Introduction
Vitiligo is a skin disease characterized by
dysfunction or destruction of melanocytes with secondary
depigmentation, which constitutes the pathophysiological hallmark
of the disease. The pathogenesis of vitiligo involves multiple
factors. In 1950, Lerner proposed the neural theory (1). Since then, different evolving theories
for the pathogenesis of vitiligo have been mentioned, including
susceptibility genes, autoimmune response, abnormalities in the
melanocytes and/or cellular damage from oxidative stress.
Genes for generalized vitiligo (GV) include
XBP1, FOXP3, NALPq, TYR, and
TLSP (2). Additionally, certain
MHC genes are also associated with vitiligo, including the
HLA-DRB1*07, HLA-A2 and HLA-B17 alleles.
Similarly, SNAPs genotyping studies have demonstrated that the 6q27
chromosome is linked to this skin depigmentation disorder (3). The pathophysiology of autoimmune vitiligo
involves humoral and cellular immunity by mechanisms that produce
melanocyte damage. Clinically, depigmentation can be a unique
symptom associated with autoantibody production and/or cell
hypersensitivity. However, in a few cases of GV, the skin disease
can be associated with other autoimmune diseases. With respect to
the mechanisms involved in the autoimmune destruction of
melanocytes, CD8 T cells appear to trigger melanocyte damage. Then,
vitiligo antigens are released by cytolysis. Therefore, the initial
insult is followed by a humoral autoimmune response against
vitiligo-associated autoantigens, including MART-1, tyrosinase, and
gp100 (2–11).
The epidemiology of this disease indicates that the
prevalence of vitiligo ranges from 0.5 to 1% of the general
population, and the disease is equally distributed in females and
males (12). Considering that vitiligo
is a common disease associated with various autoimmune diseases and
that these comorbidities are usually evaluated as separate clinical
entities, it is of interest to define the rheumatic comorbidities
that can be associated with vitiligo as part of a multi-autoimmune
syndrome, wherein this designation applies to the association of
three or more autoimmune diseases in the same patient.
The aim of the present study was to determine the
association of vitiligo with multiple autoimmune rheumatic diseases
in a database covering a period of 10 years.
Materials and methods
Subjects
The clinical files of patients who were treated in
the Department of Rheumatology from 2005 and 2015 were reviewed.
Using the data files, the main disease that led to the evaluation
was identified. Subsequently, the number of patients with or
without rheumatic autoimmune diseases such as osteoarthritis,
lumbalgia or tendinitis associated with vitiligo was determined.
Each patient was reviewed by a skilled rheumatologist and
dermatologist, respectively, and clinical criteria for disease for
classification in each autoimmune disease was followed.
Additionally, in each patient with vitiligo, the availability of
serum samples stored in a freezer was determined, allowing for
evaluation of the anti-melanocyte and anti-tyrosinase antibodies,
which are markers of autoimmune vitiligo. Additionally, a group of
rheumatic patients lacking autoimmune disease was included as the
control group. Autoimmune co-morbidities and autoantibodies were
assessed in the two groups.
The study was approved by the ethics committee of
Universidad Autónoma de Zacatecas (Zacatecas, Mexico). Patient
consent was obtained from each patient.
Anti-melanocyte antibodies
An intradermal nevus, ~0.5 cm in diameter, of the
preauricular region in a patient who was 27 years with no clinical
or serological manifestations of autoimmunity was removed for
cosmetic reasons. Prior to this procedure, a signed authorization
was obtained to use part of the nevus as an antigenic source. The
lesion was divided into two parts; one part was sent for
histopathological analysis and another part was used for indirect
immunofluorescence studies (13). The
tissue was transported to the laboratory on ice, and was
subsequently embedded in Tissue-Tek OCT® (Leica
Biosystems, Nussloch, Germany) and frozen at −20°C. Tissue samples
were cut at 4 µm using a cryostat (−20°C), and the slices were
fixed on slides. The serum samples were tested at dilutions of 1:20
to 1:160, incubated with the antigenic source for 30 min in a moist
chamber, and the slides were washed three times in
phosphate-buffered saline (PBS) (pH 7.2). This step was followed by
a 30-min incubation with polyvalent FITC-labelled rabbit anti-human
antiserum (cat. no. F4637; 1:80; Sigma-Aldrich, St. Louis, MO,
USA). After three additional PBS washes, the slides were mounted
with glycerol-PBS (9:1), and two independent observers evaluated
the samples using an Olympus B-Max BX-40 fluorescence microscope
(Olympus, Tokyo, Japan) in a blinded manner.
Anti-tyrosinase antibodies
The specificity of the sera to tyrosinase was
evaluated in triplicate by ELISA as previously described (14) with modifications. Polystyrene plates
were covered overnight with 10 µg of tyrosinase fragment 369–377
(cat. no. T8455; Sigma-Aldrich) dissolved in 70% ethanol. Uncovered
sites were neutralized with 4% BSA. The serum samples were diluted
1:100 and applied into the microwells. They were then incubated for
2 h at room temperature. After 3 washes, the samples were incubated
with secondary antibody goat anti-human IgG HRP (cat. no. sc-2453;
Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA) for 1 h. After
washing again, the colour reaction was developed with TMB in a
30-min incubation. The reaction was then stopped with 0.5 M
sulfuric acid and the microplates were read at 450 nm using a
microplate reader (Thermo Fisher Scientific, Inc., Shanghai,
China).
Other autoantibodies
Anti-thyroid antibodies on a commercial antigenic
source, anti-nuclear antibodies in HEp-2 cells (Immuno Concepts,
Inc., Sacramento, CA, USA) and anti-epithelial antibodies, using as
antigen source cow nose, were evaluated with indirect
immunofluorescence.
Statistical analysis
The probability of the association between vitiligo
and certain autoimmune rheumatic disease was calculated using the
χ2 test. The relative risk and odds ratios (OR), with
95% of confidence intervals, were determined using the Prism
software program (GraphPad Software, Inc., San Diego, CA, USA).
P<0.0001 was considered statistically significant.
Results
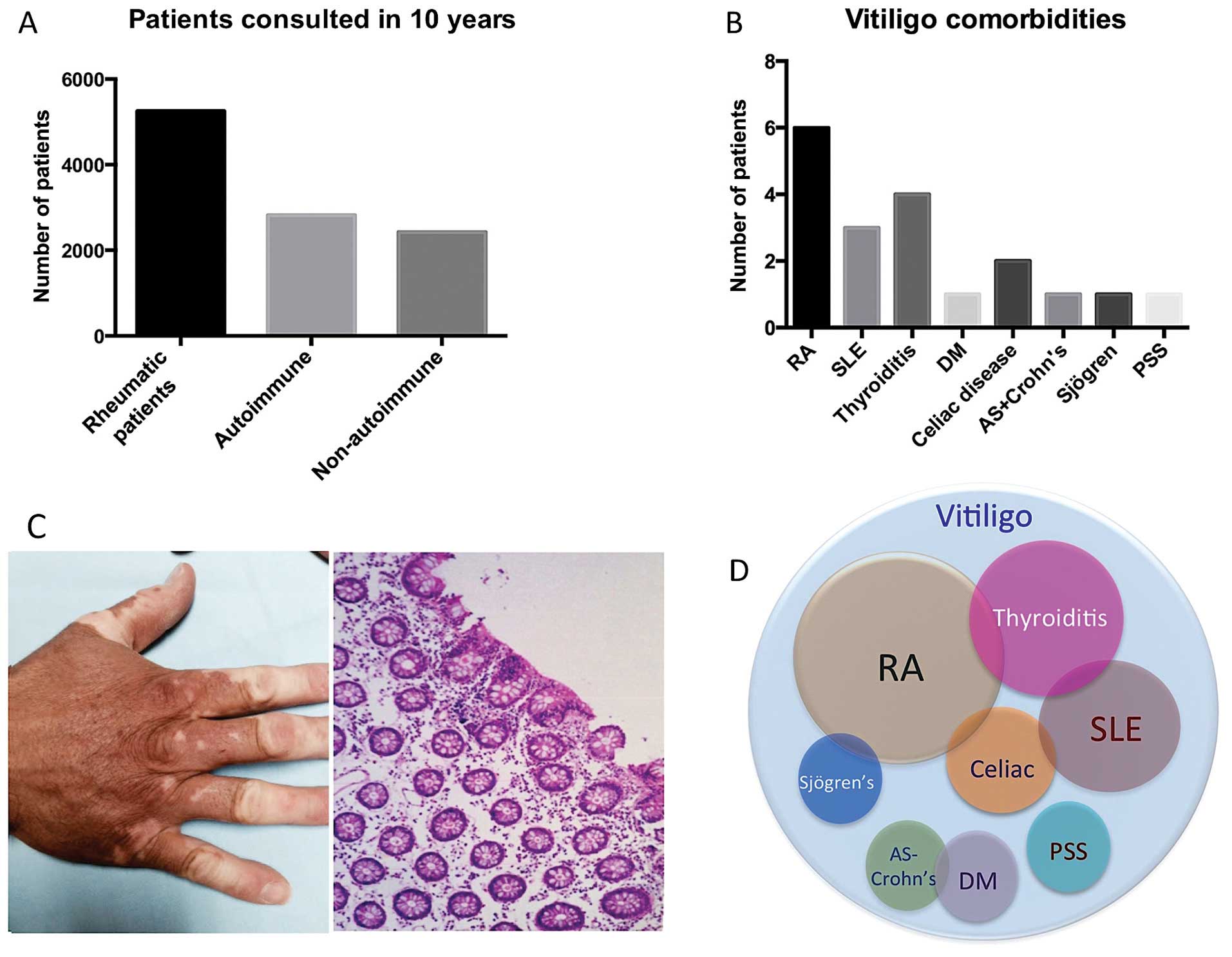
Clinical records
In 10 years, a total of 5,251 records were filed.
Each record corresponded to one patient, and these patients were
evaluated over multiple rheumatology consultations. From these,
2,824 files corresponded to patients with autoimmune disease (54%),
while the remaining 2,427 (46%) had other rheumatic diseases,
including degenerative, metabolic or other diseases. The most
prevalent autoimmune disease was exhibited by rheumatoid arthritis
(RA) patients who met the ACR/EULAR classification criteria
(15), which accounted for 43% of
autoimmune rheumatic diseases. This was followed by 26% with lupus
erythematosus, which met the ACR revised criteria for SLE (16). Other diseases, such as scleroderma,
accounted for a lower proportion of the cases (2.4%). Of the total
number of autoimmune rheumatic diseases, 19 patients, 16 women and
3 men, with a mean age of 36 years, had GV (17), corresponding to 0.672% of the sample.
Clinically, most of the patients had skin depigmentation
distributed along the face, hands and trunk (Fig. 1). In contrast to the control group,
only one patient with osteoarthritis had localized spots of
vitiligo, and the prevalence was 0.0412%. The differences between
the two groups were significant (P<0.0002) (Fig. 1). Of note, the relative risk for
developing vitiligo was significantly increased in patients who had
an additional autoimmune comorbidity, such as celiac of 33%
(18) or thyroid disease in 19%
(19) (Table
I).
 | Table I.Relative risk for developing
vitiligo. |
Table I.
Relative risk for developing
vitiligo.
| Disease | No. of patients | Vitiligo | Prevalence | P-value | Relative risk | OR |
|---|
| NARD | 2,427 | 1 | 0.041 |
|
|
|
| ARD | 2,829 | 19 | 0.672 | 0.0002 | 0.0612 | 0.0608 |
| RA | 1,899 | 6 | 0.315 | 0.0257 | 0.1304 | 0.1300 |
| SLE | 742 | 3 | 0.404 | 0.0148 | 0.1019 | 0.1015 |
| Sjögren |
91 | 1 | 1.098 | 0.0004 | 0.0374 | 0.0371 |
| PSS |
68 | 1 | 1.470 | 0.0001 | 0.0280 | 0.0276 |
| DM |
20 | 1 | 5.000 | 0.0001 | 0.0082 | 0.0078 |
| Tyroiditis + RA or
SLE |
21 | 4 | 19.047 | 0.0001 | 0.0021 | 0.0017a |
| Celiac disease +
SLE or RA |
6 | 2 | 33.333 | 0.0001 | 0.0012 | 0.0008a |
| AS + Crohn's
disease |
4 | 1 | 25.000 | 0.0001 | 0.0016 | 0.0012a |
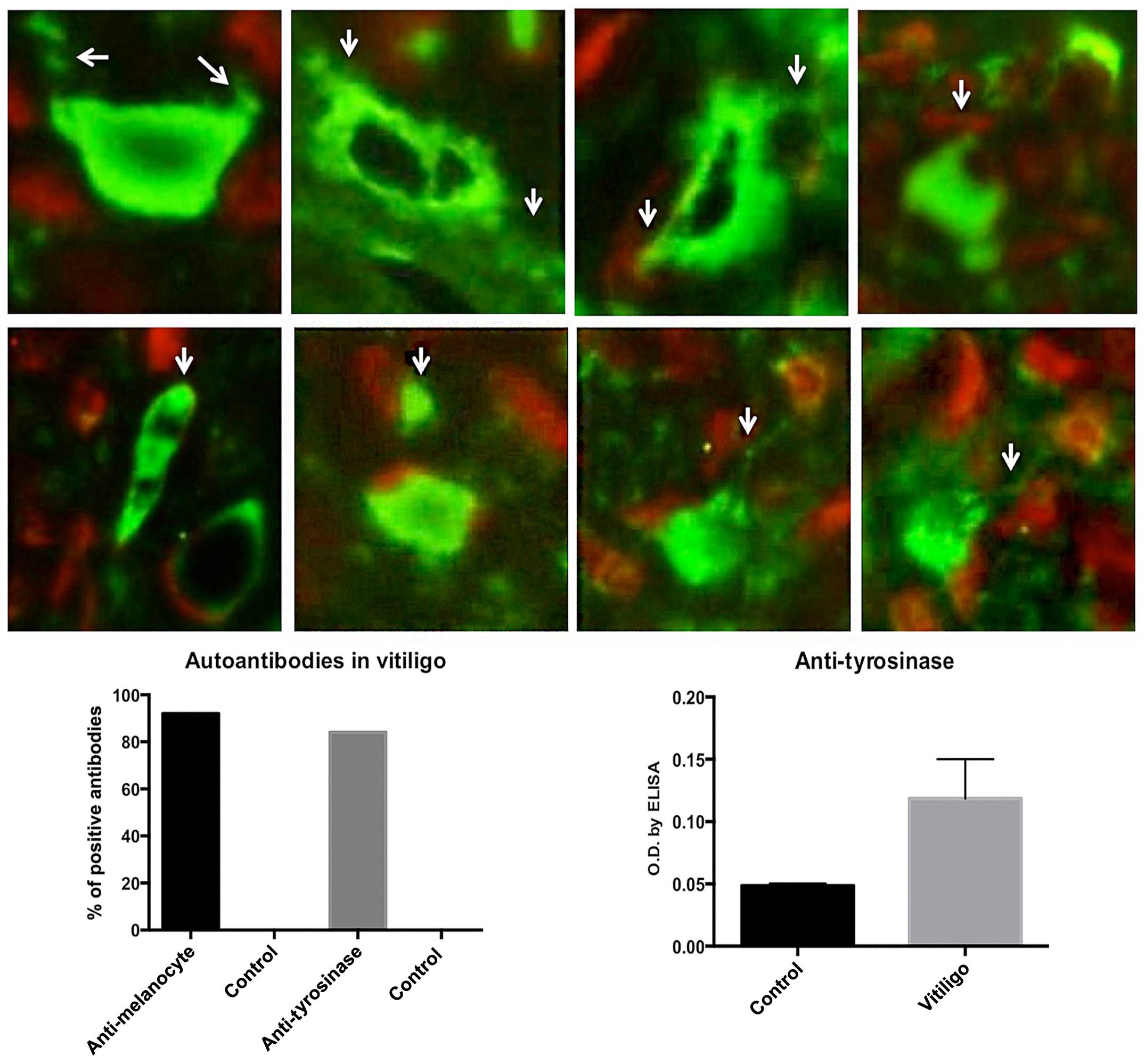
Autoantibodies
Ninety-two percent of the group with autoimmune
rheumatic disease and associated vitiligo tested positive for
anti-melanocyte antibodies. Therefore, fluorescence was observed in
scattered melanocytes along the epidermis as well as in melanosomes
and melanin granules for some patients. The antibody titres varied
across the patients. By contrast, the anti-tyrosinase antibodies
were positive in 84% of the patients (Fig.
2).
Other shared autoantibodies included rheumatoid
factor and anti-CCP, ANA, anti-thyroid and anti-epithelial
antibodies although none of the patients had symptoms of
pemphigus.
Discussion
Vitiligo is a disease characterized by the loss of
pigment-producing cells. The disease has psychological and social
consequences, and in some cases it is caused by autoimmunity. The
aim of the present study was to determine the prevalence of
vitiligo associated with other autoimmune rheumatic diseases. The
main results of the present study were as follows. First, the
prevalence of vitiligo associated with autoimmune rheumatic disease
was 0.672. Second, autoantibodies against vitiligo-associated
antigens were present in the 92% of the autoimmune group. Third, RA
and lupus were frequently associated with vitiligo, although the
relative risk of vitiligo as an event occurring, measured the
magnitude of association using the cumulative incidence, rather
than the total number. This measure showed the relative risk of
vitiligo in RA was not different than the prevalence reported in
the general population. Notably, the vitiligo risk was markedly
increased when the two diseases were associated with thyroid or
celiac disease.
Vitiligo has been extensively studied. In 1979,
Goudie et al (20) brought
attention to the comorbidities of vitiligo, suggesting that this
disease constituted a set of mosaic patches with distinctive shared
characteristics of autoimmunity. Traditionally, vitiligo alone has
been extensively studied worldwide, including in Latin America. The
present study was performed in the mestizo population of a central
region of Mexico. The mestizo population results from a mixture
between Amerindian Caucasian and African genes (21). In Mexico, the prevalence of vitiligo in
children has been estimated as 2.6% (22). The present study addresses the
prevalence of vitiligo in adult patients with rheumatic disease,
and the global prevalence of vitiligo detected in the present study
was 0.380, which is lower than the 0.5–2% reported in the overall
worldwide population by Krüger and Schallreuter (23). The differences with the present results
can be explained by ethnic factors or different methodologies used
in the patients included in each study. Of note, the prevalence of
vitiligo is variable; for instance, the prevalence in the Korean
population is 0.12% (24), while it is
lower (0.093%) in a Chinese Shaanxi Province (25). In both instances, the prevalence in
some Asiatic countries is lower than in the present study.
Concurrence of various autoimmune diseases in a
single patient captured the attention of different clinical
research groups, and diverse names have been given to these
associated comorbidities, including polyautoimmunity, multiple
autoimmunity, and shared autoimmunity (26–30). The
autoimmune rheumatic comorbidities associated with vitiligo are
variable, including RA and psoriasis (31–33). In the
Middle Eastern population, the association of vitiligo with RA is
related to the TNFα-308 A/G promoter (34), which probably reflects that this
cytokine participates in melanocyte destruction. Sjögren disease
has been reported to be associated with vitiligo (35). Other autoimmune comorbidities that
accompany rheumatic diseases and vitiligo include pernicious anemia
(36), Graves' disease, autoimmune
haemolytic anemia (37), thyroid and
celiac disease and other pathologies (38–42). Common
pathogenic mechanisms that are suggested to facilitate these
comorbidities involve the protein tyrosine phosphatase non-receptor
type 22 (PTPN22) gene, which seems to increase the
susceptibility for one patient to have a cluster of different
autoimmune diseases. This cluster includes type I diabetes, RA,
autoimmune thrombocytopenia, inflammatory myopathies, Graves'
disease, SLE, ANCA-associated vasculitis, and Cohn's disease
(43). On the other hand, HLA-DQ
pleiotropic genes are also involved in the pathogenesis of multiple
autoimmunity (44).
In conclusion, based on the results of this study,
the association between vitiligo and one autoimmune rheumatic
disease is relatively low, which is probably similar to the
prevalence of vitiligo in the general population. Nevertheless,
when this disease is associated with more than two autoimmune
comorbidities, including thyroid or celiac disease, its relative
risk is notably increased. In such a case, a multiple autoimmune
syndrome should be suspected.
References
|
1
|
Spritz RA: The genetics of vitiligo. J
Invest Dermatol. 131(E1): E18–E20. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Birlea SA, Jin Y, Bennett DC, Herbstman
DM, Wallace MR, McCormack WT, Kemp EH, Gawkrodger DJ, Weetman AP,
Picardo M, et al: Comprehensive association analysis of candidate
genes for generalized vitiligo supports XBP1, FOXP3, and TSLP. J
Invest Dermatol. 131:371–381. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Quan C, Ren YQ, Xiang LH, Sun LD, Xu AE,
Gao XH, Chen HD, Pu XM, Wu RN, Liang CZ, et al: Genome-wide
association study for vitiligo identifies susceptibility loci at
6q27 and the MHC. Nat Genet. 42:614–618. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rahoma SF, Sandhu HK, McDonagh AJ,
Gawkrodger DJ, Weetman AP and Kemp EH: Epitopes, avidity and IgG
subclasses of tyrosine hydroxylase autoantibodies in vitiligo and
alopecia areata patients. Br J Dermatol. 167:17–28. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Park YK, Kim NS, Hann SK and Im S:
Identification of autoantibody to melanocytes and characterization
of vitiligo antigen in vitiligo patients. J Dermatol Sci.
11:111–120. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Li S, Yao W, Pan Q, Tang X, Zhao S, Wang
W, Zhu Z, Gao J, Sheng Y, Zhou F, et al: Association analysis
revealed one susceptibility locus for vitiligo with immune-related
diseases in the Chinese Han population. Immunogenetics. 67:347–354.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Evoli A, Caliandro P, Iorio R, Alboini PE,
Damato V, LaTorre G, Provenzano C, Marino M, Lauriola L, Scuderi F,
et al: Poly-autoimmunity in patients with myasthenia gravis: A
single-center experience. Autoimmunity. 48:412–417. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Byrne KT, Zhang P, Steinberg SM and Turk
MJ: Autoimmune vitiligo does not require the ongoing priming of
naive CD8 T cells for disease progression or associated protection
against melanoma. J Immunol. 192:1433–1439. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Colucci R, Böhm M and Moretti S:
Commentary from the Editorial Board to Vitiligo: Interplay between
oxidative stress and immune system (Laddha et al). Exp
Dermatol. 22:397–398. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ingordo V, Cazzaniga S, Raone B,
Digiuseppe MD, Musumeci ML, Fai D, Pellegrino M, Pezzarossa E, Di
Lernia V, Battarra VC, et al: Circulating autoantibodies and
autoimmune comorbidities in vitiligo patients: a multicenter
Italian study. Dermatology. 228:240–249. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gregg RK, Nichols L, Chen Y, Lu B and
Engelhard VH: Mechanisms of spatial and temporal development of
autoimmune vitiligo in tyrosinase-specific TCR transgenic mice. J
Immunol. 184:1909–1917. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Alkhateeb A, Fain PR, Thody A, Bennett DC
and Spritz RA: Epidemiology of vitiligo and associated autoimmune
diseases in Caucasian probands and their families. Pigment Cell
Res. 16:208–214. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Petersen M, Davids LM and Kidson SH:
Simultaneous immunofluorescent labeling using anti-BrdU monoclonal
antibody and a melanocyte-specific marker in formalin-fixed
paraffin-embedded human skin samples. Appl Immunohistochem Mol
Morphol. 20:614–617. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Okamoto T, Irie RF, Fujii S, Huang SK,
Nizze AJ, Morton DL and Hoon DS: Anti-tyrosinase-related protein-2
immune response in vitiligo patients and melanoma patients
receiving active-specific immunotherapy. J Invest Dermatol.
111:1034–1039. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Aletaha D, Neogi T, Silman AJ, Funovits J,
Felson DT, Bingham CO III, Birnbaum NS, Burmester GR, Bykerk VP,
Cohen MD, et al: 2010 Rheumatoid arthritis classification criteria:
an American College of Rheumatology/European League Against
Rheumatism collaborative initiative. Arthritis Rheum. 62:2569–2581.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hochberg MC: Updating the American College
of Rheumatology revised criteria for the classification of systemic
lupus erythematosus. Arthritis Rheum. 40:17251997. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ezzedine K, Lim HW, Suzuki T, Katayama I,
Hamzavi I, Lan CC, Goh BK, Anbar T, de Silva Castro C, Lee AY, et
al: Vitiligo Global Issue Consensus Conference Panelists: Revised
classification/nomenclature of vitiligo and related issues: The
Vitiligo Global Issues Consensus Conference. Pigment Cell Melanoma
Res. 25:E1–E13. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rubio-Tapia A, Hill ID, Kelly CP,
Calderwood AH and Murray JA: American College of Gastroenterology:
ACG clinical guidelines: diagnosis and management of celiac
disease. Am J Gastroenterol. 108:656–676; quiz 677. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Garber JR, Cobin RH, Gharib H, Hennessey
JV, Klein I, Mechanick JI, Pessah-Pollack R, Singer PA and Woeber
KA: American Association of Clinical Endocrinologists and American
Thyroid Association Taskforce on Hypothyroidism in Adults: Clinical
practice guidelines for hypothyroidism in adults: cosponsored by
the American Association of Clinical Endocrinologists and the
American Thyroid Association. Endocr Pract. 18:988–1028. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Goudie RB, Spence JC and MacKie R:
Vitiligo patterns simulating autoimmune and rheumatic diseases.
Lancet. 2:393–395. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Santana C, Noris G, Meraz-Ríos MA, Magaña
JJ, Calderon-Aranda ES, Muñoz ML and Gómez R: Genetic analysis of
17 Y-STRs in a Mestizo population from the Central Valley of
Mexico. Hum Biol. 86:289–312. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ruiz-Maldonado R, Tamayo Sánchez L and
Velázquez E: Epidemiology of skin diseases in 10,000 patients of
pediatric age. Bol Med Hosp Infant Mex. 34:137–161. 1977.(In
Spanish). PubMed/NCBI
|
|
23
|
Krüger C and Schallreuter KU: A review of
the worldwide prevalence of vitiligo in children/adolescents and
adults. Int J Dermatol. 51:1206–1212. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lee H, Lee MH, Lee DY, Kang HY, Kim KH,
Choi GS, Shin J, Lee HJ, Kim DH, Kim TH, et al: Prevalence of
vitiligo and associated comorbidities in Korea. Yonsei Med J.
56:719–725. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lu T, Gao T, Wang A, Jin Y, Li Q and Li C:
Vitiligo prevalence study in Shaanxi Province, China. Int J
Dermatol. 46:47–51. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Humbert P and Dupond JL: Multiple
autoimmune syndromes. Ann Med Interne (Paris). 139:159–168.
1988.(In French). PubMed/NCBI
|
|
27
|
Anaya JM: The diagnosis and clinical
significance of polyautoimmunity. Autoimmun Rev. 13:423–426. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Anaya JM, Castiblanco J, Rojas-Villarraga
A, Pineda-Tamayo R, Levy RA, Gómez-Puerta J, Dias C, Mantilla RD,
Gallo JE, Cervera R, et al: The multiple autoimmune syndromes. A
clue for the autoimmune tautology. Clin Rev Allergy Immunol.
43:256–264. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Rojas-Villarraga A, Amaya-Amaya J,
Rodriguez-Rodriguez A, Mantilla RD and Anaya JM: Introducing
polyautoimmunity: secondary autoimmune diseases no longer exist.
Autoimmune Dis. 2012:2543192012.PubMed/NCBI
|
|
30
|
Cojocaru M, Cojocaru IM and Silosi I:
Multiple autoimmune syndrome. Maedica (Buchar). 5:132–134.
2010.PubMed/NCBI
|
|
31
|
Liu JB, Li M, Yang S, Gui JP, Wang HY, Du
WH, Zhao XY, Ren YQ, Zhu YG and Zhang XJ: Clinical profiles of
vitiligo in China: An analysis of 3742 patients. Clin Exp Dermatol.
30:327–331. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zhang Z, Xu SX, Zhang FY, Yin XY, Yang S,
Xiao FL, Du WH, Wang JF, Lv YM, Tang HY, et al: The analysis of
genetics and associated autoimmune diseases in Chinese vitiligo
patients. Arch Dermatol Res. 301:167–173. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Laberge G, Mailloux CM, Gowan K, Holland
P, Bennett DC, Fain PR and Spritz RA: Early disease onset and
increased risk of other autoimmune diseases in familial generalized
vitiligo. Pigment Cell Res. 18:300–305. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Lee YH and Bae SC: Associations between
TNF-α polymorphisms and susceptibility to rheumatoid arthritis and
vitiligo: A meta-analysis. Genet Mol Res. 14:5548–5559. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Roguedas AM, Misery L, Sassolas B, Le
Masson G, Pennec YL and Youinou P: Cutaneous manifestations of
primary Sjögren's syndrome are underestimated. Clin Exp Rheumatol.
22:632–636. 2004.PubMed/NCBI
|
|
36
|
Abraham Z, Rozenbaum M, Glück Z, Feuerman
EJ, Lahat N and Kinarty A: Vitiligo, rheumatoid arthritis and
pernicious anemia. J Dermatol. 20:418–423. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chan HL, Lee YS, Hong HS and Kuo TT:
Anticentromere antibodies (ACA): Clinical distribution and disease
specificity. Clin Exp Dermatol. 19:298–302. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ponto KA, Schuppan D, Zwiener I, Binder H,
Mirshahi A, Diana T, Pitz S, Pfeiffer N and Kahaly GJ:
Thyroid-associated orbitopathy is linked to gastrointestinal
autoimmunity. Clin Exp Immunol. 178:57–64. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Boelaert K, Newby PR, Simmonds MJ, Holder
RL, Carr-Smith JD, Heward JM, Manji N, Allahabadia A, Armitage M,
Chatterjee KV, et al: Prevalence and relative risk of other
autoimmune diseases in subjects with autoimmune thyroid disease. Am
J Med. 123:183.e1–183.e9. 2010. View Article : Google Scholar
|
|
40
|
Amador-Patarroyo MJ, Arbelaez JG, Mantilla
RD, Rodriguez-Rodriguez A, Cárdenas-Roldán J, Pineda-Tamayo R,
Guarin MR, Kleine LL, Rojas-Villarraga A and Anaya JM: Sjögren's
syndrome at the crossroad of polyautoimmunity. J Autoimmun.
39:199–205. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Larizza D, Calcaterra V, Klersy C, Badulli
C, Caramagna C, Ricci A, Brambilla P, Salvaneschi L and Martinetti
M: Common immunogenetic profile in children with multiple
autoimmune diseases: the signature of HLA-DQ pleiotropic genes.
Autoimmunity. 45:470–475. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Zakka LR, Reche PA and Ahmed AR: The
molecular basis for the presence of two autoimmune diseases
occurring simultaneously - preliminary observations based on
computer analysis. Autoimmunity. 45:253–263. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Zheng J, Ibrahim S, Petersen F and Yu X:
Meta-analysis reveals an association of PTPN22 C1858T with
autoimmune diseases, which depends on the localization of the
affected tissue. Genes Immun. 13:641–652. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Cárdenas-Roldán J, Rojas-Villarraga A and
Anaya JM: How do autoimmune diseases cluster in families? A
systematic review and meta-analysis. BMC Med. 11:732013. View Article : Google Scholar : PubMed/NCBI
|