Introduction
Granulomatous mastitis (GM) is a rare, benign,
chronic inflammatory breast disease (1). It is characterized histologically by
lymphocytes, plasma cells, epithelioid histiocytes, and
multinucleated giant cells, with the formation of non-caseating
granulomas and abscesses (2,3). Its
incidence is estimated at 2.4 cases per 100,000 females in the USA.
GM is most commonly observed in premenopausal women during or after
pregnancy, though it can also occur in nulliparous women. Reported
cases span a wide age range, from as young as 11 years to patients
in their 60s, 70s and even 80s (2,4,5).
GM is generally divided into two etiological types:
Idiopathic and secondary. Idiopathic GM has no clearly identified
cause, although an autoimmune mechanism is strongly suggested,
given its favorable response to corticosteroids and its links with
other autoimmune conditions. Secondary GM, on the other hand,
arises from specific underlying factors, including infectious
agents, such as Mycobacterium tuberculosis, fungi,
parasites, or bacteria, as well as systemic illnesses such as
sarcoidosis and granulomatosis with polyangiitis (6,7).
The clinical diagnosis of GM requires careful
evaluation, as it can be easily mistaken for other conditions, such
as non-puerperal mastitis, breast abscess, or, more commonly,
carcinoma (8). GM may also be
associated with systemic manifestations, including erythema nodosum
(EN), which is the most common form of panniculitis, an
inflammatory disorder of the subcutaneous fat characterized by
erythematous, tender nodules that typically appear on the anterior
aspect of the lower extremities. It has been linked to autoimmune
conditions, such as sarcoidosis and inflammatory bowel disease
(9,10). However, the coexistence of GM and
EN is exceedingly rare, with only limited documentation in the
literature regarding clinical features and therapeutic approaches
(11). Given this rarity, the
present case report aimed to add to the available evidence by
describing a patient with concurrent GM and EN. The present case
report follows the CaReL guidelines, and all cited references were
reviewed for eligibility and relevance (12,13).
Case report
Patient information
A 37-year-old female patient presented to Smart
Health Tower (Sulaymaniyah, Iraq) with a 2-month history of a
painful left breast mass, accompanied by painful bilateral skin
lesions on the lower limbs. She was a non-smoker with no prior
medical or surgical history and no significant family medical
history. The patient had 6 children, with a cumulative lactational
history of ~12 years
Clinical findings
A physical examination revealed a tender mass in the
left breast, accompanied by multiple tender, erythematous
subcutaneous nodules on the lower legs, thighs, and, to a lesser
extent, the buttocks (Fig. 1).
Diagnostic approach
Laboratory investigations revealed leukocytosis and
hypochromic microcytic anemia. The anti-streptolysin O (ASO) titer
and chest X-ray findings were within normal limits, and the
interferon-gamma release assay (IGRA) result was negative (Table I). A breast ultrasonography (US)
was performed, followed by a core biopsy to establish the
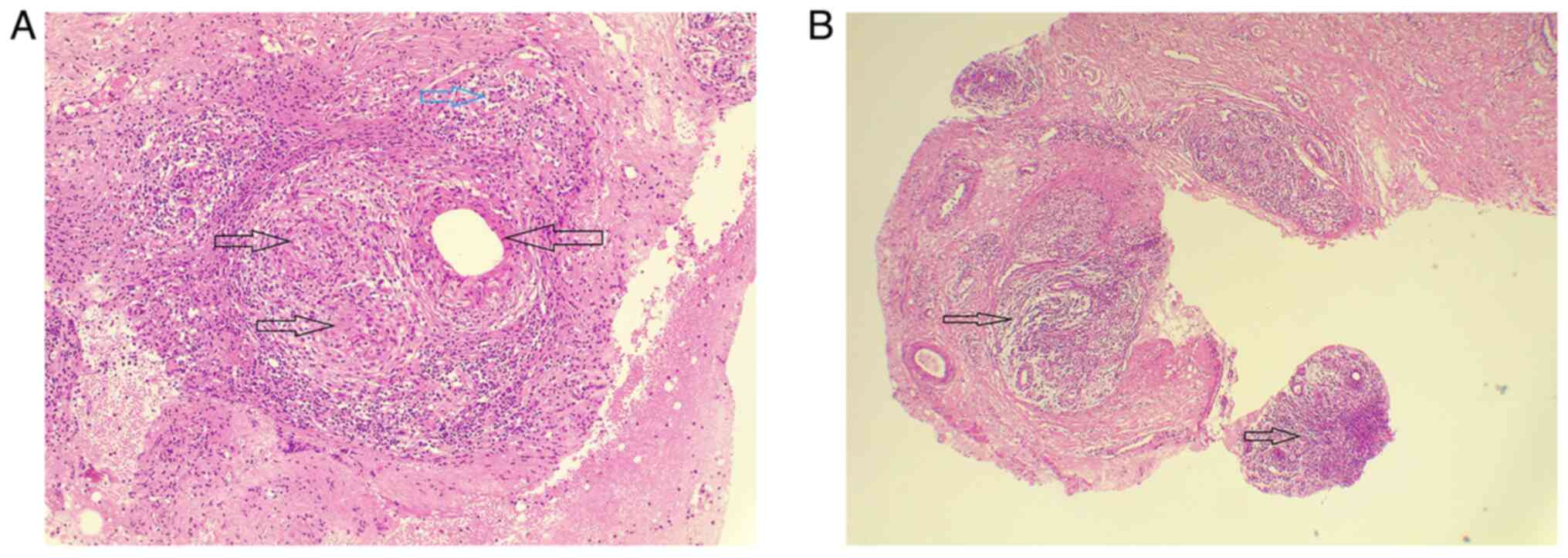
diagnosis. A histopathological examination (HPE) was performed by
the laboratory, as follows: The sections (5-µm-thick) were
paraffin-embedded and fixed with 10% neutral-buffered formalin at
room temperature for 24 h. They were then stained with hematoxylin
and eosin (H&E; Bio Optica Co.) for 1-2 min at room
temperature. The sections were then examined under a light
microscope (Leica Microsystems GmbH). The HPE revealed
non-caseating granulomas with epithelioid cells and multinucleated
giant cells, consistent with GM. Based on the clinical and
histological correlation, GM was identified as the underlying cause
of EN (Fig. 2).
 | Table ILaboratory test results with reference
ranges. |
Table I
Laboratory test results with reference
ranges.
| Test name | Result | Unit | Normal range |
|---|
| Complete blood
count | | | |
|
White blood
cell count | 12.5 | 109/l | 4-11 |
|
Lymphocytes | 2.0 | 109/l | 1-3.5 |
|
Lymphocyte
percentage | 16.3 | % | 15-45 |
|
Monocytes | 1.7 | 109/l | 0.2-1.5 |
|
Monocyte
percentage | 14.1 | % | 2-15 |
|
Granulocytes | 8.8 | 109/l | 2-7.5 |
|
Granulocyte
percentage | 69.6 | % | 40-80 |
|
Red blood
cell count | 4.34 |
1012/l | 3.8-5 |
|
Hemoglobin | 11.0 | g/dl | 11.5-15.5 |
|
Hematocrit | 34.3 | % | 36-46 |
|
Mean
corpuscular volume | 79.2 | fl | 80-100 |
|
Mean
corpuscular hemoglobin | 25.5 | pg | 27-32 |
|
Mean
corpuscular hemoglobin concentration | 32.2 | g/dl | 32-36 |
|
Red cell
distribution width | 50.8 | fl | 30-150 |
|
Red cell
distribution width percentage | 11.6 | % | 11-99.9 |
|
Platelet
count | 413 | 109/l | 150-400 |
|
Mean
platelet volume | 8.5 | fL | 7-11 |
|
Platelet
distribution width | 11.9 | fL | 0.1-99.9 |
|
Procalcitonin | 0.35 | % | 0.01-9.99 |
|
Ferritin,
serum | 33.6 | Ng/ml | 13-150 |
|
IGRAs-QuantiFERONE(R)- TB Gold Plus | | | |
|
Nil | 0.04 | IU/ml | |
|
TB1 minus
Nil | 0.0 | IU/ml | |
|
TB2 minus
Nil | 0.0 | IU/ml | |
|
Mitogen
minus Nil | 8.91 | IU/ml | |
| Interpretation
result | Mycobacterium
tuberculosis infection NOT likely |
| Anti-streptolysin
O | 56 | IU/ml | 0-200 |
Therapeutic interventions
The patient was commenced on prednisolone 30 mg
orally once daily and colchicine 0.5 mg twice daily, resulting in
the complete resolution of EN within 4 weeks.
Follow-up
At the 7-month follow-up, the patient exhibited a
complete clinical improvement, with full resolution of the EN
lesions.
Discussion
In 1972, Kessler and Wolloch (14) described the first case of GM,
emphasizing that its clinical features can closely resemble those
of breast cancer. Such features include palpable masses, breast
pain, swelling, skin alterations, abscess formation, ulceration,
sinus tract or fistula development in advanced or chronic cases,
and, at times, accompanying axillary lymphadenopathy (2,14).
GM is considered to develop following injury to the breast ductal
epithelium. Such damage permits luminal secretions to leak into the
surrounding lobular connective tissue, initiating a localized
inflammatory reaction. This process attracts lymphocytes and
macrophages to the site, ultimately leading to a granulomatous
inflammatory response (6).
The exact etiology of GM remains unclear; however,
multiple mechanisms have been proposed, suggesting a multifactorial
origin. Autoimmunity is considered the most accepted hypothesis,
supported by the favorable response to corticosteroids and other
immunosuppressive therapies, as well as the frequent association
with systemic manifestations such as EN and arthritis (15). Hormonal influences appear
significant, as GM occurs predominantly in women of reproductive
age, particularly during the postpartum period, and has been linked
to factors, such as pregnancy, breastfeeding, oral contraceptive
use and hyperprolactinemia. A potential genetic predisposition has
also been suggested, with certain human leukocyte antigen (HLA)
types, including HLA-A*10, HLA-A*2403, HLA-B*18 and HLA-DR*17,
found more commonly in affected individuals (15). Environmental and infectious
triggers, including Corynebacterium species and other
microbiological agents, have also been implicated. Overall, GM
appears to result from a complex interaction of autoimmune,
hormonal, genetic and environmental factors rather than a single
underlying cause (15).
EN is a frequently encountered condition in
rheumatology, characterized as an inflammatory process of the
subcutaneous tissue. It typically presents with the acute onset of
tender, erythematous nodules or plaques ranging from 1 to 6 cm in
diameter (16). The lesions most
often appear in a bilateral and symmetrical distribution,
predominantly involving the pretibial regions of the lower
extremities, though they may also extend to the ankles, thighs and
forearms (17). In line with these
observations, both the present case report and the study by Alungal
et al (18) documented
painful cutaneous lesions confined to the lower limbs.
In the present study, a literature review was also
conducted to identify studies reporting GM associated with EN. The
search was performed using Google Scholar with the key words
‘granulomatous mastitis’ and ‘erythema nodosum’, yielding six
relevant reports (Table II)
(1,16-20).
The association between GM and EN was first described in
1987(19). The documented patients
ranged in age from 16 to 42 years, all of whom were female. Among
the 6 cases, 3 cases involved lesions in the right breast.
 | Table IIReported cases of GM with erythema
nodosum identified in the literature. |
Table II
Reported cases of GM with erythema
nodosum identified in the literature.
| First author, year
of publication | Location of skin
lesion | No. of cases | Age (years) | Sex | Presentation | Previous
history | Physical
examination | Laboratory
tests | Imaging
findings | Histopathology
findings | Management | Follow-up | (Refs.) |
|---|
| Salesi, 2011 | Right breast,
anterior tibia | 1 | 23 | F | Pain and swelling
in the right breast, generalized body pain, arthralgia in hands,
elbows, shoulders, knees, and ankles, arthritis, swelling in both
knees and ankles, malaise, painful red nodules in the anterior
tibia, nodules in the right breast with purulent discharge | NA | Right breast: pain,
swelling, nodules with purulent discharge; anterior tibia: painful
red nodules | WBC=7,400
(Neut=68%, Lymph=25%), Hb=11.8, PLT=431,000, ESR=85, CRP ++, RF -,
ANA -, dsDNA -, ANCA -, Ca=8.6, P=3.8, Alk-P=328, Alb=3.9, FBS=102,
Wright -, 2ME -, ACE=NL, tuberculin skin test=negative | Breast mammography:
subcutaneous fat and fibroglandular tissue edema, two images of
collections with dense fluid; normal chest X-ray | Multiple granulomas
with acute inflammatory cells, lymphoplasma cells, histiocytes,
epithelioid cells, noncaseating granuloma, negative for acid-fast
bacilli and fungal infection | Prednisolone 15 mg,
colchicine 1 mg, azathioprine 100 mg daily | All lesions
disappeared 15 days after the beginning of the drugs | (1) |
| Bes, 2010 | Right leg; Both
legs | 2 | 34, 27 | F | Painful lump in
left breast; Lump in left breast and painful red EN lesions in both
legs | No history of TB,
diabetes mellitus, or family history of breast pathology; No TB
infection or breast cancer in family history (Case 2) | Case 1: Mass (5x5x4
cm) with induration in upper left breast, palpable left axillary
nodes; Case 2: 10-cm diameter, sensitive hard mass in the upper
outer quadrant of the left breast, axillary lymphadenomegaly | Case 1: Normal
chest X-ray, negative Mantoux test; Case 2: Normal chest X-ray,
negative Mantoux test, CRP 32, ESR 45 mm/h | Case 1: N/A; Case
2: Bilateral breast MRI: collections in the upper outer quadrant of
the left breast, a multiloculated abscess, diffuse contrast
involvement, increased blood flow, six lymph nodes in the left
axilla, ductuli with hemorrhagic contents, pathologic
contrast-involvement in the periductal fibroglandulary tissue | Case 1: Granulomas
with Langhans-type giant cells, neutrophils, small lymphocytes,
epithelioid cells; negative bacterial, fungal, and mycobacterium
cultures; Case 2: Microabscess foci with polymorpho-nucleated
neutrophils and epithelioid histiocytes, negative for TB | Oral Aprednisolone
32 mg/day (Case 1); Methylpredn-isolone 32 mg/day, tapered by 4 mg
weekly (Case 2) | Right leg (Case 1);
Both legs (Case 2) | (16) |
| Pesce, 2023 | Bilateral lower
legs, below the knees, on the anterior and lateral aspects of the
lower legs, and perimal-leolar areas | 1 | 42 | F | Left breast pain
and induration, bilateral erythematous/purplish-brown skin lesions
on lower legs, slightly painful, nonpruritic nodules | Left colon surgery
in early childhood due to an intestinal malformation | Left breast: firm
mass with ill-defined edges, 4-cm diameter in the upper inner
quadrant; bilateral lower legs: erythematous/purplish-brown
lesions, mildly tender nodules between 1 and 6 cm, warm to the
touch | Positive C-reactive
protein 106 mg/l; liver function tests normal; anti-streptolysin O,
blood cultures, and urine cultures negative; purified protein
derivative skin test negative | Mammography: new
developing asymmetry in the upper inner quadrant of the left
breast, no skin thickening; breast ultrasound: hypoechoic, no mass
lesion with Doppler vascularization, surrounding adipose tissue
with increased echogenicity, preserved skin around the lesion | Breast parenchyma
with marked lymphocytic lobulitis, epithelioid histiocytes with
pseudonodular appearance, intense lymphoplasmacytic inflammatory
infiltrate with polymorpho-nuclear leukocytes; PAS and
Ziehl-Neelsen staining negative for pathogens | Conservative
management with active surveillance | One month after the
initial visit, erythema nodosum resolved spontaneously, and
granulo-matous mastitis remained stable | (17) |
| Alungal, 2016 | Both legs and the
forearm | 1 | 25 | F | Pain and swelling
in the left breast with yellowish discharge from nipple, bilateral
pain, swelling, and redness of multiple joints, low-grade fever,
painful red nodules on limbs and forearm | No specific history
reported | Tender axillary
lymphadenopathy, erythematous palpable discrete nodules over both
limbs and forearm, a 5x4 cm tender and firm swelling in the upper
inner quadrant of the left breast | Hemoglobin 10.5
gm%, total leukocyte counts 12,700 cells/mm³, with 79% neutrophils,
platelet count 3.2 Lakhs/mm³, ESR 64 mm/1st h, normal renal and
liver function tests, normal urinalysis, negative blood culture,
normal chest radiography | Follow-up
ultrasonogram showed a significant decrease in the size of the
breast lump | FNAC showed a
collection of epithelioid cells, multinucleated giant cells, and
non-caseous granuloma; negative gram and acid-fast bacilli
stainings, negative fungal, TB, and atypical mycobacteria cultures,
negative tuberculin skin test, negative anti-citrullinated cyclic
peptide, antinuclear antibody, P and C antineutrophil cytoplasmic
antibodies, normal serum angiotensin converting enzyme level,
normal serum Ca | Oral
corticosteroids | Symptom-free after
one month, with a significant decrease in the size of the breast
lump | (18) |
| Adams, 1987 | Both shins | 1 | 24 | F | Painful lump in
left breast, tender red lumps on both shins, arthralgia affecting
hands, knees, and ankles; developed 4 months postpartum | No nipple
discharge, no use of contraceptive pill or other medication | Pyrexia (38˚C),
hard, tender mass (12x9 cm) in the left breast with indrawing of
nipple, erythema nodosum on both legs, periarthritis in both
ankles, no lymphadenopathy | Normal hemoglobin
and white cell count, raised ESR (104 mm/h) and CRP (374 mg/ml),
normal bio-chemical profile (including Ca and liver function
tests), negative routine cultures of sputum, urine, and breast
tissue; negative cultures of breast tissue for mycobacterium by
guinea-pig inoculation, anti-streptolysin O titre <200 Todd
units, normal chest X-ray, no evidence of immune dysfunction,
normal serum immunoglobulins, negative tests for autoantibodies,
circulating immune complexes, and activated lymphocytes, negative
tuberculin skin test, negative Kveim biopsy | Not specified | Histology showed
areas of inflammation predominantly related to breast lobules,
granulomata, and foci of microabscess formation, characteristic of
idiopathic granulomatous mastitis; four acid-fast bacilli were seen
on Ziehl-Neelson staining | Indomethacin,
rifampicin, and isoniazid for 6 weeks until negative culture
results; rapid resolution of fever, erythema nodosum, and
arthritis, sterile discharge from the wound persisted for 6
weeks | Gradual decrease in
size of the lump with almost complete resolution at 5 months | (19) |
| Laor, 2022 | Bilateral shins and
lower thighs | 1 | 16 | F | Right-sided painful
breast swelling, polyarthritis, erythema nodosum on bilateral shins
and lower thighs | No trauma, fever,
weight loss, night sweats, cough, shortness of breath, irregular
bowel patterns, or changes in stool pattern; no recent vaccination,
travel, exposure to animals, or consumption of exotic foods | Right breast with
firm, poorly circumscribed area of induration (11 cm diameter),
erythematous tender patch with central fluctuation above areola, no
abnormalities in nipple-areola complex; active arthritis of
bilateral knees and ankles, EN on lower extremities | Hemoglobin 11 g/dl,
hematocrit 34.3%, WBC 10.6x103/µlL, polymorpho-nuclear
cells 77%, lymphocytes 13%, monocytes 9%, eosinophils 1%, platelets
291x103/µl, elevated ESR (37 mm/h) | Ultrasound: large
complex area (3.3 cm thickness) with internal vascularity; negative
chest roentgenogram for mediastinal lymphadenopathy, cardiac, or
pulmonary abnormalities | Histopathology:
noncaseating granuloma within breast lobules with neutrophils and
microabscess formation; cultures negative for bacterial, fungal,
and AFB organisms | Wide local
excision, trimethoprim-sulfametho-xazole, naproxen, prednisone (60
mg daily) with taper over 12 weeks | Steady and complete
resolution of all symptoms; near return to baseline prior to
discharge; sustained improvement with steroid taper | (20) |
Adams et al (19) described the case of a 24-year-old
postpartum female patient presenting with a painful left breast
mass, florid EN on both legs and periarthritis. The initial
clinical impression suggested carcinoma due to the breast mass and
nipple retraction; however, the prominent cutaneous lesions and
joint involvement indicated an inflammatory rather than malignant
etiology (19). Similarly, Salesi
et al (1) reported the case
of a 23-year-old pregnant female who developed painful right breast
swelling, arthritis and EN on both tibiae. Their case highlighted
that systemic manifestations, such as arthritis and panniculitis,
may precede or occur concurrently with breast symptoms, supporting
a potential autoimmune or hypersensitivity component in idiopathic
GM (1).
Other reports support this pattern. Alungal et
al (18) described the case of
a 25-year-old female patient presenting with a breast mass,
polyarthritis and EN, with nodules distributed on the shins and
forearms. Bes et al (16)
documented the cases of 2 female patients, aged 27 and 34 years,
both of whom developed breast masses clinically suggestive of
carcinoma, followed by EN on the lower legs. In these cases, EN
developed either concurrently with or shortly after the breast
lesion (16), as was also observed
in the present case. Laor et al (20) extended the phenotype to a
16-year-old adolescent who presented with breast swelling,
polyarthritis, and EN on the shins and thighs, highlighting that
the same constellation can occur even in younger age groups.
Recently, Pesce et al (17)
reported the case of a 42-year-old female patient whose
presentation was initially indistinguishable from breast cancer.
However, the incidental finding of bilateral EN on her legs shifted
diagnostic suspicion toward idiopathic GM (17).
The diagnosis of GM is often challenging due to
imaging modalities, such as US, mammography and magnetic resonance
imaging, which typically yield non-specific findings, usually
demonstrating only a mass, parenchymal distortion, or multifocal
lesions. Consequently, HPE remains the definitive diagnostic
method, and the biopsy of any suspicious area is essential.
Characteristic features of GM include chronic granulomatous
inflammation with giant cells, leukocytes, epithelioid cells, and
macrophages (21).
In the case presented herein, the diagnosis was
established through a combination of histopathology and systematic
exclusion of infectious and systemic causes, consistent with
approaches reported in the literature. Clinical suspicion was
raised by a unilateral painful breast mass accompanied by EN. A
laboratory evaluation revealed leukocytosis and anemia, whereas ASO
titers, chest radiography and IGRA were negative. The US identified
a mass, prompting a core biopsy. Histopathological analysis
demonstrated non-caseating granulomas composed of epithelioid
histiocytes and multinucleated giant cells, without evidence of
caseous necrosis or microorganisms, confirming idiopathic GM as the
underlying process. The diagnosis was further supported by the
resolution of EN following immunomodulatory therapy.
In the case described in the study by Alungal et
al (18), fine-needle
aspiration cytology demonstrated epithelioid cells, multinucleated
giant cells and non-caseating granulomas. Specific stains for
bacteria, fungi and acid-fast bacilli were negative, and autoimmune
serological analyses did not yield any notable findings, supporting
a diagnosis of idiopathic GM (18). Bes et al (16) emphasized the pitfalls of
misdiagnosis: Of note, 1 patient was initially treated as having
tuberculosis due to a misinterpreted histological analysis
exhibiting necrosis. Upon reevaluation, the cultures were negative,
and the presence of EN guided the recognition of idiopathic GM
(16). Laor et al (20) performed a broader pediatric workup,
including autoimmune serologies and ophthalmological examination
for sarcoidosis, all of which yielded negative results. A
histological analysis confirmed lobulocentric granulomas with
microabscesses, establishing idiopathic GM in an adolescent
(20). Pesce et al
(17) highlighted the
cancer-mimicking nature of idiopathic GM on imaging, ultimately
reaching the diagnosis through core biopsy demonstrating
lobulocentric granulomatous inflammation, after cultures and stains
excluded infection.
The management of GM remains a subject of debate,
perhaps attributed to its infrequent occurrence and the limited
comprehension of its pathophysiology, as well as its prevalence
among economically disadvantaged patients. Several therapy
approaches have been documented, although their effectiveness has
varied. The alternatives include careful waiting, surgical
intervention, systemic corticosteroids and chemotherapeutic
medicines. Corticosteroid administration has emerged as the most
consistently effective intervention across published series.
Alungal et al (18)
reported the rapid remission of both breast and systemic
manifestations following glucocorticoid therapy, while Bes et
al (16) described the cases
of 2 female patients with idiopathic GM-associated EN who exhibited
a marked improvement on corticosteroids after the misdiagnosis of
tuberculosis was excluded. By contrast, Adams et al
(19) observed spontaneous
regression with symptomatic management, and Pesce et al
(17) described the case of a
patient managed conservatively without corticosteroids in whom EN
resolved spontaneously, suggesting a variable natural course. In
the case in the present study, oral prednisolone combined with
colchicine resulted in the complete resolution of both cutaneous
and breast manifestations. The addition of colchicine, although
less frequently reported in the literature, may be particularly
rational given its efficacy in neutrophilic dermatoses, such as EN,
as demonstrated by Salesi et al (1), who employed colchicine alongside
steroids and azathioprine with favorable outcomes.
A limitation of the present case report is the
unavailability of breast US images. Although the US was performed
and its findings described, the absence of imaging documentation
may limit the clarity and illustrative value of the case.
In conclusion, the accurate diagnosis of GM is
essential to prevent unnecessary interventions. Management with
corticosteroids can lead to favorable outcomes. Understanding
systemic associations, such as EN, is vital for comprehensive
patient care.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
RSA and AMS were major contributors to the
conception of the study, as well as to the literature search for
related studies. KMS, MKA and FHK contributed to the clinical
management of the patient, assisted in data acquisition and
interpretation, and participated in the literature review and
manuscript preparation. ASM, HMD, SHH and HOA contributed to the
conception and design of the study, the literature review, the
critical revision of the manuscript, and the processing of the
table. LRAP was the radiologist who performed the assessment of the
case. AMS, ASM, and RSA assisted in diagnosing the patient,
contributed to the management of the patient, and participated in
manuscript review. FHK and KMS confirm the authenticity of all the
raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Verbal consent was initially obtained from the
patient, followed by written informed consent at a later date for
participation in the present case report.
Patient consent for publication
Verbal consent was initially obtained from the
patient, followed by written informed consent at a later date for
the publcatoin of the present case report and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Salesi M, Karimifar M, Salimi F and
Mahzouni P: A case of granulomatous mastitis with erythema nodosum
and arthritis. Rheumatol Int. 31:1093–1095. 2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Salih AM, Pshtiwan LR, Abdullah AM, Dhahir
HM, Ali HO, Muhialdeen AS, Hussein BO, Hassan SH and Kakamad FH:
Granulomatous mastitis masking ductal carcinoma in situ: A
case report with literature review. Biomed Rep. 20:1–5.
2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Grover H, Grover SB, Goyal P, Hegde R,
Gupta S, Malhotra S, Li S and Gupta N: Clinical and imaging
features of idiopathic granulomatous mastitis-The diagnostic
challenges and a brief review. Clin Imaging. 69:126–132.
2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Parperis K, Achilleos S, Costi E and
Vardas M: Granulomatous mastitis, erythema nodosum and arthritis
syndrome: Case-based review. Rheumatol Int. 41:1175–1181.
2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Korkut E, Akcay MN, Karadeniz E, Subasi ID
and Gursan N: Granulomatous mastitis: A ten-year experience at a
university hospital. Eurasian J Med. 47:165–173. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Esmaeil NK, Salih AM, Hammood ZD, Pshtiwan
LR, Abdullah AM, Kakamad FH, Abdullah HO, Ahmed GS, Abdalla BA and
Salih RQ: Clinical, microbiological, immunological and hormonal
profiles of patients with granulomatous mastitis. Biomed Rep.
18:1–8. 2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Wang X, He X, Liu J, Zhang H, Wan H, Luo J
and Yang J: Immune pathogenesis of idiopathic granulomatous
mastitis: From etiology toward therapeutic approaches. Front
Immunol. 15(1295759)2024.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Fletcher A, Magrath IM, Riddell RH and
Talbot IC: Granulomatous mastitis: A report of seven cases. J Clin
Pathol. 35:941–945. 1982.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Cribier B, Caille A, Heid E and Grosshans
E: Erythema nodosum and associated diseases. A study of 129 cases.
Int J Dermatol. 37:667–672. 1998.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Olfatbakhsh A, Beheshtian T and Djavid GE:
Granulomatous mastitis, erythema nodosum, and oligoarthritis in a
pregnant woman. Breast J. 14:588–590. 2008.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Moreno-Vílchez C, Llobera-Ris C, Penin RM,
Pla MJ, Mitjavila F and Marcoval J: Granulomatous mastitis
associated with erythema nodosum: A case series of 42 patients. Med
Clín. 158:229–232. 2022.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
12
|
Prasad S, Nassar M, Azzam AY, José FG,
Jamee M, Sliman RKA, Evola G, Mustafa AM, Abdullah HO, Abdalla BA,
et al: CaReL guidelines: A consensus-based guidelineson case
reports and literature review (CaReL). Barw Med J. 2:13–19.
2024.
|
|
13
|
Abdullah HO, Abdalla BA, Kakamad FH, Ahmed
JO, Baba HO, Hassan MN, Bapir R, Rahim HM, Omar DA, Kakamad SH, et
al: Predatory publishing lists: A review on the ongoing battle
against fraudulent actions. Barw Med J. 2:26–30. 2024.
|
|
14
|
Kessler E and Wolloch Y: Granulomatous
mastitis: A lesion clinically simulating carcinoma. Am J Clin
Pathol. 58:642–646. 1972.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Shorbagi AI, Alwardat D, Parlakgumus A,
Pekoz BC, Taş ZA and Al Ojaimi M: An update on granulomatous
lobular mastitis: It is time to tell the untold. J Clin Pract Res.
45:115–122. 2023.
|
|
16
|
Bes C, Soy M, Vardi S, Sengul N and Yilmaz
F: Erythema nodosum associated with granulomatous mastitis: report
of two cases. Rheumatol Int. 30:1523–1525. 2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Pesce KA, Peralta KL, Chico MJ, Wernicke A
and Binder F: Granulomatous mastitis with erythema nodosum: A
breast cancer mimicking entity. Radiol Case Rep. 18:3809–3814.
2023.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Alungal J, Abdulla MC and Narayan R:
Idiopathic granulomatous mastitis with erythema nodosum and
polyarthritis. Reumatismo. 68:97–99. 2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Adams DH, Hubscher SG and Scott DG:
Granulomatous mastitis-a rare cause of erythema nodosum. Postgrad
Med J. 63:581–582. 1987.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Laor L, Ganguli S and Fakioglu E:
Granulomatous mastitis, erythema nodosum, and polyarthritis: A case
report. J Med Case Rep. 16(146)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Evans J, Sisk L, Chi K, Brown S and To H:
Concurrent granulomatous mastitis and invasive ductal cancer in
contralateral breasts-a case report and review. J Surg Case Rep.
7(rjab519)2021.PubMed/NCBI View Article : Google Scholar
|