Introduction
Hip fractures are among the most important health
problems in the elderly. Intertrochanteric fracture constitutes one
of the most common fractures of the hip, occurring mainly in
elderly people with osteoporosis (1,2). With
ageing, it is estimated that the number of hip fractures will still
increse in the population. The aim of surgical treatment for the
intertrochanteric fracture is the reduction and stable fixation of
the fracture in order to recover the ability of immediate
mobilization. Early mobilization could reduce the incidence of
fatal complications for the elderly. Intramedullary nail is
currently widely used in the treatment of unstable fractures,
including proximal femoral nail antirotation (PFNA) and Gamma nail
(3–5). For the choice of the head screw in the
intramedullary nail fixation, the bone quality of femoral head is
critically important. The lag screw of Gamma nail can exert
compression effect at the fracture site. It requires good bone
quality of femoral head to provide a sufficient gripping force.
Spiral blade of PFNA can increase the bone density during hammering
in the femoral head and it is more suitable for serious bone loss
of the femoral head in the osteoporosis patients. The bone quality
of femoral head is essential for the choice of head screw and
better choice can decrease the risk of head screw cutting out and
pulling out.
It has been widely reported that the dual-energy
X-ray absorptiometry (DXA) and the quantitative computed tomography
(QCT) were used to assess the bone mineral density (BMD) of femoral
neck and intertrochanteric. DXA is generally used in clinical work
to measure areal BMD at the proximal femur for the diagnosis of
osteoporosis (6,7). Although DXA is widely used to evaluate
BMD in clinical practice, it is well known that the method of DXA
is inadequate for accurate estimation of bone mass. Spatial
accuracy in measuring BMD and morphologic parameters of the
proximal femur by using DXA is limited, because the DXA provides
only plane 2-D images. Furthermore, due to the sheltering of
acetabular, DXA cannot assess the accurate bone mass of femoral
head. Unlike DXA image, the QCT can provide the reconstruct true
three-dimensional images for measuring true morphologic features
and BMD of trabecular bone of the femoral head (8–11). In
this study, we aimed to quantify differences in trabecular BMD of
the femoral head between patients with proximal femoral fractures
and healthy subjects in the control group by using QCT and the
conclusion may provide some guidance for the choice of head screw
in the intramedullary nail fixation.
Materials and methods
Patients and volunteers
We recruited participants who suffered
intertrochanteric fractures in Beijing Jishuitan Hospital from
January 2013 to December 2014. There were total of 536 patients
with fractures (fracture group, average age was 65.8±17.3 years)
entered into the study. In addition, we recruited 497 cases of
fracture-free, age-matched controls (control group, average age was
66.2±10.4 years) as part of a larger study. Descriptive
characteristics for the subjects are provided in Table I. This study was approved by the
Ethics Committee of Beijing Jishuitan Hospital. Patients agreed to
the use of their samples in scientific research.
 | Table I.Characteristics of the two groups. |
Table I.
Characteristics of the two groups.
| Parameters | Fracture group | Control group |
|---|
| No. of patients | 536 | 497 |
| Male/Female | 202/334 | 212/285 |
| Age (years) | 65.8±17.3 | 66.2±10.4 |
CT scan acquisition
The subjects were scanned by using a multidetector
CT scanner (LightSpeed CT; GE Medical Systems, Fairfield, CT, USA)
with standard protocol scanning from the iliac crest to the knee.
Scanning parameters were 120 kVp, 350 mA, slice thickness was 2.5
mm, and 512×512 matrix in a spiral reconstruction mode with a 36-cm
field of view.
Image processing
We measured volumetric BMD (g/cm3) using
commercial software (QCT Pro; Mindways Software, Inc., San
Francisco, CA, USA) at the proximal femur. A midcoronal
multi-planar reconstruction (MPR) view of the uninjured
contralateral proximal femur in the fracture group, and of the
bilateral proximal femur in the control group was reconstructed
using commercially available image analysis software (Virtual
Place-M; Medical Imaging Laboratory, Tokyo, Japan). Trabecular BMD
in the region of interest (ROI) was measured by tracing the
trabecular region.
We used in-house software developed using the
Visualization Toolkit (VTK 5.6; Kitware Inc., Clifton Park, NY,
USA) to calibrate the CT-measured density values based on the
calibration phantom and rescaled the images using cubic
interpolation to 1.0-mm isotropic voxels.
Determination of ROI
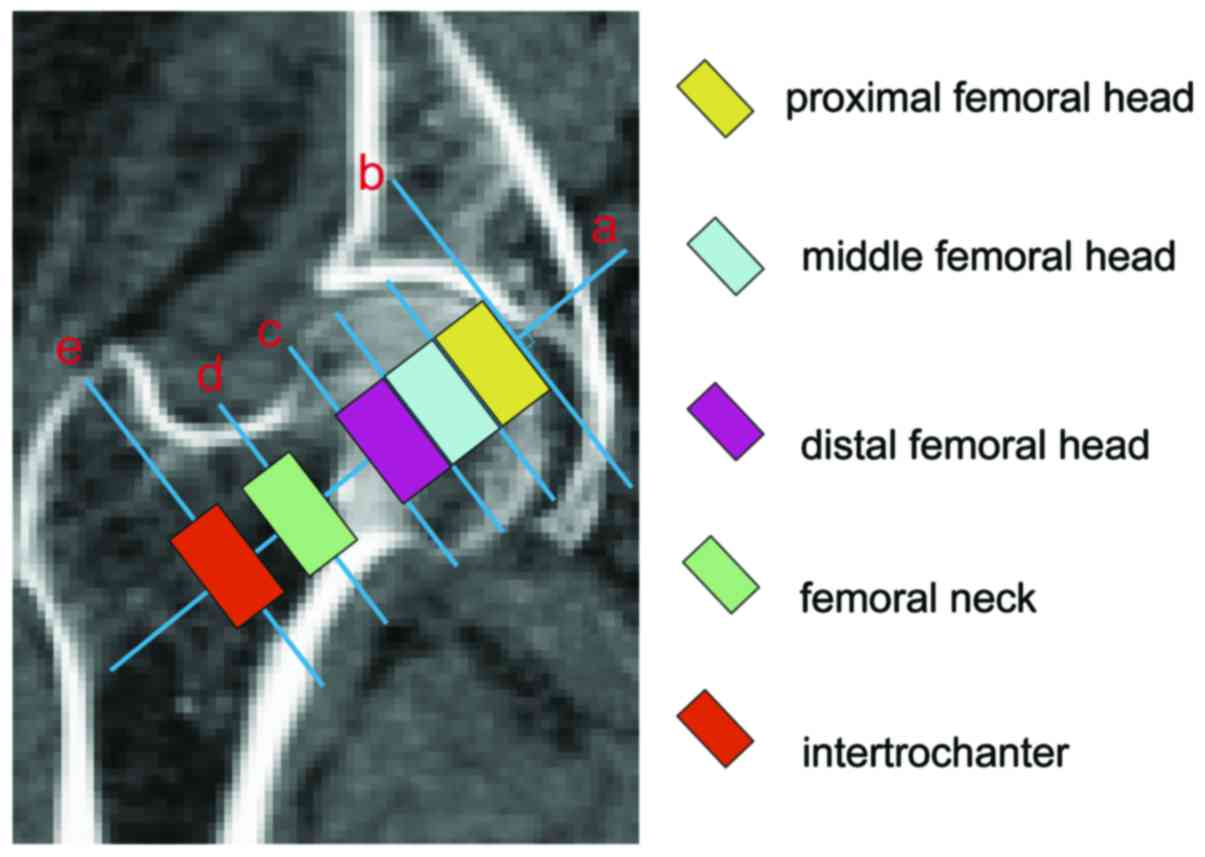
CT images were used to determine the ROI in the
proximal femur. Femural head was divided into three parts:
Proximal, middle and distal femoral head. Fig. 1 shows: line a, femoral neck axis
through the femoral head center; line b, tangent to the femoral
head and perpendicular to the line a along with intersection of
point A; line c, the boundary of femoral head and femoral neck;
line d, midline of femoral neck; and line e, midline of
intertrochanter. Five regions in different color in Fig. 1 represent five ROI of proximal,
middle and distal femoral head, femoral neck and intertrochanter.
BMD of femoral head was the mean values of proximal, middle and
distal femoral head. Each area included nine slices for the CT
images.
Statistical analysis
Comparisons of the two data sets were analyzed by
t-test, and data with more than two variables were analyzed by
two-way repeated measure-ANOVA with Tukey's post hoc test analysis.
All data are plotted as the mean ± standard error.
Results
No significant difference existed in the age between
the two groups (P>0.05) (Table
I). For control group, results showed no marked difference of
BMD between left and right proximal femur for all regions
(P>0.05). However, BMD in different ROIs was significantly
different. Results revealed that BMD of femoral head was remarkably
larger than that of femoral neck and intertrochanter in the control
group (Table II).
 | Table II.Comparison of bilateral BMD at
different regions for subjects in the control group. |
Table II.
Comparison of bilateral BMD at
different regions for subjects in the control group.
| Regions | Left | Right | P-value |
|---|
| BMD at head
(mg/cm3) | 232.5±39.3 | 228.4±38.4 | 0.753 |
| BMD at neck
(mg/cm3) | 77.1±39.4 | 74.9±41.2 | 0.641 |
| BMD at
intertrochanter(mg/cm3) | 73.6±44.7 | 74.1±43.8 | 0.683 |
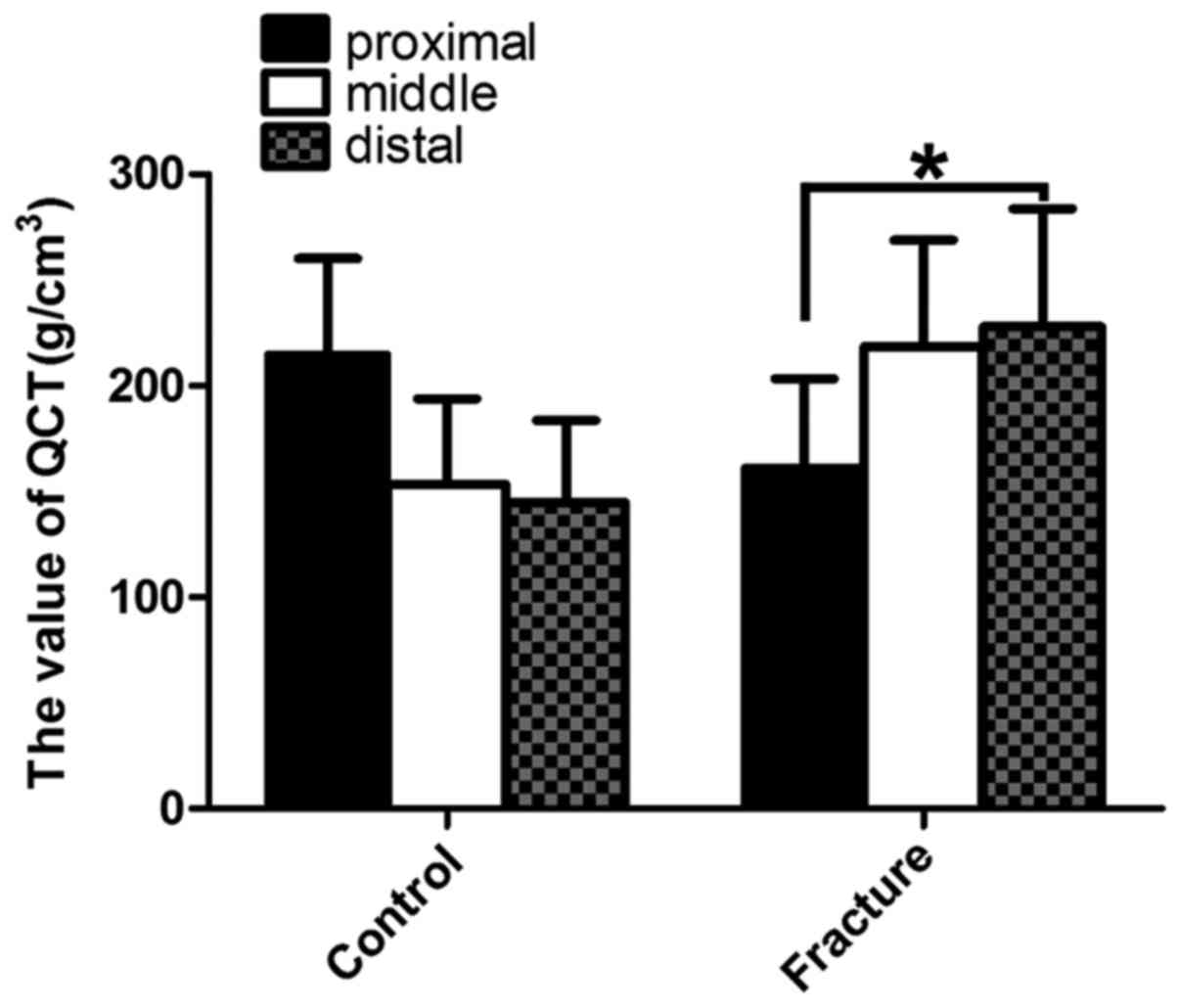
Further, we compared BMD between the two groups in
different ROIs and found that BMD of proximal femur in the fracture
group was obviously lower than that in the control group
(P<0.05) (Table III).
Furthermore, the BMD differences at distinct regions for male and
female were statistically significant between two groups (Tables IV and V). The BMD of proximal femoral head was
higher than other two parts of the head, but not statistically
significant in the control group (P>0.05). However, in the
fracture group, the BMD of proximal femoral head was significantly
lower than the distal part of the head (P<0.05) (Fig. 2).
 | Table III.Comparison of BMD at different regions
in the two groups. |
Table III.
Comparison of BMD at different regions
in the two groups.
| Regions | Control group
(left) | Trochanteric
fracture | P-value |
|---|
| BMD at head
(mg/cm3) | 232.5±39.3 | 161.2±39.4 | <0.001 |
| BMD at neck
(mg/cm3) | 77.1±39.4 | 26.9±37.5 | <0.001 |
| BMD at
intertrochanter(mg/cm3) | 73.6±44.7 | 27.6±31.3 | <0.001 |
 | Table IV.BMD of proximal femur and femoral head
are not parallels. |
Table IV.
BMD of proximal femur and femoral head
are not parallels.
|
| Control ICR | Fracture ICR |
|---|
|
|
|
|
|---|
| Regions | Male | Female | Male | Female |
|---|
| Between head and
neck, % | 38.1 | 18.0 | 22.0 | 27.1 |
| Between head and
intertrochanter, % | 9.5 | 19.5 | 20.3 | 32.9 |
 | Table V.Comparison of BMD at different
regions for male subjects in the two groups. |
Table V.
Comparison of BMD at different
regions for male subjects in the two groups.
| Regions | Control group
(N=212) | Trochanteric
fracture (N=202) | P-value |
|---|
| BMD at head
(mg/cm3) | 241.5±41.5 | 165.2±41.8 | <0.001 |
| BMD at neck
(mg/cm3) | 79.9±38.8 | 27.7±38.3 | <0.001 |
| BMD at
intertrochanter(mg/cm3) | 75.6±44.7 | 29.9±36.1 | <0.001 |
For some subjects in the two groups, we found that
the trend of BMD changes among the femoral head, femoral neck and
intertrochanter were not parallels in terms of their average value.
In the control group, there were 81 male and 51 female subjects who
had different trends of change between the femoral head and femoral
neck (male, 81/212; female, 51/285), and 20 male and 56 female
subjects between the femoral head and intertrochanter (male,
20/212; female, 56/285). Moreover, in the fracture group, there
were 44 male and 91 female subjects in the femoral head and femoral
neck (male, 44/202; female, 91/334), and 41 male and 110 female
subjects in the femoral head and intertrochanter (male, 41/202;
female, 110/334) (Table VI).
 | Table VI.Comparison of BMD at different
regions for female subjects in the two groups. |
Table VI.
Comparison of BMD at different
regions for female subjects in the two groups.
| Regions | Control group
(N=285) | Trochanteric
fracture (N=334) | P-value |
|---|
| BMD at head
(mg/cm3) | 221.7±43.8 | 156.2±37.6 | <0.001 |
| BMD at neck
(mg/cm3) | 75.1±39.4 | 25.4±38.9 | <0.001 |
| BMD at
intertrochanter(mg/cm3) | 70.8±43.9 | 25.6±30.9 | <0.001 |
Discussion
This study was aimed at quantifying the differences
in trabecular BMD among the femoral head, neck and
intertrochanteric for the healthy subjects in the control group and
patients in the fracture group by using quantitative computed
tomography to provide some guidance for the choice of head screw in
the intramedullary nail fixation.
In the literature, it has been reported that helical
blade behaves differently to a screw in the femoral head. Both
screw systems (SHS and Gamma 3) and helical blades (PFNA and
trochanteric fixation nail (TFN) are, respectively, suitable for
different populations. A biomechanical study has shown that the
blade device is more prone to cutout by comparing threaded screw
with helical blade constructs in a model of pertrochanteric
fracture fixation using polyurethane femoral heads. The main reason
described was that the blade device presents a lesser contact
surface to the cancellous bone in the axial direction due to its
shape of helical blade. Furthermore, they reported an axial contact
surface of 75 mm2 for the PFNA blade and 300
mm2 for the Gamma 3 screw (12). Xu et al found no cut-out in
the Gamma and PFNA groups, but in their study, the femoral head
condition was not described (13).
It has been reported that the initiating factors of mechanical
failure in femoral cutout include the position of screw or blade,
quality of bone and inappropriate rehabilitation (14,15). It
has been reported that both screw systems and helical blades fail
if the screw or blade was not optimally positioned, and thus that
the center-center position in the head of femur of any kind of lag
screw or blade is to be achieved to minimize rotation of the
femoral head and to prevent further mechanical complications
(16–19). For the choice of the head screw in
the intramedullary nail fixation, the bone quality of femoral head
is critically important. The lag screw requires good bone quality
of femoral head, and high density bone to provide a sufficient
gripping force (5,20,21). On
the contrary, the spiral blade of PFNA is more suitable for serious
bone loss of the femoral head in the osteoporosis patients. The
main reason is that it can increase the bone density during
hammering in the femoral head (3,4). Thus,
the bone quality of femoral head is essential for the choice of
head screw and a better choice can decrease the risk of head screw
cutting out and pulling out.
In our study, we showed that the BMD of hip for male
are greater than that for females, and therefore evaluation of BMD
values after dividing subjects into male and female groups would be
preferable (22,23). It has been reported that the BMD of
elderly was smaller than that of young by QCT and DXA due to
osteoporosis, metabolism and hormone (23–25).
Thus, this study was an age-matched study in order to avoid the
impact of age factor on the BMD of hip, and there was no
significant difference in the age between control and fracture
groups. There was significant difference in the proximal femoral
BMD between the control and fracture groups. It illustrated that
osteoporosis was an independent factor for the hip fracture and was
consistent with previous studies (26,27).
There is no perfect method for assessment of bone
quality of femoral head. Lack of theoretical basis for the choice
of head screw in the intramedullary nail fixation is an important
issue to be solved in the clinical practice (28). It has been reported that QCT has
become a useful research tool for analyzing hip geometry and
measuring BMD (29–31). However, it has not yet been widely
used in clinical practice (27,32). We
believe that the QCT can provide the reconstructed true
three-dimensional images for measuring true morphologic features
and BMD of trabecular bone of the femoral head, which was not
influenced by the bone overlapping around the femoral head by the
2-D images such as DAX (30,31,33).
Furthermore, QCT as an important preoperative assessment can
provide better guidance for the choice of head screw in the
intramedullary nail fixation.
There are some limitations to our findings. First,
the measured BMD was of the hip not on the fractured side, but on
the contralateral side. However, we have compared the sides in the
control group. Thus, the BMD of the proximal femur on both sides
generally are considered similar in this study. Second, the results
of our study cannot be used to identify risk factors for hip
fractures, because the relationship between BMD and mechanical
feature of the hip remains unclear. Thirdly, the range of normal
value in the healthy population did not result from large number of
samples. Thus, further research of expanding the normal sample size
is in progress.
In conclusion, osteoporosis is a risk factor for the
proximal femoral fracture, and the BMD of proximal femoral head
could not alone represent the femoral head. Thus, the preoperative
QCT assessment of femoral head is indispensable option for the
assessment of femoral head bone loss and it may provide some
guidance for the choice of head screw in the intramedullary nail
fixation.
References
|
1
|
Xue L, Zha L, Chen Q, Liang YJ, Li KR,
Zhou Z, Guan JL, Qin H and Li YP: Randomized controlled trials of
proximal femoral nail antirotation in lateral decubitus and supine
position on treatment of intertrochanteric fractures. Sci World J.
2013:2760152013. View Article : Google Scholar
|
|
2
|
Foss NB and Kehlet H: Hidden blood loss
after surgery for hip fracture. J Bone Joint Surg Br. 88:1053–1059.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yang YH, Wang YR, Jiang SD and Jiang LS:
Proximal femoral nail antirotation and third-generation Gamma nail:
which is a better device for the treatment of intertrochanteric
fractures? Singapore Med J. 54:446–450. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ostrum RF, P III Tornetta, Watson JT,
Christiano A and Vafek E: Ipsilateral proximal femur and shaft
fractures treated with hip screws and a reamed retrograde
intramedullary nail. Clin Orthop Relat Res. 472:2751–2758. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
McCormack R, Panagiotopolous K, Buckley R,
Penner M, Perey B, Pate G, Goetz T and Piper M: A multicentre,
prospective, randomised comparison of the sliding hip screw with
the Medoff sliding screw and side plate for unstable
intertrochanteric hip fractures. Injury. 44:1904–1909. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Watts NB: Fundamentals and pitfalls of
bone densitometry using dual-energy X-ray absorptiometry (DXA).
Osteoporos Int. 15:847–854. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tauchmanovà L, Nuzzo V, Del Puente A,
Fonderico F, Esposito-Del Puente A, Padulla S, Rossi A, Bifulco G,
Lupoli G and Lombardi G: Reduced bone mass detected by bone
quantitative ultrasonometry and DEXA in pre- and postmenopausal
women with endogenous subclinical hyperthyroidism. Maturitas.
48:299–306. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shim VB, Pitto RP and Anderson IA:
Quantitative CT with finite element analysis: towards a predictive
tool for bone remodelling around an uncemented tapered stem. Int
Orthop. 36:1363–1369. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ramamurthi K, Ahmad O, Engelke K, Taylor
RH, Zhu K, Gustafsson S, Prince RL and Wilson KE: An in vivo
comparison of hip structure analysis (HSA) with measurements
obtained by QCT. Osteoporos Int. 23:543–551. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kalkwarf HJ, Laor T and Bean JA: Fracture
risk in children with a forearm injury is associated with
volumetric bone density and cortical area (by peripheral QCT) and
areal bone density (by DXA). Osteoporos Int. 22:607–616. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ito M, Wakao N, Hida T, Matsui Y, Abe Y,
Aoyagi K, Uetani M and Harada A: Analysis of hip geometry by
clinical CT for the assessment of hip fracture risk in elderly
Japanese women. Bone. 46:453–457. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Born C, Karich B, Bauer C, von Oldenburg G
and Augat P: Hip screw migration testing: first results for hip
screws and helical blades utilizing a new oscillating test method.
J Orthop Res. 29:760–766. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Xu Y, Geng D, Yang H, Wang X and Zhu G:
Treatment of unstable proximal femoral fractures: comparison of the
proximal femoral nail antirotation and gamma nail 3. Orthopedics.
33:4732010.PubMed/NCBI
|
|
14
|
O'Malley NT, Deeb AP, Bingham KW and Kates
SL: Outcome of the dynamic helical hip screw system for
intertrochanteric hip fractures in the elderly patients. Geriatr
Orthop Surg Rehabil. 3:68–73. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Frei HC, Hotz T, Cadosch D, Rudin M and
Käch K: Central head perforation, or ‘cut through,’ caused by the
helical blade of the proximal femoral nail antirotation. J Orthop
Trauma. 26:e102–e107. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Goffin J, Pankaj P and Simpson A: The
importance of lag screw position for the stabilization of
trochanteric fractures with a sliding hip screw: a subject-specific
finite element study. J Orthop Res. 31:596–600. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kuzyk PR, Zdero R, Shah S, Olsen M,
Waddell JP and Schemitsch EH: Femoral head lag screw position for
cephalomedullary nails: a biomechanical analysis. J Orthop Trauma.
26:414–421. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schwarzkopf R, Takemoto RC, Kummer FJ and
Egol KA: Helical blade vs telescoping lag screw for
intertrochanteric fracture fixation. Am J Orthop (Belle Mead NJ).
40:452–456. 2011.PubMed/NCBI
|
|
19
|
Geller JA, Saifi C, Morrison TA and
Macaulay W: Tip-apex distance of intramedullary devices as a
predictor of cut-out failure in the treatment of peritrochanteric
elderly hip fractures. Int Orthop. 34:719–722. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Laohapoonrungsee A, Arpornchayanon O and
Phornputkul C: Two-hole side-plate DHS in the treatment of
intertrochanteric fracture: Results and complications. Injury.
36:1355–1360. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Verettas DA, Ifantidis P, Chatzipapas CN,
Drosos GI, Xarchas KC, Chloropoulou P, Kazakos KI, Trypsianis G and
Ververidis A: Systematic effects of surgical treatment of hip
fractures: gliding screw-plating vs intramedullary nailing. Injury.
41:279–284. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Keyak JH, Sigurdsson S, Karlsdottir G,
Oskarsdottir D, Sigmarsdottir A, Zhao S, Kornak J, Harris TB,
Sigurdsson G, Jonsson BY, et al: Male-female differences in the
association between incident hip fracture and proximal femoral
strength: a finite element analysis study. Bone. 48:1239–1245.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Marshall LM, Zmuda JM, Chan BK,
Barrett-Connor E, Cauley JA, Ensrud KE, Lang TF and Orwoll ES:
Osteoporotic Fractures in Men (MrOS) Research Group: Race and
ethnic variation in proximal femur structure and BMD among older
men. J Bone Miner Res. 23:121–130. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nicks KM, Amin S, LJ III Melton, Atkinson
EJ, McCready LK, Riggs BL, Engelke K and Khosla S:
Three-dimensional structural analysis of the proximal femur in an
age-stratified sample of women. Bone. 55:179–188. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ohnaru K, Sone T, Tanaka K, Akagi K, Ju
YI, Choi HJ, Tomomitsu T and Fukunaga M: Hip structural analysis: a
comparison of DXA with CT in postmenopausal Japanese women.
Springerplus. 2:3312013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Vochteloo AJ, van der Burg BL Borger,
Röling MA, van Leeuwen DH, van den Berg P, Niggebrugge AH, de Vries
MR, Tuinebreijer WE, Bloem RM, Nelissen RG, et al: Contralateral
hip fractures and other osteoporosis-related fractures in hip
fracture patients: incidence and risk factors. An observational
cohort study of 1,229 patients. Arch Orthop Trauma Surg.
132:1191–1197. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lau EM, Suriwongpaisal P, Lee JK, Das De
S, Festin MR, Saw SM, Khir A, Torralba T, Sham A and Sambrook P:
Risk factors for hip fracture in Asian men and women: the Asian
osteoporosis study. J Bone Miner Res. 16:572–580. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Herman A, Landau Y, Gutman G, Ougortsin V,
Chechick A and Shazar N: Radiological evaluation of
intertrochanteric fracture fixation by the proximal femoral nail.
Injury. 43:856–863. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Nishiyama KK, Ito M, Harada A and Boyd SK:
Classification of women with and without hip fracture based on
quantitative computed tomography and finite element analysis.
Osteoporos Int. 25:619–626. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Khoo BC, Brown K, Zhu K, Pollock M, Wilson
KE, Price RI and Prince RL: Differences in structural geometrical
outcomes at the neck of the proximal femur using two-dimensional
DXA-derived projection (APEX) and three-dimensional QCT-derived
(BIT QCT) techniques. Osteoporos Int. 23:1393–1398. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Maeda Y, Sugano N, Saito M and Yonenobu K:
Comparison of femoral morphology and bone mineral density between
femoral neck fractures and trochanteric fractures. Clin Orthop
Relat Res. 469:884–889. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Walker MD, Saeed I, McMahon DJ, Udesky J,
Liu G, Lang T and Bilezikian JP: Volumetric bone mineral density at
the spine and hip in Chinese American and White women. Osteoporos
Int. 23:2499–2506. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Liu XS, Cohen A, Shane E, Yin PT, Stein
EM, Rogers H, Kokolus SL, McMahon DJ, Lappe JM, Recker RR, et al:
Bone density, geometry, microstructure, and stiffness:
relationships between peripheral and central skeletal sites
assessed by DXA, HR-pQCT, and cQCT in premenopausal women. J Bone
Miner Res. 25:2229–2238. 2010. View
Article : Google Scholar : PubMed/NCBI
|