Introduction
Chemicals constitute a part of everyday life.
Approximately 1,000 new chemicals are placed on the market each
year, usually found as mixtures in commercial products, while more
than 100,000 chemical substances are used worldwide (1). Many of these chemicals may, especially
if not properly used, possess hazards for human health and be toxic
to the environment.
The hazards of chemicals can be classified based on
physical, chemical and ecotoxicological endpoints using criteria
developed in the framework of scientific or regulatory processes
(2). A number of national and
international schemes have been developed over the past 50 years.
To avoid multiplicity and confusion at the user level, the globally
harmonized system (GHS) for the classification and labeling of
chemicals was adopted in 1992 during the Rio Earth summit. GHS
includes easily understandable symbols that can be applied in the
manufacture, transport, use and disposal of chemical substances
(2).
At a European Union (EU) level, two Regulations have
been introduced, Regulation (EC) 1907/2006 (REACH) and Regulation
(EC) 1272/2008 aimed to effectively handle hazards and risks from
chemicals. The new EU chemicals legislation applies to all industry
sectors dealing with chemicals along the entire supply chain. It
therefore makes companies responsible for the safety of chemicals
they place on the market.
The CLP Regulation, which is based on GHS, ensures
that the hazards presented by chemicals are clearly communicated to
workers and consumers in the European Union through the
classification and labelling of chemicals. The industry must
establish the potential risks to human health and the environment
of substances and mixtures prior to placing them on the market as
commercial products, by classifying them using the classification,
labelling and packaging (CLP) criteria, in line with the identified
hazards. The need to develop harmonized criteria for classification
is essential in ensuring effective communication of the risk
(3). Hazardous chemicals also have to
be accordingly labeled using hazard and precautionary statements
and pictograms.
In addition, suppliers established in the EU and
placing hazardous products on the market have to provide
standardised information to be used only by Poison Centres (Article
45 of the CLP). The Poison Centres provide medical advice in case
of poisoning due to exposure to hazardous chemicals or to other
toxic agents to the general public and to physicians. Poison
centres in the EU answer on average 600,000 calls for support each
year. However, EU legislation does not specify the precise
information needed for this product notification. Therefore,
varying requirements have been developed by each EU member state
(4).
Safety data sheets (SDSs) are the main communication
tool under the REACH Regulation between suppliers and users of
substances and mixtures and it is a regulatory obligation for the
industry. SDSs include information on the physical, chemical and
hazardous properties of the substance or mixture as well as
instructions for their handling, disposal and transport, and for
first-aid, fire-fighting and exposure control measures.
The aim of the present study was to assess for the
first time, to the best of our knowledge, the level of
comprehension of the hazard and risk communication and awareness
regarding the safe use of chemicals among Greek professional users
and health care specialists eight years after the introduction of
the respective EU legislation.
Materials and methods
A total of 1,500 individuals (850 industrial workers
and professional users of chemicals from 35 different small and
medium enterprises, self-employed professionals included, and 650
health care specialists from 6 public and private hospitals/medical
centres, 40 private practitioners included), in Athens;
Thessaloniki; Larissa; Ionnina; Patras and Heraklion Crete, Greece,
were asked to answer an anonymous validated, self-administered
questionnaire with 26 close-ended questions from May 2016 to April
2017. The questionnaire was left at the reception desk of the
various workplaces, accompanied with an explanatory opening page,
where it was stated that the results of the survey were to be
published. The return of the completed questionnaire was considered
as written consent of the study population. A total of 350
individuals (200 workers and professional users, 150 health care
specialists) returned the questionnaire by placing it in a
specifically marked receptacle at the reception desk of the various
workplaces (return rate 23.3%, in the range of the typical
self-completed surveys) (5).
The questionnaire was developed at the University of
Thessaly, Department of Biochemistry and Biotechnology (Larissa,
Greece) in the framework of the MSc Course on Toxicology and was
structured in three sections. The first section addressed
demographic information (6 questions); the second investigated the
risk/hazard communication of chemicals (14 questions); and the
third explored the use and application of personal protective
measures (6 questions).
Once the questionnaire was constructed, a
multidisciplinary group of professionals that were not
participating in the research group was asked to review the
document and provide input. This expert group consisted of a
toxicologist, a regulatory officer, an officer from the industry
and a psychiatrist. The group provided input on the general content
and face validity of the questionnaire (Content Validity Ratio-CRV
=0.993, P<0.05) (6), which was
proven complete and adequate for distribution.
The 103rd General Assembly of Specific Interest
(09/03/2016) of the Department of Biochemistry and Biotechnology,
University of Thessaly, provided approval for the conduct of the
study and distribution of the questionnaire, as part of the
dissertation theses of the students M.A. and I.K.
Statistical analysis
Statistical analysis was performed using the SPSS
22.0 software (IBM Corp., Armonk, NY, USA). Descriptive data were
calculated as frequencies and percentages. Chi-square
(χ2) tests were computed to reveal meaningful
associations between supplements use and the categorical study
variables (sex and level of education) and Pearson's correlation
was performed for continuous variables (i.e., age and exercise
years). P<0.05 was considered to indicate a statistically
significant difference.
Results
Demographic characteristics
The demographic characteristics of the study
population are shown in Table I.
Professional users (group 1) and health care specialists (group 2)
were of statistically similar age (P=0.323) and work experience
(P=0.224). Women are statistically more in the health care
specialists group, while men dominate the professional workers
group. Twenty different professions were identified in the
participants of group 1, including industrial workers (chemical
products, plastics, pharmaceuticals, food industry and energy
products/fuels), gas station employees, painters, carpenters,
farmers, hairdressers and drivers. The vast majority of these
professions belong to the private sector (>80%). The level of
education in group 1 was significantly lower than 2, as expected.
More specifically, in group 1, 81% of the responders did not go to
University or attend post-graduate courses, whereas in group 2 the
respective value was 29%. Of note is the low percentage of
professional users of chemicals with no diagnosed health problems
(28%), while the prevalence of allergies (skin and respiratory
system) is high in this population (>50%). The picture is
opposite in health care specialists.
 | Table I.Demographical characteristics and
diagnosed health status, type of working activity, work experience
and educational level of the studied population. |
Table I.
Demographical characteristics and
diagnosed health status, type of working activity, work experience
and educational level of the studied population.
| Characteristics | Professional
users | Health care
specialists |
|---|
| Population (no) | 200 | 150 |
| Age (years) | 41.8±7.5 (21–61) | 38.8±9.5 (24–64) |
| Sex |
|
|
| Male | 115 (60) | 55 (37) |
| Female | 85 (40) | 95 (63) |
| Occupation |
|
|
| Workers (private
sector) | 78 (39) |
|
| Workers (public
sector) | 37 (18) |
|
| Self-employed | 85 (42) |
|
| Medical doctors |
| 116 (77)a |
| Nurses |
| 22 (15) |
| Clinical
chemists |
| 12 (8) |
| Working experience
(years) | 12.0±8.80 (1–40) | 16.2±9.78 (5–52) |
| Education |
|
|
| Primary | 42 (21) | 0 (0) |
| Secondary | 74 (37) | 11 (7) |
| Technological | 46 (23) | 33 (22) |
| University | 22 (11) | 63 (42) |
| Post-graduate | 18 (9) | 51 (32) |
| Diagnosed health
problems |
|
|
| None | 56 (28) | 104 (69) |
| Dermatological
problems | 66 (33) | 4 (3) |
| Respiratory
problems | 38 (19) | 4 (3) |
| Musculoskeletal
problems | 20 (10) | 9 (6) |
| Cardiovascular
problems | 4 (2) | 2 (1) |
| Hypertension | 10 (5) | 9 (6) |
| Other | 6 (3) | 18 (12) |
Perception of various GHS
pictograms
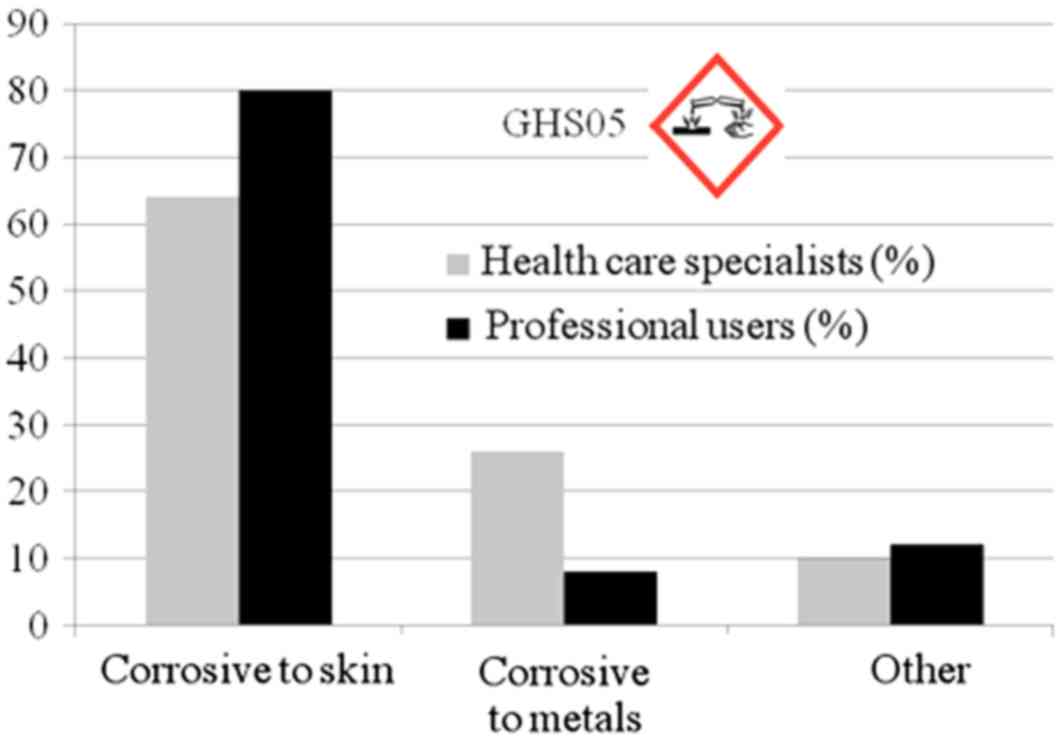
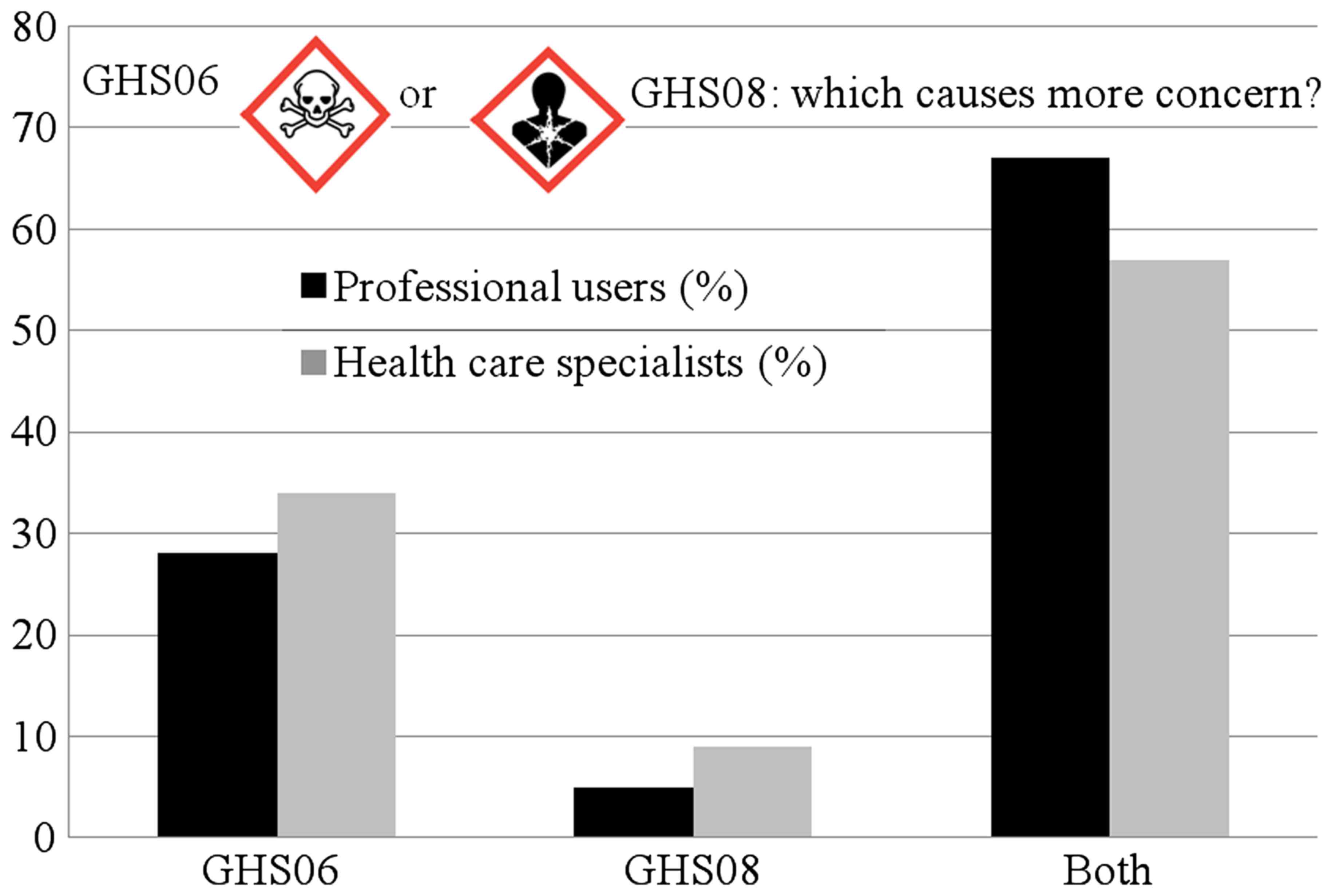
In several issues the two groups had statistically
similar responses. Over 85% of the responders are not aware of the
CLP Regulation per se, while 20% of professional users of chemicals
are aware of the REACH Regulation. Over 65% of the responders did
not notice any changes in the labeling of the products being used.
The most common pictogram encountered is the old hazard symbol of a
black cross on an orange background from the Dangerous
Substances/Products Directives (approximately 40%), which became
obsolete in June 2015. In general, 50–60% of professional users
perceive pictograms adequately, while for health care specialists
the percentage rises to 80%. Nevertheless, both groups understand
only the corrosive hazard for the skin/eyes in pictogram GHS05 and
only 8% in group 1 and 26% in group 2 also comprehended the
corrosivity for metals depicted by the same pictogram (Fig. 1). Over 65% of the responders consider
pictograms GHS06 and GHS08 equally hazardous for human health, but
only 5% in group 1 expect carcinogenicity or reproductive toxicity
to be communicated with the use of GHS08 (Fig. 2).
The majority of the responders (>75%) are aware
of the use of hazardous products during their everyday life, but
the perception of hazard and the severity varies significantly
between the two groups (P=0.012) and statistically depends on the
educational (P=0.022) and professional (P=0.014) level.
Professional users declare that they commonly use flammable liquids
(26%), while 7% declare use of carcinogens and chemicals hazardous
for the environment.
In general, age (P=0.02), work experience (P=0.025)
and profession (P=0.022) significantly correlate with the level of
familiarization with CLP. One third of the professional users
enrolled in this study read the label as the main source of
information for the product, while for health care specialists the
number increased to 65%. A strong correlation was detected with the
educational level of the responders (P=0.017). In both groups a
significant 7% declared that hazard communication through the
labeling of the product is not well understood. Limited use of SDSs
regarding the safe use of chemicals has been observed both in
professional users (18%) and in health care specialists (23%).
The use of personal protective equipment (PPE) is
almost universal in health care specialists with women being more
sensitive (P=0.041), while 25% of the professional users do not use
any PPE. In addition, 30% of the professional users who use PPE, do
so after being instructed by their employer or the shift
supervisor. The most commonly recommended PPE are gloves (50% in
group 1 and 80% in group 2) followed by protective goggles/mask
(35% in group 1 and 15% in group 2). Nevertheless, when it comes to
everyday practice, only gloves are used in group 1. In both groups,
15% of the responders do not take any special precautions regarding
their workware at home, while younger (P=0.015) and more educated
(P=0.035) users of chemicals utilize special cleaning
practices.
Almost 60% of the health care specialists
interviewed have been informed on the safe use of chemicals or
actions to be undertaken in case of accident. In the latter
situation, the National Poisoning Centre is the reference point for
information, whereas 20% of the health care specialists prefer
SDSs.
Discussion
Use of chemicals in the work environment may have
consequences on human health, which influences the protection
measures that need to be employed and the supportive system in case
of accidents or poisonings by health care specialists.
Workers in gas stations are reported to suffer from
headaches (32%) and fatigue (20%) (7). In addition, a statistically significant
increase in red blood cell counts, haemoglobin, mean corpuscular
hemoglobin and platelet counts were found in all self-reported
health-related complaints among liquefied petroleum gas workers
(8). These symptoms are directly
associated with benzene inhalation and workers are found to be
exposed regardless of their position in the gas station (9,10).
The prevalence of respiratory and pulmonary problems
and even cholangiocarcinoma in printing workers is markedly
elevated, with concerns also being applicable for consumers
(11–13). In addition the association between
exposure to chemicals and asthma and rhinitis remains independent
of exposure to dust (14). A
meta-analysis of 13 European cohorts spanning births from 1994 to
2011 indicated that employment during pregnancy in occupations
classified as possibly or probably exposed to endocrine disruptors
was associated with an increased risk of term (15). An association has also been reported
between textile industry and different types of cancer including
lung, bladder, colorectal and breast cancer (16).
In the present study, 72% of professional users of
chemicals face health issues connected to skin and respiratory
sensitisation.
Several studies have attempted to elucidate the
comprehension of the legislation on chemicals and the hazard
communication among workers and the general public (17–21).
Pictograms are the prevailing element in hazard/risk
communication. It has been shown that the underlying core elements
that enhance understanding of GHS pictograms, which are also
essential in developing competent individuals in the use of SDSs,
are training and education (22).
Cleaning workers found not to be familiar with the pictograms had
not been properly informed on the safe usage of chemicals by their
employers (20). Age and educational
level may impact workers' performance and cognitive process of
comprehension of pictograms (19), as
evidenced in the present study. Some pictograms are more easily
perceived, while others remain controversial, such as GHS05, GHS06
and GHS08, as identified in our study. Similar concerns have been
raised regarding the labeling of fragrances (23).
In a meta-analysis of 9 research studies published
from 1983 to 2005 evaluating the relationship between literacy and
hazard communication three main gaps were recognized regarding lack
of learner involvement to improve hazard communication, lack of
employer assessment of employee understanding of training provided,
and lack of studies assessing retention of the material taught and
its application at the worksite (18). In the present study, 30% of the
professional users of chemicals tend to perceive the hazard/risk of
a chemical after instruction by the employer or the shift
supervisor to use PPE. Of note, low PPE compliance persists despite
worker awareness of herbicide exposure risks, potentially as a
result of the influence of the sex dynamics and social culture
(24).
Appropriate work practices and selection and use of
PPE are strongly recommended and measurements at the workplace have
proven the efficacy thereof (25,26).
Nevertheless, use of PPEs is restricted, as observed in the present
study. Farmers that are overexposed to pesticides toxicity do not
use PPE (27). On the other hand,
disposable latex gloves commonly worn by gardeners provide
inadequate protection even for contact with pesticides over a short
period of time (28). Thus, more
emphasis should be given on awareness-raising activities and
increase of the communication of chemicals hazard/risk.
Health care specialists are expected to use PPE more
extensively to protect themselves from infectious diseases and
pathogens (29,30). Nevertheless, these PPEs are not
adequate for protection from chemicals and lack of compliance is
evident regarding PPEs, even among medical technicians (31). Consequently, the observed almost
universal use of PPEs by health care specialists in the present
study is potentially misleading. Regarding compliance of the
medical staff engagement of the personnel in auditing PPE use and
reporting activities may significatnly improve compliance (32).
Health care specialists are often asked to treat
cases that are linked with exposure to different chemicals. In the
present study, 60% of responders were informed regarding the safe
use of chemicals or actions to be undertaken in case of accident.
In the latter situation, the National Poisoning Centre is
considered the reference point for information for the vast
majority of medical doctors. However, the National Poisoning
Centers are less often consulted when emergency poisonings are
treated in the primary or tertiary care centers (33). Data legally required to be declared to
National Poisoning Centers should be harmonized within EU and the
new regulatory framework, which is the primary aim of these legal
frameworks (34,35).
In conclusion, on a national level,
awareness-raising campaigns are imperative (36,37), in
collaboration with trade unions and health care professional
associations, in order to alert professionals regarding the safe
use of chemicals to protect human health and the environment.
References
|
1
|
Shukla KP, Singh NK and Sharma S:
Bioremediation: developments, current practices and perspectives.
Genet Eng Biotechnol J. 3:1–20. 2010.
|
|
2
|
Winder C, Azzi R and Wagner D: The
development of the globally harmonized system (GHS) of
classification and labelling of hazardous chemicals. J Hazard
Mater. 125:29–44. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Morita T and Morikawa K: Expert review for
GHS classification of chemicals on health effects. Ind Health.
49:559–565. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Brekelmans P, de Groot R, Desel H, Mostin
M, Feychting K and Meulenbelt J: Harmonisation of product
notification to Poisons Centres in EU Member States. Clin Toxicol.
51:65–69. 2013. View Article : Google Scholar
|
|
5
|
Petróczi A, Naughton DP, Mazanov J,
Holloway A and Bingham J: Performance enhancement with supplements:
Incongruence between rationale and practice. J Int Soc Sports Nutr.
4:192007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cohen J: Statistical power analysis for
the behavioral sciences. 2nd edition. Lawrence Erlbaum Associates;
Hillsdale, NJ: 1988, View Article : Google Scholar
|
|
7
|
Sairat T, Homwuttiwong S, Homwutthiwong K
and Ongwandee M: Investigation of gasoline distributions within
petrol stations: Spatial and seasonal concentrations, sources,
mitigation measures, and occupationally exposed symptoms. Environ
Sci Pollut Res Int. 22:13870–13880. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sirdah MM, Al Laham NA and El Madhoun RA:
Possible health effects of liquefied petroleum gas on workers at
filling and distribution stations of Gaza governorates. EMHJ.
19:289–294. 2013.PubMed/NCBI
|
|
9
|
Moura-Correa MJ, Jacobina AJ, dos Santos
SA, Pinheiro RD, Menezes MA, Tavares AM and Pinto NF: Exposure to
benzene in gas stations in Brazil: Occupational health surveillance
(VISAT) network. Cien Saude Colet. 19:4637–4648. 2014.(In
Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fenga C, Gangemi S, Giambò F, Tsitsimpikou
C, Golokhvast K, Tsatsakis A and Costa C: Low-dose occupational
exposure to benzene and signal transduction pathways involved in
the regulation of cellular response to oxidative stress. Life Sci.
147:67–70. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Karimi A, Eslamizad S, Mostafaee M, Momeni
Z, Ziafati F and Mohammadi S: Restrictive pattern of pulmonary
symptoms among photocopy and printing workers: A retrospective
cohort study. J Res Health Sci. 16:81–84. 2016.PubMed/NCBI
|
|
12
|
Pirela SV, Lu X, Miousse I, Sisler JD,
Qian Y, Guo N, Koturbash I, Castranova V, Thomas T, Godleski J, et
al: Effects of intratracheally instilled laser printer-emitted
engineered nanoparticles in a mouse model: A case study of
toxicological implications from nanomaterials released during
consumer use. NanoImpact. 1:1–8. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sato Y, Kubo S, Takemura S, Sugawara Y,
Tanaka S, Fujikawa M, Arimoto A, Harada K, Sasaki M and Nakanuma Y:
Different carcinogenic process in cholangiocarcinoma cases
epidemically developing among workers of a printing company in
Japan. Int J Clin Exp Pathol. 7:4745–4754. 2014.PubMed/NCBI
|
|
14
|
Schyllert C, Rönmark E, Andersson M,
Hedlund U, Lundbäck B, Hedman L and Lindberg A: Occupational
exposure to chemicals drives the increased risk of asthma and
rhinitis observed for exposure to vapours, gas, dust and fumes: A
cross-sectional population-based study. Occup Environ Med.
73:663–669. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Birks L, Casas M, Garcia AM, Alexander J,
Barros H, Bergström A, Bonde JP, Burdorf A, Costet N, Danileviciute
A, et al: Occupational exposure to endocrine-disrupting chemicals
and birth weight and length of gestation: A European meta-analysis.
Environ Health Perspect. 124:1785–1793. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Singh Z and Chadha P: Textile industry and
occupational cancer. J Occup Med Toxicol. 11:392016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sathar F, Dalvie MA and Rother HA: Review
of the literature on determinants of chemical hazard information
recall among workers and consumers. Int J Environ Res Public
Health. 13:132016. View Article : Google Scholar
|
|
18
|
Bouchard C: Literacy and hazard
communication: Ensuring workers understand the information they
receive. J AAOHN. 55:18–25. 2007. View Article : Google Scholar
|
|
19
|
Beaufils E, Hommet C, Brault F, Marqué A,
Eudo C, Vierron E, De Toffol B, Constans T and Mondon K: The effect
of age and educational level on the cognitive processes used to
comprehend the meaning of pictograms. Aging Clin Exp Res. 26:61–65.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Martí Fernández F, van der Haar R, López
López JC, Portell M and Torner Solé A: Comprehension of hazard
pictograms of chemical products among cleaning workers. Arch Prev
Riesgos Labor. 18:66–71. 2015.(In Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Vaillancourt R, Pouliot A, Streitenberger
K, Hyland S and Thabet P: Pictograms for safer medication
management by health care workers. Can J Hosp Pharm. 69:286–293.
2016.PubMed/NCBI
|
|
22
|
Ta GC, Mokhtar MB, Mohd Mokhtar HA, Ismail
AB and Abu Yazid MF: Analysis of the comprehensibility of chemical
hazard communication tools at the industrial workplace. Ind Health.
48:835–844. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Klaschka U: The hazard communication of
fragrance allergens must be improved. Integr Environ Assess Manag.
9:358–362. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Andrade-Rivas F and Rother HA: Chemical
exposure reduction: Factors impacting on South African herbicide
sprayer's personal protective equipment compliance and high risk
work practices. Environ Res. 142:34–45. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ceballos DM, Whittaker SG, Lee EG, Roberts
J, Streicher R, Nourian F, Gong W and Broadwater K: Occupational
exposures to new dry cleaning solvents: High-flashpoint
hydrocarbons and butylal. J Occup Environ Hyg. 13:759–769. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Park H, Park HD and Jang JK: Exposure
characteristics of construction painters to organic solvents. Saf
Health Work. 7:63–71. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Quinteros E, Ribó A, Mejía R, López A,
Belteton W, Comandari A, Orantes CM, Pleites EB, Hernández CE and
López DL: Heavy metals and pesticide exposure from agricultural
activities and former agrochemical factory in a Salvadoran rural
community. Environ Sci Pollut Res Int. 24:1662–1676. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Beránková M, Hojerová J and Peráčková Z:
Estimated exposure of hands inside the protective gloves used by
non-occupational handlers of agricultural pesticides. J Expo Sci
Environ Epidemiol. 27:625–631. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Honda H and Iwata K: Personal protective
equipment and improving compliance among healthcare workers in
high-risk settings. Curr Opin Infect Dis. 29:400–406. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Gralton J, Rawlinson WD and McLaws ML:
Health care worker's perceptions predicts uptake of personal
protective equipment. Am J Infect Control. 41:2–7. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Dukic K, Zoric M, Pozaic P, Starcic J,
Culjak M, Saracevic A and Miler M: How compliant are technicians
with universal safety measures in medical laboratories in
Croatia?-A pilot study. Biochem Med. 25:386–392. 2015. View Article : Google Scholar
|
|
32
|
Hennessy KA and Dynan J: Improving
compliance with personal protective equipment use through the model
for improvement and staff champions. Clin J Oncol Nurs. 18:497–500.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Schurter D, Rauber-Lüthy C, Jahns M,
Haberkern M, Kupferschmidt H, Exadaktylos A, Eriksson U and Ceschi
A: Factors that trigger emergency physicians to contact a poison
centre: Findings from a Swiss study. Postgrad Med J. 90:139–143.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Settimi L, Orford R, Davanzo F, Hague C,
Desel H, Pelclova D, Dragelyte G, Mathieu-Nolf M, Adams R and
Duarte-Davidson R: Development of a new categorization system for
pesticides exposure to support harmonized reporting between EU
Member States. Environ Int. 91:332–340. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
de Groot R, Brekelmans P, Desel H and de
Vries I: New legal requirements for submission of product
information to poisons centres in EU member states. Clin Toxicol.
Jun 23–2017.(E-pub ahead of print).
|
|
36
|
Walsh C: CLP activities and control in
Ireland. Ann Ist Super Sanita. 47:165–170. 2011.PubMed/NCBI
|
|
37
|
Pistolese P and Scimonelli L: CLP
Regulation and REACH Regulation: Links, implementation and control
in Italy. Ann Ist Super Sanita. 47:157–164. 2011.PubMed/NCBI
|