Introduction
Liver cancer is the sixth most common cancer
worldwide with varying geographic distribution. High incidence
rates have been reported in developing countries, particularly in
China (~26 per 100,000 people) when compared with developed
countries (~10 per 100,000 people) (1). Early diagnosis of liver cancer remains
a major obstacle and typically results in poor outcomes after
clinical intervention (2). Resection
of tumors is a common intervention to increase the survival of
patients (3). However, large tumors
within the liver and multiple metastases require complete resection
in order to improve the long-term survival of patients, and
numerous approaches have been attempted to achieve complete
resection (3). Staged hepatectomy
and approaches to induce hypertrophy, including percutaneous portal
vein embolization and intraoperative portal vein ligation, are
recent advances in liver surgery (4). Schnitzbauer et al (5) indicated that a two-staged hepatectomy
was performed for the first time in a patient with hilar
cholangiocarcinoma in 2007 and that associating liver partition and
portal vein ligation for staged hepatectomy (ALPPS), a surgical
approach for liver cancer with excessive tissue resection, was
first described in 2012. However, ALPPS surgery has several
limitations, including a large wound surface, incomplete drainage
and high mortality rates (5,6). Acute liver and renal failure and
infectious complications have been identified as predominant causes
for mortality (6). Numerous
modifications to the originally described ALPPS approach have been
reported (7). Previous studies have
demonstrated that careful selection of specific patients for ALPPS
resulted in reduced or no associated mortality (5,6). In
February 2015, the first international consensus meeting concerning
ALPPS was conducted in Germany, and the following recommendations
were made via patient selection and inclusion criteria: ALPPS would
only be considered for patients requiring right trisectionectomy,
patients with hepatocellular carcinoma or cholangiocarcinoma and
patients with extensive bilobar colorectal liver metastases
requiring an extended hepatectomy (7). Furthermore, in cases where portal vein
embolization or portal vein ligation failed, ALPPS may be an
alternative surgery. Hence, ALPPS is a novel surgical technique
that has been indicated for use in specific patients with liver
cancer.
Negative pressure wound therapy (NPWT; also known as
vacuum-assisted closure) is a therapeutic approach that utilizes a
vacuum dressing to promote the healing of large wounds and vacuum
sealing drainage (VSD; Wuhan VSD Medical Science & Technology
Corp., Wuhan, China) is one of the novel NPWT techniques (8). In VSD, the commonly used polyurethane
material is replaced by polyvinyl alcohol (PVA) (9). PVA has higher tissue compatibility and
tensile strength that does not result in debris shedding or stick
to surrounding tissues (9).
Considering the aforementioned characteristics of PVA, the VSD
technique may be used to improve wound healing in ALPPS surgery.
Hence, the present case report describes a patient with liver
cancer who underwent ALPPS surgery and co-application of NPWT to
heal the large wound and improve the outcome of therapeutic
intervention.
Case report
Ethical statement
The present case study was approved by the Ethics
Committee of The Fourth Affiliated Hospital of Harbin Medical
University (Harbin, China). Written informed consent was obtained
from the patient.
Presenting concerns
In November 2014, a 46-year-old male patient was
hospitalized in the Department of General Surgery at The Fourth
Affiliated Hospital of Harbin Medical University (Harbin, China)
due to right upper abdominal pain with no symptoms of jaundice. The
patient had no disease history or treatment history related to the
liver prior to this hospitalization.
Diagnostic focus and assessment
Routine blood test results revealed the following:
White blood cell count, 6.1×109/l (reference range:
3.5–9.5×109/l); neutrophils, 69.9% (reference range:
40–75%); red blood cell count, 5.02×1012/l
(3.8–5.1×1012/l); hemoglobin, 155 g/l (reference range:
115–150 g/l); and hematocrit, 46.3% (reference range: 35–50%).
Liver function test results revealed the following: Total
bilirubin, 264.6 µmol/l (reference range: 3.1–22.5 µmol/l);
aspartate aminotransferase, 48 U/l (reference range: 13–35 U/l);
alanine aminotransferase, 120 U/l (reference range: 7–40 U/l); and
albumin, 38.6 g/l (reference range: 40–55 g/l). The patient's
carbohydrate antigen-199 level was 1,000 U/ml (reference range:
0–27 U/ml) and the α-fetoprotein level was 2,048 ng/ml (reference
range: 13–150 ng/ml). Computed tomography scan and magnetic
resonance cholangiopancreatography scan results indicated
gallbladder cancer accompanied by multiple liver metastases
including segments V, VIII and IV of the liver. Right posterior
lobe metastases were observed in the vicinity of the portal and
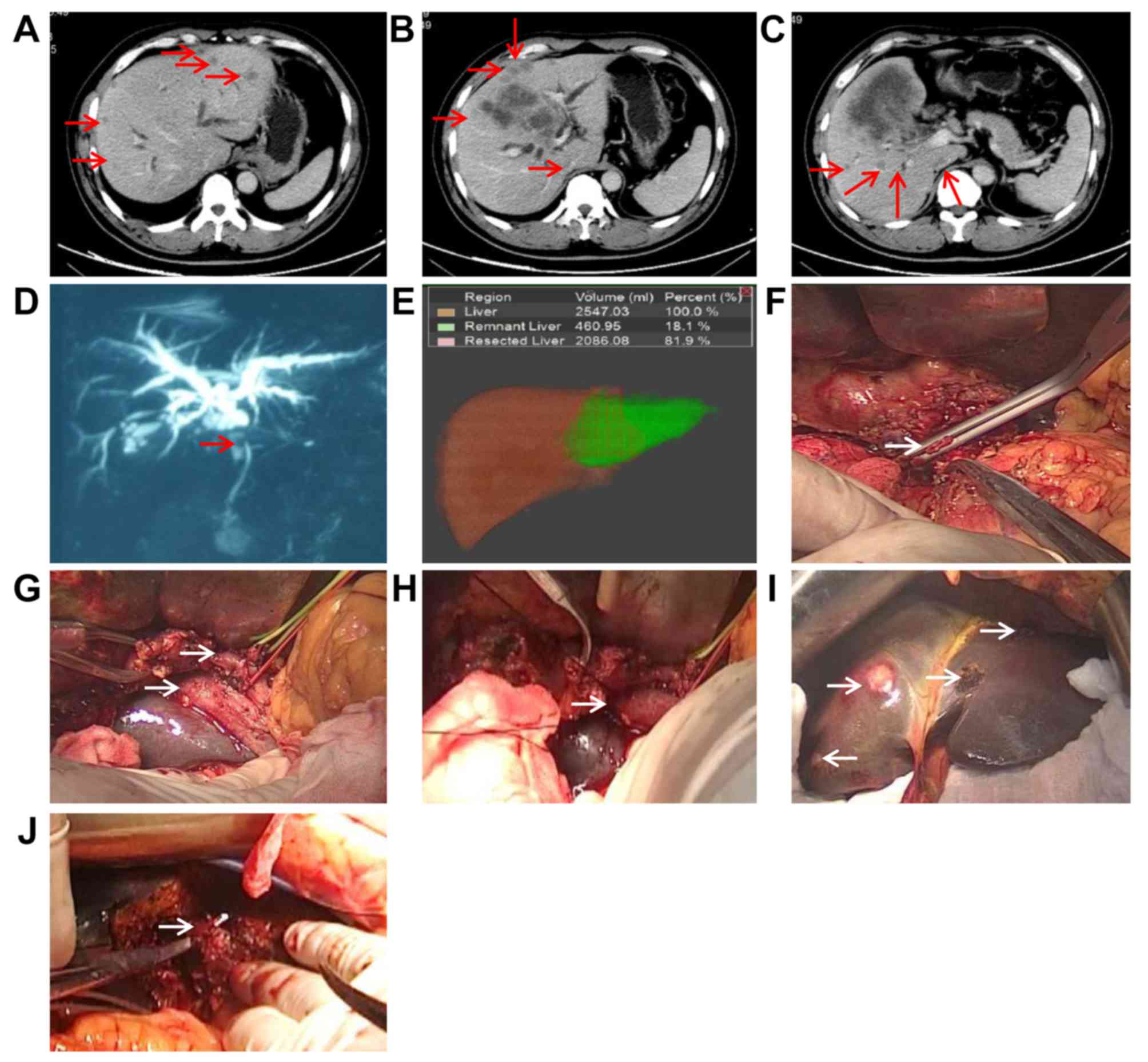
hepatic veins (Fig. 1A-D).
Therapeutic focus and assessment
Liver volume was calculated using liver resection
simulation in the 3D+Medical Imaging Visualization system (Yorktal
Digital Medical Imaging Technology, Co., Ltd., Shenzhen, China).
The total liver volume, residual liver volume (RLV), and tumor
volume were calculated. The RLV was calculated as the total liver
volume minus the tumor volume. The RLV was 460.95 ml (18.1% of the
total liver volume; Fig. 1E).
Subsequently, resection of the right trisegment was performed.
Prior to surgery, intense glucose therapy (50% glucose solution
containing 100 g of glucose daily for 2 days; CR Double-Crane
Pharmaceuticals Co., Ltd., Beijing, China) was administered to the
patient to increase the liver glycogen stores and vitamin K
(vitamin K1, 10 mg, and vitamin K3, 8 mg daily via intramuscular
injection for 3 days; Cisen Pharmaceutical Co., Ltd., Jining,
China) was administered to improve blood coagulation. Furthermore,
reduced glutathione (1,800 mg/day intravenously for 5 days;
YaoPharma Co., Ltd., Chongqing, China) and magnesium
isoglycyrrhizinate (200 mg intravenous daily for 5 days; Chia Tai
Tianqing Pharmaceutical Group Co., Ltd., Lianyungang, China) were
also administered to protect liver function.
The first surgery was performed in November 2014.
The common bile duct along the lateral part of duodenum was
disarticulated and the hepatoduodenal ligament was skeletonized.
Three metastatic nodules in segments II and III of the left outer
lobe of the liver were partially resected. A liver portion between
segment IV and segments II–III was disarticulated. Following this,
the portal vein and hepatic artery branches connected to segment IV
were ligated, the right portal vein was ligated, and the bile duct
at left hepatic duct confluence was disarticulated. Subsequently, a
Y-tube was inserted to drain the bile out of the body. Developer
agent (fat emulsions; B. Braun Melsungen AG, Melsungen, Germany)
was injected into the Y-tube to examine the bile leakage at the
liver cross-section (Fig. 1F-J). A
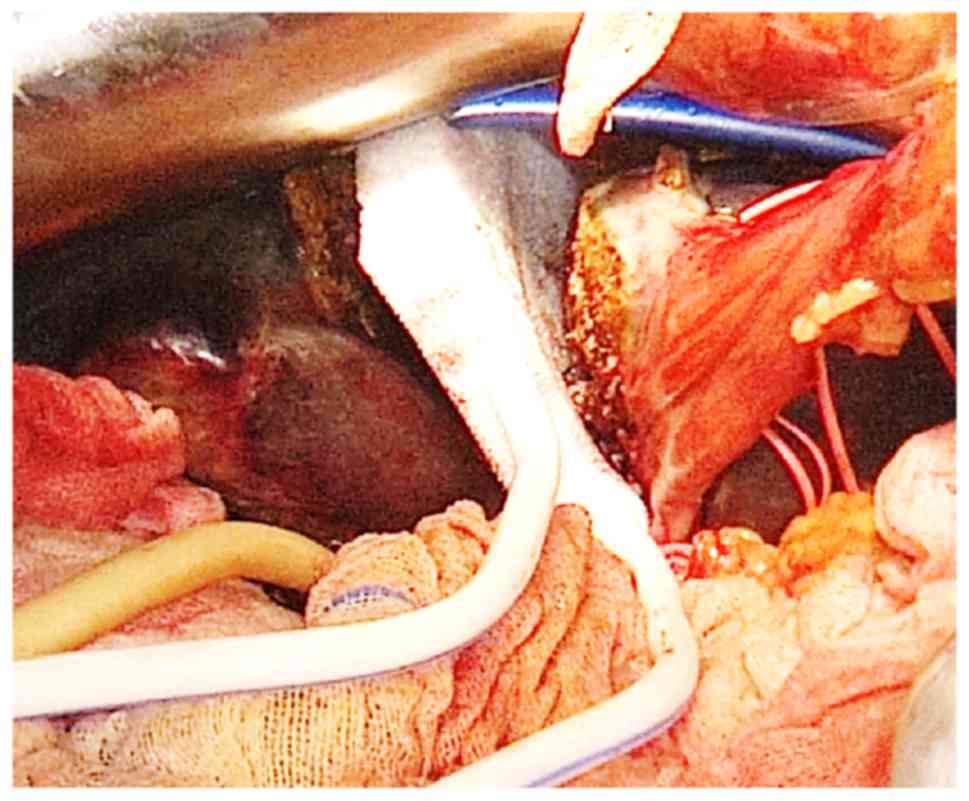
VSD dressing was placed on the resected surface of the liver, with
inferior and anterior margins 1 cm beyond the resection surface. It
had two drainage tubes 3 cm apart. When a secondary surgery was not
feasible, the VSD dressing could be removed through the 3-cm
incision between the two tubes (Fig.
2). Moreover, two normal drainage tubes were also placed at the
liver cross-section. One tube was placed at the hepatorenal recess
(the lowest point of the supine position) and the other was placed
behind the liver duodenum ligament to drain the residual effusion
at the cross section and small omentum, respectively. Post-surgery,
continuous negative pressure suction was applied via VSD at 50 kPa
and an intermittent saline flush (50 ml every hour) was performed
through a flush pipe. No negative pressure suction was performed
for the normal drainage tubes. The patient received prophylactic
antibiotic therapy in the form of Ulinastatin (200,000 U/day
intravenously for 5 days; Techpool Bio-Pharma Co., Ltd., Guangzhou,
China) and Omegaven (100 ml/day intravenously for 5 days
postoperative; Fresenius Kabi Asia-Pacific, Ltd., Wanchai, Hong
Kong) as anti-inflammatory medications, and proteins (albumin, 20
g/day intravenously for 3 days; Shanghai RAAS Blood Products Co.,
Ltd., Shanghai, China) as treatment to protect liver function. A
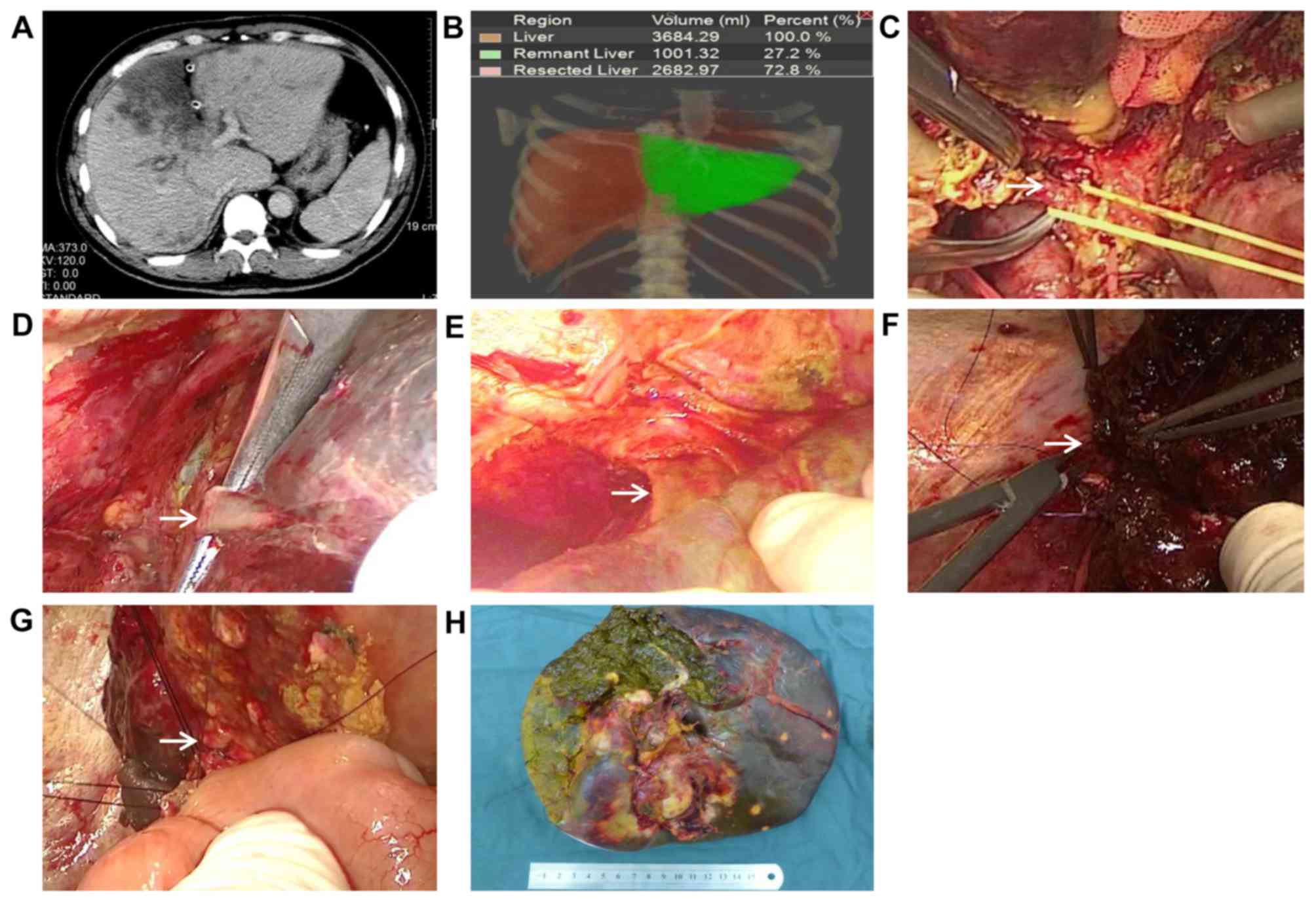
total of 7 days after the first surgery, remnant liver volume was
increased to 117% of the original volume, accounting for 39.3%
(Fig. 3A and B) of the standard
liver volume.
The second surgery was performed 8 days after the
first surgery and the abdomen was accessed along the original
incision. On investigation, the volume of the left outer lobe was
notably increased and the VSD duct was appropriately fixed on the
liver cross section (adhered to both sides of the liver cross
section). The adhesion was slight and easy to separate. No effusion
was observed surrounding the VSD duct and no bleeding occurred at
the liver cross section when VSD was removed. Furthermore, the
perihepatic ligament was liberated and the right hepatic artery and
right hepatic vein were ligated and excised. The hepatic vein was
disarticulated below the confluence point of the middle hepatic and
left hepatic veins and the broken ends were sutured. The left outer
lobe bile duct was disarticulated, the right liver trisegment was
resected and Roux-Y anastomosis was achieved on the left outer lobe
bile duct and jejunum. One drainage tube was retained at the lower
cross section (Fig. 3C-H).
Outcome
The patient exhibited improved wound healing after
the application of VSD compared with conventional ALPPS surgery.
There was positive improvement in wound adhesion and effusion
drainage. The VSD dressing reduced intraoperative abdominal
adhesion and effusion and protected the residual liver from tumor
invasion of the diseased liver. Previous studies support that the
conventional ALPSS method is disadvantageous when used with or
without a plastic bag (6,7). Indeed, it is difficult to completely
drain the fluid from the plastic bag. Both non-treatment and fibrin
glue application present the problem of incomplete drainage and the
tumors proximal to the resection surface may invade the residual
liver.
This patient was followed up until December 2016,
and no evidence of recurrence or metastasis was observed.
Discussion
With the improvements in technology and surgical
techniques, major hepatectomies may be performed with low morbidity
and mortality. In the present case report, a two-staged hepatectomy
(ALPPS) was performed in a patient with liver cancer and VSD was
implanted to improve surgical wound healing. Results indicated that
wound healing in the patient was improved after the application of
VSD compared with conventional ALPPS surgery.
Application of VSD in ALPPS surgeries
To the best of our knowledge, the application of VSD
to treat abdominal surgical wounds has not yet been reported. VSD
dressing has been rarely used for abdominal surgeries because it is
non-absorbable. Since it is also large and not smooth, it cannot be
pulled out as with a drainage tube; a secondary surgery is required
to remove a VSD dressing. In ALPPS surgery, the dressing may be
removed during the second surgery. Furthermore, the application of
a VSD dressing in this surgery alleviates abdominal inflammation,
reduces tissue adhesion and improves the difficulty of secondary
surgery. Notably, the placement of a VSD dressing between the
diseased and residual parts of the liver prevents tumor invasion.
The authors of the present study suggest that the two drainage
tubes of the VSD dressing are placed beneath the skin, 3 cm apart.
Therefore, when a secondary surgery is not feasible, it is possible
to incise the skin and remove the VSD dressing under local
anesthesia. It overcomes the disadvantage of the plastic bag, which
is difficult to remove. In the present case report these challenges
were overcome effectively. First, VSD was removed without
difficulty as the second surgery was performed ~1 week after ALPPS.
Therefore, as the interval between the two surgeries was short, the
obtained adhesion was relatively limited and VSD limited the extent
of the adhesions. In conclusion, the present case study indicated
that the use VSD combined with ALPPS surgery for a patient with
liver cancer resulted in improved recovery and wound healing.
Use of VSD in ALPPS surgery
In the present study, VSD was pre-implanted
appropriately and fixed on both sides of the liver cross section.
To enable complete suction, the front of the upper bound of VSD was
outplaced 1 cm above the liver cross section. Two VSD drainage
tubes were placed 3 cm apart in order to enable easy accessibility
during the second surgery and easy removal, if required.
Negative pressure applied at 50 kPa
Excessive negative pressure may increase the
bleeding risk and may result in the attraction of intestine and
omentum tissues, leading to wrapping and adhesions (10). Thus, a low negative pressure of 50
kPa was chosen in the present case. However, specific factors
should be considered when choosing an appropriate negative
pressure. Firstly, pressure should be high enough to resist the
resistance of VSD sponge material to ensure that the negative
pressure may suck the liquid surrounding VSD; continuous negative
pressure suction and syphonage effect of sponges allow for more
complete drainage (8–10). Secondly, if the pressure is too low,
the sponge becomes too wet, which affects the adhesion properties
of the sponge. Hence, choosing an optimal negative pressure is
important to improve the functionality of VSD.
Surgeons performed ALPPS along with VSD on another
patient who was diagnosed with Bismush type IV hilar
cholangiocarcinoma. In September 2015, a 59-year-old male patient
was hospitalized at the Department of General Surgery at The Fourth
Affiliated Hospital of Harbin Medical University (Harbin, China)
due to symptoms of jaundice. White blood cell count was
3.7×109/l; neutrophils, 63.1%; red blood cell count,
4.5×1012/l (3.8–5.1×1012/l); hemoglobin, 120
g/l; and hematocrit, 41.1%. Liver function test results revealed
the following: Total bilirubin, 383.6 µmol/l; aspartate
aminotransferase, 72 U/l; alanine aminotransferase, 100 U/l; and
albumin, 41.8 g/l The patient's carbohydrate antigen-199 level was
1,000 U/ml. A percutaneous transhepatic cholangial drainage tube
was placed preoperatively at the right hepatic lobe to drain the
bile. It was found that tumors had invaded the right hepatic duct
and adjacent tissues, which indicated the necessity of right
hemi-liver resection. However, as treatment for jaundice had not
been performed on the left hemi-liver, the risk of postoperative
liver function failure was relatively high. Thus, ALPPS was
performed on the right hemi-liver. As biliary-enteric anastomosis
was performed at the same time, conventional plastic bags, VSD
joint wound protection and suction approaches were adopted to
prevent bile leakage and adhesion.
The present case report has certain limitations. VSD
material must be improved in order to obtain satisfactory adhesion
to tissues and improve the suction of bile wastes. Certain factors,
including the selection of optimal negative pressure, VSD material
and interval time between staged hepatectomies require further
investigation. Moreover, large-scale randomized trials are required
to demonstrate the safety, efficacy and long-term outcomes of this
approach.
In conclusion, in cases where patients that require
conventional two-staged hepatectomies do not fulfill the criteria
to undergo resection due to insufficient hypertrophy or tumor
progression, ALPPS may be used as a salvage procedure, despite the
risk of increased morbidity and possible mortality. As a wound
protection and drainage technique, VSD may be employed in ALPPS
surgeries in order to decrease effusion and adhesion complications.
In the meantime, its application in alternative abdominal surgeries
remains to be established.
Acknowledgements
The present study was supported in part by the
National Natural Scientific Foundation of China (grant 81401975),
Natural Science Foundation of Heilongjiang Province (grant no.
D201250), China Postdoctoral Science Foundation (grant no.
2016M591564), Heilongjiang Postdoctoral Fund (grant no. LBH-Z14219
and LBH-Z16191), Scientific Research Project of Heilongjiang
Medical Science Institute (grant no. 201502 and 201710), and
Heilongjiang Province Health Bureau (grant no. 2014-399).
References
|
1
|
Ananthakrishnan A, Gogineni V and Saeian
K: Epidemiology of primary and secondary liver cancers. Semin
Intervent Radiol. 23:47–63. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yuen MF, Cheng CC, Lauder IJ, Lam SK, Ooi
CG and Lai CL: Early detection of hepatocellular carcinoma
increases the chance of treatment: Hong Kong experience.
Hepatology. 31:330–335. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bruix J and Sherman M: American
Association for the Study of Liver Diseases: Management of
hepatocellular carcinoma: An update. Hepatology. 53:1020–1022.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Della Sala S: A daguerreotype of Phineas
Gage? Cortex. 47:4152011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Schnitzbauer AA, Lang SA, Goessmann H,
Nadalin S, Baumgart J, Farkas SA, Fichtner-Feigl S, Lorf T,
Goralcyk A, Hörbelt R, et al: Right portal vein ligation combined
with in situ splitting induces rapid left lateral liver lobe
hypertrophy enabling 2-staged extended right hepatic resection in
small-for-size settings. Ann Surg. 255:405–414. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Torres OJ, Ede S Fernandes, Oliveira CV,
Lima CX, Waechter FL, Moraes-Junior JM, Linhares MM, Pinto RD,
Herman P and Machado MA: Associating liver partition and portal
vein ligation for staged hepatectomy (ALPPS): The Brazilian
experience. Arq Bras Cir Dig. 26:40–43. 2013.(In English,
Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang GQ, Zhang ZW, Lau WY and Chen XP:
Associating liver partition and portal vein ligation for staged
hepatectomy (ALPPS): A new strategy to increase resectability in
liver surgery. Int J Surg. 12:437–441. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Banasiewicz T, Borejsza-Wysocki M,
Meissner W, Malinger S, Szmeja J, Kościński T, Ratajczak A and
Drews M: Vacuum-assisted closure therapy in patients with large
postoperative wounds complicated by multiple fistulas. Wideochir
Inne Tech Maloinwazyjne. 6:155–163. 2011.PubMed/NCBI
|
|
9
|
Hu N, Wu XH, Liu R, Yang SH, Huang W,
Jiang DM, Wu Q, Xia T, Shao ZW and Ye ZW: Novel application of
vacuum sealing drainage with continuous irrigation of potassium
permanganate for managing infective wounds of gas gangrene. J
Huazhong Univ Sci Technolog Med Sci. 35:563–568. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ren H and Li Y: Severe complications after
negative pressure wound therapy in burned wounds: Two case reports.
Ther Clin Risk Manag. 10:513–516. 2014. View Article : Google Scholar : PubMed/NCBI
|