AA, Alshoabi SA, Alhazmi FH, Hamid
AM, Alsharif WM and Gameraddin MB: A rare phenotype of breast
hydatid cyst causing misdiagnosis and unnecessary intervention: A
case report. Radiol Case Rep. 16:3226–3230. 2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Abu-Mandeel E, Mahmoud MM and Azizieh O:
The ‘serpent sign’-A classical sign in a nonclassical location: A
case report of breast hydatid cyst. Radiol Case Rep. 18:1329–1333.
2023.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Dattal D, Mardi K, Sharma M and Chandran
A: Primary hydatid cyst of the breast: A rare cause of breast lump.
Ann Breast Dis. 1:30–32. 2023.
|
|
21
|
Ines M, Mariem BL, Marwa M, Amina BS and
Chiraz H: Isolated breast hydatid cyst: Imaging features. Clin Case
Rep. 10(e6362)2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Assefa W, Dessalegn M, Admassu S and Molla
B: Breast hydatid cyst presented as a fluctuant painless lump
mimicking galactocele: A case report. Int J Infect Dis.
125:228–230. 2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Mahmood S and Mahmood R: Pre-operative
diagnosis of hydatid cyst in the breast: A case report of a rare
entity and review of literature. J Pak Med Assoc. 73:1530–1532.
2023.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Sharma N, Sharma RA and Sharma S: Case
report: Hydatid cyst in breast. Indian J Surg. 83 (Suppl
2):S523–S524. 2021.
|
|
25
|
Ajmal M, Khan M and Van Fossen K: Breast
Fibroadenoma. In: StatPearls. StatPearls Publishing, Treasure
Island, FL, 2025.
|
|
26
|
Bannour B, Romdhani M, Chiba D, Bannour I,
Abdelkader AB, Mokni M and Boughizane S: Isolated hydatid cyst of
the breast: A rare pseudotumor of the breast. Eur J Breast Health.
21:182–185. 2025.PubMed/NCBI View Article : Google Scholar
|
|
27
|
American Cancer Society. Survival Rates
for Breast Cancer. American Cancer Society, Atlanta, 2025.
Available from: https://www.cancer.org/cancer/types/breast-cancer/understanding-a-breast-cancer-diagnosis/breast-cancer-survival-rates.html.
|
|
28
|
Sozutok S, Kaya O, Akkaya H and Gulek B: A
rare lesıon of breast: Hydatıd cyst. Malawi Med J. 34:68–70.
2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Gharbi HA, Hassine W, Brauner MW and
Dupuch K: Ultrasound examination of the hydatic liver. Radiology.
139:459–463. 1981.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Jones KN, Guimaraes LS, Reynolds CA, Ghosh
K, Degnim AC and Glazebrook KN: Invasive micropapillary carcinoma
of the breast: Imaging features with clinical and pathologic
correlation. AJR Am J Roentgenol. 200:689–695. 2013.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Gaillard F, Knipe H and Ashraf A: Benign
and malignant characteristics of breast lesions at ultrasound.
Available from: https://doi.org/10.53347/rID-1014. Accessed at Aug 31,
2025.
|
|
32
|
Abdullah AM, Rashid RJ, Tahir SH, Fattah
FH, Hama JI, Abdullah HO, Kakamad SH, Kakamad FH and Abdalla BA:
Diagnosis of a pulmonary hydatid cyst by fine needle aspiration: A
case report with literature review. Ann Med Surg (Lond).
86:552–555. 2023.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Tamarozzi F, Silva R, Fittipaldo VA,
Buonfrate D, Gottstein B and Siles-Lucas M: Serology for the
diagnosis of human hepatic cystic echinococcosis and its relation
with cyst staging: A systematic review of the literature with
meta-analysis. PLoS Negl Trop Dis. 15(e0009370)2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Menon G, Alkabban FM and Ferguson T:
Breast Cancer. In: StatPearls. StatPearls Publishing, Treasure
Island, FL, 2025.
|