Introduction
In the past, due to the limited understanding of
hemorrhoid pathogenesis, freezing and laser therapy were usually
applied to treat hemorrhoids, which have been gradually eliminated
because of high expense and poor therapeutic effect (1). The rise of the anal cushion down
hypothesis has led to greater understanding of hemorrhoid resulting
in the use of novel operation methods (2). Previous investigations focused on the
Milligan-Morgan operation, a procedure for prolapse and hemorrhoids
(PPH), and Doppler ultrasound-guided hemorrhoidal arterial ligation
(DG-HAL). The latter is a widely applied operation method in
western countries (3,4). The procedures of DG-HAL are
comparatively safe, constituting this method as the most effective
method for hemorrhoid (5). However,
there are inevitable complications including postoperative
secondary hemorrhage, infection, anal edge edema and pain, and the
long-term effect remains to be clarified (5,6).
At present, there are no uniform criteria for
surgery selection for hemorrhoids. Clinicians therefore aim to
improve surgical methods and develop a novel surgical operation
method. ‘Tying, binding and fixing operation’ was suggested by
Huang et al (7), which is the
creative application based on the ‘bound therapy’ in Traditional
Chinese Medicine (TCM). The method involves an operation based on
the two etiological theories of varicosity and anal cushion down,
which can not only improve varicosity but also restore and repair
the anal cushions. The ‘tying, binding and fixing operation’ theory
has been accepted to a certain extent, although sufficient clinical
evidence is lacking.
In the current study, we selected DG-HAL, a widely
applied and accepted method in western countries, as the control to
compare the therapeutical effect of the TCM ‘tying, binding and
fixing operation’ in treating hemorrhoids, post-operative
complication, length of hospital stay and hospitalization cost. The
therapeutical effect, feasibility and safety were also evaluated.
The results indicated that this is a promising technique.
Patients and methods
Patients
A total of 160 patients with severe mixed
hemorrhoids admitted to the Department of Anorectal Surgery, Xin
Hua Hospital Affilliated to Shanghai Jiao Tong University School of
Medicine (Shanghai, China) between June 2012 and June 2013 were
selected. The digital rectal exam and anoscopy were used to
evaluate the hemorrhage, prolapse and volume of internal
hemorrhoid. Inclusion criteria for the study were: i) Age, 18–70
years; ii) patients conformed to the diagnostic criteria of mixed
hemorrhoid (8,9), and the internal hemorrhoid was degree
III–IV; iii) the blood routine test, urine routine test, liver and
kidney function examination were normal; and iv) there were no
systemic diseases and other anorectal disease, such as anal
fissure, anal fistula, and anorectal tumor. Patients conforming to
the above criteria received information and education, which
introduced the principle and advantages of DG-HAL and the ‘tying,
binding and fixing operation’, the universality of DG-HAL and the
innovativeness of the ‘tying, binding and fixing operation’ method.
A total of 160 cases were voluntarily included in this clinical
experiment, and all 160 patients provided signed informed consent
for participation in the study. The 160 patients were randomly
divided into the experimental group (tying, binding and fixing
operation) and the control group (DG-HAL) with 80 cases in each
group. The gender, age, degree of internal hemorrhoid and disease
course were not statistically different (P>0.05) between the two
groups, which were comparable (Table
I).
 | Table I.General clinical data for two
groups. |
Table I.
General clinical data for two
groups.
| Item | Experimental group
(n=80) | Control group
(n=80) | t/χ2
value | P-value |
|---|
| Gender,
male/female | 43/37 | 47/33 | 5.327 | 1.518 |
| Age, year | 53.16±12.16 | 51.74±12.63 | 2.736 | 3.527 |
| Degree of internal
heamorrhoids, case |
|
| 6.724 | 1.196 |
| III | 55 | 51 |
|
|
| IV | 25 | 29 |
|
|
| Disease course,
month |
84.49±101.56 |
95.16±107.75 | 4.629 | 2.117 |
| RBC count,
×1012/l | 4.6 | 4.5 |
|
|
| Hb count, g/l | 98 | 100 |
|
|
Approval for the study was obtained from the ethics
committee of Xin Hua Hospital.
Operation method
Preoperative preparation
Patients of the two groups were required not to
consume a solid diet from 8:00 p.m. onwards. Prior to sleep, warm
saline was used for cleansing enema, and the morning that surgery
was performed, patients received enema of warm saline. The lumbar
anesthesia was used for anesthesia, and the position was lithotomy
position.
Experimental group
The anus was disinfected and sufficiently dilated,
and when the finger touched the hemorrhoid artery, the 2-0
absorbable suture of 5/8 radian was used for transfixion, and the
prolapsed hemorrhoid was compressed and pushed to the anatomic
site. The needle was entered from 0.3 to 0.5 cm above the dentate
line, and exited the hemorrhoids from the other side to make an ‘8’
suture. The hemorrhoids were pushed and compressed, and the ‘8’
suture was made at 1.3–1.5 cm above the dentate line. For larger
hemorrhoids, the ‘8’ suture was made at 2.3–2.5 cm above the
dentate line. Following transfixion, pushing, compression and
transfixion, the prolapsed hemorrhoids were completely fixed above
the dentate line.
Control group
After the anus was disinfected and dilated, a
Doppler ultrasound anoscope and probe (AMI Co., Feldkirch, Austria)
were inserted. When the probe was inserted to 2.0–3.0 cm above the
dentate line, it was rotated along the vertical axis of rectum and
anus, and the sound from the Doppler detector and the arterial
signal on the screen were observed. After finding the artery, 2-0
absorption suture was used for the ‘8’ suture. The anoscope was
rotated by 360° to ligate the hemorrhoidal arteries, after which
the probe was rotated again to examine the ligation effect. After
the hemorrhoidal arteries were examined, the probe and anoscope
were removed.
Postoperative management
The patients in the two groups received intestinal
mucosa protector (titanoreine suppository), and the dressing was
changed in the morning and evening or after defecation daily.
Following the operation, cefuroxime was intravenously injected for
48–72 h to prevent the infection. Following the operation, the
patients were requested to remain in bed, and had liquid food on
the same day. Patients followed a normal diet after 24 h.
Drugs and equipments
Titanoreine suppository, generic name: Compound
Carraghenates Suppositories (Xian-Janssen Pharmaceutical Co., Ltd.,
Xian, China). Cefuroxime sodium for injection was purchased from
Beijing Pharmaceutical Co., Ltd. (Beijing, China). HAL-Doppler II
Doppler diagnostic apparatus and the matched anoscope were
purchased from AMI.
Observational indicators and follow-up
Observational indicators for the study were: i)
Conditions during the operation, the operative time, the
intraoperative blood loss; ii) evaluation indicators of therapeutic
effect: hemorrhage, prolapse improvement, and shrinkage of
hemorrhoid volume, the preservation of anal function and
satisfaction degree survey; iii) length of stay and hospitalization
cost; iv) postoperative complications: secondary hemorrhage,
infection, thrombogenesis, anal enema, pain and urination; and v)
1-year reoccurrence rate.
The patients were observed for 7–10 days after
surgery. After 7–10 days of surgery, the anus surrounding was
inspected. The patient did not undergo digital rectal examination
to avoid tearing of the suture. At 1 month following surgery, the
patient underwent digital rectal examination and an anoscope was
used to identify hemorrhage, prolapse and hemorrhoids, which were
compared with pre-operative conditions to observe improvement of
the symptoms in order to evaluate the therapeutic effect. The
condition of anal function preservation was recorded to survey the
satisfaction degree of the therapeutic effect. The postoperative
complications of patients after 3 months were recorded, the pain
and urination on the 1st day were evaluated, the anal enema
condition on the 3rd day was evaluated (pain mostly occurs on the
1st day, while an enema mostly occurs on the 3rd day). The
reoccurrence condition of the hemorrhoid was followed up, and
hemorrhoids that conformed to the diagnosis and treatment of
hemorrhoids were diagnosed as reoccurrence.
Evaluation criteria
Operative effect
The effect was evaluated according to the
hemorrhage, improvement of prolapse, and shrinkage of hemorrhoid
volume: i) Recover indicated >90% symptoms or physical symptoms
disappear; ii) effective indicated >50% symptoms or physical
signs disappear; and iii) invalid indicated <50% symptoms and
physical signs disappear.
Determination of postoperative pain, enema and
urinary retention
Scoring criteria were: i) No indicated no pain of
wound surface when defecation and changing dress, no enema of wound
surface, and urination was fluent without discomfort; ii) mild
indicated a slight discomfort when defecation and changing dress,
the edema area was ≤1/4 of anus surrounding area, and slight
discomfort during urination; iii) moderate indicated pain on the
wound surface that was alleviated when defecation and changing
dress, patients were required to take analgesic, the edema area was
1/4-1/2 of the anus surrounding area, and there was obvious
difficulty during urination, albeit catheterization was not
compulsory; and iv) severe indicated severe pain of wound surface,
patients required to take strong analgesics such as dolantin or
morphine, the edema area was >1/2 of anus surrounding area, and
urination was difficult, requiring catheterization.
Statistical analysis
SPSS 19.1 software (IBM SPSS, Armonk, NY, USA) was
used to analyze the data. Quantitative data, such as age, disease
course and operative time, were presented as mean ± standard
deviation, and the t-test was used for comparison among groups.
Enumerated data such as gender, stage and some postoperative
complications, were analyzed using the χ2 test. Data in
the two groups were classified as: therapeutic effect, satisfaction
degree and some postoperative complications; these were analyzed by
Wilcoxon rank-sum test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Analysis of typical case
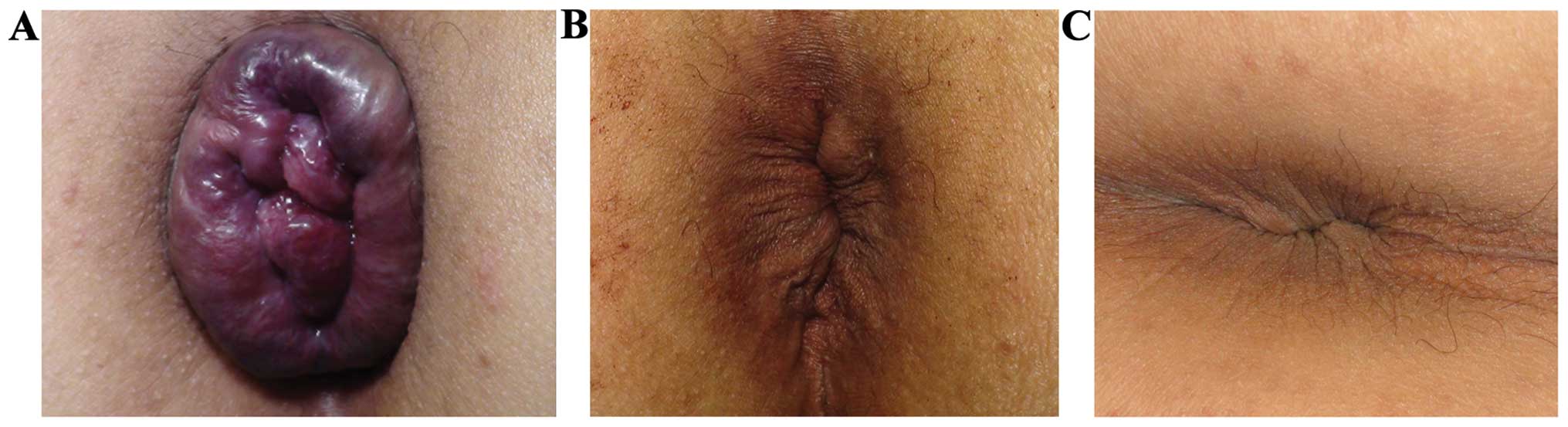
Analysis of typical cases in the two groups is shown
in Figs. 1 and 2.
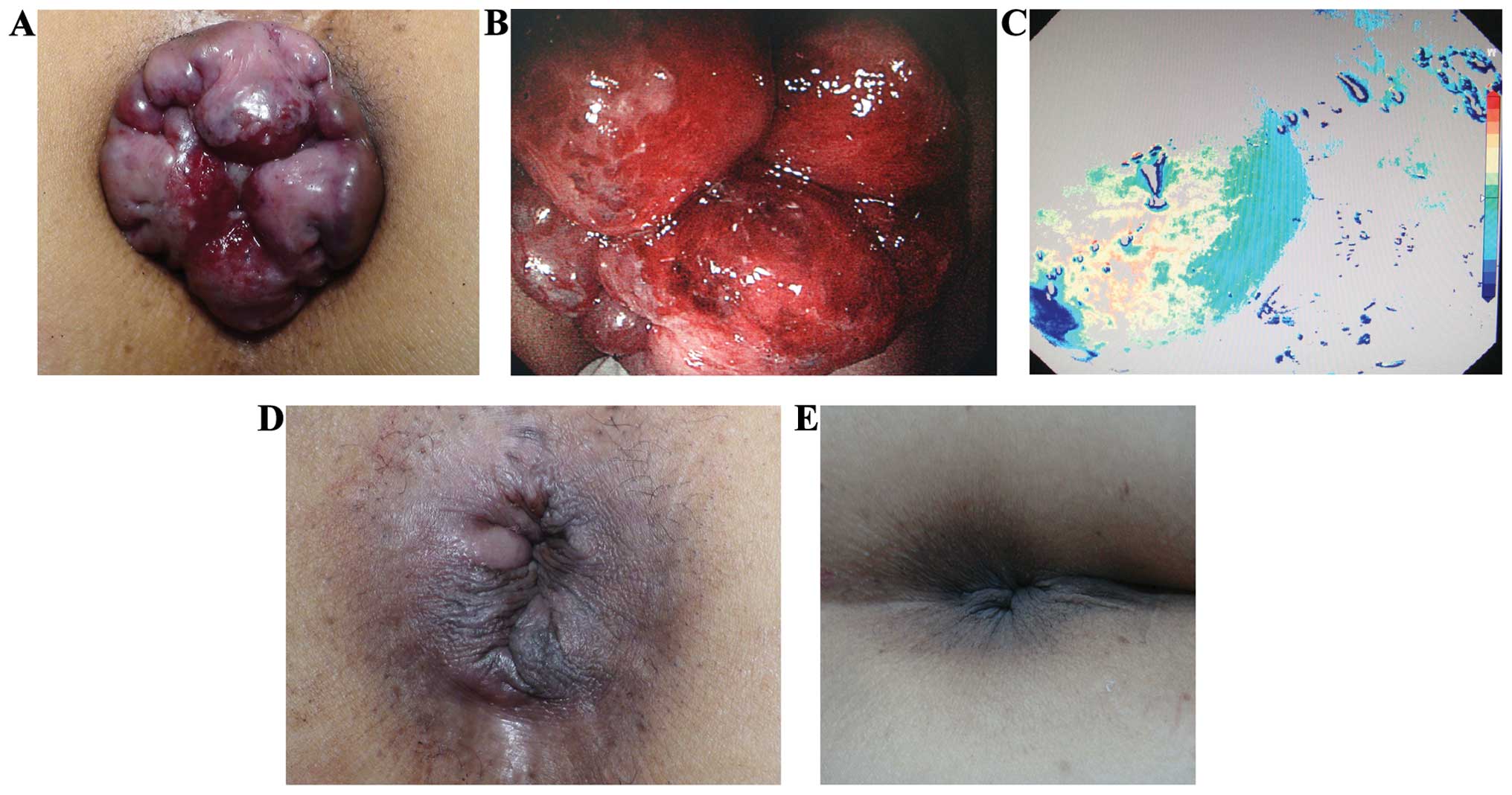
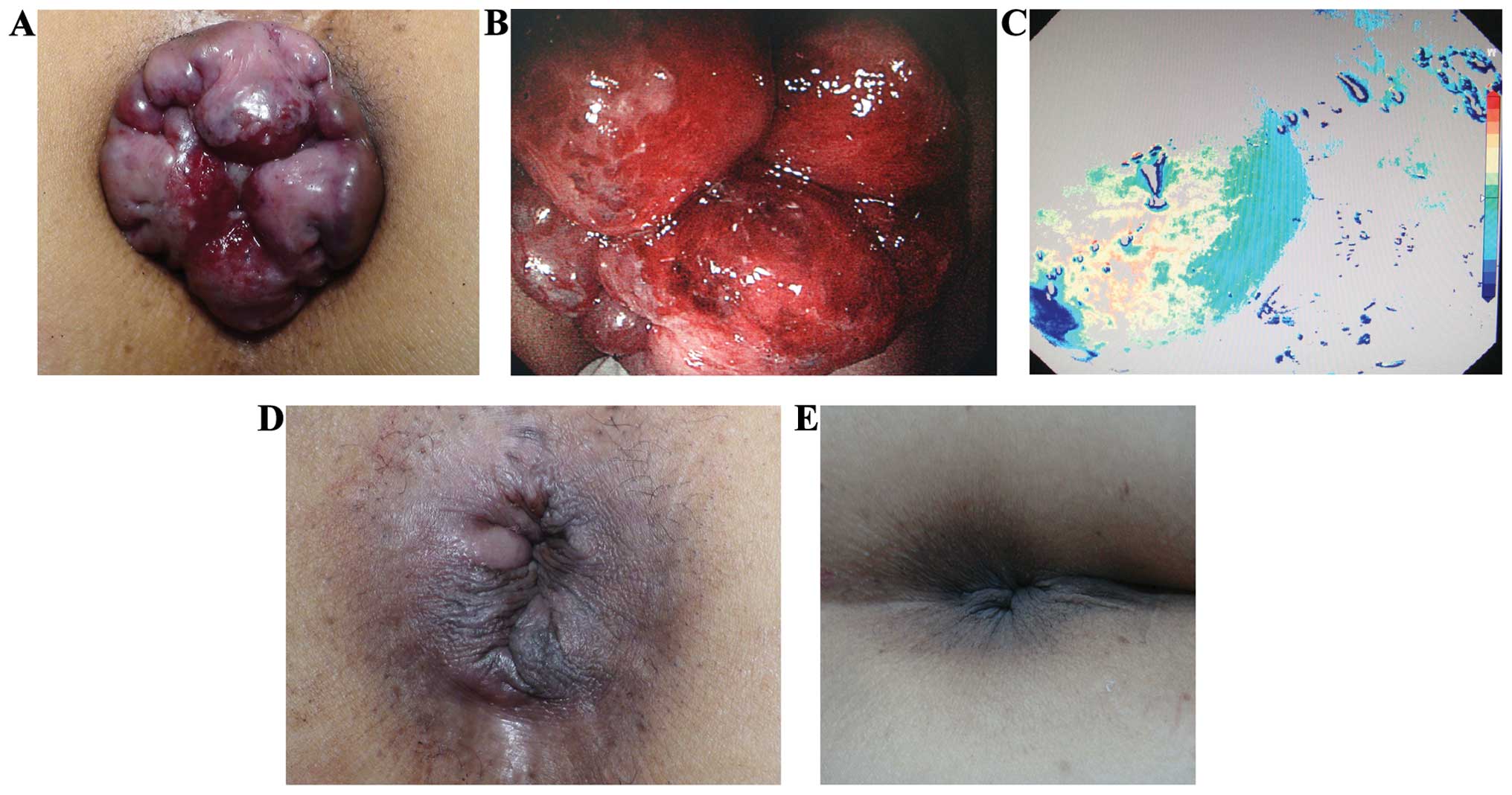 | Figure 2.Therapeutic effect of DG-HAL. (A)
Female, 62 years of age exhibiting severe mixed hemorrhoids.
Internal hemorrhoids were degree V, there were obvious hemorrhage
and prolapse symptoms, and the volume of hemorrhoids was 2.6
cm3. (B) Anoscope examination, there were ≥3
hemorrhoids, the total volume was around 2.6 cm3, and
there was diffuse erosion and hemorrhage on the surface. (C)
Hemorrhoidal artery can be accurately and rapidly localized by the
signal on the screen of Doppler ultrasound equipment. (D) At 8 days
after the operation, hemorrhage and prolapsed symptoms disappeared,
there was moderate varicosity on external hemorrhoid, and the
hemorrhoid was invisible. (E) At 1 month after operation, there was
no hemorrhage, the prolapsed and varicosity of external
hemorrhoidal varicosity were improved with slight skin tag, and
there was no secondary hemorrhage or infection. |
The experimental group included a 58-year-old male
patient with complication of anal skin tag for 10 years. The anal
lump prolapsed for 3 years, and could be returned spontaneously or
by hand to the anal canal. In the last 2 weeks the symptoms were
aggravated, the blood in stool was increased showing fresh red
color and had a teardrop shape, the prolapsed tissue could not be
returned spontaneously or by hand to the anal canal. A physical
examination showed that there was dark violet circularity goiter,
edema of skin surface, with hard texture and pressing pain. There
was prolapse of internal hemorrhoids, which could be returned by
hand. Anoscopy examination showed that the volume of hemorrhoids
was ~1.2 cm3, there was mucous membrane erosion at
points 5 and 7. The blood routine test showed red blood cells (RBC)
3.50×1012/l, and hemoglobin (Hb) 109 g/l. The
diagnosis was severe mixed haemorrhoids, the degree of hemorrhoids
was degree IV, and there was slight anemia. There was no severe
disease history in the past. Patients received ‘tying, binding and
fixing operation’ at the Xin Hua Hospital Affilliated to Shanghai
Jiao Tong University School of Medicine (Fig. 1), the operation duration time was ~45
min, the intraoperative blood loss was ~8.5 ml, there was no
obvious hemorrhage in stool and no hemorrhoid prolapse at 3 days
after operation, and the pain was alleviated. The patient was
discharged on the 4th day and the hospitalization cost was ~700
dollars. In the follow up, the hemorrhage and prolapse symptoms
disappeared, the hemorrhoids were almost disappeared, there was no
reoccurrence within 1 year and no adverse effect on defecation. The
blood routine test was recovered and the patient was satisfied with
the therapeutic effect.
The control group included a 62-year-old female,
with complication of hematochezia for 10 years. The anal lump
prolapsed for 5 years, but could be returned spontaneously and by
hand to the anal canal. In the last 1 month, the symptoms were
aggravated, the prolapsed tissue could not be returned with
intolerable pain. Physical examination showed a dark violet mass
around the anus, and prolapse of internal hemorrhoids and
hemorrhage on the surface were obvious. The texture was hard and
there was compressing pain. There were ≥3 hemorrhoids that could
not be returned by hand to the anal canal. The anoscopy examination
showed that there was diffuse erosion and hemorrhage on the surface
of hemorrhoids, and the hemorrhoids volume was 2.6 cm3.
The blood routine test showed RBC 3.0×1012/l, and Hb 88
g/l. The patient was diagnosed as having severe mixed hemorrhoids,
the internal hemorrhoids degree was degree IV, and had moderate
anemia. The patient had no severe disease history, and underwent
DG-HAL surgery (Fig. 2), with an
operation time of ~20 min. Blood loss during operation was ~7.5 ml,
the prolapse symptoms disappeared at 3 days after the operation,
although there was obvious edema around anus, a little blood and
obvious pain when defecation. After 8 days of operation, the
prolapse symptom disappeared and there was moderate varicosity on
external hemorrhoids after which the patient was discharged. The
total hospitalization cost was ~1,400 dollars. After 1 month follow
up, there was no hemorrhage or prolapse symptom, the external
varicosity was improved, and there was only slight skin tag without
secondary hemorrhage or infection. There was no reoccurrence within
1 year and no dysporia, the anemia was improved and the patient was
satisfied.
Conditions during operation and operative effect. In
the comparison of conditions during operation, the average
operative time of the experimental group (35.57±6.17) was
significantly higher than that of the control group (12.73±4.92).
There was no significant difference in the intraoperative blood
loss between the two groups (P>0.05) (Table II).
 | Table II.Comparison of the conditions in
operation. |
Table II.
Comparison of the conditions in
operation.
| Conditions in
operation | Experimental
(n=80) | Control group
(n=80) | T-value | P-value |
|---|
| Operation duration
time, min | 35.57±6.17 | 12.73±4.92 | 13.693 | 0.000 |
| Blood loss, ml |
8.52±4.61 |
6.35±3.28 |
0.713 | 8.652 |
The therapeutic effect showed no significant
difference in improving hemorrhage symptoms of the two groups
(P>0.05). However, regarding improvement of prolapse symptoms
and reduction of the volume of hemorrhoids, the experimental group
was significantly better than the control group. There was no anal
function damage in the two groups (Table III). The 1-year reoccurrence rate
(22.5%) in the control group was significantly higher than that in
the experimental group (2.5%) (Table
III).
 | Table III.Comparison of operative efficacy and
length of stay between the two groups. |
Table III.
Comparison of operative efficacy and
length of stay between the two groups.
| Item | Experimental group
(n=80) | Control group
(n-80) |
t/χ2/T-value | P-value |
|---|
| Hemorrhage
symptom |
|
|
1.758a | 5.763 |
|
Recover | 38 | 35 |
|
|
|
Effective | 33 | 38 |
|
|
|
Invalid | 9 | 7 |
|
|
| Prolapse |
|
| 11.976a | 0.008 |
|
Recovery | 47 | 24 |
|
|
|
Effective | 29 | 30 |
|
|
|
Invalid | 4 | 26 |
|
|
| Shrinkage of
hemorrhoid volume |
|
| 13.779a | 0.006 |
|
Recovery | 36 | 25 |
|
|
|
Effective | 34 | 22 |
|
|
|
Invalid | 10 | 33 |
|
|
|
Preservation of anal
function | 80 | 80 |
|
|
| Satisfaction
degree |
|
|
9.751a | 0.001 |
| Very
satisfied | 16 | 7 |
|
|
|
Satisfied | 38 | 12 |
|
|
|
Ordinary | 22 | 46 |
|
|
|
Unsatisfied | 4 | 15 |
|
|
| Length of stay |
5.18±1.79 | 5.98±2.18 |
4.217b | 0.985 |
| Hospitalization
cost |
5,334.77±875.54 |
8,551.81±1,806.54 |
8.436b | 0.025 |
| Reoccurrence | 2 | 18 | 17.752c | 0.000 |
Postoperative complications
Postoperative complications were followed up,
perianal pain and urination were observed on the 1st day, anal
edema was observed on the 3rd day, and the other complications were
observed within 3 months. The incidences of perianal pain, anal
edema and dysuria between the two groups were not significantly
different (P>0.05), and <7% patients were severe. The above
complications disappeared spontaneously or following treatment
(Table IV). There were 10 cases of
secondary bleeding and 18 cases of infection in the experimental
group, 12 cases of secondary hemorrhage and 14 cases of infection
in the control group. However, the differences between the two
groups were not statistically significant (P>0.05). Infection
was alleviated spontaneously or following treatment, the incidence
rate of local hematoma in the experimental group (1.2%) was
significantly lower than that in the control group (15.0%)
(Table IV).
 | Table IV.Comparison of postoperative
complications between the two groups. |
Table IV.
Comparison of postoperative
complications between the two groups.
| Postoperative
complications | Perianal pain | Anal edema | Dysuresia | Secondary
hemorrhage | Infection | Local hematoma |
|---|
| Experimental group
(n=80) |
|
|
| 10 | 18 | 1 |
| No | 37 | 33 | 30 |
|
|
|
|
Mild | 32 | 32 | 35 |
|
|
|
|
Moderate | 9 | 10 | 14 |
|
|
|
|
Severe | 2 | 5 | 2 |
|
|
|
| Control group
(n=80) |
|
|
| 12 | 14 | 12 |
| No | 40 | 35 | 32 |
|
|
|
|
Mild | 30 | 31 | 26 |
|
|
|
|
Moderate | 6 | 13 | 19 |
|
|
|
|
Severe | 4 | 2 | 3 |
|
|
|
|
χ2/T-value |
8.754a | 6.579a |
5.557a |
2.113b |
5.773b | 18.926b |
| P-value | 0.857 | 1.372 | 1.569 | 6.187 | 1.897 |
0.000 |
Hospitalization cost
The length of hospital stay in the two groups was
not significantly different (P>0.05). However, the
hospitalization cost in the experimental group was significantly
lower than that of the control group (5,334.77±875.54 vs.
8,551.81±1,806.54, P=0.025), and the satisfaction degree was
significantly higher than the control group (Table III).
Discussion
There is insufficient clinical practice criteria for
the ‘tying, binding and fixing operation’ method to examine its
potential therapeutic effect in severe mixed hemorrhoids and
evaluate its clinical value. In the present study, we used DG-HAL,
which is commonly applied and recognized in western countries, as
the control to compare the effect in the surgical treatment of
hemorrhoids, postoperative complication, length of stay and
hospitalization cost, and assess the therapeutic effect and
safety.
A comparison of the therapeutic effect in the two
groups with regard to the ‘tying, binding and fixing operation’
method was significantly better than that of DG-HAL, mainly
manifesting as improvement of prolapse symptoms and shrinkage of
hemorrhoid volume. Previously, it was reported that in DG-HAL,
hemorrhoidal arteries are ligated to effectively block the bleeding
vessels, thus DG-HAL has a positive effect on hemorrhage symptoms
(8). However, this method is not
able to induce the degeneration of chronic hemorrhoid tissues and
obvious prolapsed hemorrhoids cannot completely shrink following
the establishment of collateral circulation, which leads to an
increase in pressure of hemorrhoids tissue. Consequently, it is not
good at improving prolapse symptoms and decreasing hemorrhoid
volume (4–6,9–12). It has been reported that DG-HAL and
PPH have good therapeutic effect, however, the effect for
hemorrhoids with prolapse symptoms is poor, which demonstrated the
limit of therapeutical treatment including DG-HAL (13,14). In
this study, the hemorrhoidal artery was also ligated in ‘tying,
binding and fixing operation’ to decrease the pressure of
hemorrhoidal tissue, which was similar to DG-HAL in improving
hemorrhage symptoma. Additionally, during the operation the reseted
anal cushion was ligated by absorbable suture, which was the
foreign matter stimulus to cause local aseptic inflammation and
gradual fibrosis of mucosa, and further repair the anal cushion at
the normal anatomical position. This improves the symptom of
prolapse; the creative point of this method was that the
hemorrhoids were continuously compressed, pushed and ligated, which
was the same as the TCM ‘bound therapy’ (15). The aim was to block the superficial
hemorrhoidal vein to ensure deep blood circulation, which improves
blood stasis and varicosity. There was also small thrombus
formatted in the tissue between two sutures due to the long-term
compression. Thus, the aseptic inflammation and suspension effect
of the anal cushion were enhanced, which has a better effect in
improving prolapse symptoms and reducing hemorrhage symptoms than
the control group. The two groups had good effects in preserving
anal function because the surgical trauma was little and the anal
cushion tissue was not damaged, and suture and ligation were
completed above the dentate line to avoid the stimulus to somatic
nerve (16), thus its effect on
defecation controlling was small. The reoccurrence rate of the
control group was higher than that of the experimental groups,
possibly due to the fact that although DG-HAL has good effect on
hemostasis, the effect on improving hemorrhoid volume prolapse and
reducing hemorrhoid volume was poor. Thus, the prolapsed tissue was
not completely atrophic, and following the establishment of
collateral circulation, the blood and pressure in hemorrhoid
tissues were increased, and the risk of vein flexion and anal
cushion moving down was increased (17). This led to the reoccurrence risk
being increased and the satisfaction degree decreased. As DG-HAL
was completed under the guidance of Doppler ultrasound, the
hemorrhoidal artery was accurately located, which was significantly
shortened the operative time.
However, due to the application of Doppler
ultrasound equipment, the hospitalization cost was 600 dollars
higher than the ‘tying, binding and fixing operation’ method, which
may affect the independent choice of patients in the future.
Except the formation of local hematoma, the other
complications were not statistically different between the two
groups. The occurrence rates of perianal pain, uroschesis after 1
day in the two groups and the moderate and severe anal edema were
10–20%, which may be improved spontaneously or after treatment, and
there was no severe adverse event. The ‘tying, binding and fixing
operation’ method and DG-HAL were minimally invasive operations,
compared with the conventional Milligan-Morgan operation, the
trauma was small and the operation was above the dentate line.
Thus, the patients recovered rapidly and the length of stay was
significantly reduced, theoretically the anal pain and discomfort
caused by trauma was avoided (4,18).
However, practically because anal dilatation was not complete, it
caused skin split or a clip was used to clip the perianal skin
during operation; thus, postoperative perianal pain was inevitable.
The anal edema was mainly considered to be associated with the
operation, and 90% of the edema can disappear as recovery from the
disease. The dysuresia was considered to be associated with lumbar
anesthesia, and the pain stimulus to anus reflectively caused
urethral sphincter muscle contraction to induce uroschesis
(19). After observation, 95% of
uroschesis disappears with alleviation of pain. There was an
infection rate and secondary hemorrhage in the two groups.
Postoperative infection was considered to be due to the special
infection susceptibility of anus (20), however, it can be controlled by
antibiotics. The secondary hemorrhage manifested as sticky bloody
stool, which was considered to be related to mucosa damage,
ischemic inflammatory necrosis, constipation and suture tear caused
by hard stool (21,22). However, the hemorrhage was not
severe, and it was suggested that patients at the Department of
Anorectal Surgery following a light diet, with more fiber to avoid
the secondary damage caused by constipation and hard stool. In the
present study, 15% patients in the control group had local
hematoma, however, there was no hematoma in the experimental group.
The difference may be linked to the principles of the two methods.
In the ‘tying, binding and fixing operation’ method, arterial blood
can be prevented from entering the hemorrhoid tissue, and the
venous blood can be extruded from the tissue to improve blood
stasis. The absorbable suture is used to hang the hemorrhoids to
rectum wall near to anus (7), which
can improve the prolapse symptoms and effectively decrease the risk
of local hematoma formation.
In the present study, ‘tying, binding and fixing
operation’ is a promising method for the treatment of hemorrhoids,
and is better than DG-HAL in improving the prolapse and reducing
the volume of hemorrhoids. There were less postoperative
complications, the anal function was not affected, the risk of
hematoma formation and reoccurrence was significantly decreased,
the postoperative satisfaction degree was improved and the
hospitalization cost was significantly reduced.
Although there are many advantages, the ‘tying,
binding and fixing operation’ may cause complications such as pain
and secondary hemorrhage. As a novel method, there may be potential
risks that have not been identified. There was an optimal effect in
this study, however, this was just the primary step of ‘tying,
binding and fixing operation’ application clinically. Future
studies are therefore required to fully evaluate the clinical value
of this method.
Acknowledgements
The present study was supported by Fund of Shanghai
Sanitary Bureau (no. 2010L011A).
References
|
1
|
Higuero T: Hemorrhoids. Rev Prat.
64:867–874. 2014.(In French). PubMed/NCBI
|
|
2
|
Henderson PK and Cash BD: Common anorectal
conditions: Evaluation and treatment. Curr Gastroenterol Rep.
16:4082014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cerato MM, Cerato NL, Passos P, Treigue A
and Damin DC: Surgical treatment of hemorrhoids: A critical
appraisal of the current options. Arq Bras Cir Dig. 27:66–70. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Testa A and Torino G: Doppler-guided
hemorrhoidal artery ligation (DG-HAL): A safe treatment of II–III
degree hemorrhoids for all patients. Could it be potentially also
good prophylaxis? Minerva Chir. 65:259–265. 2010.PubMed/NCBI
|
|
5
|
Ratto C: THD Doppler procedure for
hemorrhoids: The surgical technique. Tech Coloproctol. 18:291–298.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gomez-Rosado JC, Sanchez-Ramirez M,
Capitan-Morales LC, Valdes-Hernandez J, Reyes-Diaz ML,
Cintas-Catena J, Guerrero-Garcia JM, Galan-Alvarez J and
Oliva-Mompean F: One year follow-up after doppler-guided
haemorrhoidal artery ligation. Cir Esp. 90:513–517. 2012.(In
Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Huang H, Yao Y and Ding M: Clinical
observation of blocking and fixing operation for mixed hemorrhoids
with severe complications. Shanghai J Trad Chin Med. 44:45–46.
2010.
|
|
8
|
Ahmad A, Kant R and Gupta A: Comparative
analysis ofdoppler guided hemorrhoidal artery ligation (DG-HAL) and
infrared coagulation (IRC) in management of hemorrhoids. Indian J
Surg. 75:274–277. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lohsiriwat V: Approach to hemorrhoids.
Curr Gastroenterol Rep. 15:3322013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Buntzen S, Christensen P, Khalid A,
Ljungmann K, Lindholt J, Lundby L, Walker LR, Raahave D and Qvist
N: Danish Surgical Society: Diagnosis and treatment of
haemorrhoids. Dan Med J. 60:B47542013.PubMed/NCBI
|
|
11
|
Pol RA, van der Zwet WC, Hoornenborg D,
Makkinga B, Kaijser M, Eeftinck Schattenkerk M and Eddes EH:
Results of 244 consecutive patients with hemorrhoids treated with
Doppler-guided hemorrhoidal artery ligation. Dig Surg. 27:279–284.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
de Wallis Vries BM, van der Beek ES, de
Wijkerslooth LR, van der Zwet WC, van der Hoeven JA, Eeftinck
Schattenkerk M and Eddes EH: Treatment of grade 2 and 3 hemorrhoids
with Doppler-guided hemorrhoidal artery ligation. Dig Surg.
24:436–440. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shi J, Jin J and Li J: Clinical
observation on barron ligation and blocking and fixing operation in
treatment of mixed hemorrhoids. J Liaoning Univ Trad Chin Med.
16:188–190. 2014.
|
|
14
|
Khafagy W, El Nakeeb A, Fouda E, Omar W,
Elhak NG, Farid M and Elshobaky M: Conventional haemorrhoidectomy,
stapled haemorrhoidectomy, Doppler guided haemorrhoidectomy artery
ligation; post operative pain and anorectal manometric assessment.
Hepatogastroenterology. 56:1010–1015. 2009.PubMed/NCBI
|
|
15
|
Zhang ZJ: effects of ‘Tying, binding and
fixing operation’ in the treatment of mixed hemorrhoids: 40 cases
reports. Chin Health Care and Nutrition. 12:7077. 2013.
|
|
16
|
Hall JF: Modern management of hemorrhoidal
disease. Gastroenterol Clin North Am. 42:759–772. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Altomare DF and Giuratrabocchetta S:
Conservative and surgical treatment of haemorrhoids. Nat Rev
Gastroenterol Hepatol. 10:513–521. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Langley GB and Sheppeard H: The visual
analogue scale: Its use in pain measurement. Rheumatol Int.
5:145–148. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Joshi GP and Neugebauer EA: PROSPECT
Collaboration: Evidence-based management of pain after
haemorrhoidectomy surgery. Br J Surg. 97:1155–1168. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Slauf P, Antoš F and Marx J: Complications
of hemorrhoids. Rozhl Chir. 93:223–225. 2014.(In Czech). PubMed/NCBI
|
|
21
|
Lienert M and Ulrich B: Doppler-guided
ligation of the hemorrhoidal arteries. Report of experiences with
248 patients. Dtsch Med Wochenschr. 129:947–950. 2004.(In German).
PubMed/NCBI
|
|
22
|
Zhu J, Ding JH, Zhao K, Zhang B, Zhao Y,
Tang HY and Zhao YJ: Complications after procedure for prolapse and
hemorrhoids for circular hemorrhoids. Zhonghua Wei Chang Wai Ke Za
Zhi. 15:1252–1255. 2012.(In Chinese). PubMed/NCBI
|