Introduction
Collecting duct carcinoma (CDC), which is also known
as Bellini duct carcinoma, is a type of kidney cancer that
originates in the papillary duct of the kidney. Accounting for
<1% of all renal cell carcinoma (RCC) cases, patients with CDC
have a poor prognosis (1).
Predominantly, clinicians recognize this disease due to past
experience and case reports, and a standard treatment is yet to be
established. However, since CDC is diagnosed based on pathological
examination, surgery is thus inevitable in the majority of such
cases. To the best of our knowledge, the majority of patients with
CDC that present at an advanced stage will succumb to the disease
within one year post-surgery, regardless of whether they receive or
deny adjuvant therapies (1–7).
According to the literature, the majority of CDC
cases have been high grade, advanced stage and unresponsive to
conventional therapies (8). As shown
in studied cases in the present study (Table I), the majority of CDC cases survived
between 4 and 9 months post-operatively, and the majority of such
patients present at an advanced stage, regardless of whether they
receive or deny adjuvant therapies. The current study reports a CDC
case treated with surgical monotherapy, and the post-surgery
survival conditions are compared with other reported cases. The aim
of the study is to determine whether surgical monotherapy is a
suitable therapeutic strategy for patients with advanced CDC.
 | Table I.Summary of patient tumor
characteristics and survival duration. |
Table I.
Summary of patient tumor
characteristics and survival duration.
| Author, year | TNM
classificationa | Stagea | Treatment | Survival duration
(months)b | Refs. |
|---|
| Surgery alone |
|
| The
present case | T2bN2M0 | IV | RN | 9 | – |
| Bansal
et al, 2012 | T4N0M0 | IV | RN | 9 | (2) |
|
| T1bN0M0 | I | RN | 9 |
|
| Méjean
et al, 2003 | T3N2M1 | IV | RN | Very short | (3) |
|
| T3N2M1 | IV | RN | Very short |
|
|
| T3N2M1 | IV | RN | Very short |
|
|
| T3N2M1 | IV | RN | 6 |
|
|
| T3N2M1 | IV | RN | 9 |
|
| Chao
et al, 2002 | T3aN1M1 | IV | RN | 7 | (10) |
|
| T4N2M1 | IV | RN | 13 |
|
| Surgery plus
chemotherapy |
|
| Milowsky
et al, 2002 | T4N2M0 | IV | RN + Dox + Gem | 10 | (4) |
| Orsola
et al, 2005 | T4N1MO | IV | RN + Dox + Gem | Mean 5.6 | (5) |
|
| T3aN1M0 | III | RN + Dox + Gem |
|
|
| Surgery plus combined
therapy |
|
| Husillos
et al, 2011 | T1N0M1 | IV | RN + Tem | 4 | (6) |
|
| T3bN2M1 | IV | RN + Sun | 7 |
|
| Procopio
et al, 2012 | TxN1-2Mx | III–IV | RN + Sor | Mean 4 | (7) |
|
| TxN1-2Mx | III–IV | RN + Sor |
|
|
|
| TxN1-2Mx | III–IV | RN + Sor |
|
|
|
| TxN1-2Mx | III–IV | RN + Sun |
|
|
|
| TxN1-2Mx | III–IV | RN + Tem |
|
|
| Chao
et al, 2002 | T3aN0M1 | IV | RN + Pac + Car | 9 | (10) |
|
| T3aN0M1 | IV | RN + Pac + Car | 17 |
|
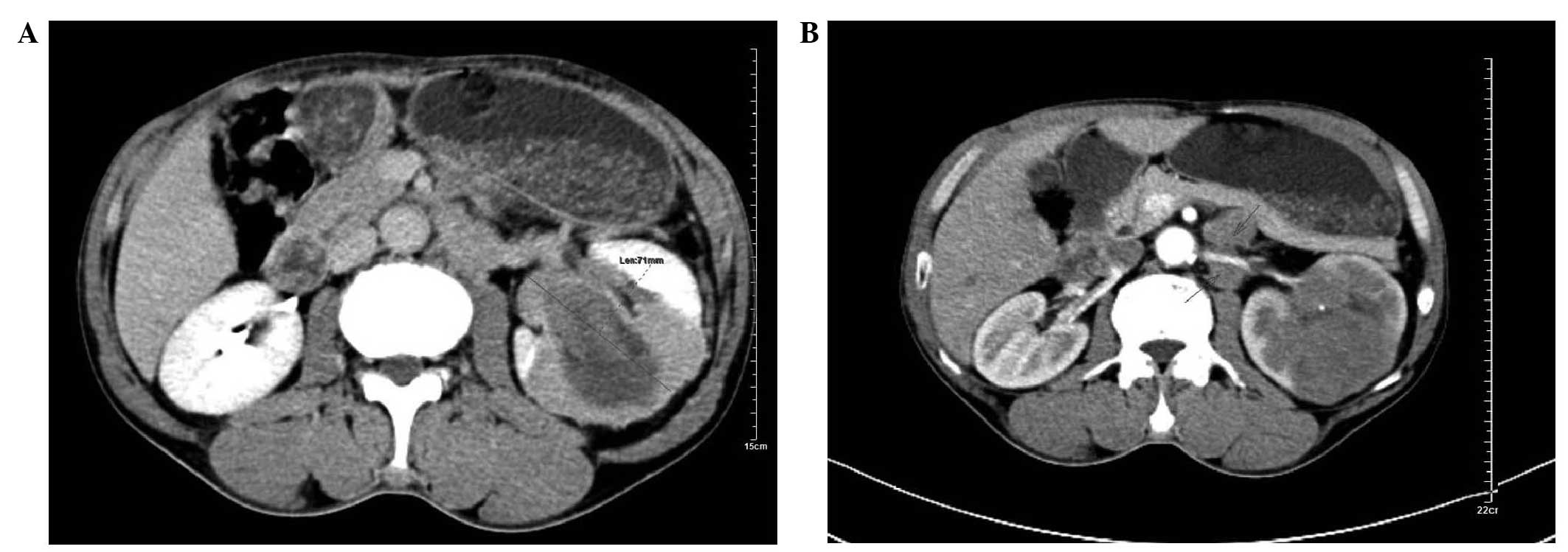
Case report
A 57-year-old male presented at the Department of
Urology at The Second Xiangya Hospital, Central South University
(Changsha, China) in July 2013 with intermittent painless gross
hematuria that lasted for two weeks. The results of laboratory
tests demonstrated that blood electrolytes were within the normal
ranges, and renal and liver function were normal. An X-ray was
performed, which showed the patient had a clear chest. A subsequent
computerized tomography (CT) scan demonstrated a rough bordered
tumor measuring 7.1×6.0 cm on the left kidney, which was
heterogeneously enhanced, and multiple enlarged lymph nodes were
detected in the retroperitoneal space, particularly in the area
surrounding the left renal artery (Fig.
1). No other abnormalities or metastasis were detected.
According to 2009 TNM classification system (8), the patient was diagnosed as clinical
stage T2bN2M0. Written informed consent was obtained from the
patient prior to publication.
Following diagnosis, a left laparoscopic radical
nephrectomy (RN) was performed. During surgery, a group of enlarged
lymph nodes were found fused with one another near the left renal
hilum, and were firmly fixed to the psoas major and the aorta
descendens. Notably, the left renal artery was engulfed by this
nodular mass and it was impossible to remove all of these lymph
nodes due to their infiltration; therefore, only partial resection
of these lymph nodes was performed for biopsy. The affected left
kidney was successfully removed, and on gross examination a
reddish-brown tumor measuring 6.8×6.5×2.5 cm3 was found
in the upper pole of the kidney. A postoperative pathological
diagnosis of renal collecting (Bellini) duct carcinoma was made as
the lymph nodes were positive for cancer, according to the
following criteria: i) Pre-operative CT scan shown multiple
enlarged lymph nodes; ii) perinephric lymph nodes enlarged and
hardened during surgery; iii) post-operative pathologic examination
confirmed that the resected lymph nodes were cancerous.
Pathological diagnosis was performed at the Department of Pathology
of The Second Xiangya Hospital, Central South University. Tissue
was formalin-fixed and the core lesion was embedded in paraffin,
cut into ~5 µm sections, dried at room temperature overnight, then
de-paraffinized and rehydrated for staining. Immunohistochemical
analysis was performed using the following antibodies purchased
from Abcam (Cambridge, UK): Ki-67 (rabbit polyclonal antibody; cat.
no. ab15580,), epithelial membrane antigen (rabbit polyclonal; cat.
no. ab139390) and vimentin (mouse polyclonal; cat. no. ab7752); and
cytokeratin 7 (CK7; mouse polyclonal; cat. no. ab82253), smooth
muscle actin, renal cell carcinoma (RCC; rabbit polyclonal; cat.
no. ab152111), cluster of differentiation 10 (mouse monoclonal;
cat. no. ab951), prostate specific antigen (mouse monoclonal; cat.
no. ab49395), human melanoma black 45 (HMB45; mouse monoclonal;
cat. no. ab787), thyroid transcription factor-1 (mouse monoclonal;
cat. no. ab72876), S100 (rabbit polyclonal; cat. no. ab15520),
hematopoietic cell kinase (HCK; rabbit polyclonal; cat. no.
ab32860) and lymphocyte-specific protein tyrosine kinase-negative
(rabbit monoclonal; cat. no. ab32149). SignalStain Boost ICH
Detection Reagent (Cell Signaling Technology, Inc., Danvers, MA,
USA) was used.
The patient discharged from hospital 5 days
post-surgery. When the final diagnosis was made, the patient was
offered adjuvant chemotherapy but he refused due to the fear of the
adverse effects of chemotherapy and, more importantly, the
uncertainty of the current regimens. The patient was followed-up
three months post-surgery and he reported no discomfort. Since the
gross hematuria had been alleviated, the patient was quite relieved
and satisfied with his condition. Six months after surgery, on his
second follow-up, the patient did not complain of any discomfort.
Abdominal CT scanning demonstrated enlarged residual lymph nodes in
the retroperitoneal space that were in the same position as the
previously CT scan.
Two months later, at eight months post-surgery, the
patient presented at The Second Xiangya Hospital again complaining
a loss of appetite. Chest X-ray analysis demonstrated a nodular
mass located near the right lung hilus. Lung metastasis was
considered and a chest CT scan was recommended; however, the
patient refused to complete further CT examination for personal
reasons, nor was he willing to receive further therapies.
Although the patient did attend our hospital again,
consultations were performed over the telephone. One month later,
the patient developed dyspnea due to hydrothorax, and thoracentesis
was performed several times at The First People Hospital and
Yueyang (Yueyang, China) to aid his breathing. Palliative treatment
was administered and the patient succumbed to respiratory failure
nine months and two days post-surgery.
Discussion
CDC is a highly malignant tumor which accounts for
<1% of all RCC cases (1). Due to
its rarity, the majority of clinicians only recognize this disease
due to past experience and case reports. To the best of our
knowledge, the largest CDC case series to date includes 81 patients
(9), and the majority of patients
with CDC present with advanced staged disease, predominantly with
lymphadenopathy or metastasis. However, no consensus has been
reached concerning treatment protocols. The present case report and
review aimed to summarize and evaluate patient's experiences with
CDC.
Surgery remains the most effective treatment for
patients with renal cancer, even in patients with advanced disease.
Since CDC is diagnosed on the basis of pathology, imaging
examinations and clinical manifestations prior to surgery are
unable to accurately distinguish CDC from other types of kidney
tumors; thus surgery is inevitable in the majority of cases.
Regrettably, no survival data of patients with advanced kidney
cancer without surgery is available in the literature.
In a previous study by Tokuda et al (9), 98.8% of cases underwent surgery as
primary treatment, including radica nephrectomy, partial
nephrectomy, total nephroureterectomy and biopsy of the metastatic
site. These surgeries were performed in 88.9, 2.5, 7.4 and 1.2% of
cases, respectively. Furthermore, Bansal et al (2) reported two cases of CDC (T4N0M0 and
T1bN0M0), both of whom received RN alone and survived for 9 months.
In another previous report, two patients with CDC (T3aN1M1 and
T4N2M1) also received RN and survived for 7 and 13 months
post-surgery, respectively (10). In
a study performed by Méjean et al (3), one of three patients succumbed to stage
T3N2M1 CDC shortly after surgery, whereas the remaining two cases
survived for 6 and 9 months following surgery, respectively. The
patient patient survived for 9 months and 2 days following RN
surgery, which appears to be consistent with the previous cases
(Table I).
The majority of CDC cases reported in the literature
were unresponsive to conventional therapies. In the report
published by Milowsky et al (4), a patient with T4N2M0 CDC was treated
with RN plus adjuvant chemotherapy (doxorubicin + gemcitabine) and
survived for 10 months post-surgery. Furthermore, Orsola et
al (5) reported two cases
(T4N1M0 and T3aN1M0) who received the same treatment as the patient
described by Milowsky et al (4); however, the mean survival time was only
5.6 months post-surgery (5). Chao
et al (10) described two
stage T3aN0M1 CDC cases, both of whom were treated with RN plus
adjuvant chemotherapy (paclitaxel + carboplatin); the patients
succumbed to CDC 9 and 17 months post-surgery, respectively. These
previous cases demonstrated that, in addition to the side effects
and economic burden of chemotherapy, the improvement in patient
survival induced by adjuvant chemotherapy is unsatisfactory.
Targeted therapy is another promising therapeutic
option for patients with advanced RCC; however, according to the
literature, its curative effect for CDC remains poor. Husillos
et al (6) reported two CDC
cases at stages T1N0M2 and T3bN2M1, respectively, whom were treated
with RN plus targeted therapy (temsirolimus and sunitinib) and
survived for 4 and 7 months post-RN, respectively. Furthermore, in
another previous report, five CDC patients with nodal involvement
were treated with RN plus targeted therapy [sorafenib (n=3);
sunitinib (n=1); 1 temsirolimus (n=1)] as first-line treatment,
and, after suffering from early progression, the mean survival time
of these patients was 4 months (7).
In previous cases, chemotherapy has been combined
with targeted therapy. Staehler et al (11) reported two stage T3aN2M0 CDC cases
treated with RN plus combined therapy (first line, gemcitabine +
cisplatin; second line, sunitinib); both patients succumbed to the
disease 8 months after the initial diagnosis. However, Barrascout
et al (12) described a
patient with T3aN0m0 CDC treated with RN plus combined therapy
(gemcitabine, cisplatin and bevacizumab) who survived >35 months
following the initial diagnosis.
It is cursory to state that all patients with CDC
have a poor prognosis, as there have been reports of patients with
CDC who have survived >5 years with controlled disease (4,7,13). Notably, none of these patients
exhibited lymphadenopathy or metastasis prior to surgery and all
received different therapies. Conversely, all advance staged CDCs
patients, particularly those with nodal involvements, suffered from
a poor prognosis regardless of the therapy they received, which
suggests that adjuvant therapy may not be an independent
factor.
In conclusion, following case comparison, no
superiority in the type of adjuvant therapy was detected in the
present case report and literature review. Therefore, the patient's
quality of life and economic factors should be taken into
consideration until novel adjuvant therapies are proven effective.
The authors of the present study hypothesize that surgical
monotherapy may be the most suitable treatment for patients with
advanced CDC.
Glossary
Abbreviations
Abbreviations:
|
CDC
|
collecting duct carcinoma
|
|
RCC
|
renal cell carcinoma
|
|
RN
|
radical nephrectomy
|
|
CT
|
computerized tomography
|
References
|
1
|
McDougal WS, Wein AJ, Kavoussi LR, Novick
AC, Partin AW, Peters CA and Ramchandani P: Campbell-Walsh Urology.
Malignant Renal Tumors. Campbell SC and Lane BR: Chapter 49. 10th.
Elsevier Health Sciences; USA: pp. 14362011
|
|
2
|
Bansal P, Kumar S, Mittal N and Kundu AK:
Collecting duct carcinoma: A rare renal tumor. Saudi J Kidney Dis
Transpl. 23:810–812. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Méjean A, Rouprêt M, Larousserie F,
Hopirtean V, Thiounn N and Dufour B: Is there a place for radical
nephrectomy in the presence of metastatic collecting duct (Bellini)
carcinoma? J Urol. 169:1287–1290. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Milowsky MI, Rosmarin A, Tickoo SK,
Papanicolaou N and Nanus D: Active chemotherapy for collecting duct
carcinoma of the kidney. Cancer. 94:111–116. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Orsola A, Trias I, Raventós CX, Español I,
Cecchini L and Orsola I: Renal collecting (Bellini) duct carcinoma
displays similar characteristics to upper tract urothelial cell
carcinoma. Urology. 65:49–54. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Husillos A, Herranz-Amo F, Subirá D, Lledó
E, Molina-Escudero R and Hernández-Fernández C: Collecting duct
renal cell carcinoma. Actas Urol Esp. 35:368–371. 2011.(In
Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Procopio G, Verzoni E, Iacovelli R,
Colecchia M, Torelli T and Mariani L: Is there a role for targeted
therapies in the collecting ducts of Bellini carcinoma? Efficacy
data from a retrospective analysis of 7 cases. Clin Exp Nephrol.
16:464–467. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sobin LH, Gospodarowicz MK and Wittekind
C: TNM Classification of Malignant Tumors. 7th. Blackwell
Publishing, Ltd.; Oxford: pp. 3362009
|
|
9
|
Tokuda N, Naito S, Matsuzaki O, Nagashima
Y, Ozono S and Igarashi T: Japanese Society of Renal Cancer:
Collecting duct (Bellini duct) renal cell carcinoma: A nationwide
survey in Japan. J Urol. 176:40–43; discussion 43. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chao D, Zisman A, Pantuck AJ, Gitlitz BJ,
Freedland SJ, Said JW, Figlin RA and Belldegrun AS: Collecting duct
renal cell carcinoma: Clinical study of a rare tumor. J Urol.
167:71–74. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Staehler M, Schöppler G, Haseke N, Stadler
T, Karl A, Siebels M, Ihrler S and Stief CG: Carcinoma of the
collecting ducts of Bellini of the kidney: Adjuvant chemotherapy
followed by multikinase inhibition with sunitinib. Clin Genitourin
Cancer. 7:58–61. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Barrascout E, Beuselinck B, Ayllon J,
Bättig B, Moch H, Teghom C and Oudard S: Complete remission of
pulmonary metastases of Bellini duct carcinoma with cisplatin,
gemcitabine and bevacizumab. Am J Case Rep. 13:1–2. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chua ME, Olondriz K, Maniwa M, Mendoza J
and Castillo J: Collecting duct of Bellini renal carcinoma with
psoas muscle recurrence: A case report and review of literature.
Can Urol Assoc J. 8:E167–E171. 2014. View Article : Google Scholar : PubMed/NCBI
|