Introduction
Omeprazole is one of the most commonly clinically
used proton pump inhibitors (PPIs), which can selectively and
non-competitively inhibit the H+/K+-ATP
enzyme in parietal cell membranes, and can act for 24 h for lasting
effects (1,2). It is widely used in the clinic for the
treatment of peptic ulcer, gastroesophageal reflux disease,
Zollinger Ellison syndrome, infections caused by Helicobacter
pylori, gastrointestinal bleeding and nonsteroidal
anti-inflammatory drug-induced gastric mucosal injuries (2–6).
A number of adverse reactions caused by omeprazole
have been reported, including allergic reactions, tachycardia,
alimentary tract hemorrhage, liver damage, leucopenia, mental
disorders and joint pain (7–18). In the present study, a patient
developed allergic shock, significant drug eruption and severe
diarrhea following the oral administration of omeprazole. This
report reminded doctors and pharmacists that pharmaceutical care of
PPIs should be strengthened in future work.
Case report
A 61-year-old female was admitted to The First
Affiliated Hospital of Bengbu Medical College (Bengbu, Anhui,
China) on May 4, 2015 as a result of experiencing a whole-body rash
for 10 days, diarrhea for 7 days, and unconsciousness and oliguria
for 1 day. The patient had been diagnosed with hyperthyroidism 30
years ago, but was not administered a formal treatment or
monitored. The patient had been experiencing arthritic pain for
>1 month and had received an intra-articular injection and oral
administration of non-steroidal anti-inflammatory drugs (NSAIDs),
but the exact drug was unknown. The patient was prescribed 20 mg
twice daily and orally of omeprazole enteric-coated tablets (ECT;
Kaikaii Yuansheng Pharmaceutical Co., Ltd, Xinyang, China) to treat
the stomach discomfort caused by these NSAIDs. However, the patient
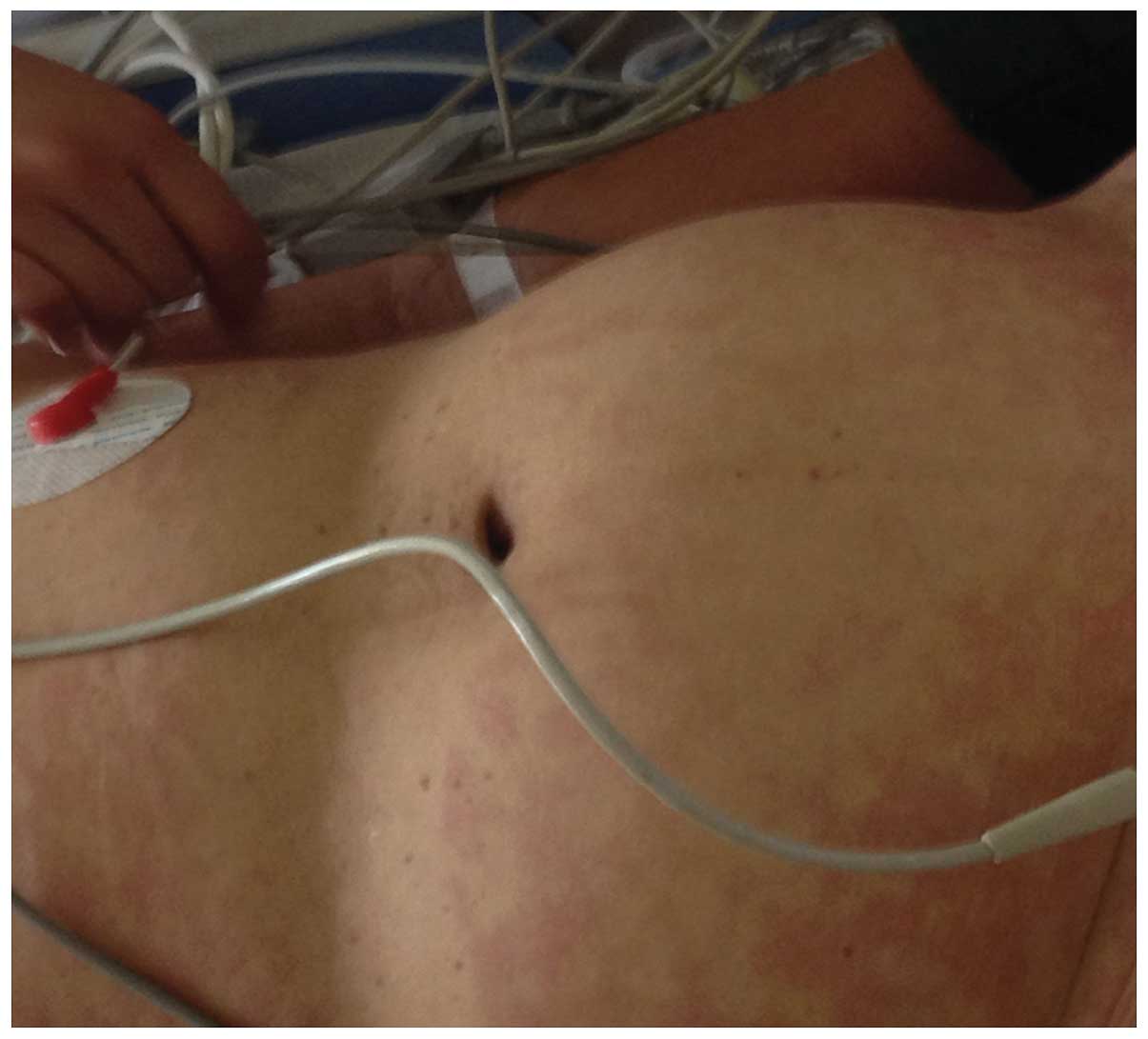
developed a whole-body rash 7 days after omeprazole administration,
which was 10 days before admission. This rash did not disappear
following anti-allergy treatment at a local clinic on April 24,
2015 (Fig. 1). The patient also
experienced diarrhea >10 times a day, and nausea and vomiting
from 7 days prior to admission. The patient's diarrhea was treated
with an infusion of unknown drugs 2 days prior to admission at the
local Suzhou Municiple Hospital on May 2, 2015 but demonstrated no
marked improvement in symptoms. The patient developed a high fever
reaching 40°C, 1 day prior to admission, and was transferred the
Intensive Care Unit (ICU) to continue treatment for low blood
pressure and oliguria. The patient was treated with 20 mg
norepinephrine (Wuhan Yuanda Pharmaceutical Co., Ltd, Wuhan, China)
intravenously once per day to treat low blood pressure, and
furosemide injection (40 mg) was administered intravenously once
per day to cure oliguria. Norepinephrine activates the alpha
receptor, then induces the small artery and vein blood vessel to
contract and thus increases the blood pressure. The patient lost
consciousness and her condition did not improve following treatment
for allergies and a fluid infusion of 20 mg norepinephrine was
pumped into the blood intravenously once per day in order to
increase blood pressure. Norepinephrine activates the α-receptor,
then induces the small artery and small vein blood vessel to
contract and finally increases the blood pressure.
The patient was then transferred to the ICU
department of The First Affiliated Hospital of Bengbu Medical
College on May 4, 2015 for further treatment as described below. A
tracheal intubation with mechanical ventilation was performed due
to the patient's loss of consciousness and dyspnea. Blood gas
analysis revealed severe metabolic acidosis and electrolyte
disturbance of pH 6.86, PaCO2 41 mmHg, PaO2
120 mmHg, HCO3− 7.1 mmol/l, BE−
26.1 mmol/l, Na+ 134.7 mmol/l, K+ 2.26 mmol/l
and Ca2+ 0.93 mmol/l. Fluid infusion, correcting
acid-base disturbance (by sodium bicarbonate injection) and other
treatment, including calcium and potassium supplements, calcium
gluconate injection (Yunan Baiyao Group Co., Ltd., Kunming, China)
and potassium chloride injection (Hebei Kelun Pharmaceutical Group
Co., Ltd., Xiantao, China). Admission examination results were as
follows: Temperature, 37°C; pulse, 117 times/min; respire, 34
times/min; blood pressure, 106/56 mmHg; and Glasgow score, 3
(19,20). The patient maintained a whole-body
rash and did not respond to loud noise or physical stimuli, but did
respond to pain stimulation induced by piercing with a needle,
meaning that the central nervous system functioned normally. The
patient's pupils measured 1 mm and did not react to light. The
patient's breath sounded rough and rale upon lung auscultation as
determined by a stethoscope, but was not obviously dry.
Electrocardiogram monitoring (model DASH5000; GE Healthcare Life
Sciences, Chalfont, UK) showed a regular sinus rhythm (heart rate,
117 beats/min) and no cardiac murmur. The abdomen was soft and the
patient demonstrated no presence of pain when it was pressed. The
liver and spleen were small enough to feel by doctors, implying
that their function is normal, and bowel movement sounds could be
heard. No obvious edema was observed in the four limbs, but the
patient presented with oliguria. A routine blood test indicated
that the patient's white blood cell (WBC) count had increased, and
neutrophils (NEUTs) were not measured (WBC, 32.67×109
cells/l; hemoglobin, 127 g/l; hematocrit, 34%; platelet,
386×109 platelets/l). The results led to the following
symptom identification: i) Allergic shock; ii) pulmonary infection
and respiratory failure; iii) acute kidney injury; iv) metabolic
acidosis; v) electrolyte disturbance, hypokalemia and hypocalcemia;
vi) hyperthyroidism; and vii) diarrhea.
The patient was administered 500 ml glucose and
sodium chloride injection and 500 ml polygeline injection both
intravenously. A total of 20 mg norepinephrine was also
administered intravenously by a drip once per day in order to
maintain blood pressure. 2.25 g piperacillin sodium (Haerbin
Pharmaceutical Group Co., Ltd, Haerbin, China) and tazobactam
sodium (Haerbin Pharmaceutical Group Co., Ltd) were both
administered intravenously three time per day for antibiotic
treatment upon admission to the ICU of The First Affiliated
Hospital of Bengbu Medical College on May 4th. In addition, blood
filtration was performed for acute kidney injury, 3.0 g calcium
gluconate injection once daily and 6.0 g 10% potassium chloride
injection once daily were administered to treat electrolyte
disturbance, hypokalemia and hypocalcemia. Furthermore, 6.0 g
montmorillonite powder (Hunan Fangsheng Pharmaceutical Group Co.,
Ltd., Changsha, China) was injected through the nose three times a
day and 2.0 g triple viable Bifidobacterium lactobacillus
(Shanghai Xinyi Pharmaceutical Group Co., Ltd., Shanghai, China)
were administered through the npse three times a day in order to
treat diarrhea and regulate intestinal flora. Loperamide
hydrochloride (Xian Janssen Pharmaceutical Ltd., Hefei, China)
capsules at 4.0 g were administered through the nose once per day
to inhibit intestinal motility, as the patient was experiencing
diarrhea >10 times a day. Furthermore, an injection of 80 mg
methylprednisolone sodium succinate (Belgium Pharmacia The Upjohn
Company, Shanghai, China) was administered intravenously once per
day and 80 mg compound ammonium glycyrrhetate S (Jincheng Haisi
Pharmaceutical Group Co., Ltd., Jincheng, China) was administered
intravenously once per day for anti-allergy treatment. The patient
was diagnosed with diarrhea, allergic shock caused by omeprazole,
and omeprazole enteric-coated tablet-induced rash following a
consultation between the Departments of Pharmacy and
Gastroenterology on May 5th. Blood gas analysis on May 7th
demonstrated a blood pH 7.48, PaCO2 35.5 mmHg,
PaO2 61.5 mmHg, BE 2.9 mmol/l, Na+ 142.3
mmol/l, K+ 3.42 mol/l and LAC 2.3 mmol/l. The patient's
metabolic acidosis had been treated, but lactic acid levels
remained high, which highlighted that there remained an obstruction
to circulatory function, and a poor oxygenation index of ~100 mmHg.
A routine blood test on May 7th returned the following results:
WBC, 9.49×109 cells/l; NEUT, 84.1%; red blood cell
count, 3.79×1012 cells/l; hemoglobin, 119.00 g/l;
hematocrit, 0.33; and platelet count, 72×109
platelets/l. The routine blood test and body temperature (37.0°C)
revealed a significant attenuation of the infection; a sputum smear
revealed dysbacteriosis, and diarrhea, and the patient was
administered norvancomycin by a nasal tube. On May 8th, the patient
demonstrated marked deflorescence and a normal urine output, which
indicated a significant improvement in kidney function. The patient
stopped experiencing diarrhea on May 13th, after which her
condition began to stabilize. Genetic screening revealed that the
patient had a poor metabolism of omeprazole. Therefore, the severe
adverse reactions (omeprazole enteric-coated tablet-induced rash,
diarrhea and allergic shock) experienced by the patient were
hypothesized to be caused by the accumulation of omeprazole
metabolites in vivo. Informed consent was obtained from the
patient's family.
Discussion
In the current case, family members reported that
the patient only experienced stomach discomfort following the oral
administration of NSAIDs, and that the patient's severe adverse
reactions described above developed after administering omeprazole.
As the patient's symptoms significantly improved when the
administration of omeprazole was discontinued and treatment for
these symptoms was provided, this reveals a relationship between
the severe adverse reactions and the administration of omeprazole.
There are multiple reports describing allergic shock caused by
omeprazole, the majority of which occur during the infusion of
omeprazole in the clinic (1,3,4).
However, to the best of our knowledge, a case of severe adverse
reactions, in particular severe diarrhea (>10 times a day with a
stool quantity of ~3000–5000 ml per day) following the oral
administration of omeprazole has not been reported. The adverse
reactions appeared 7 days after omeprazole was first administered,
which suggests that these adverse reactions may be caused by the
accumulation of omeprazole metabolites in vivo. Research has
demonstrated that the pharmacokinetics of omeprazole in vivo
is primarily determined by the cytochrome P450 2C19
(CYP2C19) gene. CYP2C19 proteins are divided into slow and
fast metabolizers (21,22). If patients are slow metabolizers, it
will lead to the accumulation of omeprazole metabolites in
vivo, which induce adverse reactions (13,14).
Based on this, genetic screening of the patient was performed, and
it was revealed that the patient was a slow metabolizer of
omeprazole. In more detail, cell and tissue fluorescence
quantitative PCR was performed and CYP2C19 was affected. This
result verifies the speculation that the severe adverse reactions
experienced by the patient were caused by the accumulation of
omeprazole metabolites in vivo.
In the clinic previously, a patient presented with
dermatitis exfoliativa ~1 month after being administered
lansoprazole and esomeprazole on an alternate basis (23). All of these other rare and severe
adverse reactions mentioned in the present study following
administration of PPIs highlight that clinicians, in particular
clinical pharmacists, must carefully regulate pharmaceutical
treatment with PPIs. In recent years, with the increasing use of
PPIs, a number of novel severe adverse reactions are being
gradually discovered (15–18,23). In
particular, the overuse of PPIs in the clinic has become
problematic (24–26). A review of PPI prescriptions by
pharmacists revealed that the primary reasons underlying PPI
overuse are its prescription to patients who should not take it,
excessive dosing frequencies and long treatment duration (26).
If PPIs are not used reasonably it may cause a
series of consequences, including adverse reactions and drug
resistance. If PPIs are used reasonably by the doctors. the life
cycle of the drug can be extended. The regulated use of PPIs mainly
depends on the following two aspects: Whether the clinicians can
judge the therapeutic effects accurately; and whether the dosage
regimen utilised by clinical pharmacists is appropriate. Due to the
current lack of specific and detailed clinical guidelines regarding
PPIs, clinicians and pharmacists should develop and optimize PPIs
using certain criteria that will gradually aim at solving the main
problems with usage of PPIs in the hospital. Pharmacists master the
therapeutic indications of PPIs accurately in cooperation with
physicians and pay attention to pharmaceutical care. The clinical
application of PPIs should be monitored and performed as follows:
PPIs should be administered as a short course of treatment;
de-escalation therapy of acid inhibition should be used
specifically; the usage of PPIs should be based on the results of
gastroscopy examination; and regular risk assessment should be used
if the PPI treatment duration is long. De-escalation therapy of
acid inhibition means that PPIs are used for several weeks to
inhibit gastric acid secretion, then H2-receptor blocking drugs
such as ranitidine and famotidine should be used to continue
inhibiting gastric acid secretion. Alternatively PPIs are given
intravenously following oral administration. According to the
gastroscopy results, duodenal ulcer, gastric ulcer, gastric mucosal
injury and chronic gastritis are favorable for PPI use. If these
recommendations are carefully followed by medical staff, patients
may benefit from the use of PPIs.
References
|
1
|
Labenz J and Malfertheiner P: Treatment of
uncomplicated reflux disease. World J Gastroenterol. 11:4291–4299.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zeng Y, Ye Y, Liang D, Guo C and Li L:
Meta-analysis of the efficacy of lansoprazole and omeprazole for
the treatment of H.pylori-associated duodenal ulcer. Int J
Physiol Pathophysiol Pharmacol. 7:158–164. 2015.PubMed/NCBI
|
|
3
|
Wedemeyer RS and Blume H: Pharmacokinetic
drug interaction profiles of proton pump inhibitors: An update.
Drug Saf. 37:201–211. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Watson C, Zhu L, Guan S, Machen TE and
Forte JG: Reaction of proton pump inhibitors with model peptides
results in novel products. J Pharmacol Sci. 122:213–222. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Solana MJ, López-Herce J, Sánchez A,
Sánchez C, Urbano J, López D and Carrillo A: 0.5 mg/kg versus 1
mg/kg of intravenous omeprazole for the prophylaxis of
gastrointestinal bleeding in critically ill children: A randomized
study. J Pediatr. 162:776–782. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ivey KJ: Mechanisms of nonsteroidal
anti-inflammatory drug-induced gastric damage. Actions of
therapeutic agents. Am J Med. 84:41–48. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Abdul Razzak E, Tomás M, Tornero P and
Herrero T: Nine cases of allergy to omeprazole. J Investig Allergol
Clin Immunol. 22:228–230. 2012.PubMed/NCBI
|
|
8
|
Pirson F, Geubel A and Marot L: Late
hypersensitivity to omeprazole and other proton pump inhibitors.
Acta Clin Belg. 67:301–303. 2012.PubMed/NCBI
|
|
9
|
Stefanaki EC, Vovolis V, Letsa I and
Koutsostathis N: Anaphylactic reaction to omeprazole. Am J
Gastroenterol. 103:1581–1583. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Reyes Balaguer J, Campos Andreu A and
Hernández Fernández de Rojas D: Anaphylaxis to proton pump
inhibitors. Med Clin (Barc). 128:7992007.(In Spanish). PubMed/NCBI
|
|
11
|
Ramírez E, Cabañas R, Laserna LS, Fiandor
A, Tong H, Prior N, Calderón O, Medrano N, Bobolea I, Frías J and
Quirce S: Proton pump inhibitors are associated with
hypersensitivity reactions to drugs in hospitalized patients: A
nested case-control in a retrospective cohort study. Clin Exp
Allergy. 43:344–352. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Reimer C and Bytzer P: Adverse events
associated with long-term use of proton pump inhibitors. Ugeskr
Laeger. 174:2289–2293. 2012.(In Danish). PubMed/NCBI
|
|
13
|
Shimura S, Hamamoto N, Yoshino N,
Kushiyama Y, Fujishiro H, Komazawa Y, Furuta K, Ishihara S, Adachi
K and Kinoshita Y: Diarrhea caused by proton pump inhibitor
administration: Comparisons among lansoprazole, rabeprazole, and
omeprazole. Curr Ther Res Clin Exp. 73:112–120. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Femer RE and Allison TR: Omeprazole
overdose. Hum Exp Toxicol. 12:541–542. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
El-Matary W and Dalzell M:
Omeprazole-induced hepatitis. Pediatr Emerg Care. 21:529–530. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Beutler M, Hartmann K, Kuhn M and Gartmann
J: Arthralgias and omeprazole. BMJ. 309:16201994. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kraus A and Flores-Suárez LF: Acute gout
associated with omeprazole. Lancet. 345:461–462. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Odou P, Martin P, Membré S, Gressier B,
Tamiji L, Dine T, Luyckx MM, Brunet C, Dehee D and Moulron S:
Omeprazole-induced leukopenia. A case report. J Clin Pharm Ther.
24:317–321. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Osler T, Cook A, Glance LG, Lecky F,
Bouamra O, Garrett M, Buzas JS and Hosmer DW: The differential
mortality of Glasgow Coma Score in patients with and without head
injury. Injury. April 22–2016.(Epub ahead of print) doi:
10.1016/j.injury.2016.04.016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kasprowicz M, Burzynska M, Melcer T and
Kübler A: A comparison of the full outline of unresponsiveness
(FOUR) score and Glasgow Coma Score (GCS) in predictive modelling
in traumatic brain injury. Br J Neurosurg. 30:211–220. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shiohira H, Yasui-Furukori N, Tateishi T
and Uno T: Chairal assay of omeprazole and metabolites and its
application to a pharmacokinetics related to CYP2C19 genotypes. J
Chromatogr B Analyt Technol Biomed Life Sci. 879:2465–2470. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Serrano D, Torrado S, Torrado-Santiago S
and Gisbert JP: The influence of CYP2C19 genetic polymorphism on
the pharmacokinetics/- pharmacodynamics of proton pump
inhibitor-containing Helicobacter pylori treatments. Curr Drug
Metab. 13:1303–1312. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Qiu Z, Liu H, He L, Ma Y, Song H, Bai W
and Yu M: Proton pump inhibitor-induced exfoliative dermatitis: A
case report. Exp Ther Med. 11:543–546. 2016.PubMed/NCBI
|
|
24
|
Hood W, McJunkin B, Warnock A, Girme A,
Smith N and Robinson B: Proton pump inhibitor prescribing and costs
in a large outpatient clinic. W V Med J. 110:16–21. 2014.PubMed/NCBI
|
|
25
|
Mouterde O, Bellaïche M, Dumant C and
Mallet E: Gastroesophageal reflux and proton pump inhibitors:
Panacea or prescription abuse? Arch Pediatr. 17:739–740. 2010.(In
French). View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Forgacs I and Loganayagam A:
Overprescribing proton pump inhibitors. BMJ. 336:2–3. 2008.
View Article : Google Scholar : PubMed/NCBI
|