Introduction
Surgical procedures on patients in the prone
position while under general anesthesia (GA) may be associated with
significant hemodynamic changes including reductions in cardiac
index (CI) and arterial blood pressure (BP), as well as increases
in central venous pressure (CVP) and systemic vascular resistance
(SVR). These changes may be attributed to alteration of
intra-abdominal pressure and compression of the thoracic space
(1–4). Intra-operative hypotension (IOH) has
been reported to be independently associated with adverse
perioperative outcomes and associated with patient postoperative
long-term mortality (5–7). Perioperative stroke has often been
attributed to IOH (8), and IOH has
been reported to be one of the most important concerns associated
with the occurrence of postoperative myocardial ischemia and
infarction (6). It is crucial to
avoid the occurrence or shorten the duration of IOH and
subsequently prevent peri-operative complications. Clinicians
usually reverse IOH by decreasing anesthetic dosages, enhancing
intravenous fluid administration or applying vasopressors (9).
Ephedrine and phenylephrine (PE) are two commonly
used vasoconstrictors that restore BP to normal values (10,11).
Ephedrine acts on α- and β-adrenergic receptors and displaces
norepinephrine from adrenergic terminals (12–14). The
release of catecholamines and subsequent activation of adrenergic
receptors is thought to be the primary mechanism underlying the
cardiovascular response to ephedrine. PE predominantly acts on the
α1-adrenergic receptor (12–14), which causes a direct increase in SVR,
arterial pressure and left ventricular afterload.
A previous study demonstrated that cerebral tissue
oxygen saturation (SctO2) was significantly decreased
following PE administration, but not following ephedrine treatment,
and cardiac output (CO) was identified to have the most significant
association with SctO2 (15). The use of PE to correct hypotension
induced by anesthesia has a negative impact on SctO2,
whereas ephedrine maintains frontal lobe oxygenation, which may be
associated with an increase in CO (14). Bolus PE reduced maternal CO when
compared with ephedrine during elective spinal anesthesia in
cesarean delivery (12).
The hemodynamic effects of ephedrine and PE used
while patients are in the prone position under GA have not been
fully described. The aim of the present study was to investigate
the effects of ephedrine and PE bolus administration on
physiological variables including intra-arterial systolic BP
(ISBP), intra-arterial diastolic BP (IDBP), CO, heart rate (HR),
stroke volume variation (SVV), cardiac index (CI), stroke volume
(SV), SV index (SVI), central venous pressure (CVP), and bispectral
index (BIS) of anesthetized patients in the prone position.
Materials and methods
Patients, study design and ethical
considerations
This was a prospective, randomized, and double-blind
study that was performed at Zhongda Hospital, Southeast University
(Nanjing, China). A total of 60 patients were randomly assigned to
one of two groups: An ephedrine group (n=30), and a PE group
(n=30). Patients included in the study were aged between 20 and 60
years, were undergoing elective lumbar spine surgery, and had an
American Society of Anesthesiologists physical status of I–II
(16). Patients were excluded from
this study if they had a history of symptomatic cardiovascular
disorders including sinus bradycardia, hypertension, diabetes
mellitus, a body mass index >28 kg/m2, or other
disorders known to affect autonomic nervous activity.
Over the course of the study, if the ISBP of a
patient increased to >160 mmHg or the IDBP increased to >95
mmHg for >2 min following ephedrine (0.1 mg/kg) or PE
administration, the patient was withdrawn from the study. Patients
were also withdrawn from the study if their HR decreased to <45
beats/min and required a bolus dose of 25–50 µg nitroglycerin,
20–40 mg esmolol or 0.5 mg atropine as a rescue treatment to
recover BP or HR. Shanghai, China
The study protocol was approved by the Institutional
Review Board of Zhongda Hospital, Southeast University. Patients
provided both verbal consent and signed informed consent forms. The
study was registered on the Chinese Clinical Trial Center (ChiCTR;
Registration no. ChiCTR-RNRC-13003094; Registration date, March 7
2013; Principal investigator, Dr Jiangyan Xia).
Study protocol
Following patient anesthesia and endotracheal
intubation, a radical intra-arterial catheter and a central venous
catheter with BIS electrodes were inserted in addition to
measurement of vital signs. Lead II electrocardiography data were
continuously monitored throughout the study. A third generation
Vigileo™/FloTrac™ device (Edwards Lifesciences, Irvine, CA, USA)
was used for the continuous recording of hemodynamic
parameters.
All patients were pre-oxygenated with 100% oxygen
via a face mask for 2–3 min prior to the induction of GA. The
protocol of induction and maintenance of GA were identical between
the two groups. Briefly, GA was induced with fentanyl (2–3 µg/kg;
Yichang Humanwell Pharmaceutical, Co., Ltd., Yichang, China),
followed by the intravenous administration of propofol (2–2.5
mg/kg; AstraZeneca plc, Wuxi, China). Endotracheal intubation was
facilitated with intravenous cisatracurium (0.15 mg/kg; Jiangsu
Hengrui Medicine, Co., Ltd., Lianyungang, China). Anesthesia was
maintained with a 1.5–3% end-tidal concentration of sevoflurane
(Maruishi Pharmaceutical Co., Ltd., Osaka, Japan) 50:50 oxygen and
air mixture, remifentanyl (5–10 µg/kg/h; Yichang Humanwell
Pharmaceutical, Co., Ltd.), and cisatracurium (150 µg/kg/h). The
concentration of inhaled sevoflurane was adjusted to maintain the
BIS between 40–60. Ventilation was controlled using a mechanical
ventilator. The tidal volume was held constant at 10 ml/kg and
end-tidal CO2 was maintained at 30–40 mmHg by adjusting
the frequency of ventilation. The patients were placed in the prone
position following induction of anesthesia and confirmation of the
correct position of the endotracheal tube. Hetastarch (10 ml/kg;
6%; Jiangsu Hengrui Medicine, Co., Ltd.) was administered as a
bolus fluid expansion for 30 min, prior to the administration of 15
ml/kg/h lactated Ringer's solution (Chimin Pharmaceutical, Co.,
Ltd., Zhejiang, China).
A single dose of ephedrine (0.1 mg/kg; Northeast
Pharmaceutical Group, Co., Ltd., Shenyang, China) or PE (1 µg/kg;
Shanghai Harvest Pharmaceutical, Co., Ltd., Shanghai, China) was
administered through the central venous catheter as a bolus
injection after the patient achieved a stable hemodynamic status
for ≥10 min. The ISBP was maintained at 85–105 mmHg by adjusting
the concentration of end-tidal sevoflurane. Ephedrine was diluted
to 5 mg/ml (0.02 ml/kg) with saline, and PE was diluted to 50 µg/ml
(0.02 ml/kg). Hemodynamic parameters were measured and recorded at
1 min intervals for 10 min (T1-T10) following bolus injection of
ephedrine or PE. All measurements were performed during the
surgical procedure under GA in the prone position. No
vasoconstrictors or vasodilators were used within 1 h prior to
hemodynamic measurements and the concentrations of the general
anesthetics used to maintain the anesthesia were not changed for
≥10 min prior to the measurements. There was also no significant
blood loss (<200 ml) resulting from the surgical procedure prior
to administration of the bolus ephedrine or PE.
Assessments
The primary parameters assessed in this study were
ISBP, IDBP and CO. Secondary parameters included CVP, CI, SVV, SVR
and HR. Baseline values (immediately prior to ephedrine or PE
administration) and post-ephedrine/PE values were measured and
compared. Adverse events were also recorded.
Statistical analysis
Statistical analysis and calculations were conducted
using GraphPad Prism 5.0 (GraphPad Software, Inc., La Jolla, CA,
USA). Data were expressed as mean ± standard deviation.
Intra-arterial mean BP (IMAP) was calculated as IDBP + 1/3 × (ISBP
- IDBP). Intergroup statistical comparisons were performed using
two-way analysis of variance (ANOVA), followed by Student's
t-test with Bonferroni's correction. BP and HR values over
time following ephedrine or PE injection were analyzed using
repeated one-way ANOVA, followed by a paired t-test with
Bonferroni's correction for paired data in each group. P<0.05
was considered to indicate a statistically significant result.
Results
Demographic and baseline
characteristics
The two experimental groups were comparable with
respect to age, gender, body weight and height (P>0.05; Table I). There was also no significant
difference between the two experimental groups with regard to the
end-tidal concentration of sevoflurane and remifentanyl used to
maintain the depth of anesthesia (DOA; P>0.05; Table I). Baseline (0 min, immediately prior
to ephedrine or PE injection) hemodynamic parameters of ISBP, IDBP,
IMAP, CO, SVV, CVP, CI, SVR and HR were comparable between the two
experimental groups (P>0.05; Table
I). All 60 patients completed the study and were included in
the statistical analysis. No patients were excluded from the study
due to exaggerated pressor reaction or severe tachycardia.
 | Table I.Baseline data and hemodynamic
parameters in the two groups at 0 min (mean ± standard
deviation). |
Table I.
Baseline data and hemodynamic
parameters in the two groups at 0 min (mean ± standard
deviation).
| Characteristic | Ephedrine | Phenylephrine | P-value |
|---|
| Gender
(male/female) | 17/13 | 14/16 | 0.3006 |
| Age (years) | 52.2±4.27 | 51.4±5.25 | 0.5028 |
| Weight (kg) | 66.7±9.93 | 67.3±10.14 | 0.8178 |
| Height (cm) | 166.0±8.54 | 166.6±7.43 | 0.7727 |
| Hemodynamic
parameters prior to anesthesia |
|
|
|
| SBP
(mmHg) | 131.5±11.0 | 134.5±12.2 | 0.3117 |
| DBP
(mmHg) | 78.8±7.6 | 81.6±7.9 | 0.1672 |
| HR
(beats/min) | 71.3±7.7 | 73.5±8.6 | 0.2919 |
| Hemodynamic
parameters prior to bolus injection |
|
|
|
| ISBP
(mmHg) | 95.8±6.7 | 96.4±7.6 | 0.7744 |
| IDBP
(mmHg) | 54.5±5.8 | 54.4±5.6 | 1.0000 |
| IMAP
(mmHg) | 68.2±5.7 | 68.4±5.8 | 0.9044 |
| HR
(beats/min) | 61.2±7.2 | 61.0±6.3 | 0.8649 |
| CO
(l/min) | 3.7±0.8 | 3.7±0.8 | 0.8921 |
| CI
(l/min/m2) | 2.2±0.4 | 2.2±0.4 | 0.8427 |
| CVP
(mmHg) | 7.4±2.6 | 7.3±2.6 | 0.8435 |
|
BIS | 41.1±3.7 | 42.7±3.5 | 0.1194 |
|
SVV | 10.7±2.6 | 10.2±2.1 | 0.4555 |
| SV | 60.3±8.1 | 60.2±9.6 | 0.9652 |
| End-tidal
concentration |
|
|
|
|
Sevoflurane (%) | 1.94±0.53 | 1.91±0.54 | 0.8087 |
|
Remifentanyl (mg/h) | 0.34±0.07 | 0.34±0.08 | 0.2429 |
Hemodynamic changes
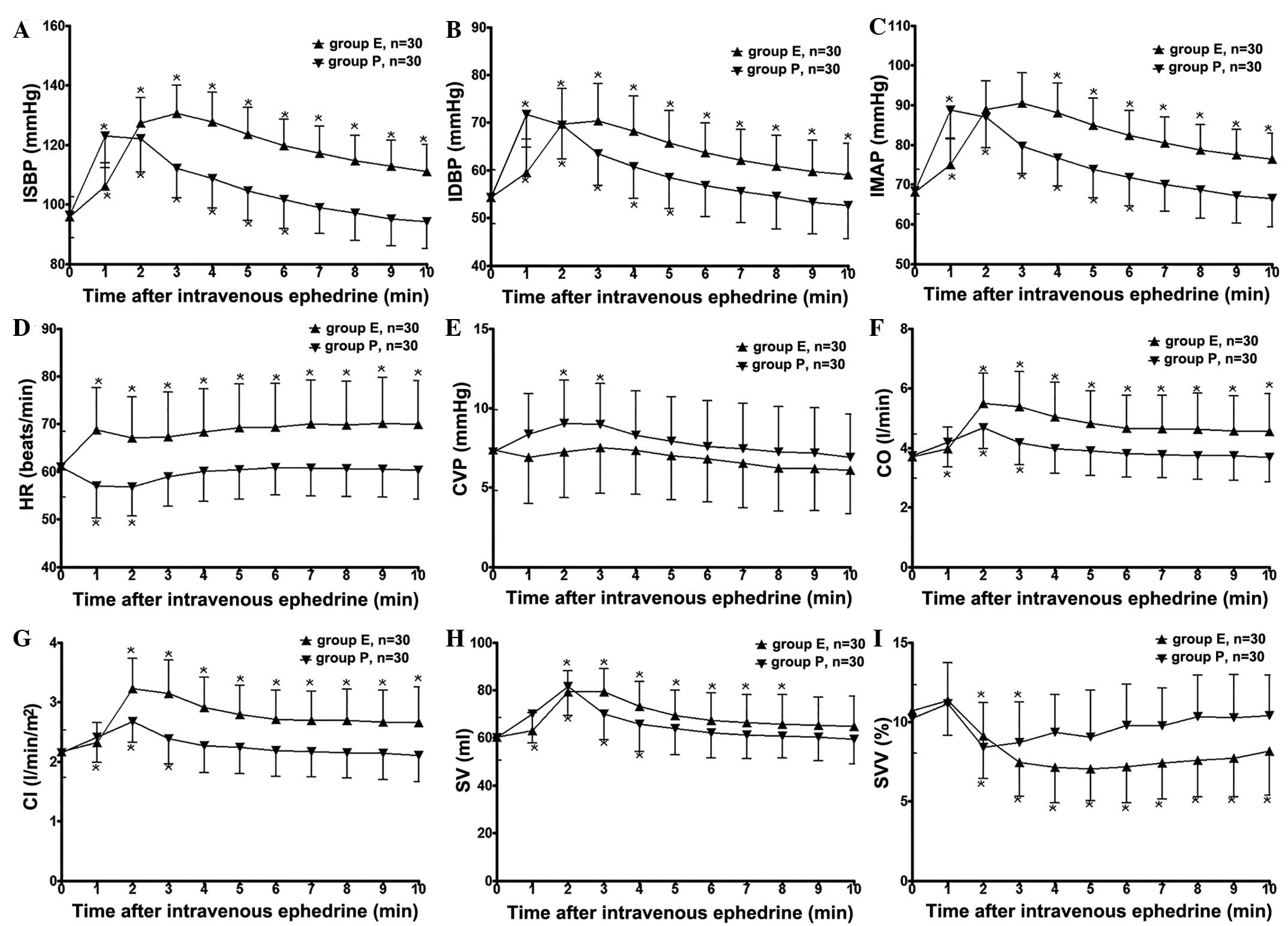
Following the bolus injection of ephedrine or PE, a
significant increase in ISBP was observed in the two experimental
groups compared with pre-ephedrine and pre-PE values (Fig. 1A). The duration of the increment in
ISBP was considerably longer in the ephedrine group compared with
the PE group. A similar response was observed in IDBP (Fig. 1B) and IMAP (Fig. 1C). Ephedrine caused a significant
increase in the HR from 1 to 10 min (61.27 to 70.20 beats/min),
whereas PE only caused a 2-min reduction in the HR (1–2 min; 60.97
to 56.87 beats/min; Fig. 1D).
Intravenous ephedrine resulted in a decline in CVP, whereas PE
produced a significant increase in CVP at 2–3 min (Fig. 1E). The significant elevation in ISBP,
IDBP and IMAP was initiated at 1 min following bolus injection in
the ephedrine group, reached maximum values at 3 min and lasted for
10 min. In the PE group, the effect only lasted 6 min and the
maximum was reached 1 min following treatment. A significant
increase in CO and CI (Fig. 1F and
G) was initiated at 1 min after dosing and lasted for the
entire observation period following ephedrine injection, whereas it
was only sustained for 3 min after the bolus injection of PE. The
significant increase in SV (Fig. 1H)
lasted from 2 to 8 min and 1 to 4 min in the ephedrine and PE
groups, respectively. Treatment with either bolus ephedrine or PE
caused an instant and transient elevation and then a subsequent
significant reduction in SVV (Fig.
1I). The significant reduction in SVV lasted longer in the
ephedrine group (from 2 to 10 min) compared with the PE group (from
2 to 3 min).
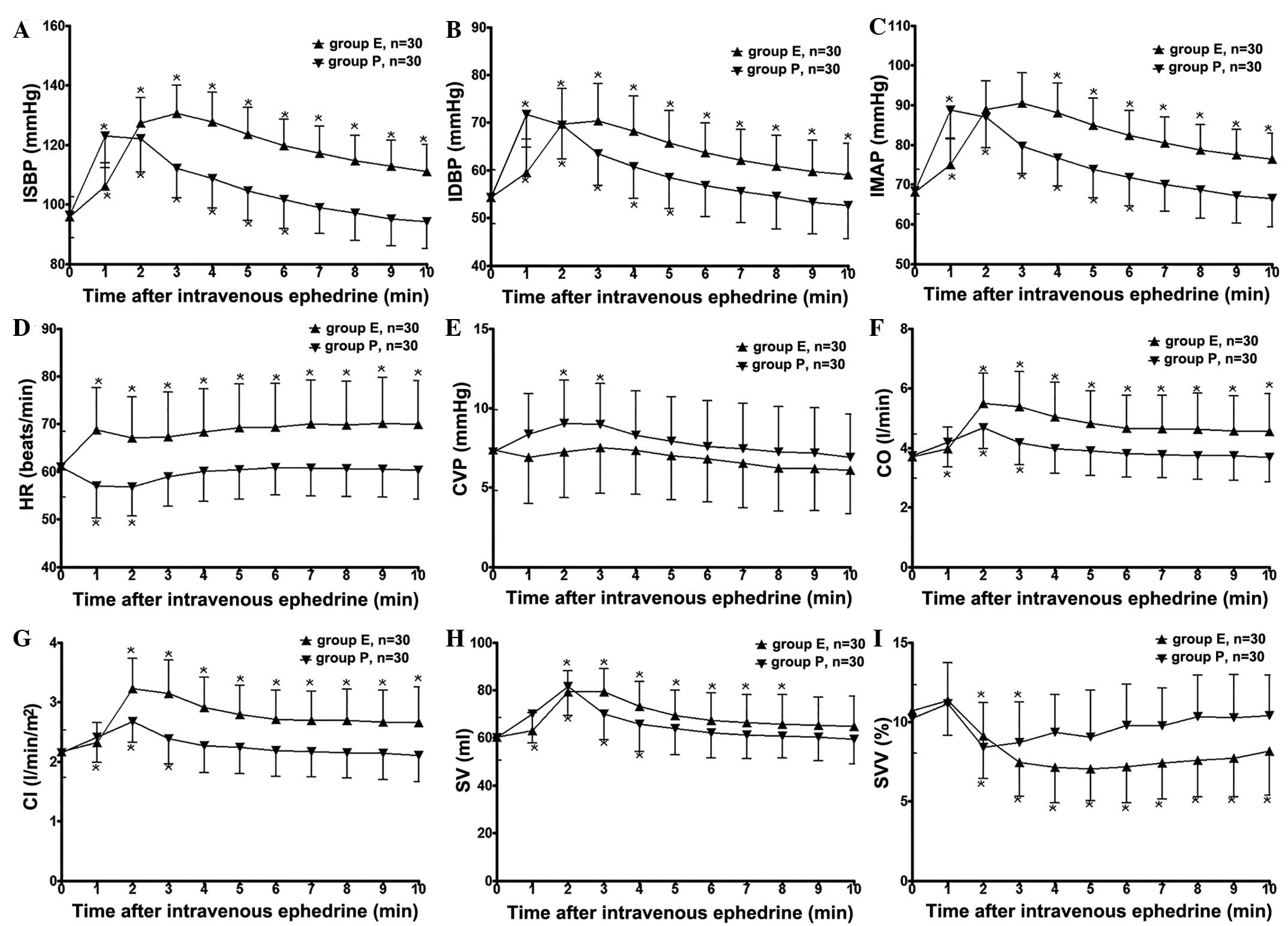 | Figure 1.Hemodynamic parameters of patients
that received a single dose of E (0.1 mg/kg) or P (1 µg/kg) through
a central venous catheter via bolus injection for the time period
of 0 to 10 min. The following parameters were measured: (A) ISBP,
(B) IDBP, (C) IMAP, (D) HR, (E) CVP, (F) CO, (G) CI, (H) SV and (I)
SVV. Data are presented as the mean ± standard deviation.
*P<0.05 between the two groups. Group P, patients treated with
phenylephrine; group E, patients treated with ephedrine. ISBP,
intra-arterial systolic blood pressure; IDBP, intra-arterial
diastolic blood pressure; IMAP, intra-arterial mean blood pressure;
HR, heart rate; CVP, central venous pressure; CO, cardiac output;
CI, cardiac index; SV, stroke volume; SVV, stroke volume
variation. |
Safety assessments
In the present study, ephedrine and PE were used at
doses that are comparatively low for a clinical setting in order to
observe the pressor response and hemodynamic effects during GA in
the prone position. Intervention was only provided when patient
ISBP was <105 mmHg or the IMAP ≤20% compared with the
pre-induction values. No patient appeared to have an exaggerated
pressor response or severe tachycardia following the intravenous
administration of 0.1 mg/kg ephedrine or 1 µg/kg PE.
Discussion
Hypotension is a common complication observed
following the use of various anesthesia techniques (11,17),
particularly in patients who are in the prone position while under
GA (1,4). IOH and intraoperative hemodynamic
fluctuation contribute to perioperative morbidity and mortality
(6,7,18,19).
Hypotension while prone may also be a risk factor for perioperative
ischemic optic neuropathy in spine surgery (20). Avoiding IOH, or shortening the
duration of IOH and maintaining stable vital parameters may provide
patients with improved outcomes. Although vasoconstrictors have a
rapid time of onset and reliable pressor effects, their
inappropriate administration may lead to adverse outcomes such as
tachycardia, hypertension and increased blood loss (21). Among all the frequently used
vasopressors, ephedrine and PE are used to reverse or avoid
hypotension associated with the performance of anesthesia
techniques or application of anesthetic agents (10,22,23).
The results of the present study suggested that
compared with PE, a bolus intravenous injection of ephedrine
resulted in a more durable pressor effect when patients were in the
prone position under GA. This effect was accompanied by increased
CO, CI, SV, SVI and HR, and decreased CVP and SVV, suggesting that
the pressor response of ephedrine during GA in the prone position
may be predominantly induced by the activation of β-adrenergic
receptors. Compared with ephedrine, the hemodynamic changes induced
by bolus PE include an acute but temporarily elevation of CO, CI,
SV, SVI and CVP, and a short-term reduction in HR and SVV. There
are two main mechanisms underlying the effects of PE on CO. PE
increases ventricular afterload and thereby decreases SV and CO.
Additionally, the release of blood from peripheral veins to central
veins caused by PE elevates CVP and SV, and thus CO (24,25). It
has been suggested that the impact of PE on CO is associated with
preload dependency (26,27). When the heart is preload-independent,
a bolus injection of PE usually induces a reduction in CO. When the
heart is dependent on the blood volume that reaches the ventricle
(preload dependent), PE boluses usually induce an increase in CO
(28). Patients undergoing spinal
surgery in the prone position may be preload-dependent due to the
decreased returned blood volume resulting from enhanced
intra-abdomen pressure and compression of the inferior vena cava
and thoracic space. The bolus injection of PE would cause an
instant increase in CO and CI and the increased venous returned
blood would change the state of preload-dependent to
preload-independent. The CO and CI would decline shortly following
the transient elevation.
Controversy exists regarding the equivalent doses of
PE and ephedrine. Previous studies have used ratios varying from
20:1 to 250:1 (12,29). In the patient population of the
present study, a 0.1 µg/kg bolus of PE and a 0.1 mg/kg bolus of
ephedrine restored the IMAP to within a range of 20% above or below
baseline.
Previous investigations have demonstrated that the
pressor effect of ephedrine is greater in anesthetized patients
compared with awake patients (30).
Propofol, enflurane and pre-medicated clonidine have been shown to
enhance the pressor response to ephedrine (11,30–33).
This response has been reported to be associated with differences
in sympathetic tone and adrenergic receptor status (30–33). The
pressor response has been found to be more intense at the lower
basal level of sympathetic activity. Our previous study
demonstrated that in comparison with the supine position, the prone
position would induce a pressor response to ephedrine, which may be
attributed to the enhanced parasympathetic nerve activity
associated with the prone position (unpublished data).
Previous researchers postulated that the DOA may be
one of the factors that influence the pressor response to
vasoconstrictors (30,32). However, in the present investigation,
the two study groups followed the same anesthesia and fluid
administration protocol. There was no significant difference
between the dosages and concentrations of anesthetics used for
induction and maintenance of anesthesia between the two groups.
Pre-ephedrine and pre-PE hemodynamic parameters and BIS values were
comparable between the two groups. Therefore, it was unlikely that
there was a significant difference in the DOA between the two
experimental groups.
One of the limitations of the present study was the
use of a third generation Vigileo-FloTrac device for continuous
recording of hemodynamic parameters. Although previous studies have
verified the accuracy, sensitivity and reliability of this
pressure-based cardiac output measurement system (5,34), there
have been reports that the pulse-contour method used by this system
cannot accurately track changes in CO induced with PE and ephedrine
(35,36). Another limitation of the present
study was that the autonomic nervous system (ANS) tone was not
assessed during GA in the prone position, despite previous studies
indicating that the tone of the ANS may influence the pressor
response to some vasoconstrictors (30,32). In
addition, the level of cerebral tissue oxygenation and intraocular
pressure were not monitored. Further studies are required to
investigate the effects of vasopressors on the perfusion of tissues
and major organs. Based on previous and present studies that have
evaluated the inhibition or augmentation of biological responses to
several vasoconstrictors under various anesthetic techniques, it
can be derived that additional investigations focusing on
amelioration of the hypo-reactivity and vasoplegia induced by
sepsis through the regulation of the activity of ANS are
required.
In conclusion, the present study demonstrated that
bolus ephedrine will produce a more persistent pressor response and
durable increase in CO and CI compared with PE when patients are in
the prone position under GA for spine surgery. Ephedrine may be the
more appropriate choice to reverse the IOH induced by GA in the
prone position for spine surgery, as it induces a longer pressor
response than PE. Ephedrine may also induce a more stable elevation
of CI and CO, which may be beneficial to the perfusion of major
organs, particularly the cerebral nervous system.
Acknowledgements
The present study was supported by a grant from the
Natural Science Foundation for Young Fund (grant no.
81201449/H1502).
References
|
1
|
Poon KS, Wu KC, Chen CC, Fung ST, Lau AW,
Huang CC and Wu RS: Hemodynamic changes during spinal surgery in
the prone position. Acta Anaesthesiol Taiwan. 46:57–60. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tabara Y, Tachibana-Iimori R, Yamamoto M,
Abe M, Kondo I, Miki T and Kohara K: Hypotension associated with
prone body position: A possible overlooked postural hypotension.
Hypertens Res. 28:741–746. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Toyota S and Amaki Y: Hemodynamic
evaluation of the prone position by transesophageal
echocardiography. J Clin Anesth. 10:32–35. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dharmavaram S, Jellish WS, Nockels RP,
Shea J, Mehmood R, Ghanayem A, Kleinman B and Jacobs W: Effect of
prone positioning systems on hemodynamic and cardiac function
during lumbar spine surgery: An echocardiographic study. Spine
(Phila Pa 1976). 31:1388–1393. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Biais M, Bernard O, Ha JC, Degryse C and
Sztark F: Abilities of pulse pressure variations and stroke volume
variations to predict fluid responsiveness in prone position during
scoliosis surgery. Br J Anaesth. 104:407–413. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bijker JB, Persoon S, Peelen LM, Moons KG,
Kalkman CJ, Kappelle LJ and van Klei WA: Intraoperative hypotension
and perioperative ischemic stroke after general surgery: A nested
case-control study. Anesthesiology. 116:658–664. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bijker JB, van Klei WA, Vergouwe Y,
Eleveld DJ, van Wolfswinkel L, Moons KG and Kalkman CJ:
Intraoperative hypotension and 1-year mortality after noncardiac
surgery. Anesthesiology. 111:1217–1226. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Reich DL, Bodian CA, Krol M, Kuroda M,
Osinski T and Thys DM: Intraoperative hemodynamic predictors of
mortality, stroke and myocardial infarction after coronary artery
bypass surgery. Anesth Analg. 89:814–822. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hiltebrand LB, Koepfli E, Kimberger O,
Sigurdsson GH and Brandt S: Hypotension during fluid-restricted
abdominal surgery: Effects of norepinephrine treatment on regional
and microcirculatory blood flow in the intestinal tract.
Anesthesiology. 114:557–564. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Erkinaro T, Mäkikallio K, Kavasmaa T,
Alahuhta S and Räsänen J: Effects of ephedrine and phenylephrine on
uterine and placental circulations and fetal outcome following
fetal hypoxaemia and epidural-induced hypotension in a sheep model.
Br J Anaesth. 93:825–832. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nazir I, Bhat MA, Qazi S, Buchh VN and
Gurcoo SA: Comparison between phenylephrine and ephedrine in
preventing hypotension during spinal anesthesia for cesarean
section. J Obstet Anaesth Crit Care. 2:92–97. 2012. View Article : Google Scholar
|
|
12
|
Dyer RA, Reed AR, van Dyk D, Arcache MJ,
Hodges O, Lombard CJ, Greenwood J and James MF: Hemodynamic effects
of ephedrine, phenylephrine and the coadministration of
phenylephrine with oxytocin during spinal anesthesia for elective
cesarean delivery. Anesthesiology. 111:753–765. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zaimis E: Vasopressor drugs and
catecholamines. Anesthesiology. 29:732–762. 1968. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nissen P, Brassard P, Jørgensen TB and
Secher NH: Phenylephrine but not ephedrine reduces frontal lobe
oxygenation following anesthesia-induced hypotension. Neurocrit
Care. 12:17–23. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Meng L, Cannesson M, Alexander BS, Yu Z,
Kain ZN, Cerussi AE, Tromberg BJ and Mantulin WW: Effect of
phenylephrine and ephedrine bolus treatment on cerebral oxygenation
in anaesthetized patients. Br J Anaesth. 107:209–217. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Daabiss M: American Society of
Anesthesiologists physical status classification. Indian J Anaesth.
55:111–115. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Reich DL, Hossain S, Krol M, Baez B, Patel
P, Bernstein A and Bodian CA: Predictors of hypotension after
induction of general anesthesia. Anesth Analg. 101:622–628. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Aronson S, Stafford-Smith M, Phillips-Bute
B, Shaw A, Gaca J and Newman M: Cardiothoracic Anesthesiology
Research Endeavors: Intraoperative systolic blood pressure
variability predicts 30-day mortality in aortocoronary bypass
surgery patients. Anesthesiology. 113:305–312. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Dwyer T, Ponsonby AL, Newman NM and
Gibbons LE: Prospective cohort study of prone sleeping position and
sudden infant death syndrome. Lancet. 337:1244–1247. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chang SH and Miller NR: The incidence of
vision loss due to perioperative ischemic optic neuropathy
associated with spine surgery: The Johns Hopkins Hospital
Experience. Spine (Phila Pa 1976). 30:1299–1302. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Arndt JO, Bömer W, Krauth J and Marguardt
B: Incidence and time course of cardiovascular side effects during
spinal anesthesia after prophylactic administration of intravenous
fluids or vasoconstrictors. Anesth Analg. 87:347–354. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ngan Kee WD, Khaw KS and Ng FF: Prevention
of hypotension during spinal anesthesia for cesarean delivery: An
effective technique using combination phenylephrine infusion and
crystalloid cohydration. Anesthesiology. 103:744–750. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sookplung P, Siriussawakul A, Malakouti A,
Sharma D, Wang J, Souter MJ, Chesnut RM and Vavilala MS:
Vasopressor use and effect on blood pressure after severe adult
traumatic brain injury. Neurocrit Care. 15:46–54. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Thiele RH, Nemergut EC and Lynch C III:
The clinical implications of isolated alpha(1) adrenergic
stimulation. Anesth Analg. 113:297–304. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Thiele RH, Nemergut EC and Lynch C III:
The physiologic implications of isolated alpha(1) adrenergic
stimulation. Anesth Analg. 113:284–296. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gelman S: Venous function and central
venous pressure: A physiologic story. Anesthesiology. 108:735–748.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Cannesson M, Jian Z, Chen G, Vu TQ and
Hatib F: Effects of phenylephrine on cardiac output and venous
return depend on the position of the heart on the Frank-Starling
relationship. J Appl Physiol. 113:281–289. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Cannesson M, Jian Z, Chen G, Vu TQ and
Hatib F: Effects of phenylephrine on cardiac output and venous
return depend on the position of the heart on the Frank-Starling
relationship. J Appl Physiol. 113:281–289. 1985. View Article : Google Scholar
|
|
29
|
Saravanan S, Kocarev M, Wilson RC, Watkins
E, Columb MO and Lyons G: Equivalent dose of ephedrine and
phenylephrine in the prevention of post-spinal hypotension in
Caesarean section. Br J Anaesth. 96:95–99. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Goyagi T, Tanaka M and Nishikawa T: Oral
clonidine premedication enhances the pressor response to ephedrine
during spinal anesthesia. Anesth Analg. 87:1336–1339. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hayakawa-Fujii Y, Iida H and Dohi S:
Propofol anesthesia enhances pressor response to ephedrine in
patients given clonidine. Anesth Analg. 89:37–41. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kanaya N, Satoh H, Seki S, Nakayama M and
Namiki A: Propofol anesthesia enhances the pressor response to
intravenous ephedrine. Anesth Analg. 94:1207–1211. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Nishikawa T, Kimura T, Taguchi N and Dohi
S: Oral clonidine preanesthetic medication augments the pressor
responses to intravenous ephedrine in awake or anesthetized
patients. Anesthesiology. 74:705–710. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Behnia M, Powell S, Fallen L, Tamaddon H
and Behnia M: Correlation of stroke volume measurement between
Sonosite portable echocardiogram and Edwards Flotrac sensor-Vigileo
monitor in an intensive care unit. Clin Med Insights Circ Respir
Pulm Med. 7:45–51. 2013.PubMed/NCBI
|
|
35
|
Camporota L and Beale R: Pitfalls in
haemodynamic monitoring based on the arterial pressure waveform.
Crit Care. 14:1242010. View
Article : Google Scholar : PubMed/NCBI
|
|
36
|
Meng L, Tran NP, Alexander BS, Laning K,
Chen G, Kain ZN and Cannesson M: The impact of phenylephrine,
ephedrine and increased preload on third-generation Vigileo-FloTrac
and esophageal doppler cardiac output measurements. Anesth Analg.
113:751–757. 2011. View Article : Google Scholar : PubMed/NCBI
|