Introduction
Cervical spondylosis is a degenerative disc disease.
It has been reported that it may be identified in the majority of
people aged over 50 years, and the most prevalent symptom of
cervical spondylosis is pain in the neck and/or arms in China
(1). Furthermore, the neck or arm pain
caused by cervical spondylosis has become a worldwide health
problem (2). In the USA, ~14% of
adults aged ≥18 years have experienced or suffered from neck pain
over the course of the last few months (3).
Anterior cervical discectomy and fusion (ACDF) has
been widely used in clinical practice, and is accepted as the
standard procedure in the treatment of cervical spondylosis. As one
of the most important procedures in the treatment of cervical
degenerative disease, it has the effect of not only relieving the
spinal cord and the nerve roots' pressure, but also of reinforcing
the stability of the cervical vertebrae. However, with the
increased number of total operations being performed and the
accumulation of follow-up information over time, several studies
have reported certain adverse effects, including higher reoperation
rates at adjacent levels (4,5).
In 1966, Fernström (6)
first introduced cervical disc arthroplasty (CDA) as an operational
method in the treatment of cervical spondylosis, and it has been
gradually accepted as an alternative and effective approach in the
treatment of cervical spondylosis. However, over time, several
studies have indicated certain untoward adverse effects resulting
from this procedure, including increased neck and/or arm pain
following the operation and heterotopic ossification (7,8).
As the most commonly used procedures in cervical
spondylosis, only a few studies have been published which compare
these two operation types, particularly with respect to their
mid-term efficacy and safety. In these studies, even large sample
trials have generated controversial results with respect to each
other (9,10), making it inconvenient for clinicians to
refer to them. Therefore, the aim of the present study and
systematic review was to assess the advantages and shortcomings of
the two operational methods, CDA and ACDF.
Materials and methods
Search strategy and selection
criteria
According to the method of Cochrane guidelines
(Cochrane Handbook for Systematic Reviews of Interventions, version
5.1.0; see www.handbook.cochrane.org), the electronic databases,
PubMed, Web of Science, Cochrane library, EMBASE, the China
Biological Medicine and China National Knowledge Infrastructure
(CNKI), were carefully searched. Up to March 2016, the randomized
controlled trials (RCTs) and prospective comparative trials (PCTs),
including all languages that compared ACDF and CDA, were selected.
The Boolean terms ‘AND, ‘OR’ and ‘NOT’ were introduced to combine
the key words, including ‘anterior cervical discectomy and fusion’,
‘cervical disc arthroplasty’, ‘cervical spondylosis’, ‘mid-term
efficacy’, ‘randomized controlled trial’, ‘prospective comparative
trials’, ‘systematic review’, ‘cervical osteoarthritis’, ‘disease
of vertebrae cervicales’, ‘fusion’, ‘arthrodesis’, ‘spine fusion’,
‘cervical disc replacement’, ‘degeneration disc disease’, ‘PCT’,
‘CDA’, ‘ACDF’, ‘RCTs’ and ‘PCTs’.
Inclusion criteria were as follows: RCTs and PCTs in
all languages that compared CDA with ACDF in the treatment of
cervical osteoarthritis; either gender (male or female); the
patient was aged 18 years or above with cervical osteoarthritis;
there was at least 24 months' postoperative follow-up; and at least
one of the following indexes were included: The Short Form survey
(SF-36) score, range of motion (ROM) in the operation level, Visual
Analog Scale (VAS) of neck and/or arm pain, Neck Disability Index
(NDI), the reoperation rate of adjacent levels following surgery,
the rate of neurologic improvement, surgical parameters (age of
patients, blood loss, hospital stay and surgical time) and the
total complication rate.
Exclusion criteria were as follows: Infection,
presentation of bone tumors for CDA/ACDF surgical treatment,
non-RCTs or non-PCT trials, severely cervical spinal stenosis, and
reoperation cases.
Assessment of the studies'
quality
Following the Cochrane collaboration guidelines
(Cochrane Handbook for Systematic Reviews of Interventions version
5.1.0), the quality of the studies was independently assessed by
two authors. The quality of these trials was assessed in seven
aspects, including selection bias (predominantly to judge the
generation of random sequence and allocation concealment),
performance bias (to evaluate the blinding of participants and
personnel) and attrition bias (to evaluate the degree of the
incomplete outcome data), together with other biases.
Combination data and meta
analysis
Review Manager (RevMan) 5.2.0 software was used to
analyze the data. The predominant outcomes extracted from these
trials were as follows: Age of the patients, blood loss, SF-36
score, VAS of neck and/or arm pain following the surgery, ROM at
the operation level, NDI following surgery, and the reoperation
rate of adjacent levels following surgery.
The heterogeneity was assessed using the chi-square
test and I-square statistics (11).
Fixed effect models (P<0.01, I2≤50%) were used when
there was insignificant heterogeneity; otherwise, the random effect
models (when P≤0.01, I2>50%) were applied. Odds ratio
(OR; relative risk) combined with 95% confidence intervals (CIs)
was used to describe the data of binary variables. For the
continuous variables, the weighted mean difference (WMD or standard
mean difference (SMD) with 95% CIs were applied. Begg's and Egger's
tests (12,13) using Stata version 12.0 software
(StataCorp, College Station, TX, USA) were introduced to test the
publication bias of the main marker of the reoperation rate of
adjacent levels following surgery. Sensitivity (14) and cumulative (15) analyses were also performed to assess
the stability of the main indicators. P<0.05 was considered to
indicate a statistically significant value.
Results
Results of the included online
searches and their quality evaluation
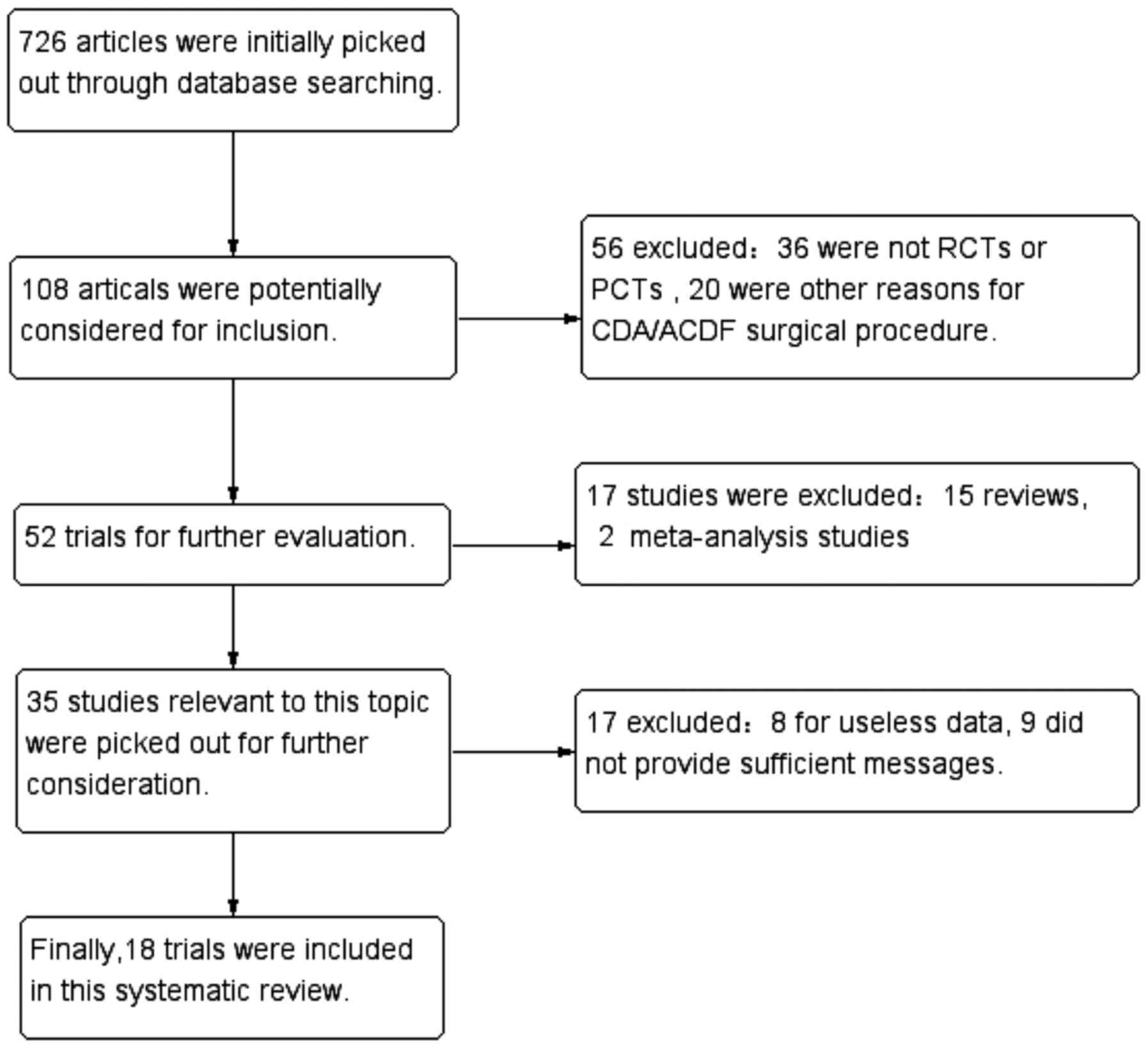
According to the search strategies previously
undertaken by our group, 726 articles were selected first of all.
In accordance with the exclusion and inclusion criteria, as
specified above, two authors read the titles and abstracts
independently. A total of 12 RCTs (9,10,16–25) and six
PCTs (26–31), including 3,040 patients (1,588 treated
with CDA and 1,452 with ACDF) were finally included in the present
systematic review (Fig. 1).
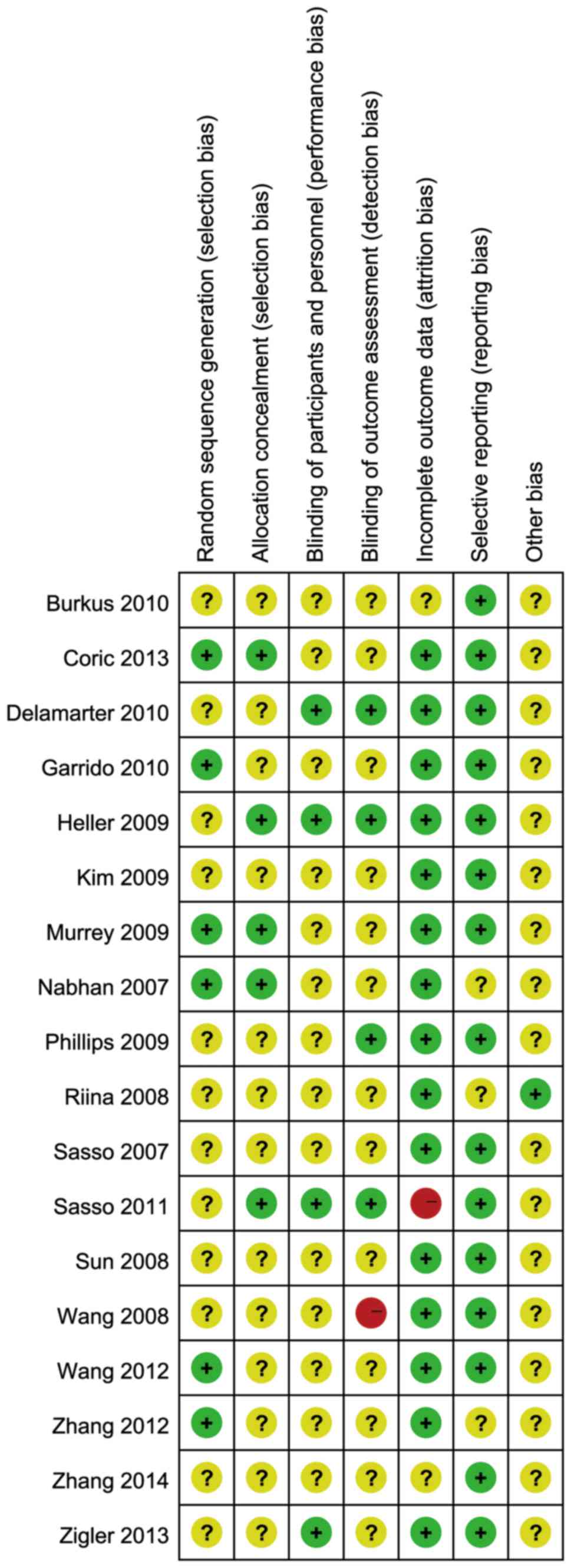
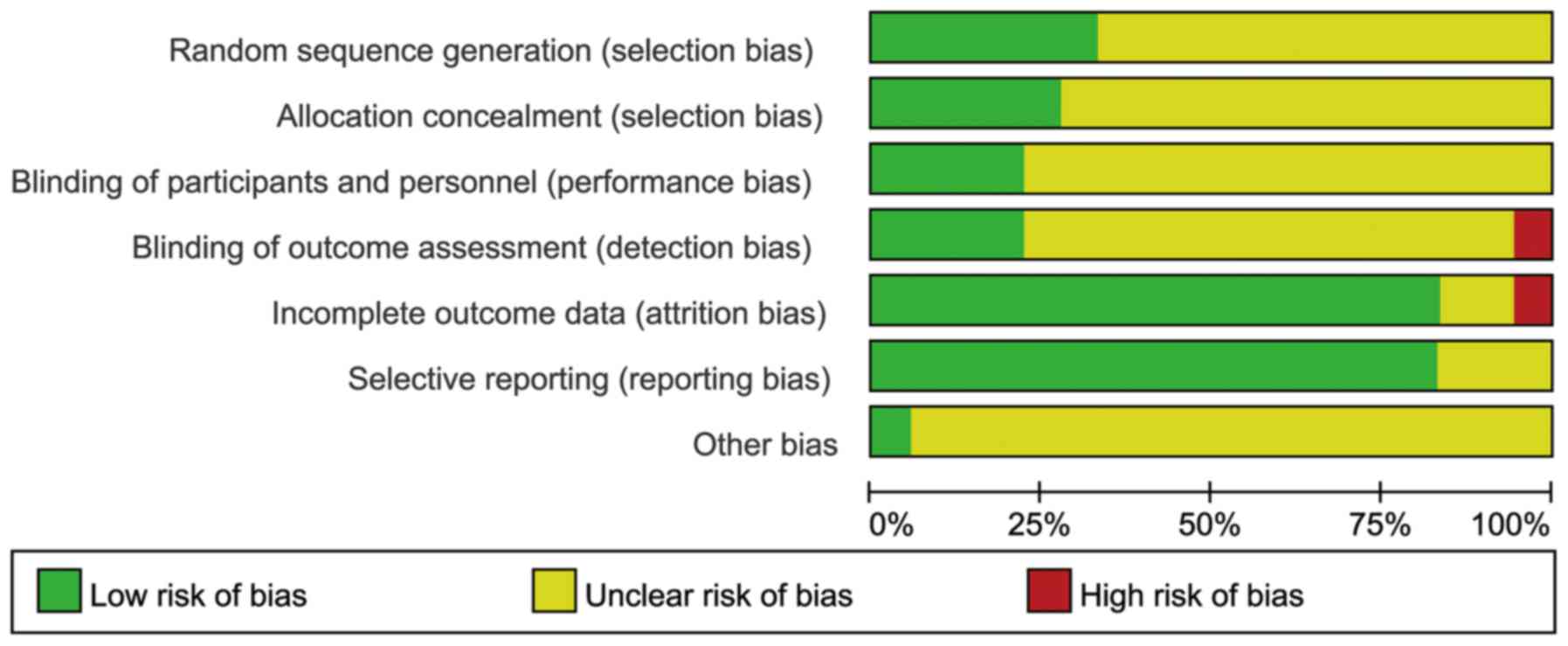
The Cochrane Collaboration rating system was used to
evaluate the risks of the included trials. There were seven
evaluation indexes, each of which had three levels, according to
this rating system: Low risk (denoted with ‘+’), high risk (denoted
with ‘-’), and unclear risk (denoted with ‘?’). The results are
shown in Figs. 2 and 3.
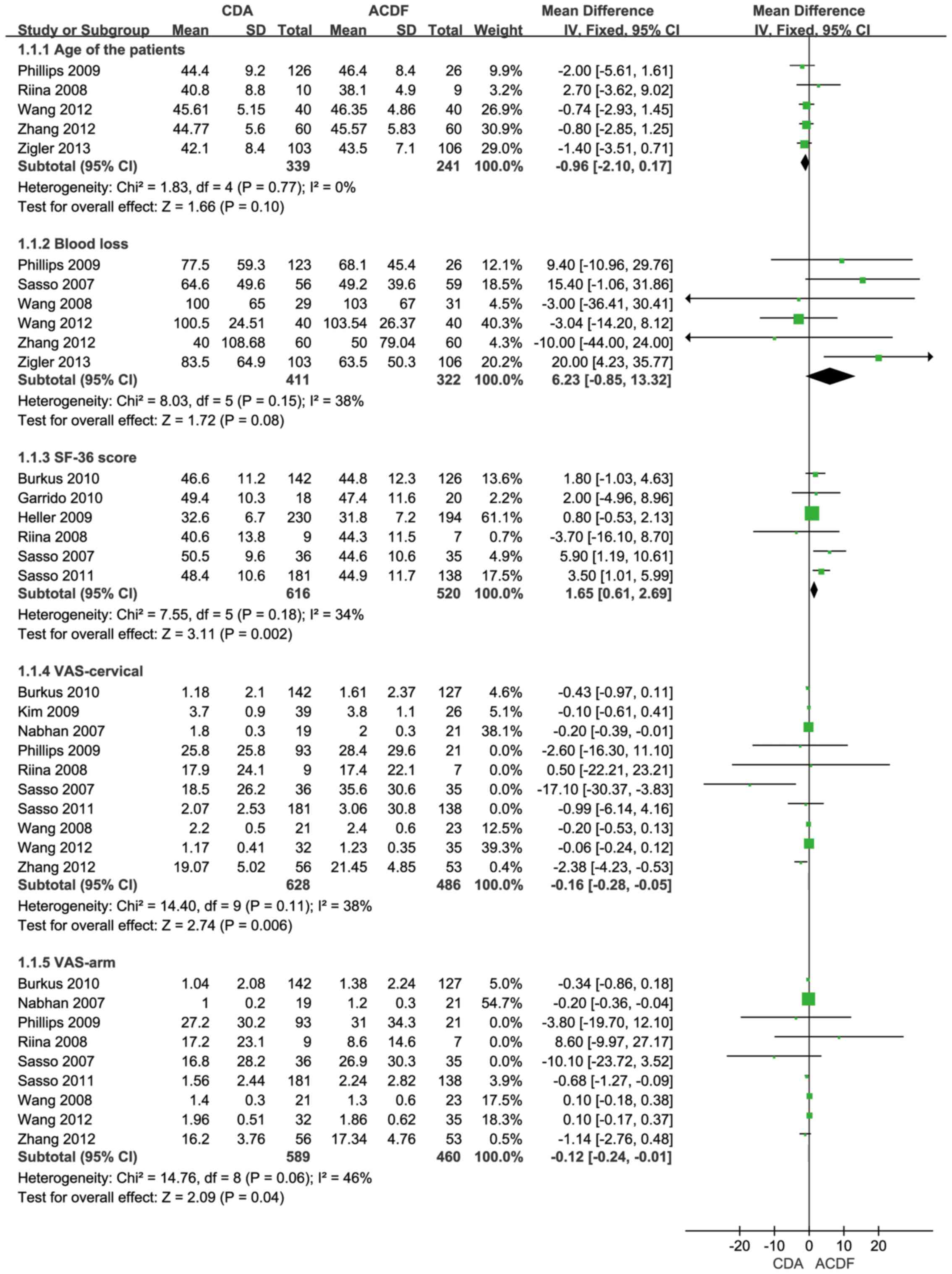
Age of the patients and the blood loss during the
surgery. Of the studies that were included, five of the trials
reported detailed data of the patients, including the standard
deviation (SD) and the mean of the ages. The combined results
indicated that the differences between two groups were not
statistically different (WMD=0.96; 95% CI, 2.10 to 0.17; P=0.10).
In addition, no significant differences were identified for the
heterogeneity tests (I2=0%; P=0.77), as shown in
Fig. 4.
The volume of blood loss during the operation was
assessed in six trials. From the combing results, no statistical
significance was observed with the WMD (WMD=6.23; 95% CI, 0.85 to
13.32; P=0.08), and moderate heterogeneity was identified among the
trials (I2=38%; P=0.15) (Fig.
4).
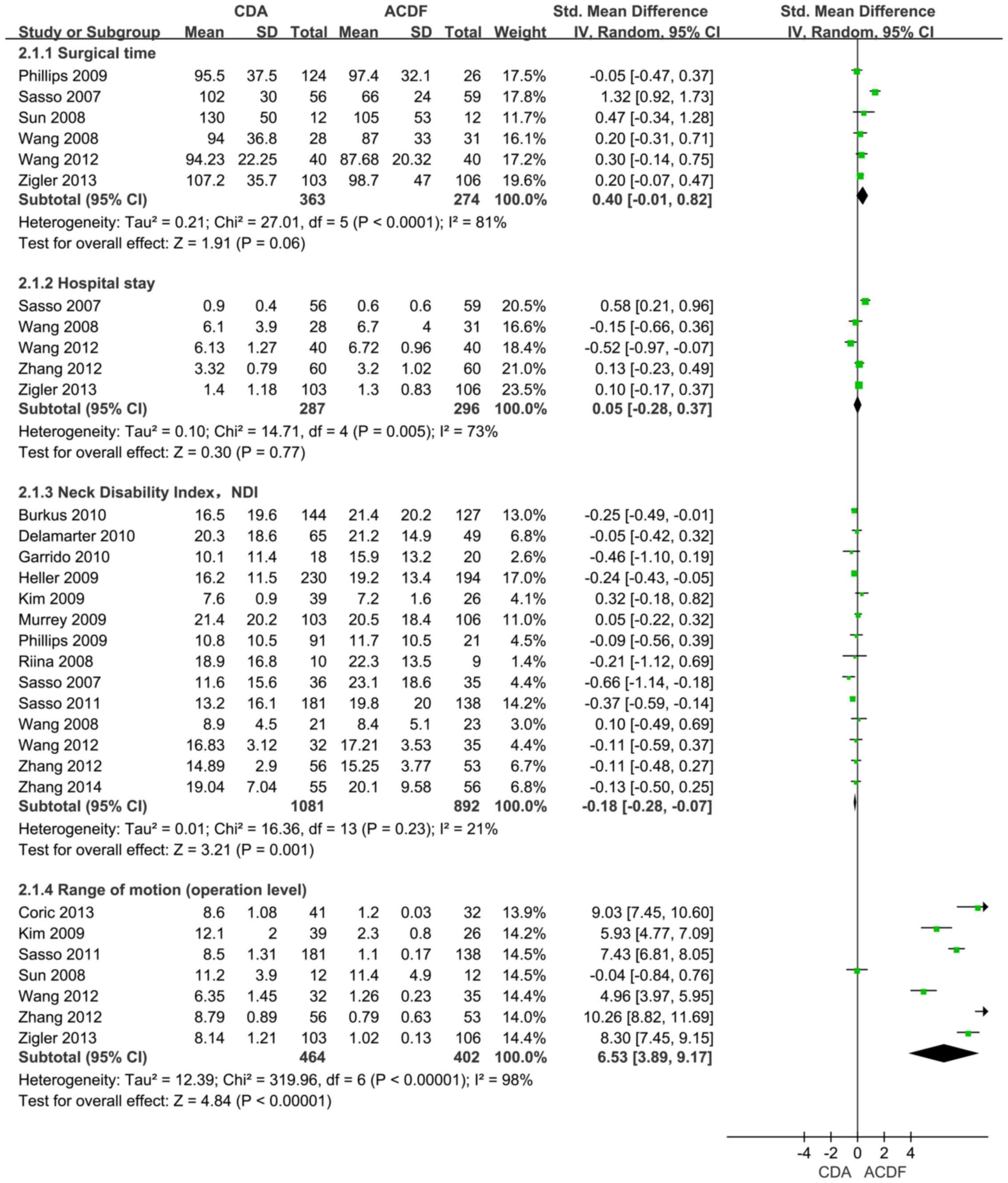
Operation time and hospital stay
Six trials provided the necessary data on the mean
operation time and the SD. The overall estimate revealed no
significant difference for the two procedures with respect to this
indicator (SMD=0.40; 95% CI, −0.01 to 0.82; P=0.06). The
heterogeneity of the studies was determined to be significant
(I2=81%; P<0.0001), as shown in Fig. 5.
Adequate data concerning the hospital stay were
available in five of the studies, and the comprehensive statistics
revealed no significant differences between CDA and ACDF (SMD=0.05;
95% CI, −0.28 to 0.371 P=0.77), although there was moderate
heterogeneity between them (I2=73%; P=0.005), as shown
in Fig. 5.
SF-36 score and VAS score following
surgery at a mid-term follow-up
SF-36 scores were available in six of the studies
with at least 24 months' follow-up. The overall results indicated
that the CDA group had the higher SF-36 scores (WMD=1.65; 95% CI,
0.61–2.69; P=0.002). The heterogeneity between these studies was
moderate (I2=34%, P=0.18), as shown in Fig. 4.
A VAS score of neck pain with at least 24 months'
follow-up following the operation was identified from ten trials,
and the comprehensive statistics indicated that the CDA procedure
had the lower VAS score of neck pain (WMD= 0.16; 95% CI, −0.28 to
−0.05; P=0.006), and that moderate heterogeneity was observed
between the CDA and ACDF groups (I2=38%; P=0.11), as
shown in Fig. 4.
Nine trials were concerned with the VAS scores of
arm pain with at least 24 months' follow-up, and the pool
statistics revealed that the CDA procedure was associated with less
arm pain (WMD=−0.12; 95% CI, −0.24 to −0.01; P=0.04) with moderate
heterogeneity observed between the CDA and ACDF groups
(I2=46%; P=0.06), as shown in Fig. 4.
NDI and ROM at the operational level
at a mid-term follow-up
Data regarding the NDI on a mid-term follow-up (at
least 24 months' follow-up) following the surgery were available in
14 of the trials. The comprehensive statistics showed that CDA had
the lower NDI (SMD=−0.18; 95% CI, −0.28 to −0.07; P=0.001).
Furthermore, the heterogeneity between the CDA and ACDF groups was
insignificant (I2=21%; P=0.23), as shown in Fig. 5.
Data concerning the ROM at the operational level (24
or more months' follow-up) were available in seven of the studies.
The overall results indicated that the CDA had a larger ROM at the
operational level (SMD=6.53; 95% CI, 3.89 to 9.17; P<0.0001).
The level of heterogeneity was significant among the trials
(I2=98%; P<0.00001), as shown in Fig. 5.
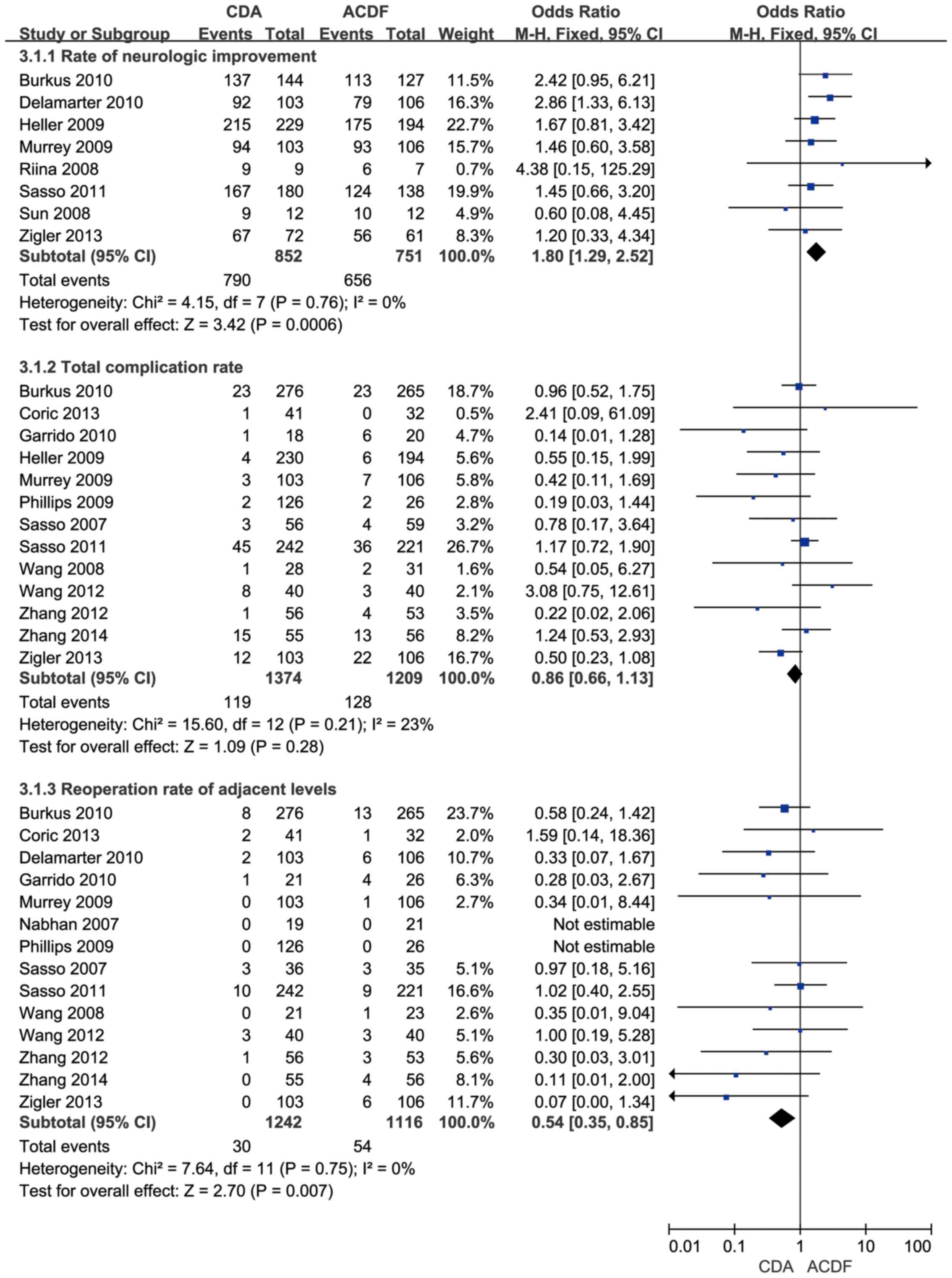
Rate of neurological improvement
following the operation at a mid-term follow-up
The rate of neurological improvement following the
operation was obtained from eight of the studies. Overall, the pool
statistics indicated that there was a significant difference in
favor of the CDA group (OR=1.80; 95% CI 1.29 to 2.52; P=0.0006),
although the heterogeneity test revealed an insignificant
difference (I2=0%; P=0.76), as shown in Fig. 6.
Total complications rate and the
reoperation rate of adjacent levels following surgery in a mid-term
follow-up
A total of 13 trials involving 2,583 patients
provided detailed information about the total complications rate
following surgery in a mid-term follow-up. From the final results
it was possible to conclude that there was an insignificant
difference between the CDA and ACDF groups (OR=0.86; 95% CI,
0.66–1.13; P=0.28), and the result of the heterogeneity test was
moderate (I2=23%; P=0.21), as shown in Fig. 6.
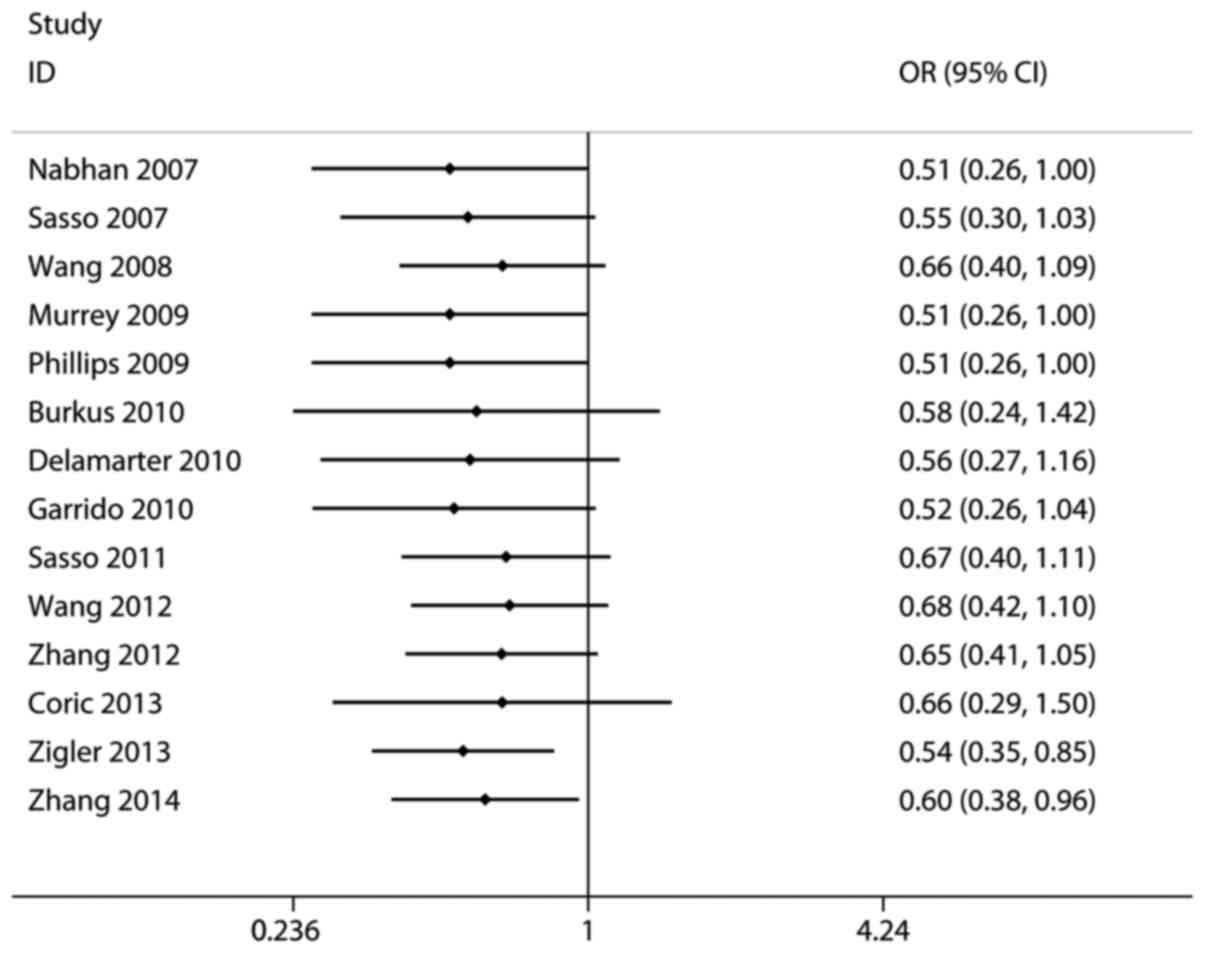
Data regarding the reoperation rate of adjacent
levels following surgery in a mid-term follow-up was available in
14 trials. Overall, the comprehensive statistics indicated that the
CDA procedure had a lower reoperation rate of adjacent levels
following surgery (OR=0.54; 95% CI, 0.35 to 0.85; P=0.007), with
insignificant heterogeneity bias (I2=0%; P=0.75), as
shown in Fig. 6.
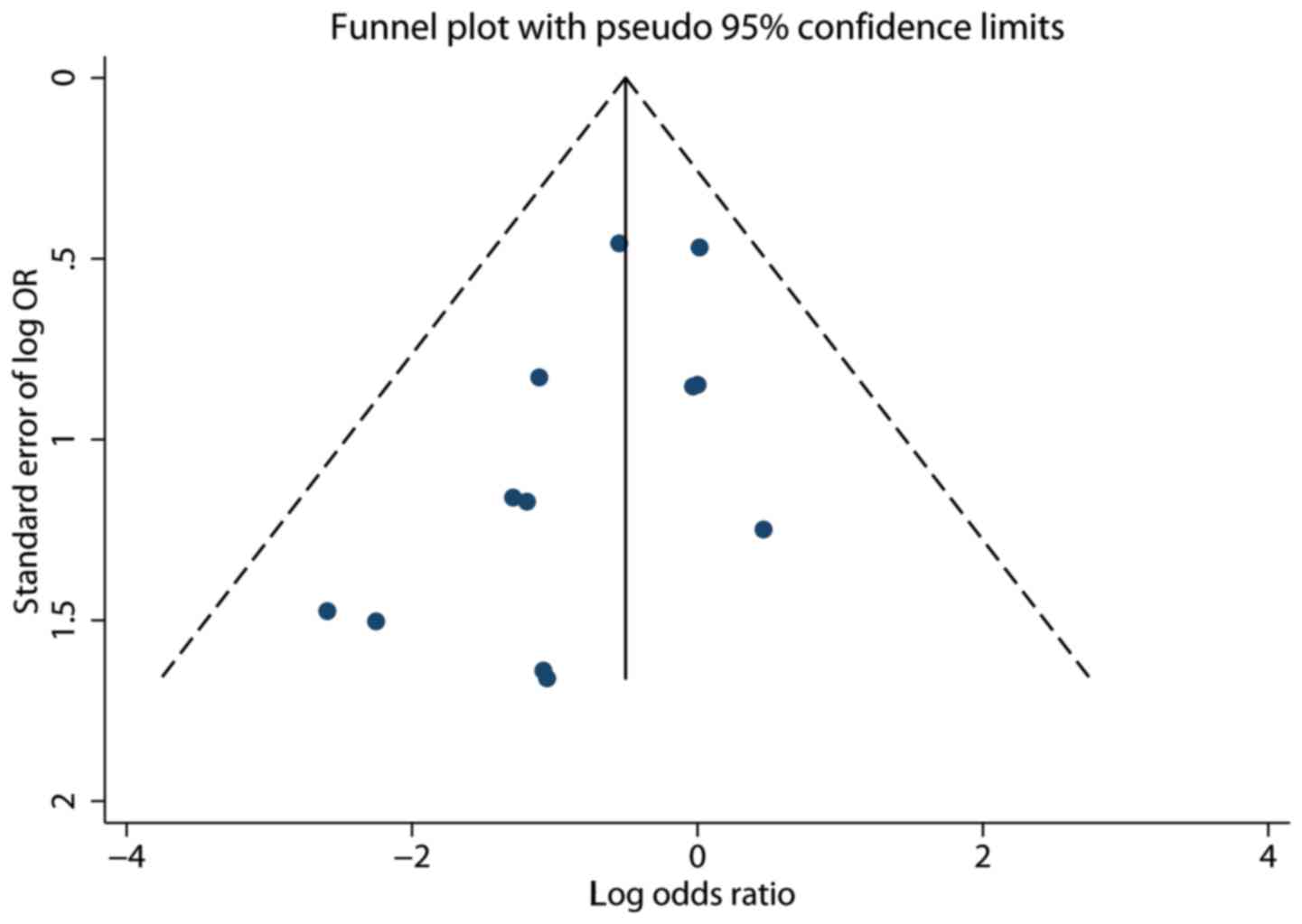
The test of publication bias and
sensitivity and cumulative analysis
For the reoperation rate of adjacent levels
following surgery, Stata version 12.0 software (StataCorp) was used
to test the publication bias (Begg's and Egger's tests). The
results of the Begg's test was Pr> |z|=0.373 (continuity
corrected), and the outcome of the Egger's test was 0.057, the two
tests revealing that there was insignificant publication bias in
this index. Funnel plots were also introduced to illustrate the
publication bias of the reoperation rate of adjacent levels
following surgery, as shown in Fig.
7.
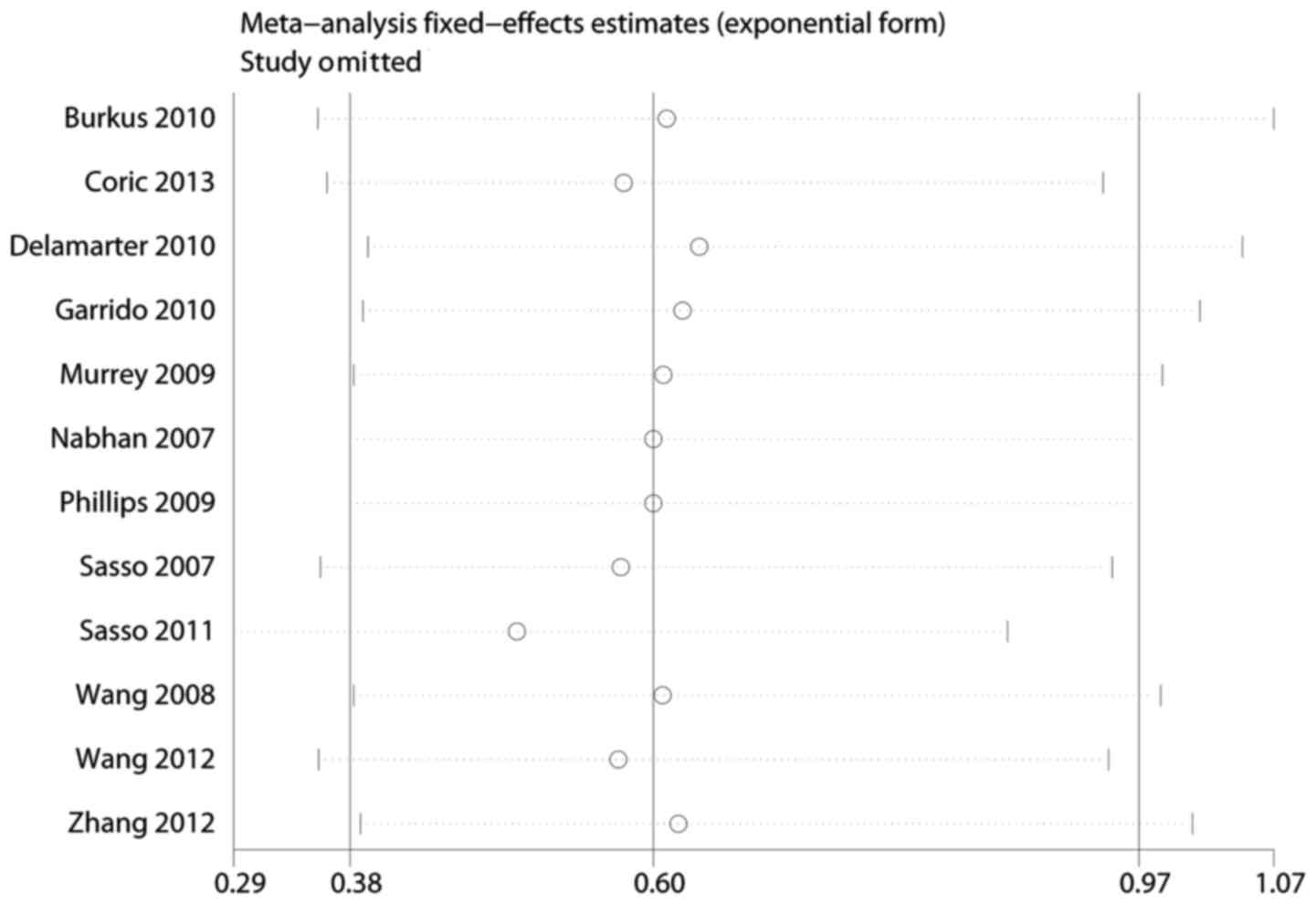
In order to explore the influence of each trial on
the pooled OR, sensitivity analysis was applied. The final
statistical results were not materially altered by the elimination
of any trials in the reoperation rate of adjacent levels following
surgery, as shown in Fig. 8.
For the main indicator of the reoperation rate of
adjacent levels following surgery, cumulative analysis was also
performed according to the publication year of these trials. The
results revealed a stable trend over time, as shown in Fig. 9.
Discussion
To date, two procedures have predominantly featured
in cervical intervertebral disc surgery: ACDF and CDA. ACDF was
first introduced in the 1950s, and since then, this method has been
accepted as a standard procedure by numerous clinical doctors and
scholars in order to treat the disease of vertebrae cervicales. It
has been well established that ACDF has the apparent effect of not
only relieving the spinal cord and the nerve roots' pressure, but
also of reinforcing the cervical vertebrae's stability. However, it
is associated with several side effects, including a high rate of
reoperation of adjacent level following operation (4). Goffin et al (32) identified that ~6–10% of the patients
who were admitted for the ACDF treatment required the operation to
be performed again in the long run. The other procedure, CDA, was
first introduced by Fernstrom (6) in
1966. Since then, other types of artificial cervical intervertebral
disks have been manufactured, including the Bristol/Cummins
(33), Prestige I, Prestige II,
Prestige ST, Bryan, PCM and CerviCore devices. However, CDA remains
one of the most widely accepted candidates for selection in order
to treat cervical spondylosis. In addition, with the passage of
time, several published studies have revealed that there are
certain untoward reactions associated with this procedure,
including heterotopic ossification, which may limit the ROM of the
operation segment following the surgery (7,8).
Several meta analysis studies (34–36) have
already been performed to compare the efficacy and safety of CDA
with ACDF for the treatment of cervical spondylosis. However, the
majority of these included studies with short-term follow-up. In
order to compare the therapeutic effects of these two operation
procedures, particularly with respect to their mid-term efficacy
and safety, the present systematic review was performed, which
included more recently published studies with a longer
follow-up.
In the present study, several important indicators
were analyzed to assess the efficacy of these two procedures after
the mid-term follow-up (at least 24 months). The results indicated
that, following mid-term follow-up, CDA had a higher SF-36 score,
larger ROM at the operational level and a superior rate of
neurological improvement. Furthermore, with respect to other
important indices for evaluation of the effectiveness of CDA and
ACDF, the former was associated with an inferior score of VAS in
neck/arm pain and a lower NDI following the surgery.
To measure the safety of the two procedures, a few
important indicators were assessed in the present study after the
24 months (or longer) follow-up. The results demonstrated that the
prosthesis remained in a good working condition to preserve the
motion at the site of surgery, and the CDA method was associated
with a lower reoperation rate of adjacent levels. By contrast, with
respect to the rate of the total complications in the mid-term
follow-up, no significant differences were observed between the two
operational methods.
In our meta analysis, insignificant differences
between the two methods were observed for other important
indicators, including the age of the patients, blood loss during
the operation and hospital stay. However, a previously published
meta analysis revealed that the CDA group had a longer operative
time and more blood loss compared with the ACDF group (34). To interpret these differences, one may
surmise that, as the number of total operations of CDA has
increased over time, the longer operative times and enhanced levels
of blood loss for arthroplasty reported in the study of Gao et
al (34) may be attributable to
the fact that CDA was, at that time, a novel technique that had not
undergone the improvements that have now been implemented. Our
results indicated that CDA and ACDF were efficient procedures in
the mid-term follow-up.
Finally, in order to check the stability of the
predominant indicators, Begg's and Egger's tests, sensitivity and
cumulative analyses were performed. With regard to the predominant
data (the reoperation rate of adjacent levels following surgery),
the results of the cumulative test, sensitivity analysis and the
shape of the Funnel plots all verified the reliability of the
results in the present study.
The present study had several limitations. First,
only 12 RCTs met our criteria and were therefore finally included.
Secondly, the follow-up period obtained from the studies was
usually 2 years and no more than 4 years, and therefore articles
that feature longer term follow-up in comparing CDA with ACDF would
be required for a more complete analysis. Multicenter, long term
follow-up RCT studies comparing CDA with ACDF are also required for
inclusion in the analysis.
On the basis of the data acquired in the present
study from the mid-term follow-up, it may be concluded that CDA and
ACDF are efficient and safe methods for dealing with cervical
spondylosis. However, with respect to certain, specific indicators,
such as the reoperation rate of adjacent levels following surgery,
the former method has several advantages.
References
|
1
|
Wang C, Tian F, Zhou Y, He W and Cai Z:
The incidence of cervical spondylosis decreases with aging in the
elderly, and increases with aging in the young and adult
population: A hospital based clinical analysis. Clin Interv Aging.
11:47–53. 2016.PubMed/NCBI
|
|
2
|
Que Q, Ye X, Su Q, Weng Y, Chu J, Mei L,
Huang W, Lu R and Zheng G: Effectiveness of acupuncture
intervention for neck pain caused by cervical spondylosis: Study
protocol for a randomized controlled trial. Trials. 14:1862013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Strine TW and Hootman JM: US national
prevalence and correlates of low back and neck pain among adults.
Arthritis Rheum. 57:656–665. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hilibrand AS, Carlson GD, Palumbo MA,
Jones PK and Bohlman HH: Radiculopathy and myelopathy at segments
adjacent to the site of a previous anterior cervical arthrodesis. J
Bone Joint Surg Am. 81:519–528. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Matsumoto M, Okada E, Ichihara D, Watanabe
K, Chiba K, Toyama Y, Fujiwara H, Momoshima S, Nishiwaki Y, Iwanami
A, et al: Anterior cervical decompression and fusion accelerates
adjacent segment degeneration: comparison with asymptomatic
volunteers in a ten year magnetic resonance imaging follow-up
study. Spine. 35:36–43. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fernström U: Arthroplasty with
intercorporal endoprothesis in herniated disc and in painful disc.
Acta Chir Scand Suppl. 357:154–159. 1966.PubMed/NCBI
|
|
7
|
Leung C, Casey AT, Goffin J, Kehr P,
Liebig K, Lind B, Logroscino C and Pointillart V: Clinical
significance of heterotopic ossification in cervical disc
replacement: A prospective multicenter clinical trial.
Neurosurgery. 57:759–763. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Malham GM, Parker RM, Ellis NJ, Chan PG
and Varma D: Cervical artificial disc replacement with ProDisc-C:
Clinical and radiographic outcomes with long-term follow-up. J Clin
Neurosci. 21:949–953. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sasso RC, Anderson PA, Riew KD and Heller
JG: Results of cervical arthroplasty compared with anterior
discectomy and fusion: Four-year clinical outcomes in a
prospective, randomized controlled trial. Orthopedics. 34:8892011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Burkus JK, Haid RW, Traynelis VC and
Mummaneni PV: Long term clinical and radiographic outcomes of
cervical disc replacement with the Prestige disc: results from a
prospective randomized controlled clinical trial. J Neurosurg
Spine. 13:308–318. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lau J, Ioannidis JP and Schmid CH:
Quantitative synthesis in systematic reviews. Annals of internal
medicine. 127:820–826. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Begg CB and Mazumdar M: Operating
characteristics of a rank correlation test for publication bias.
Biometrics. 50:1088–1101. 1994. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sterne JA, Egger M and Smith GD:
Systematic reviews in health care: Investigating and dealing with
publication and other biases in meta analysis. BMJ. 323:101–105.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Copas J and Shi JQ: Meta analysis, funnel
plots and sensitivity analysis. Biostatistics. 1:247–262. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Leimu R and Koricheva J: Cumulative meta
analysis: A new tool for detection of temporal trends and
publication bias in ecology. Proc Biol Sci. 271:1961–1966. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Coric D, Kim PK, Clemente JD, Boltes MO,
Nussbaum M and James S: Prospective randomized study of cervical
arthroplasty and anterior cervical discectomy and fusion with long
term follow-up: results in 74 patients from a single site. J
Neurosurg Spine. 18:36–42. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Delamarter RB, Murrey D, Janssen ME, et
al: Results at 24 months from the prospective, randomized,
multicenter Investigational Device Exemption trial of ProDisc C
versus anterior cervical discectomy and fusion with 4 year
follow-up and continued access patients. SAS journal. 4:122–128.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Garrido BJ, Taha TA and Sasso RC: Clinical
outcomes of Bryan cervical disc arthroplasty a prospective,
randomized, controlled, single site trial with 48 month follow-up.
J Spinal Disord Tech. 23:367–371. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zigler JE, Delamarter R, Murrey D, Spivak
J and Janssen M: ProDisc C and anterior cervical discectomy and
fusion as surgical treatment for single level cervical symptomatic
degenerative disc disease: five year results of a Food and Drug
Administration study. Spine. 38:203–209. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Murrey D, Janssen M, Delamarter R, et al:
Results of the prospective, randomized, controlled multicenter Food
and Drug Administration investigational device exemption study of
the ProDisc C total disc replacement versus anterior discectomy and
fusion for the treatment of 1 level symptomatic cervical disc
disease. Spine J. 9:275–286. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sasso RC, Smucker JD, Hacker RJ and Heller
JG: Clinical outcomes of BRYAN cervical disc arthroplasty: a
prospective, randomized, controlled, multicenter trial with 24
month follow-up. J Spinal Disord Tech. 20:481–491. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nabhan A, Ahlhelm F, Shariat K, et al: The
ProDisc C prosthesis: clinical and radiological experience 1 year
after surgery. Spine. 32:1935–1941. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhang HX, Shao YD, Chen Y, et al: A
prospective, randomised, controlled multicentre study comparing
cervical disc replacement with anterior cervical decompression and
fusion. Int Orthop. 38:2533–2541. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang X, Zhang Y and Xiao S: Medium and
long term result of the single level cervical disc arthroplasty for
cervical spondylosis meylopathy. Zhongguo Ji Zhu Ji Sui Za Zhi.
22:879–883. 2012.(In Chinese).
|
|
25
|
Zhang X, Chen C, Zhang Y, et al:
Randomized, controlled, multicenter, clinical trial comparing BRYAN
cervical disc arthroplasty with anterior cervical decompression and
fusion in China. Spine. 37:433–438. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wang Y, Cai B, Zhang XS, et al: Clinical
outcomes of single level Bryan cervical disc arthroplasty: A
prospective controlled study. Zhonghua Wai Ke Za Zhi. 46:328–0332.
2008.(In Chinese). PubMed/NCBI
|
|
27
|
Riina J, Patel A, Dietz JW, Hoskins JS,
Trammell TR and Schwartz DD: Comparison of single level cervical
fusion and a metal on metal cervical disc replacement device. Am J
Orthop (Belle Mead NJ). 37:E71–E77. 2008.PubMed/NCBI
|
|
28
|
Phillips FM, Allen TR, Regan JJ, et al:
Cervical disc replacement in patients with and without previous
adjacent level fusion surgery: A prospective study. Spine.
34:556–565. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Peng-Fei S and Yu-Hua J: Cervical disc
prosthesis replacement and interbody fusion: A comparative study.
Int Orthop. 32:103–106. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Heller JG, Sasso RC, Papadopoulos SM, et
al: Comparison of BRYAN cervical disc arthroplasty with anterior
cervical decompression and fusion: clinical and radiographic
results of a randomized, controlled, clinical trial. Spine.
34:101–107. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kim SW, Limson MA, Kim SB, Arbatin JJ,
Chang KY, Park MS, Shin JH and Ju YS: Comparison of radiographic
changes after ACDF versus Bryan disc arthroplasty in single and
bi-level cases. Eur Spine J. 18:218–231. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Goffin J, Geusens E, Vantomme N, Quintens
E, Waerzeggers Y, Depreitere B, Van Calenbergh F and van Loon J:
Long term follow-up after interbody fusion of the cervical spine. J
Spinal Disord Tech. 17:79–85. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Porchet F and Metcalf NH: Clinical
outcomes with the Prestige II cervical disc: Preliminary results
from a prospective randomized clinical trial. Neurosurg Focus.
17:E62004. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Gao Y, Liu M, Li T, Huang F, Tang T and
Xiang Z: A meta-analysis comparing the results of cervical disc
arthroplasty with anterior cervical discectomy and fusion (ACDF)
for the treatment of symptomatic cervical disc disease. J Bone
Joint Surg Am. 95:555–561. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yin S, Yu X, Zhou S, Yin Z and Qiu Y: Is
cervical disc arthroplasty superior to fusion for treatment of
symptomatic cervical disc disease? A meta analysis. Clin Orthop
Relat Res. 471:1904–1919. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhang Y, Liang C, Tao Y, Zhou X, Li H, Li
F and Chen Q: Cervical total disc replacement is superior to
anterior cervical decompression and fusion: A meta-analysis of
prospective randomized controlled trials. PLoS One.
10:e01178262015. View Article : Google Scholar : PubMed/NCBI
|