Introduction
Sarcoidosis is a systemic inflammatory disorder of
unknown etiology, which is characterized and defined by the
presence of non-caseating granulomata. The incidence of this
multisystem disease is 10–15 cases per 100,000 each year (1). The development of sarcoidosis has been
associated with a number of environmental factors, genes, immune
factors, and exposure to certain microbial agents (1). Approximately 25% of sarcoidosis may
have cutaneous involvement, with a variety of clinical
presentations (2) and pulmonary
involvement occurs in 90–95% of cases. Therefore patients with
cutaneous sarcoidosis require an evaluation of symptoms that may be
caused by extracutaneous diseases (1). Among cutaneous sarcoidosis, scar
sarcoidosis is rare and occurs predominantly in young adults,
particularly in females (2). The
present study reports the case of an elderly female patient who
developed scar sarcoidosis in 20-year-old scars initially acquired
in a traffic accident.
Case report
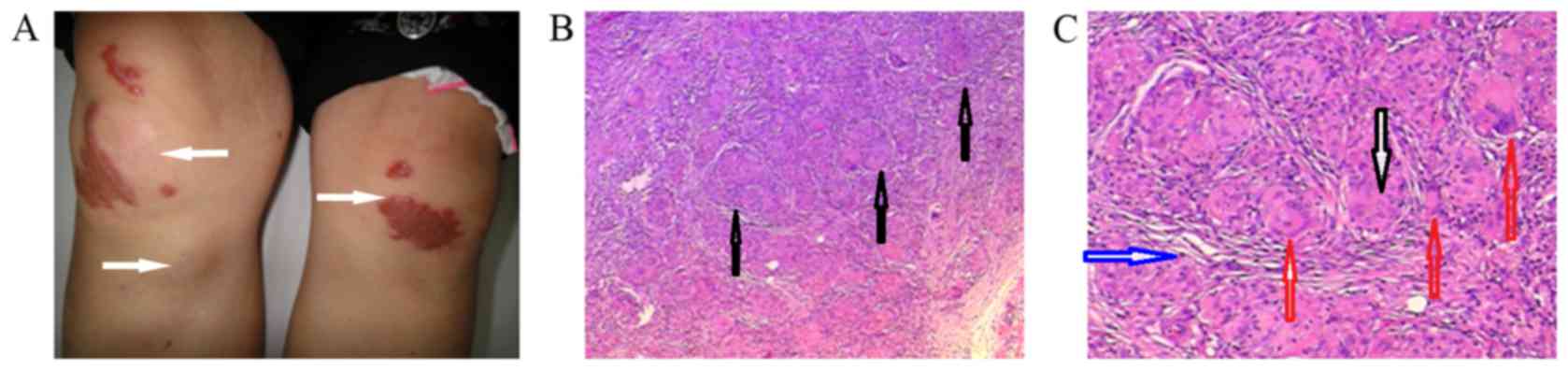
A 70-year-old female patient presented painful
reactivation of 20-year-old-scars located on the knees, originally
acquired in a traffic accident. The patient suffered localized scar
pain without itching for two months prior to her visit to the
outpatient dermatology clinic at the Dermatology Department of the
Clinical Medical School of Yangzhou University on 12th October
2012. Systemic symptoms such as weight loss, fever and cough were
also absent and systematic physical examinations for the
respiratory, cardiovascular and nervous systems, such as lung and
heart auscultation, reported normal results. However,
dermatological physical examinations found erythematous swelling
and small papules localized to the knee scars and, on the right
knee, two subcutaneous indurated nodules, one 3×5 cm in size and
another one 2×3 cm in size, were found under and below the scars,
respectively (Fig. 1A).
The patient additionally underwent auxiliary
examinations, including a complete blood count and tests to
determine erythrocyte sedimentation rate, c-reactive protein and
electrolyte levels, and liver and renal function, which identified
no pathological findings. Blood levels of angiotensin-converting
enzyme, typically used to aid in the diagnosis of sarcoidosis
(2), was 52 IU/l (reference range
24–65 IU/l), and the urinary analysis was found to be normal. The
tuberculosis skin test also reported negative results (the size of
red nodule in test site was >5 mm). However, a biopsy was
carried out on the skin lesion and histopathology under light
microscopy (Olympus CX41; Olympus Corporation, Tokyo, Japan) of the
tissue revealed multiple non-caseating granulomas composed of
epithelioid cells, numerous multinucleated giant cells and a small
number of lymphocytes (Fig. 1B and
C).
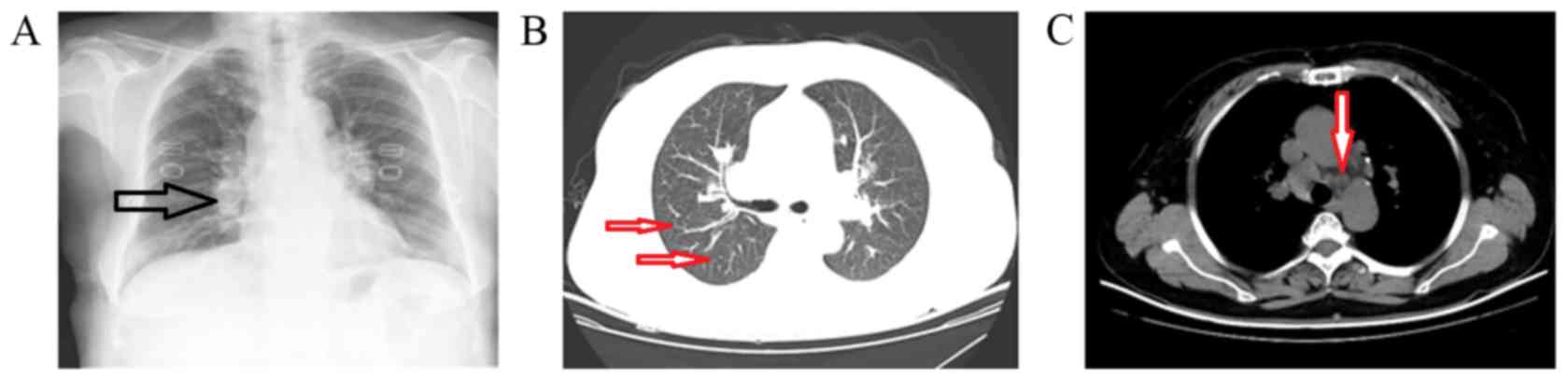
The patient's chest was also examined. A chest x-ray
revealed bilateral hilar lymphadenopathy (Fig. 2A), while computer tomography of the
chest revealed multiple obscure tubercles (largest one ~10 mm in
size) in the lungs and swollen lymph nodes in the hilum pulmonis
and mediastinum (Fig. 2B and C).
Following the diagnosis of scar sarcoidosis, the patient refused
treatment. The patient provided informed written consent for her
data to be used in the present study.
Discussion
Sarcoidosis is a systemic disease with an unknown
etiology. The disease is characterized by the formation of
epithelioid granulomas that lack caseations, with skin lesions
occurring in 20–25% of cases (2).
The diversity of clinical presentations mean that sarcoidosis is
difficult to diagnose. Disease diagnosis requires a combination of:
i) Supporting clinical-radiological findings such as hilar and/or
paratracheal lymph node enlargement with or without pulmonary
infiltrates; ii) histological evidence of non-caseating epithelioid
granulomas at disease sites; and iii) exclusion of alternative
causes for the granulomatous inflammation and local sarcoid-like
reactions (3). Skin lesions in
sarcoidosis may appear as maculae, papules, plaques, nodules,
ulcers, localized alopecia, ichthyotic areas, subcutaneous nodules,
lupus pernio, scar sarcoidosis, psoriasiform and even pustules.
Among these, scar sarcoidosis is rare, accounting for 5.4–13.8% of
sarcoidosis cases (4,5). The present case of scar sarcoidosis is
the third to be recorded in China (6,7).
Scar sarcoidosis is characterized by the onset of
erythematous swelling and the development of papules and nodules
within the original scars. In cases of cutaneous or subcutaneous
swelling in the area of an old scar or beside a scar, a scar
sarcoidosis is a possible differential diagnosis (1). Excluding skin damaged by mechanical
injury, scar sarcoidosis can occur on skin sites damaged by a range
of factors, including venipuncture, intramuscular injections,
inoculations, tattoos and infections such as herpes zoster
(8). It is suggested that foreign
material within the scar, deposited by external factors including
those stated above, is a possible cause of epithelioid granuloma
(9). The specific skin lesions that
occur and the resulting sarcoidosis may be associated with the
severity and duration of the disease, with scar sarcoidosis often
being accompanied by systemic involvement (4). Alterations, such as further damage or
stress to the existing scars, often prompt worsening of sarcoidosis
(10).
The case of scar sarcoidosis presented here is an
elderly woman, displaying no other health problems, including
tuberculosis and hepatitis. The patient visited the clinic due to
the development of painful nodules and erythematous swelling on
preexisting scars located on her knees, which formed following a
traffic accident 20 years prior. Although the patient did not
report any systemic symptom, physical examinations found that she
had stage II pulmonary involvement in the sarcoidosis, while all
other organs were not involved. As chest X-ray or computed
tomography scan examination was not performed on the patient within
several years, it could not be determined whether the onset of
pulmonary involvement occurred before or after scar sarcoidosis;
however the majority of patients with scar sarcoidosis develop
systemic disease (8). Therefore, it
is necessary for patients who are presenting with painful
inflammation on or around their existing scars to be examined
systematically and followed up. Standard therapies for sarcoidosis
include the administration of corticosteroids, antimalarials and
methotrexate (11). However, scar
sarcoidosis often resolves slowly and spontaneously (4). Thus, the patient in the present case
refused treatment. Alternative second-line drug treatments include
methotrexate and hydroxychloroquine; however, these agents are not
100% effective (12). For patients
with progressive cutaneous sarcoidosis or refractory cases,
monoclonal antibodies are a novel therapeutic option. For example,
etanercept antibodies (3,13) that target tumor necrosis factor-α
have been demonstrated to be beneficial in treating recalcitrant
sarcoidosis. In the treatment of scar sarcoidosis, injection of the
corticosteroid triamcinolone acetonide into the skin lesions is
also effective (8). Furthermore, it
is necessary to continually survey patients via pulmonary
examination and chest radiography every two months, as well as
periodic monitoring for other systemic manifestations (8).
Unfortunately, a follow-up of the patient in the
present case was not possible. Contact with the patient was
attempted on numerous occasions; however the contact information
provided was invalid.
References
|
1
|
Henrichs MP, Streitbürger A, Gosheger G,
Surke C, Dierkes C and Hardes J: Scar sarcoidosis on a finger
mimicking a rapidly growing soft tissue tumour: A case report. BMC
Res Notes. 5:545–549. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fernandez-Faith E and McDonnell J:
Cutaneous sarcoidosis: Differential diagnosis. Clin Dermatol.
25:276–287. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Spagnolo P: Sarcoidosis: A critical review
of history and milestones. Clin Rev Allergy Immunol. 49:1–5. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Marchell RM and Judson MA: Chronic
cutaneous lesions of sarcoidosis. Clin Dermatol. 25:295–302. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mana J, Marcoval J, Graells J, Salazar A,
Peyrí J and Pujol R: Cutaneous involvement in sarcoidosis.
Relationship to systemic disease. Arch Dermatol. 133:882–888. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shen B, Chen XL and Wu LM: Scar
sarcoidosis: First case report in China. Chin J Dermatol. 44:91–93.
2011.
|
|
7
|
Zeng YP, Jiang GT, Qu T, Ma DL, Liu YH,
Jin HZ and Sun QN: A case report of Scar sarcoidosis. Chin J
Dermatol. 44:211–212. 2011.(In Chinese).
|
|
8
|
Choi SY, Hyun MY, No YA, Park KY, Li K,
Kim BJ, Seo SJ, Kim MN and Hong CK: Scar sarcoidosis on a
hypertrophic scar. Clin Exp Dermatol. 39:945–947. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cervigon I, Palomo A and Torres LM:
Cutaneous lesions on scars. Actas Dermosifiliogr. 98:433–434.
2007.(In Spanish). PubMed/NCBI
|
|
10
|
Marcoval J, Mañá J and Rubio M: Specific
cutaneous lesions in patients with systemic sarcoidosis:
Relationship to severity and chronicity of disease. Clin Exp
Dermatol. 36:739–744. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Doherty CB and Rosen T: Evidence-based
therapy for cutaneous sarcoidosis. Drugs. 68:1361–1383. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Haimovic A, Miguel S, Judson MA and
Prystowsky S: Sarcoidosis: A comprehensive review and update for
the dermatologist: Part I. Cutaneous disease. J Am Acad Dermatol.
66:699.e1–e18. 2012. View Article : Google Scholar
|
|
13
|
Tuchinda C and Wong HK: Etanercept for
chronic progressive cutaneous sarcoidosis. J Drugs Dermatol.
5:538–540. 2006.PubMed/NCBI
|