Introduction
Chronic obstructive pulmonary emphysema (COPE)
behaves as progressive dyspnea, which seriously attenuates the
quality of life of patients. The study of the National Emphysema
Treatment Trial (NETT) has indicated that lung function and the
quality of life of patients after lung volume reduction surgery
(LVRS) were superior to medical treatment (1). Studies have shown that the improved
duration course of staged bilateral LVRS was superior to unilateral
or simultaneous bilateral LVRS (2).
We examined a total of 11 patients with bilateral COPE combined
with bullae from January 2013 to June 2014. The patients underwent
staged bilateral single-port thoracoscopic LVRS treatment, which
significantly improved their lung function and quality of life.
Patients and methods
Patients
The selection of single-port thoracoscopic LVRS
patients was carried out as defined in NETT (3). Eleven male patients with bilateral COPE
and bullae who underwent staged bilateral single-port thoracoscopic
LVRS in our hospital from January 2013 to June 2014 were enrolled
in our study. Mean patient age was 60.27±12.11 years and body
weight index was 34.35±0.69. Among the total cases, 1 case was
confirmed with inhomogeneous emphysema and bullae combined with
bronchial dilatation under CT imaging before surgery. Two cases
were confirmed with a long-term history of chest distress and
asthmatic suffocation. These patients had a medicine treatment
course of 10.09±4.25 years, combined with pneumothorax upon
admission, with relatively poor recruitment maneuver of lung after
thoracic close drainage. Before surgery, the patient was required
to stop smoking and was treated by atomization, coughing and
expectorating to effectively control asthmatic suffocation,
bronchial dilatation and pulmonary infection. In addition, the
patient also received respiratory function exercise and
standardized medication to prevent being exposed to allergen. After
the lung function was confirmed to be consistent with the operation
indications, single-port thoracoscopic LVRS was performed under
general intravenous anesthesia. Parameters of the lung function and
arterial blood gas one week before surgery included: forced
expiratory volume in the first second (FEV1), 1.37±0.24 liters;
arterial oxygen partial pressure (pO2), 66.91±2.95 mmHg;
carbon dioxide partial pressure (pCO2), 46.82±2.96 mmHg
and 6-minute walk distance (6MWD), 297.73±8.91 m (Table I).
 | Table I.Pulmonary function and 6MWD in
patients before and after LVRS. |
Table I.
Pulmonary function and 6MWD in
patients before and after LVRS.
|
| FEV1 (liters) | FEV1 (%) | PO2
(mmHg) | pCO2
(mmHg) | 6MWD (m) |
|---|
| Pre-surgery | 1.37±0.24 | 52.41±3.60 | 66.91±2.95 | 46.82±2.96 | 297.73±8.91 |
| 3 months after
unilateral surgery | 1.69±0.20 | 60.43±3.35 | 74.36±5.64 | 42.73±2.83 |
433.36±19.10 |
| 3 months after
bilateral surgery | 1.75±0.19 | 65.60±4.77 | 79.09±3.78 | 40.27±2.05 |
472.09±33.08 |
Methods
Surgical method
Double lumen endotracheal intubation was performed,
with atracurium, fentanyl and propofol used for general anesthesia.
Subsequently, unilateral lung ventilation was carried out; holes
were made in the fifth or sixth rib intercostal space of the
anterior axillary line and the length of the incision was 4.54±0.47
cm. The target region was determined according to CT and the
condition was observed by thoracoscope. The endoscopic cutting
device (Endo-GIA) was used to excise the overinflated lung tissues
in the target region. The cutting edges were overlapped and
consecutively the incisal margins were sutured by 4–0 prolene
followed by biological protein glue. The inferior pulmonary
ligament was loosened and the parietal pleura was rubbed and
pleural perfusion by group A Streptococcus (OK-432) was performed
to promote pleural adhesion. After surgery, the lung was dilated to
exclude the incisal margin from air leakage. A no. 7 chest tube was
placed between the second intercostal space in the midclavicular
line and one no. 26 chest tube between the eighth and ninth rib.
After surgery, 1 µg/ml fentanyl automatic control vein pump was
used to alleviate pain for 48 h. The patients were sent to ICU for
continuous monitoring and treatment for 1.73±0.64 days. The
patients were assisted with independent expectoration,
strengthening of respiratory tract nursing, and the time of
tracheal intubation was shortened. Three to four months after
unilateral LVRS when the lung function and general condition of the
patients were improved, bilateral LVRS was carried out.
Evaluation of the quality of life
Lung function and arterial blood gas were determined
under non-oxygen uptake state and 6MWD examinations one week before
surgery, three months after unilateral LVRS and three months after
bilateral LVRS. In the meanwhile, the patients were guided to
complete the short form 36-item health survey (SF-36) and their
scores was analyzed for evaluation of their quality of life.
Statistical analysis
SPSS 19.0 software (SPSS Inc., Chicago, IL, USA) was
applied for statistical analysis. Continuous variables are
presented as mean ± SD. The Student's t-test or Mann-Whitney U test
was applied for comparisons between groups. The χ2 or
Fisher's exact test was used for comparisons between groups with
regard to categorical variables and enumeration data. P<0.05 was
considered to indicate a statistically significant difference.
Results
None of the patients included in our study had
perioperative death. Surgery lasted for 126.36±14.40 min,
post-surgery mechanical ventilation lasted for 9.68±1.49 h,
post-surgery thoracic drainage tube lasted for 9.09±1.31 days, and
hospitalization lasted for 15.73±2.75 days. Among the cases, 5
cases had lung air leakage for 10.40±2.97 days, 7 cases had
pulmonary infection, and 5 cases had atelectasis. All patients were
cured and there was no other complications such as heart and lung
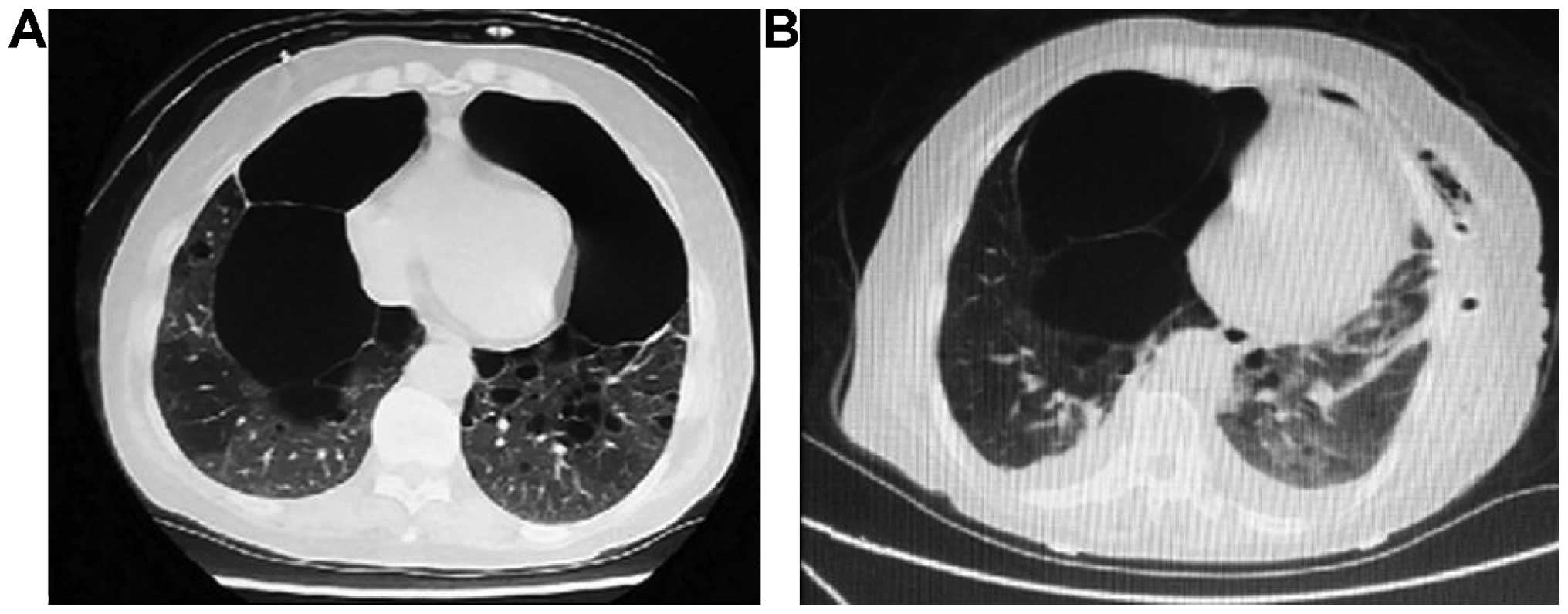
failure or thrombosis. One case was relatively typical, and was
diagnosed as COPE with giant bullae (also known as vanishing lung
syndrome). After unilateral LVRS surgery, parameters of lung
function of the patients were improved significantly compared with
those prior to surgery (Fig. 1).
The pulmonary function, arterial blood gas analysis
and activity of the daily living of the patients before surgery
were compared three months after unilateral LVRS and three months
after bilateral surgery. Comparative results showed that the
proportion of FEV1 in predicting value [FEV1 (%)], arterial
PO2 and 6MWD were increased compared with these
parameters before surgery while arterial pCO2 was
reduced compared with that before surgery; there was no significant
difference in the pulmonary function and blood gas analysis of the
patients between unilateral and bilateral LVRS (p>0.05)
(Table I).
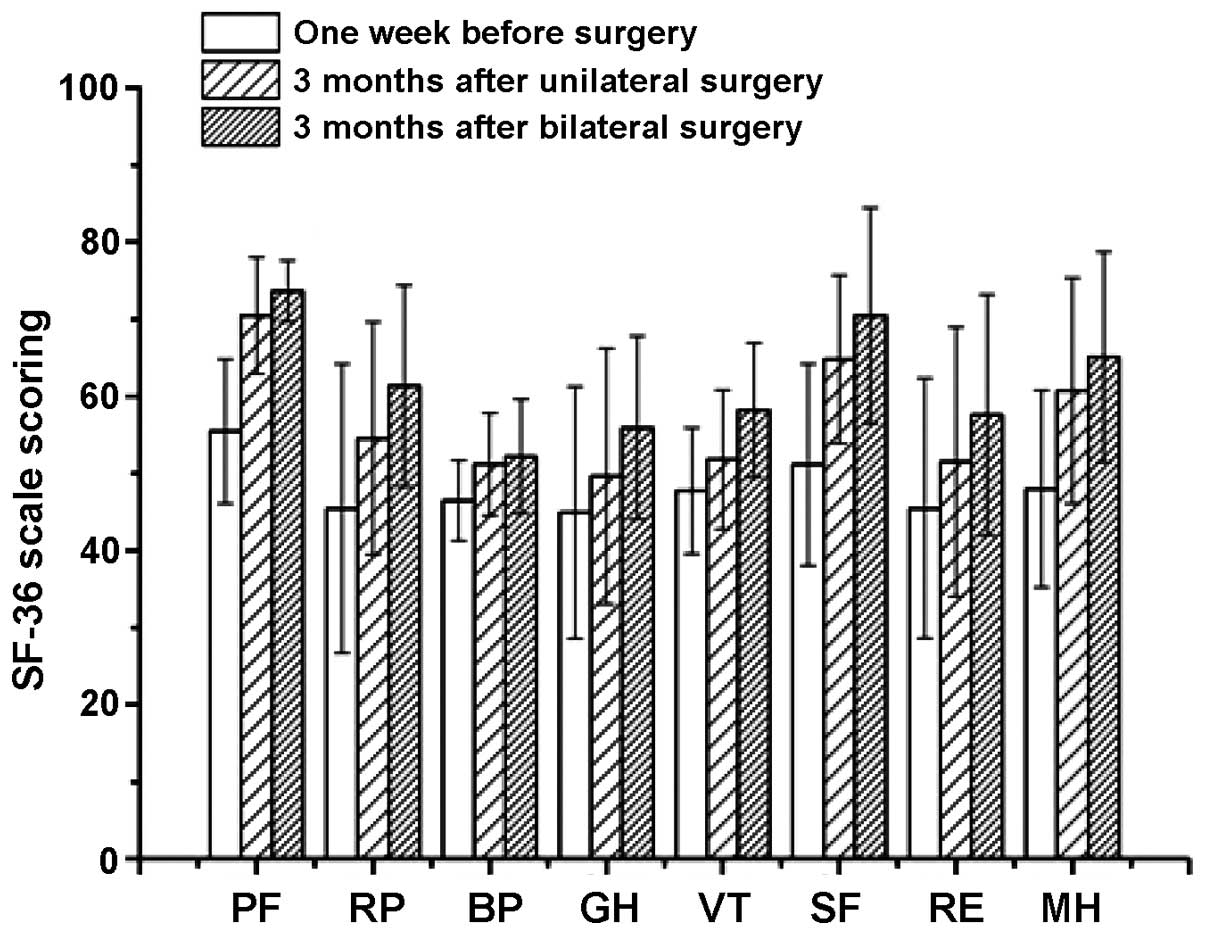
Moreover, the SF-36 included items such as physical
functioning (PF), role-physical (RP), bodily pain (BP), general
health (GH), vitality (VT), social functioning (SF), role-emotional
(RE) and mental health (MH) and were used to evaluate preliminarily
the quality of life. Fig. 2 shows
the scores for the SF-36 scale. Compared with pre-surgery,
short-term life quality of patients after LVRS surgery was greatly
improved and patients could take care of themselves. Comparison of
bilateral and unilateral LVRS surgery was not statistically
significant in terms of lung function and quality of
life(p>0.05).
Discussion
Physical and psychology effects of thoracic surgery
on patients are relatively slight and small. Patients gain
physiologic functions very soon after thoracic surgery (4). The indications for single-port
thoracoscope have been gradually extended (5). Gonzalez-Rivas et al reported on
the single-port thoracoscope bronchus and pulmonary artery double
sleeve pulmonary lobectomy (6). The
mechanism of LVRS involves the excision of 20–40% of the
overventilated lung tissues to increase their elasticity,
adjustment of the ventilation/blood flow ratio, reduction of the
pulmonary heterogeneity to alleviate the respiratory pump failure,
and improvement of alveolar gas exchange. Additionally, the
improvement of pulmonary function and quality of life of the
patients after LVRS could last for 3–4 years (7). For COPE dominated by the superior lobe,
we recommend LVRS (8). It was
reported that the lung function and quality of life of COPE
patients was significantly improved 6 months after simultaneous
bilateral thoracoscopic LVRS (9).
This may be because ventilation efficiency was greatly improved
after LVRS surgery (10).
The incision of single-port thoracoscope was between
the fifth and sixth rib between the anterior axillary line and the
midaxillary line. An endoscopic cut stapler of 5 mm was selected,
with 30̊ angle and rotatable head (11). After one-lung ventilation, due to
obstructive airway obstruction, patients in this group sometimes
had insufficient lung collapse and extensive pleural adhesion, thus
greatly limiting the vision and operation. To avoid the residue of
pulmonary bulla tissues and protect the normal lung tissues, the
incision had to be performed several times, thus resulting in
extended surgical time and a waste of medical resources. The single
direction incison procedure by Liu and the preoperative CT
reconstruction may be utilized to precisely locate the target lung
tissues (12), thus it was a
favorable method to overcome such a limit and save medical
resources. Major complications of LVRS included pulmonary
atelectasis, pulmonary infection and persistent pulmonary leakage.
Overlap of the incisal margins and interlocking suture by 4–0
prolene thread, combined with biogel significantly reduced
post-surgery air leakage (13). The
chest was closed after 10 min of lung filling. Conventionally, 2
chest tubes were inserted individually, with the ends of the tube
placed into the top and bottom of the thoracic cavity. Special care
was given to avoid that the tube did not touch the heart so as to
prevent arrhythmia such as atrial fibrillation after surgery. The
patient were provided with nutrition, assistance in coughing and
expectorating and off-bed activity and were regularly monitored by
chest X-ray to clarify the degree of pulmonary re-expansion. It has
been reported that OK-432 effectively reduces the recurrence of
pneumothorax and the adverse effects were relatively minimal
(14). We used OK-432 to perform
thoracic cavity perfusion on patients after pneumothorax and
pulmonary trachea operation to promote pleural adhesion and have
received quite favorable curative effects.
The major causes of post-surgery pulmonary infection
in patients with chronic obstructive pulmonary disease is increased
sputum secretion and obstructed discharge, most of which are
complicated by tracheal colonization bacteria. The airway passage
needs to be healthy before surgery and thus sensitive antibiotics
should be selected before and after surgery (15). Furthermore, the lung function of
patients with chronic obstructive lung disease is relatively poor,
thus assistant sputum excretion and rehabilitation therapy after
surgery was required (16). In the
present study, patients were treated with conventional small dose
hormone aerosol inhalation to control airway inflammation.
By contrast, patients in our study received partial
resection of the pulmonary lobe, including pulmonary bullae so as
to preserve the reserve function of their lung. Beckers et
al reported that, compared with pulmonary lobe partial
resection, lobectomy could better improve the curative effects on
the lung function of patients with severe emphysema (17). A meta-analysis by Iftikhar et
al indicated that bronchoscopic lung volume reduction (BLVR)
was a simple replacement therapy of emphysema (18). Chen et al confirmed the
curative effects of lung transplantation and LVRS on treating
end-stage emphysema, indicating that compared with LVRS, lung
transplantation could better improve lung function of patients,
blood gas analysis and quality of life after surgery. Therefore, it
was suggested that if conditions permitted, lung transplantation be
considered the first choice of surgical treatment for patients with
end-stage emphysema (19). However,
Trotter and Hopkins demonstrated the role of lung volume reduction
and lung transplantation for treating emphysema. Since there were
few lung donors available, endobronchial valve therapy, bronchial
vapor ablation and LVRS should be considered (20). Shah and Herth reported that
endobronchial valve therapy could significantly improve the lung
function and activity endurance of patients with emphysema
(21).
In conclusion, staged bilateral single-port
thoracoscopic LVRS is safe and effective for treating patients with
COPE combined with pulmonary bullae. Since the sample number of our
study was relatively small, its short-term curative effect still
requires a multi-center, large scale study and its long-term
curative effect requires closer follow-up.
References
|
1
|
Kaplan RM, Sun Q, Naunheim KS and Ries AL:
Long-term follow-up of high-risk patients in the National Emphysema
Treatment Trial. Ann Thorac Surg. 98:1782–1789. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Oey IF, Morgan MD, Spyt TJ and Waller DA:
Staged bilateral lung volume reduction surgery-the benefits of a
patient-led strategy. Eur J Cardiothorac Surg. 37:846–852. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ginsburg ME, Thomashow BM, Yip CK, DiMango
AM, Maxfield RA, Bartels MN, Jellen P, Bulman WA, Lederer D, Brogan
FL, et al: Lung volume reduction surgery using the NETT selection
criteria. Ann Thorac Surg. 91:1556–1560. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhou Y, Liu L, Yu P, Su J, Shen C, Pu Q,
Ma L and Che G: Fast-track recovery of cardiopulmonary function
after complete video-assisted thoracoscopic lobectomy. Chin J Clin
Thorac Cardiovasc Surg. 20:168–171. 2013.
|
|
5
|
Ng CS, Rocco G, Wong RH, Lau RW, Yu SC and
Yim AP: Uniportal and single-incision video-assisted thoracic
surgery: the state of the art. Interact Cardiovasc Thorac Surg.
19:661–666. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gonzalez-Rivas D, Delgado M, Fieira E and
Fernandez R: Double sleeve uniportal video-assisted thoracoscopic
lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg.
3:E22014.PubMed/NCBI
|
|
7
|
Wei H, Bo D, Wang R, et al: Effect of lung
volume reduction surgery for patients with emphysema. China J
Thorac Cardiovasc Surg. 28:312–314. 2012.
|
|
8
|
Clark SJ, Zoumot Z, Bamsey O, Polkey MI,
Dusmet M, Lim E, Jordan S and Hopkinson NS: Surgical approaches for
lung volume reduction in emphysema. Clin Med Lond. 14:122–127.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wei Q, Zhang A, Lin Z, et al: Bilateral
lung volume reduction by video assisted thoracic surgery for 21
cases. Chin J Clin Thorac Cardiovasc Surg. 19:444–446. 2012.
|
|
10
|
Armstrong HF, Dussault NE, Thirapatarapong
W, Lemieux RS, Thomashow BM and Bartels MN: Ventilatory efficiency
before and after lung volume reduction surgery. Respir Care.
60:63–71. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Che G and Liu L: Advancement and progress
of single-port video-assisted thoracoscopic surgery in the
treatment of thoracic diseases. Chin J Clin Thorac Cardiovasc Surg.
19:181–184. 2012.
|
|
12
|
Liu C and Liu L: Uniportal VATS: a
sublimation of micro-invasive lung cancer resection. Zhongguo Fei
Ai Za Zhi. 17:527–530. 2014.(In Chinese). PubMed/NCBI
|
|
13
|
Rathinam S, Naidu BV, Nanjaiah P, Loubani
M, Kalkat MS and Rajesh PB: BioGlue and Peri-strips in lung volume
reduction surgery: pilot randomised controlled trial. J
Cardiothorac Surg. 4:372009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
How CH, Tsai TM, Kuo SW, Huang PM, Hsu HH,
Lee JM, Chen JS and Lai HS: Chemical pleurodesis for prolonged
postoperative air leak in primary spontaneous pneumothorax. J
Formos Med Assoc. 113:284–290. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhi X: Expert consensus of airway
management in Department of Thoracic Surgery. Chin J Clin Thorac
Cardiovasc Surg. 20:251–255. 2013.
|
|
16
|
Mei J, Liu L, Tang M, Xu N, Pu Q, Liu C,
Ma L, Shi H and Che G: Airway bacterial colonization in patients
with non-small cell lung cancer and the alterations during the
perioperative period. J Thorac Dis. 6:1200–1208. 2014.PubMed/NCBI
|
|
17
|
Beckers F, Lange N, Koryllos A, Picchioni
F, Windisch W and Stoelben E: Unilateral lobe resection by
video-assisted thoracoscopy leads to the most optimal functional
improvement in severe emphysema. Thorac Cardiovasc Surg. Dec
23–2014.(Epub ahead of print). PubMed/NCBI
|
|
18
|
Iftikhar IH, McGuire FR and Musani AI:
Efficacy of bronchoscopic lung volume reduction: a meta-analysis.
Int J Chron Obstruct Pulmon Dis. 9:481–491. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chen Y, Chen J and Wang Z: analysis of
clinical outcomes of lung volume reduction surgery and lung
transplantation on end-stage emphysema. Chin J Clin Thorac
Cardiovasc Surg. 19:141–144. 2012.
|
|
20
|
Trotter MA and Hopkins PM: Advanced
therapies for COPD-What's on the horizon? Progress in lung volume
reduction and lung transplantation. J Thorac Dis. 6:1640–1653.
2014.PubMed/NCBI
|
|
21
|
Shah PL and Herth FJ: Current status of
bronchoscopic lung volume reduction with endobronchial valves.
Thorax. 69:280–286. 2014. View Article : Google Scholar : PubMed/NCBI
|