Introduction
Critically ill patients are prone to developing
intra-abdominal hypertension (IAH) and abdominal compartment
syndrome (ACS). IAH has been reported in 35% of intensive care unit
(ICU) patients, 5% of which also manifest ACS (1), which is an important factor leading to
an increased mortality rate in ICU patients. In critically ill
patients, contributing factors often overlap, leading to elevated
intra-abdominal pressure (IAP), and resulting in multiple organ
failure (2–4).
The severity and duration of IAH is associated with
the incidence and mortality of multiple organ dysfunction syndrome
(MODS) (5). Previous results have
indicated that global hemodynamics, oxygenation and organ function
are notably affected by sustained IAH of 12 h combined with severe
acute pancreatitis (SAP) (6). Animal
models of SAP treated with 25 mmHg IAH/ACS undergoing delayed
decompression had a higher grade of lung and intestinal injury
(7). Increased oxygenation index and
urinary output were the most pronounced effects of decompressive
laparotomy, with a mortality rate of 49.2% (8). Surgical abdominal incision
decompression resulted in a rapid decline in intra-abdominal
pressure by 50%, without improving the Sepsis-Related Organ Failure
Assessment (SOFA) score (9).
Patients with bowel dysfunction, which leads to
IAH/ACS, are typically treated using conservative therapy to reduce
intra-abdominal pressure. Currently, glycerin enema is commonly
used for catharsis. The content of 1,2,3-propanetriol is 42.7 g per
100 g of glycerin enema, which is not absorbed after entering the
rectum and acts as a laxative.
IAH/ACS is characterized by declining
gastrointestinal peristalsis as well as intestinal mucosal edema
and damage to the intestinal mucosal barrier, resulting in acute
lung injury/acute respiratory distress syndrome (ALI/ARDS), acute
renal failure and serious systemic inflammatory response syndrome
(SIRS) (10,11). Therefore, catharsis alone may not be
adequate therapy for IAH/ACS. Rhubarb is associated with multiple
therapeutic effects and is often used to relieve constipation
(12). A recent study also indicated
that rhubarb also promotes intestinal epithelial proliferation and
improves intestinal function in sepsis (13). It has been reported to inhibit the
expression of inflammatory markers and exert a protective effect
against organ damage in sepsis (14).
Based on these previous results, the current study
aimed to investigate the pharmacological effects of raw rhubarb in
reducing IAP and improving the function of the intestinal tract and
other organs. To this end, a randomized and controlled clinical
trial was conducted to compare rhubarb and glycerin enemas in
IAH/ACS patients. The protective role of rhubarb in IAH/ACS were
evaluated in order to assess its potential as a therapeutic
alternative.
Patients and methods
Patients and groups
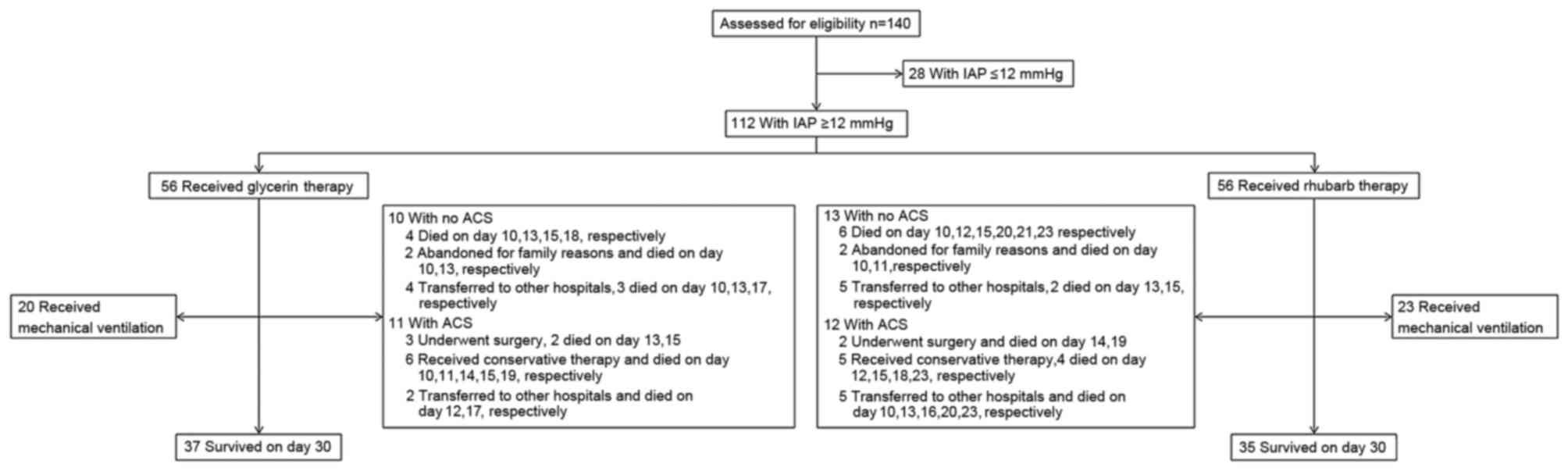
The current study was conducted in the Departments
of General Surgery, ICU and Emergency of the Affiliated Hospital of
Jiangsu University. Critically ill patients with IAH and acute
gastrointestinal injury (AGI) stage I–III, aged 18–80 years, were
consecutively recruited into this study. AGI was defined by the
criteria of the European Society of Intensive Care Medicine Working
Group (15). IAH was defined as a
consistently increased IAP value of ≥12 mmHg. ACS was defined as
IAP >20 mmHg. Single organ dysfunction or MODS/ACS was diagnosed
using the criteria of the World Society of ACS (16). Patients with mechanical intestinal
obstruction or AGI at stage IV were excluded. Patients with a high
probability of receiving abdominal surgery were also excluded. From
October 2011 to July 2015, 140 patients were assessed for
eligibility, and 112 patients were selected for inclusion in the
trial. According to the order of admission, patients were randomly
assigned to the glycerin enema group or the rhubarb group (Fig. 1). Patients' clinical demographics at
admission are summarized in Table
I.
 | Table I.Patient clinical demographics. |
Table I.
Patient clinical demographics.
| Parameter | Glycerin group | Rhubarb group | P-value |
|---|
| Number of cases
(n) | 56 | 56 |
|
| Sex
(male/female) | 46/10 | 43/13 | 0.483 |
| Age (years) | 43±16 | 45±15 | 0.673 |
| Class of
intra-abdominal hypertension at admission, n (%) |
|
|
|
| I | 28 (50%) | 27 (48.2%) | 0.850 |
| II | 18 (32.1%) | 21 (37.5%) | 0.552 |
| III | 10 (17.9%) | 8 (14.3%) | 0.607 |
| Abdominal compartment
syndrome at day 30, n (%) | 10 (17.9%) | 13 (23.2%) | 0.483 |
| Diagnosis, n (%) |
|
|
|
| Severe
acute pancreatitis | 36 (64.3%) | 30 (53.6%) | 0.249 |
| Septic
shock | 10 (17.9%) | 13 (23.2%) | 0.483 |
|
Post-cardiopulmonary
resuscitation | 5 (8.9%) | 10 (17.9%) | 0.165 |
| Bowel
obstruction | 5 (8.9%) | 3 (5.4%) | 0.463 |
| Co-morbidities, n
(%) |
|
|
|
|
Hypertension | 11 (19.6%) | 6 (10.7%) | 0.188 |
|
Diabetes | 7 (12.5%) | 9 (16.1%) | 0.589 |
|
Hyperthyroidism | 2 (3.6%) | 0 (0.0%) | 0.154 |
|
Schistosomal cirrhosis | 1 (1.8%) | 2 (3.6%) | 0.558 |
| Chronic
obstructive pulmonary disease | 3 (5.4%) | 5 (8.9%) | 0.463 |
| No
co-morbidities | 32 (57.1%) | 34 (60.7%) | 0.701 |
| Liver function |
|
|
|
| Alanine
aminotransferase (U/l) | 89.60±25.81 | 95.18±27.23 | 0.268 |
|
Aspartate aminotransferase
(U/l) | 88.75±20.56 | 96.20±26.64 | 0.101 |
| Kidney
function |
|
|
|
| Blood
urea nitrogen (mmol/l) | 19.52±7.70 | 18.85±9.84 | 0.691 |
|
Creatinine (µmol/l) | 151.39±45.93 | 139.96±27.44 | 0.113 |
| White blood cells
(×109/l) | 17.06±8.51 | 16.35±7.37 | 0.636 |
| Body mass index
(kg/m2) | 23.73±4.38 | 25.09±3.77 | 0.080 |
Treatment
All patients with IAH/ACS underwent necessary
treatment (17). Patients with
respiratory failure received mechanical ventilation (MV) until
recovery. The initial parameters of MV included a tidal volume of
6–8 ml/kg, platform pressure of 30–35 cm H2O and a
positive end-expiratory pressure (PEEP) of 8–16 cm H2O. The
parameters were adjusted according to arterial blood gas (ABG)
analysis.
Patients in the glycerin group received 110 ml
glycerin enema (Winguide Huangpu Pharmaceutical, Shanghai, China)
via coloclysis once daily for 7–9 days. Patients were maintained in
the supine position to retain glycerin in the intestine for more
than 10 min.
Patients in the rhubarb group received 0.3 g/kg body
weight rhubarb powder (Gansu Yalan Pharmaceutical Co., Ltd., Gansu,
China) soaked in 100 ml warm water (80–100°C, for 30 min and cooled
down to 37°C) via coloclysis once daily for 7–9 days. Enteral
nutrition (EN) was administrated to patients via the nasogastric
tube or oral route. EN suspension was initiated with Peptison (1
kcal/ml; Nutricia Pharmaceutical Wuxi Co., Ltd) and switched to
Nutrition Fibre (1.5 kcal/ml) with feeding speed from 30 ml/h to
100 ml/h by using a nutrition pump.
Testing
Acute Physiology and Chronic Health Evaluation II
(APACHE II) (18) and SOFA scores
(19) were conducted twice on days
1–5, 7 and 9 post-admission, and the scores indicating greatest
severity on each day were recorded.
Peripheral venous blood samples were collected on
days 1–5, 7 and 9 post-admission to measure the concentrations of
serum interleukin (IL)-6, tumor necrosis factor-α (TNF-α),
procalcitonin (PCT) and C-reactive protein (CRP) using ELISA kits
(ab178013, ab181421, ab100630 and ab99995; Abcam, Cambridge, MA,
USA).
Arterial blood samples were tested at least twice
per day in patients that received MV and the most severe results of
ABG were used to calculate the oxygenation index
(PaO2/FiO2). PEEP, alveolar-arterial partial
pressure of oxygen (P(A-a)O2) and peak
inspiratory pressure (PIP), duration of MV, duration of ICU
hospital stay, first day of EN and 30-day mortality were
recorded.
The bladder inner pressure measured in a recumbent
position was used to assess the level of IAP. A Foley catheter (18
Fr) was inserted into the bladder, to drain urine, followed by
injection of 25 ml saline. The catheter was connected to a pressure
transducer. The operator selected the zero level of axillary
midline for measurement at the end of the breath. The measurement
was performed three times in total and the mean of the data was
recorded (16,17).
Statistical analysis
The primary endpoints of this study were the
duration of MV, ICU hospital stay, first day of EN and 30-day
mortality. The secondary endpoints were the level of IAP, systemic
inflammation and disease severity. Data were expressed as the mean
± standard deviation. Differences between groups were analyzed
using the chi-squared test, a rank sum test and repeated analysis
of variance, on SPSS 20.0 software (IBM SPSS, Armonk, NY, USA).
P<0.05 was considered to indicate statistical difference.
Results
Effect of rhubarb and glycerin
therapies on IAP
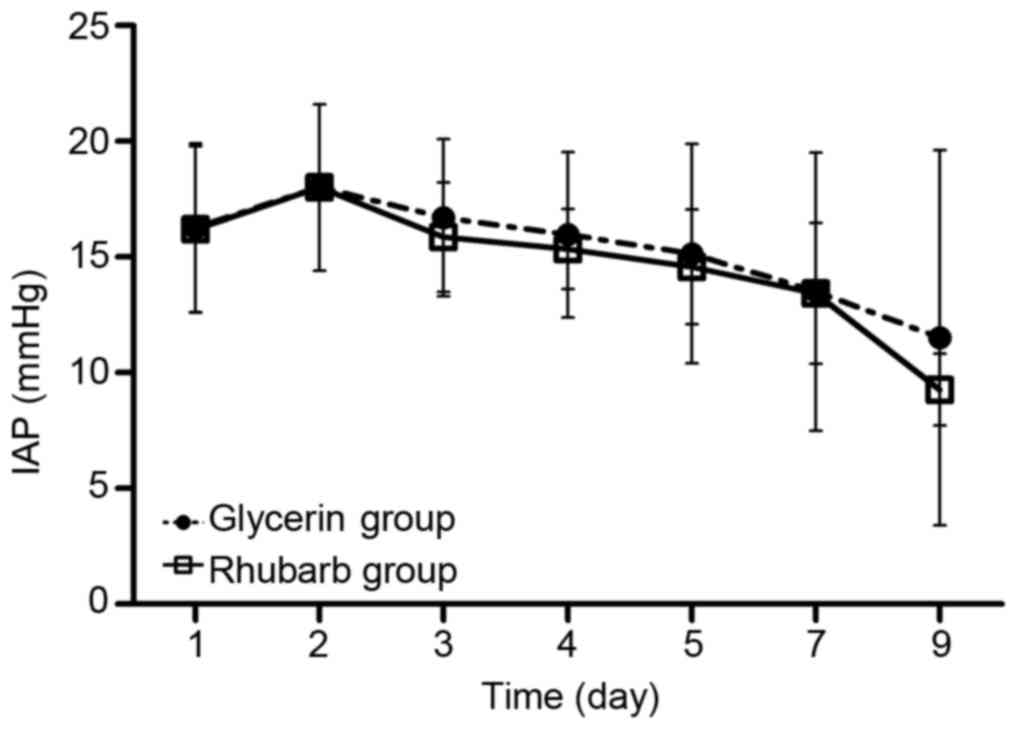
After intervention with rhubarb or glycerin enema,
the IAP of patients in both groups began to decrease from day 3
(Fig. 2). No significant differences
were observed between the two groups at any time point.
Effect of rhubarb and glycerin
therapies on severity scores
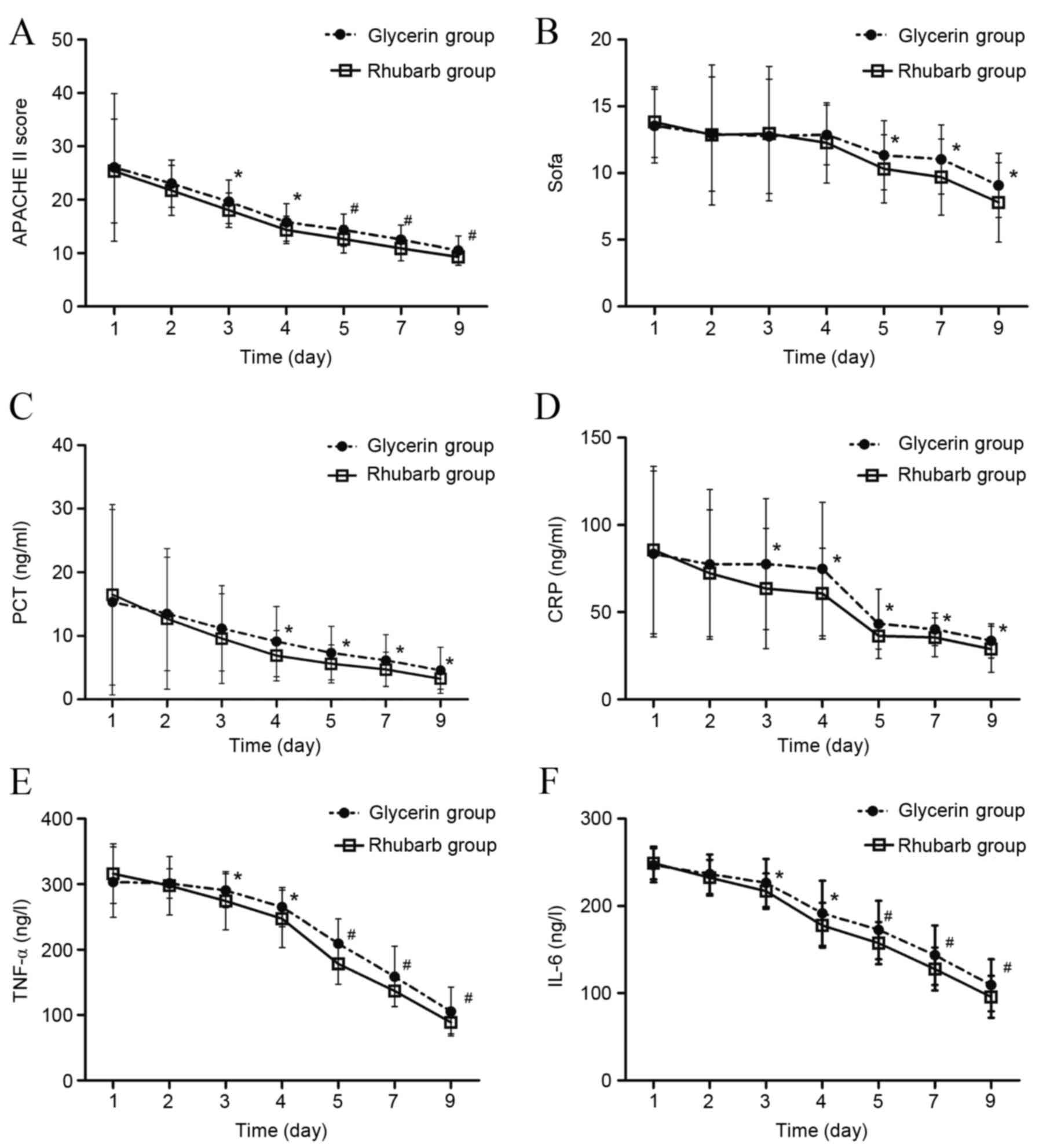
The APACHE II scores in both groups showed a
declining trend (Fig. 3A). The
APACHE II scores in the rhubarb group were significantly lower
compared with the glycerin group from day 3 to day 9 (day 3–4,
P<0.05; day 5–9, P<0.01). The SOFA scores showed no
significant difference between the two groups from day 1 to day 4
however, from day 5 to 9, the SOFA scores of the rhubarb group were
significantly lower compared with the glycerin group (P<0.05;
Fig. 3B).
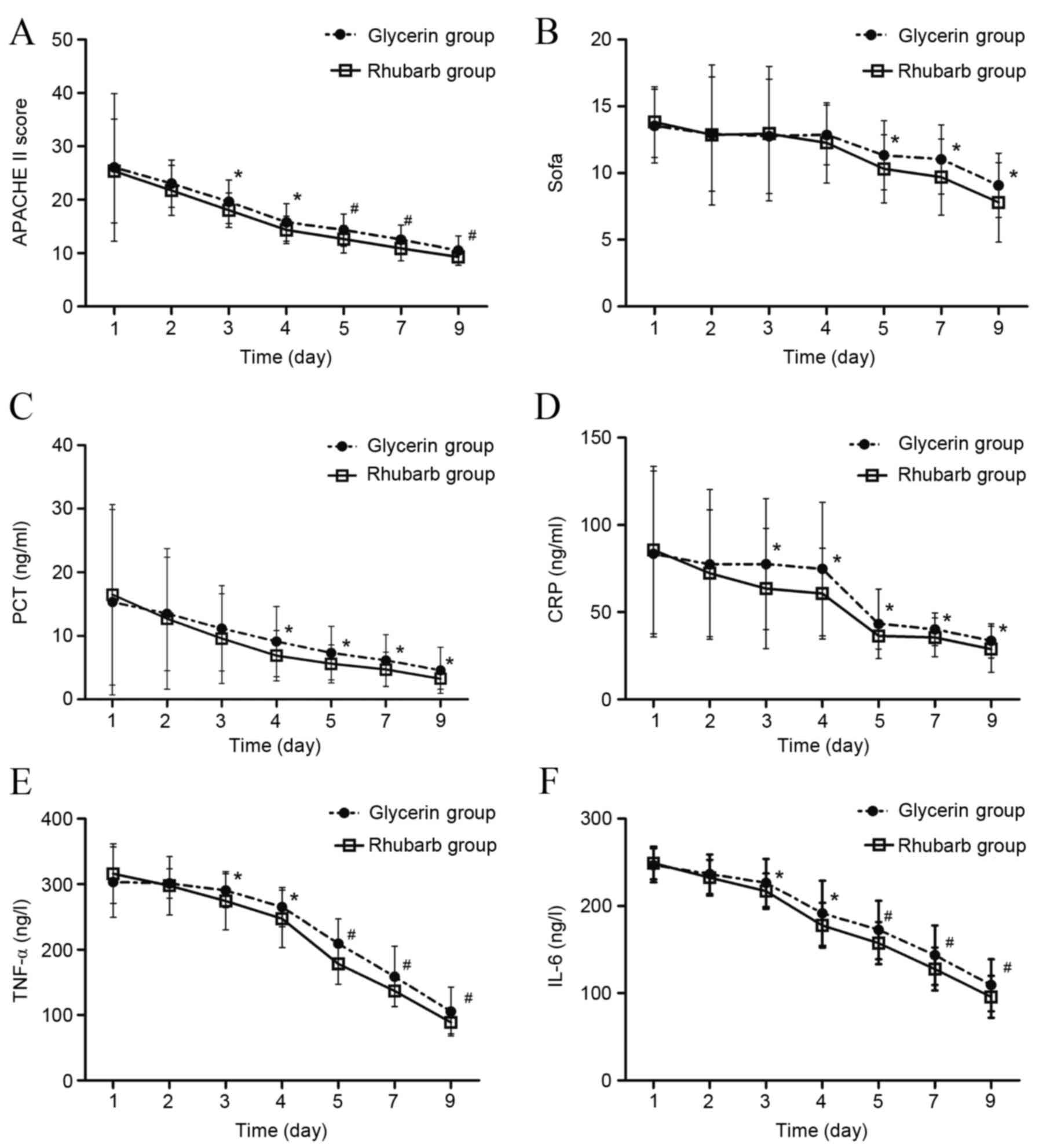 | Figure 3.Effect of rhubarb or glycerin enema on
severity scores and inflammatory marker levels. (A) APACHE II
score, (B) SOFA score, (C) PCT level, (D) CRP level, (E) TNF-α
level and (F) IL-6 level after rhubarb or glycerin enema.
*P<0.05 and #P<0.01 vs. glycerin group. APACHE II,
Acute Physiology and Chronic Health Evaluation II; SOFA,
Sepsis-Related Organ Failure Assessment; PCT, procalcitonin; CRP,
C-reactive protein, TNF-α, tumor necrosis factor-α; IL-6,
interleukin-6. |
Effect of rhubarb and glycerin
therapies on the levels of inflammatory markers
PCT, CRP, TNF-α and IL-6 levels in both groups
showed a declining trend (Fig.
3C-F). From day 4 to 9, the PCT levels of the rhubarb group
were significantly lower compared with the glycerin group
(P<0.05; Fig. 3C). From day 3 to
9, the CRP levels of the rhubarb group were significantly lower
compared with the glycerin group (P<0.05; Fig. 3D). Similarly, from day 3 to 9, the
TNF-α and IL-6 levels of the rhubarb group were significantly lower
compared with the glycerin group (day 3–4, P<0.05; day 5–9,
P<0.01; Fig. 3E and F).
Effect of rhubarb and glycerin
therapies on the duration of MV, first day of EN and ICU hospital
stay
A total of 20 patients in the glycerin group and 23
patients in the rhubarb group received MV (20/56 vs. 23/56,
χ2=0.340, P=0.698). The duration of MV and the ICU hospital stay in
the rhubarb group were significantly lower compared with the
glycerin group (both P<0.05; Table
II). The first day of EN administration was significantly
earlier in the rhubarb group compared with the glycerin group
(P<0.05).
 | Table II.Timing of patient treatment. |
Table II.
Timing of patient treatment.
| Parameter | Glycerin group | Rhubarb group | P-value |
|---|
| Duration of
mechanical ventilation (days) | 8.20±3.93 |
4.13±2.36a | 0.034 |
| First day of
enteral nutrition (day) | 7.64±2.94 |
5.91±1.99a | 0.017 |
| Intensive care unit
hospital stay (days) | 16.02±4.93 |
14.29±3.53a | 0.039 |
Effect of rhubarb and glycerin
therapies on respiratory parameters in patients with MV
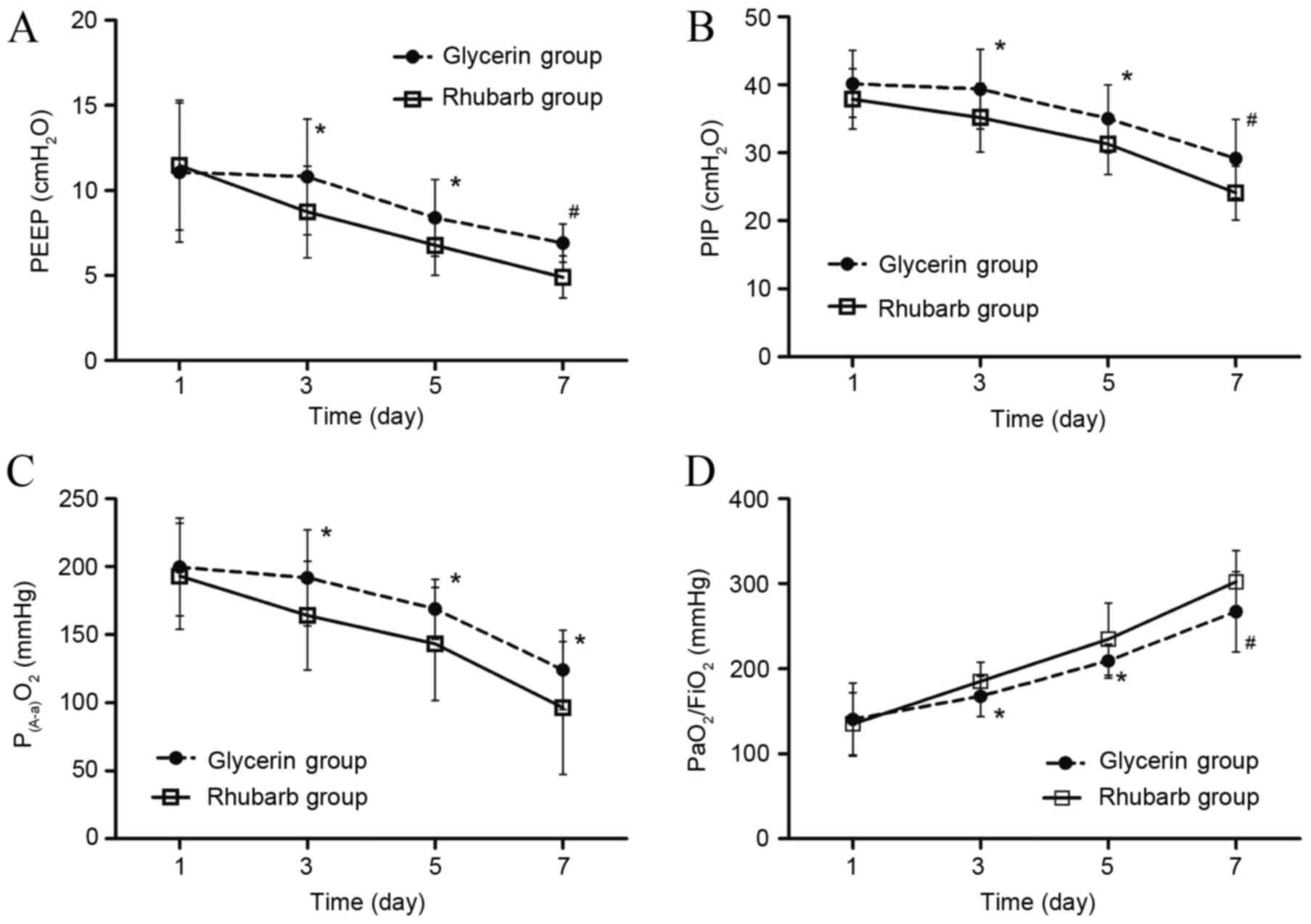
From day 3 to day 7, the level of PEEP and PIP in
the two groups declined. The levels of PEEP and PIP in the rhubarb
group were significantly lower compared with the glycerin group
(P<0.05 on day 3 and 5; P<0.01 on day 7; Fig. 4A and B). The level of P(A-a)O2
declined from day 1 to 7, and was significantly lower in the
rhubarb group compared with the glycerin group from day 3 to 7
(P<0.05; Fig. 4C). The
oxygenation index increased from day 1 to 7, and was significantly
higher in the rhubarb group compared with the glycerin group from
day 3 to 7 (P<0.05 on day 3 and 5; P<0.01 on day 7; Fig. 4D).
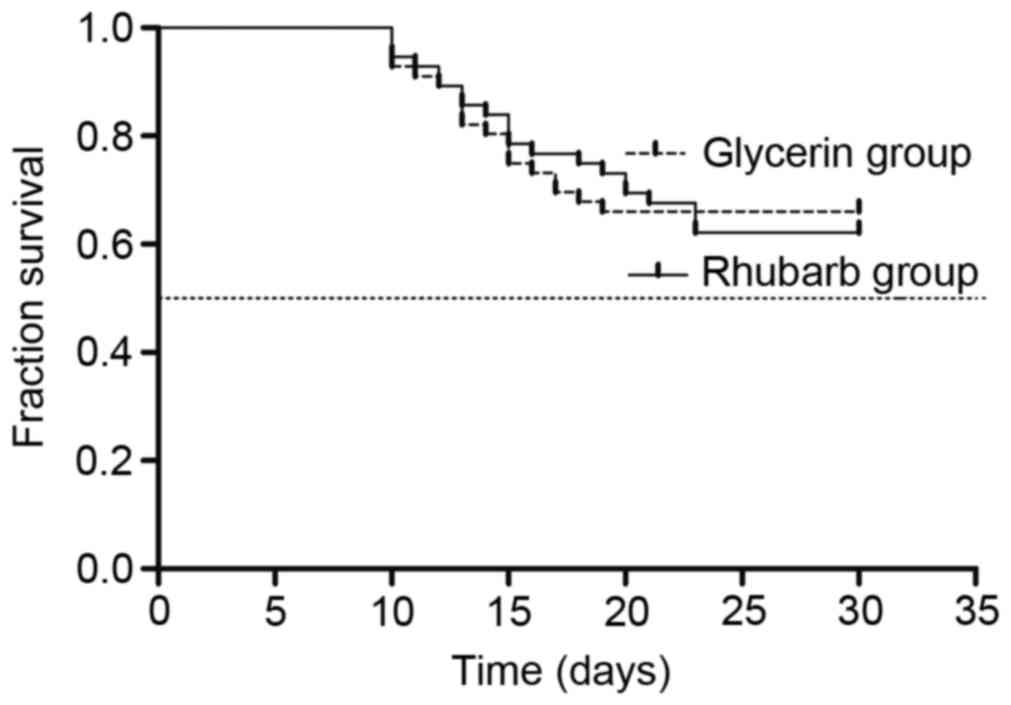
30-day mortality
No significant difference in 30-day mortality was
indicated between the groups (33.9 vs. 37.5%, χ2=0.156, P=0.693;
Fig. 5).
Adverse events
In the rhubarb group, there were 23 patients with
abdominal pain (41.1%), 10 patients with nausea (17.9%) and five
patients with vomiting (8.9%). One patient suffered bleeding from
hemorrhoids, which stopped after cessation of enema. In the
glycerin group, there were 30 patients with abdominal pain (53.6%),
13 patients with nausea (23.2%) and 3 patients with vomiting
(5.4%). No specific treatment was administered to eliminate these
adverse symptoms. No significant difference in adverse event rate
was observed between the two groups (χ2=0.104, P=0.588).
Discussion
IAH developed with MODS may lead to ACS in
critically ill patients (20). In
addition to the abdominal cavity, multiple organs are affected
directly and indirectly, resulting in decreased cardiac output,
pulmonary edema, atelectasis, increased intracranial pressure,
deterioration of consciousness, reduced renal blood flow and even
kidney failure (17,21).
APACHE II, CRP and IAP levels are good predictors of
disease severity in critical acute pancreatitis (22). Previous results indicated that APACHE
II and SOFA scores were positively associated with the severity of
IAP (20). The current study
demonstrated that rhubarb inhibited inflammatory factors, improved
APACHE II and SOFA scores, increased the intestinal tolerance to EN
(allowing earlier administration) and decreased the duration of
hospital stay in ICU. Rhubarb and its active ingredients not only
reduce IAP, but also inhibit inflammatory factors and protect organ
function, particularly gastrointestinal function. (12,23).
ALI is considered to be a risk factor for IAH
(9). IAH has also been reported to
dramatically increase the incidence of ALI/ARDS (24). In previous studies, rhubarb and
dexamethasone significantly reduced the edema of lung tissue,
decreased the red blood cell exudation, neutrophil infiltration and
plasma protein exudation in the alveoli, and inhibited nitric oxide
(NO) and the activities of inducible NO synthase in acute lung
injury (21,25). Rhubarb has also been reported to
protect lung fibroblast cells against oxidative damage by enhancing
cellular antioxidant activity and modulating cellular signal
transduction pathways (26) These
studies could potentially explain the improvement of oxygenation
index and P(A-a)O2 in the rhubarb group of
the current study.
In conclusion, rhubarb enema had a protective effect
against IAH and may be more effective compared with glycerin enema.
However, the current study was limited by a relatively small sample
size and a trial design that was not fully rigorous due to
restrictions involving clinical research and ethics. The dose of
rhubarb could not be further increased due to ethical restrictions.
These factors may have led to bias in this research results. To
address these issues, the current authors intend to develop an
optimized design and conduct a multicenter observational study.
Further clinical and basic studies are required to confirm these
findings and elucidate the mechanism of action of rhubarb.
Acknowledgements
This study was supported by grants from the National
Natural Science Foundation of China (grants nos. 81370172 and
81570078), the Jiangsu Province TCM Project (grant no. YB2015184)
and Jiangsu Provincial Key Research and Development Program (grant
no. BE2016721).
References
|
1
|
Sugrue M: Abdominal compartment syndrome.
Curr Opin Crit Care. 11:333–338. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schachtrupp A, Lawong G, Afify M, Graf J,
Toens C and Schumpelick V: Fluid resuscitation preserves cardiac
output but cannot prevent organ damage in a porcine model during 24
h of intraabdominal hypertension. Shock. 24:153–158. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Balogh ZJ, Lumsdaine W, Moore EE and Moore
FA: Postinjury abdominal compartment syndrome: From recognition to
prevention. Lancet. 384:1466–1475. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ganeshanantham G, Walsh SR and Varty K:
Abdominal compartment syndrome in vascular surgery-A review. Int J
Surg. 8:181–185. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Malbrain ML, Chiumello D, Pelosi P, Wilmer
A, Brienza N, Malcangi V, Bihari D, Innes R, Cohen J, Singer P, et
al: Prevalence of intra-abdominal hypertension in critically ill
patients: A multicentre epidemiological study. Intensive Care Med.
30:822–829. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ke L, Tong ZH, Ni HB, Ding WW, Sun JK, Li
WQ, Li N and Li JS: The effect of intra-abdominal hypertension
incorporating severe acute pancreatitis in a porcine model. PLoS
One. 7:e331252012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ke L, Ni HB, Tong ZH, Li WQ, Li N and Li
JS: The importance of timing of decompression in severe acute
pancreatitis combined with abdominal compartment syndrome. J Trauma
Acute Care Surg. 74:1060–1066. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
de Waele JJ, Hoste EA and Malbrain ML:
Decompressive laparotomy for abdominal compartment syndrome-a
critical analysis. Crit Care. 10:R512006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Malbrain ML, Chiumello D, Pelosi P, Bihari
D, Innes R, Ranieri VM, Del Turco M, Wilmer A, Brienza N, Malcangi
V, et al: Incidence and prognosis of intraabdominal hypertension in
a mixed population of critically ill patients: A multiple-center
epidemiological study. Crit Care Med. 33:315–322. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kirkpatrick AW, Roberts DJ, De Waele J,
Jaeschke R, Malbrain ML, De Keulenaer B, Duchesne J, Bjorck M,
Leppaniemi A, Ejike JC, et al: Intra-abdominal hypertension and the
abdominal compartment syndrome: Updated consensus definitions and
clinical practice guidelines from the World Society of the
Abdominal Compartment Syndrome. Intensive Care Med. 39:1190–1206.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mohmand H and Goldfarb S: Renal
dysfunction associated with intra-abdominal hypertension and the
abdominal compartment syndrome. J Am Soc Nephrol. 22:615–621. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wan B, Fu H, Yin J and Xu F: Efficacy of
rhubarb combined with early enteral nutrition for the treatment of
severe acute pancreatitis: A randomized controlled trial. Scand J
Gastroenterol. 49:1375–1384. 2014.PubMed/NCBI
|
|
13
|
Cui YL, Wang L, Tian ZT, Lin ZF and Chen
DC: Effect of rhubarb pre-treatment on intestinal microcirculation
in septic rats. Am J Chin Med. 42:1215–1227. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen DC and Wang L: Mechanisms of
therapeutic effects of rhubarb on gut origin sepsis. Chin J
Traumatol. 12:365–369. 2009.PubMed/NCBI
|
|
15
|
Blaser A Reintam, Malbrain ML, Starkopf J,
Fruhwald S, Jakob SM, De Waele J, Braun JP, Poeze M and Spies C:
Gastrointestinal function in intensive care patients: Terminology,
definitions and management. Recommendations of the ESICM Working
Group on Abdominal Problems. Intensive Care Med. 38:384–394. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Malbrain ML, Cheatham ML, Kirkpatrick A,
Sugrue M, Parr M, De Waele J, Balogh Z, Leppäniemi A, Olvera C,
Ivatury R, et al: Results from the International Conference of
Experts on Intra-abdominal Hypertension and Abdominal Compartment
Syndrome. I. Definitions. Intensive Care Med. 32:1722–1732. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cheatham ML, Malbrain ML, Kirkpatrick A,
Sugrue M, Parr M, De Waele J, Balogh Z, Leppäniemi A, Olvera C,
Ivatury R, et al: Results from the International Conference of
Experts on Intra-abdominal Hypertension and Abdominal Compartment
Syndrome. II. Recommendations. Intensive Care Med. 33:951–962.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Knaus WA, Draper EA, Wagner DP and
Zimmerman JE: APACHE II: A severity of disease classification
system. Crit Care Med. 13:818–829. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Vincent JL, De Mendonça A, Cantraine F,
Moreno R, Takala J, Suter PM, Sprung CL, Colardyn F and Blecher S:
Use of the SOFA score to assess the incidence of organ
dysfunction/failure in intensive care units: Results of a
multicenter, prospective study. Working group on ‘sepsis-related
problems’ of the European Society of Intensive Care Medicine. Crit
Care Med. 26:1793–1800. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
de Waele JJ, De Laet I, Kirkpatrick AW and
Hoste E: Intra-abdominal Hypertension and Abdominal Compartment
Syndrome. Am J Kidney Dis. 57:159–169. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Malbrain ML and Cheatham ML: Definitions
and pathophysiological implications of intra-abdominal hypertension
and abdominal compartment syndrome. Am Surg. 77 Suppl 1:S6–S11.
2011.PubMed/NCBI
|
|
22
|
Ke L, Tong ZH, Li WQ, Wu C, Li N, Windsor
JA, Li JS and Petrov MS: Predictors of critical acute pancreatitis:
A prospective cohort study. Medicine (Baltimore). 93:e1082014.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Li H, Yang T, Zhou H, Du J, Zhu B and Sun
Z: Emodin Combined with Nanosilver Inhibited Sepsis by
Anti-inflammatory Protection. Front Pharmacol. 7:5362017.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li C, Gui P, He X and Yang H: Actions of
NO and INOS on endotoxin induced rat acute lung injury and effect
of rhubarb on them. J Tradit Chin Med. 20:216–222. 2000.PubMed/NCBI
|
|
25
|
Li C, Zhou J, Gui P and He X: Protective
effect of rhubarb on endotoxin-induced acute lung injury. J Tradit
Chin Med. 21:54–58. 2001.PubMed/NCBI
|
|
26
|
Zhang R, Kang KA, Piao MJ, Lee KH, Jang
HS, Park MJ, Kim BJ, Kim JS, Kim YS, Ryu SY, et al: Rhapontigenin
from Rheum undulatum protects against oxidative-stress-induced cell
damage through antioxidant activity. J Toxicol Environ Health A.
70:1155–1166. 2007. View Article : Google Scholar : PubMed/NCBI
|