Introduction
Teeth are crucial to the survival of most mammals
(1,2). The basic tooth structure consists of a
brittle and stiff enamel shell, encasing a tough and compliant
dentin interior (3,4). Despite their durability, tooth
fractures are daily encountered by dentists (5). As known, tooth cracks have become the
third largest cause of tooth loss after dental caries and
periodontal disease (6). Tooth
cracks could lead to all kinds of symptoms, and patients always
fail to receive treatment timely when the tooth has no obvious
symptom. Most patients with cracks often see a dentist after
suffering pulpitis and periapical periodontitis, or even severe
fracture (7). A variety of different
clinical symptoms of tooth cracks depend on the depth of crack,
with the increase of crack depth, clinical symptoms may be obvious
and aggravating (8). The
symptomatology described by the patients included localized pain
during chewing or biting, inexplicable sensitivity to cold, as well
as pain on release of pressure (9–12).
Additionally, there are no measures to interfere with crack
development.
Tooth cracks have a multi-factorial etiology, in
which several dominant categories are classified, i.e. tooth
anatomical morphology, biomechanical factors, iatrogenic causes and
miscellaneous factors (9,13). It is also well established that the
high and steep cusp inclinations of tooth plays a vital role in
tooth cracks (9). Related studies
indicate that the horizontal component of occlusal force at the
bottom of the fovea changes along with the cusp inclinations. The
value of horizontal component will increase with the increase of
cusp inclinations (14). Steep cusp
inclines and deep grooves have been of concern as one of the
predisposing factors for the incidence of tooth fracture in
posterior natural dentition (15).
Therefore, the cusp inclinations has a significant influence on
tooth fractures. This indicates an effective reduction of cuspal
inclination to the compromised teeth for dentists (16).
There are many methods for the treatment of cracked
teeth, according to the sites and extent of the fracture (17,18),
i.e. immediate, direct restorations placed intracoronally without
cuspal coverage, direct restorations, which provide cuspal
coverage, indirect restorations placed intracoronally without any
cuspal support and indirect restorations which provide cuspal
coverage (onlays and full coverage restorations). While there is no
universally accepted restorative treatments, it is generally agreed
to keep fixed part of the tooth for moving on loading. The latter
may be achieved in a limited number of cases simply by the removal
of the affected cusp and restoring the defect with an appropriate
material, or in the majority of cases by the placement of a
restoration that prevents independent movement of the tooth
segments on either side of the crack (11). Therefore, early evaluation of the
extent of cracks has important role in therapy and prognosis.
Herein, we aimed to investigate the impact of cusp
inclination on dental fracture by means of stress analysis by
creating a simulated artificial tooth-crack model, with the degrees
of risks estimated and risk scale formulated, this may provide
certain theoretical bases for treatment plans of tooth cracks, and
the evaluation of long-term prognosis.
Materials and methods
Specimen preparation
This study was approved by the Ethics Committee of
the Affiliated Xuzhou Stomatology Hospital of Xuzhou Medical
University. All enrolled outpatients undergoing orthodontic
extraction provided written informed consent and a total of 70
maxillary premolars with intact radices dentis were included.
Exclusion criteria: abnormal morphology; dental caries, severe wear
or erosion, crack and defect; filling treatment; root canal
therapy; root no. ≥2; curved root canal >30°.
Measurements of cusp inclination
The cusp inclination of extracted maxillary
premolars was measured by digital radiovisiography (RVG). The mean
buccal cusp inclination was 49±1.6° (95% CI, 48.6°-49.3°) and
palatal cusp inclination was 40±1.9° (95% CI, 39.7°-40.3°). To
obviate bias, 40 maxillary premolars with the cusp inclination of
95% CI were enrolled. All eligible teeth underwent cleansing of
soft tissues and calculi, and were stored at room temperature in
normal saline prior to experiment.
Establishment of cracked tooth
model
Forty maxillary premolars were randomized into four
groups (n=10). The bias angle of mean mediobuccal and mediolingual
cusp inclination in CTS was reportedly 9.29° and 9.02° (16), respectively, in order to create a
simulated artificial tooth-crack model, as compared with the value
of the reported cusp inclinations, thereby maxillary premolars in
groups I, II and III as CTS groups were fabricated by increment of
cusp inclination by 10°, 15° and 20°, with those intact teeth in
group IV as controls (Table I).
 | Table I.Grouping of tooth tip samples. |
Table I.
Grouping of tooth tip samples.
| Group | N | Group
descriptions |
|---|
| 1 | 10 | Buccal cusp
inclination 59°, palatal 50° |
| 2 | 10 | Buccal cusp
inclination 64°, palatal 55° |
| 3 | 10 | Buccal cusp
inclination 69°, palatal 60° |
| 4 | 10 | Control group
(intact) |
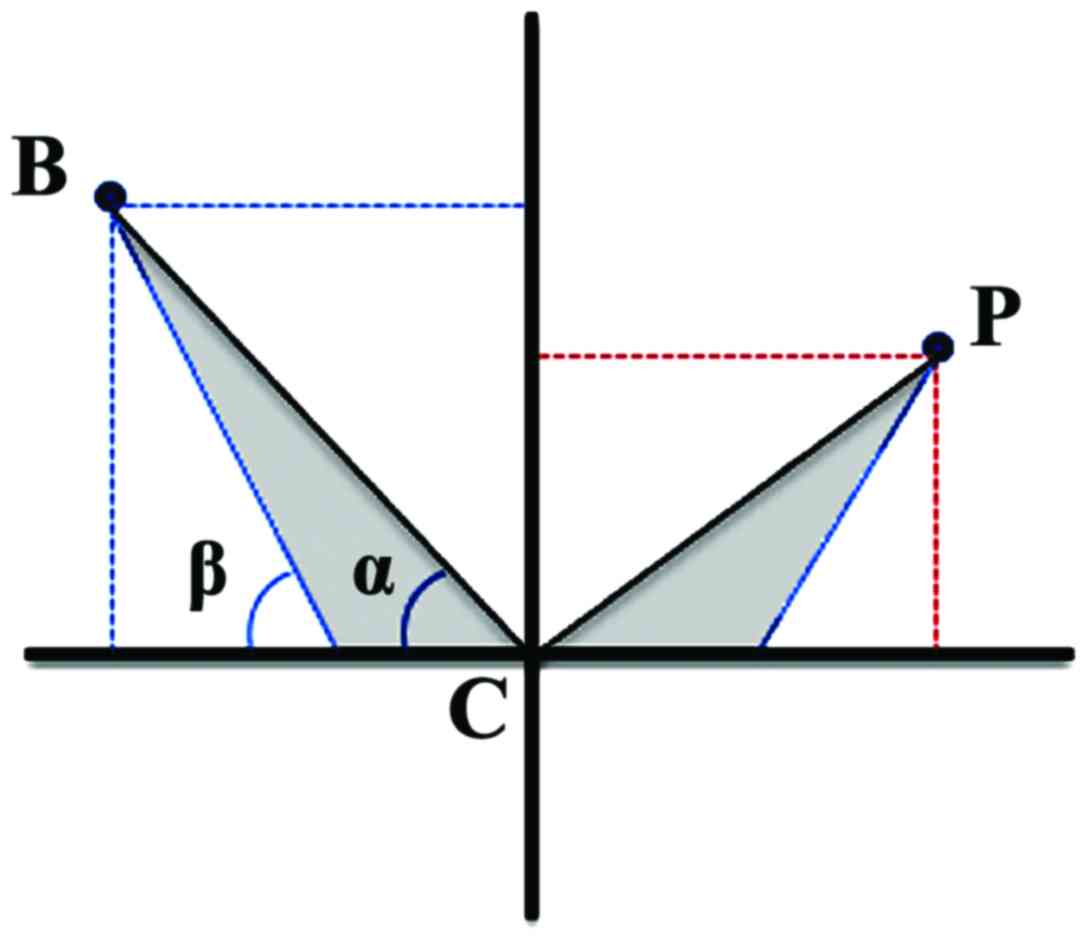
RVG was employed to measure the height (the distance
from cusps to the central fossa plane) and width (the distance from
cusps to the dental longitudinal axis plane) of the buccal and
palatal tooth cusps in the experimental groups for planar mapping
(Fig. 1). To simulate the de facto
cusp inclinations in CTS, parameters were adjusted with the aid of
vernier caliper (precision at 0.02 µm) and diamond burs for
pre-crack on the ~2/3 of mesiodistal diameter of the crown and the
height to the cementoenamel junction (CEJ) by the #700 drill. The
severe and irregular abrasion of the tooth will make the cusps
steeper in clinical practice, thus generating the wedging effect
which could lead to the tooth cracks and fractures. It is required
to maintain the integrity of the bottom of the fovea as far as
possible for simulating clinical condition of such steep cusps
during the adjustment of cuspal inclination. The grinding of cusps
is confined to the enamel layer without involving the dentin.
Therefore, the partial enamel on the cuspal slopes are removed in
order to keep more tooth tissues. The patents would fail to see the
dentist timely when the symptom is not obvious. The clinical
symptoms has a significant relationship with the crack size.
Therefore, the cracks have already expanded when most patients want
to receive the treatment. A tiny silicon carbide bur is used to
prepare relatively larger crack for simulating clinical situation.
All the samples were embedded in the type box, using silicone
rubber to simulate periodontal membrane and self-setting resin to
simulate alveolar bone.
Compression loading test
Prior to compression loading test, bite force test
of Paris plaster molds of CTS by silicone rubber was performed,
which revealed diverse biting contact sites, whereas the majority
of bite contact sites were located in the middle and lower 1/3 of
cusp inclination. All groups underwent compression-loading test to
determine the crack thresholds on an electronic universal
material-testing machine. Briefly, the samples were mounted to the
type boxes, with the teeth longitudinally vertical to the platform,
and loader vertically against the contact site. The loader was
advanced at a velocity of 2 mm/min until the onset of fracture,
with the fracture modes recorded and fracture risk scores
calculated.
Statistical analysis
All analyses were performed using the SPSS version
16.0 (SPSS, Chicago, IL, USA). Data were expressed as mean ± SD.
The rank sum test was used to compare the means of crack threshold
among groups and P<0.05 was considered statistically
significant.
Results
Fracture modes
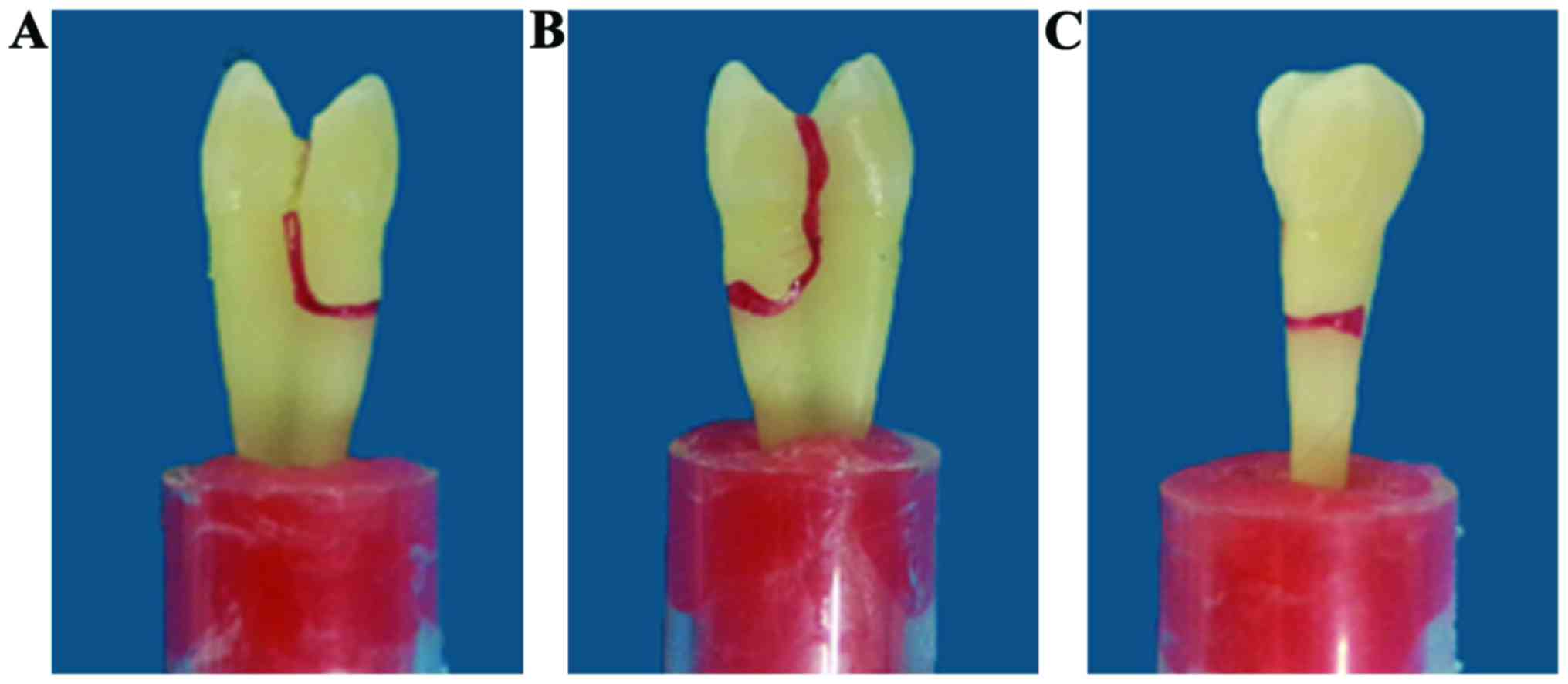
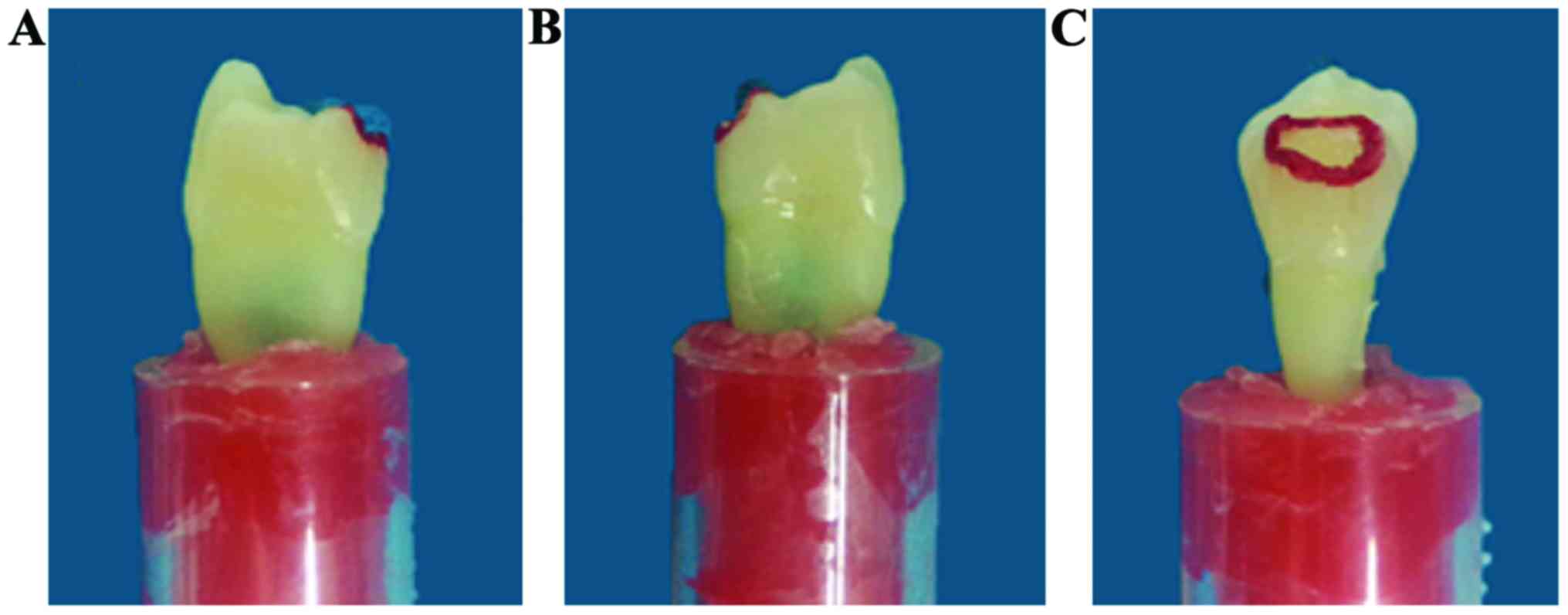
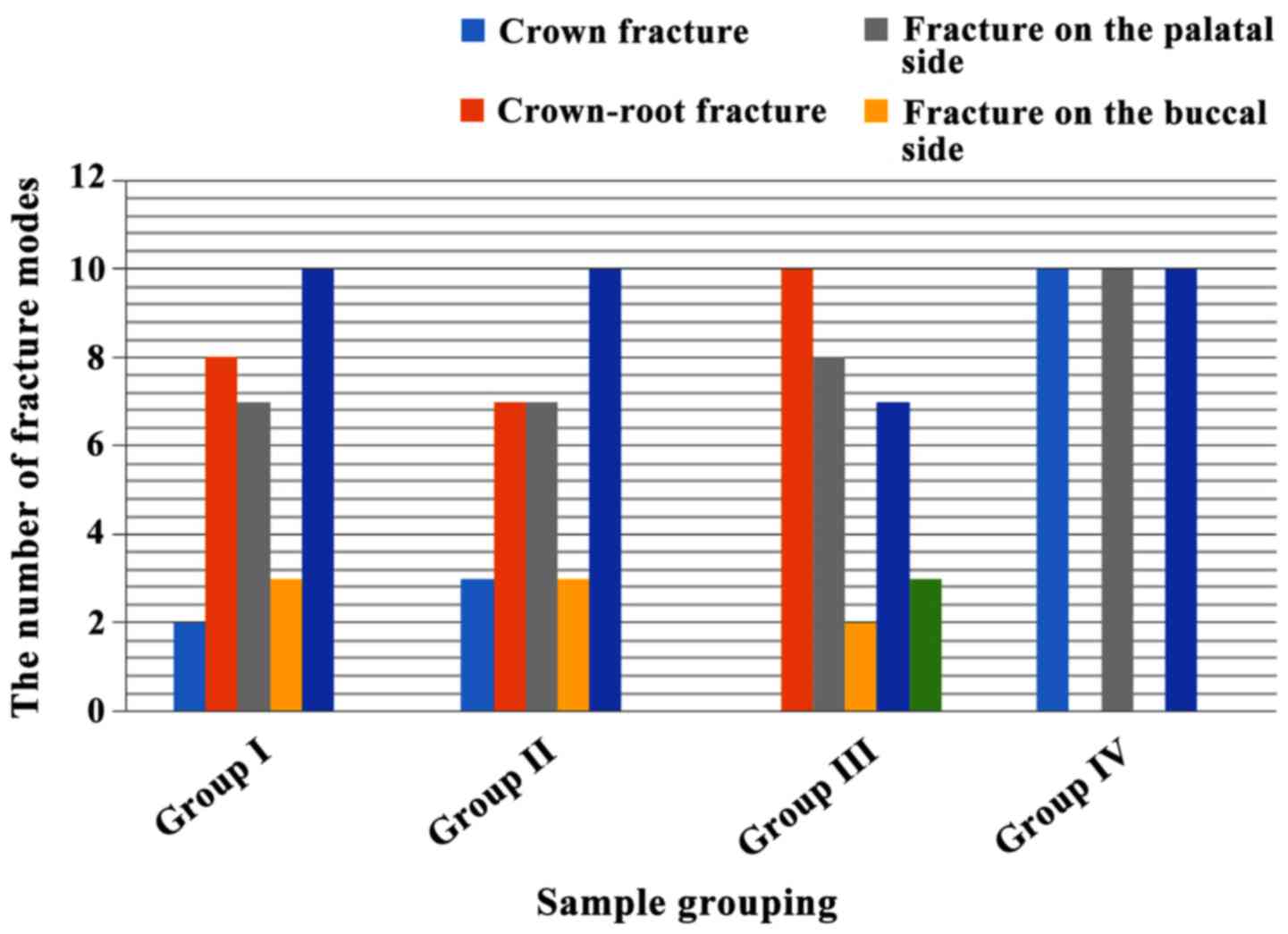
Samples in all groups underwent compression loading
test, resulting in complete fracture (Figs. 2–5).
The fracture modes and numbers in each group are depicted in
Fig. 6. With respect to fracture
sites, groups I and II revealed a majority of fractures of corona
radicis and a minority of coronal fractures, where groups III and
IV exclusively exhibited coronal radical fractures and crown
fracture, respectively; in terms of orientations and angles of
fractures, oblique fractures were dominant in all groups, with a
paucity of longitudinal fractures. With regard to fracture
typology, CTS groups demonstrated complexity and variety in
contrast to the control group.
In group I, the downward extension of cracks was
either from the base of the pre-crack side or across the marginal
ridge. The majority of cracks deflected palatolaterally from the
site 1–2 mm below the CEJ, with a variety of deflect angles and a
multitude of oblique fractures (Table
II). Group II was comparable to group I in crack orientation,
except for occasional crack extension from compression loading
sites and a majority of palatolateral crown root fractures
(Table III). Group III displayed a
likewise crack extension till the CEJ, from where more complicated
crack extensions arose: Either nearby deflection or radical
progression and deflection at different angles and ultimately
complete fractures resulted (Table
IV). In addition, there were a majority of palatolaterally
oblique fractures, with exclusive radical fractures in all samples.
In the control group, oblique cracks generally extended
palatolaterally downward from the compression loading sites at a
variety of deflection angles, with enamel fracture mainly in
mesocoronal or sub-coronal 1/3 portions (Table V). All samples presented
palatolateral coronal fractures (Fig.
6).
 | Table II.Fracture modes of cracked teeth in
group I. |
Table II.
Fracture modes of cracked teeth in
group I.
|
| Fracture modes |
|---|
|
|
|
|---|
| Samples | Coronal | Radical | Palatal | Buccal | Oblique | Vertical |
|---|
| 1 |
| + | + |
| + |
|
| 2 |
| + | + |
| + |
|
| 3 |
| + | + |
|
| + |
| 4 |
| + |
| + | + |
|
| 5 |
| + |
| + | + |
|
| 6 |
| + | + |
| + |
|
| 7 | + |
| + |
| + |
|
| 8 |
| + | + |
| + |
|
| 9 |
| + |
| + | + |
|
| 10 | + |
| + |
| + |
|
| Total | 2 | 8 | 7 | 3 | 9 | 1 |
 | Table III.Fracture modes of cracked teeth in
group II. |
Table III.
Fracture modes of cracked teeth in
group II.
|
| Fracture modes |
|---|
|
|
|
|---|
| Samples | Coronal | Radical | Palatolateral | Buccolateral | Oblique | Vertical |
|---|
| 1 | + |
| + |
| + |
|
| 2 |
| + | + |
| + |
|
| 3 |
| + |
| + | + |
|
| 4 |
| + | + |
| + |
|
| 5 |
| + |
| + | + |
|
| 6 |
| + | + |
| + |
|
| 7 |
| + | + |
| + |
|
| 8 |
| + | + |
| + |
|
| 9 | + |
|
| + | + |
|
| 10 |
| + | + |
| + |
|
| Total | 3 | 7 | 7 | 3 | 10 | 0 |
 | Table IV.Fracture modes of cracked teeth in
group III. |
Table IV.
Fracture modes of cracked teeth in
group III.
|
| Fracture modes |
|---|
|
|
|
|---|
| Samples | Coronal | Radical | Palatolateral | Buccolateral | Oblique | Vertical |
|---|
| 1 |
| + |
| + | + |
|
| 2 |
| + | + |
| + |
|
| 3 |
| + | + |
| + |
|
| 4 |
| + | + |
| + |
|
| 5 |
| + | + |
| + |
|
| 6 |
| + | + |
| + |
|
| 7 |
| + | + |
|
| + |
| 8 |
| + |
| + | + |
|
| 9 |
| + | + |
| + |
|
| 10 |
| + | + |
| + |
|
| Total | 0 | 10 | 8 | 2 | 8 | 2 |
 | Table V.Fracture modes of cracked teeth in
group IV. |
Table V.
Fracture modes of cracked teeth in
group IV.
|
| Fracture modes |
|---|
|
|
|
|---|
| Samples | Coronal | Radical | Palatolateral | Buccolateral | Oblique | Vertical |
|---|
| 1 | + |
| + |
| + |
|
| 2 | + |
| + |
| + |
|
| 3 | + |
| + |
| + |
|
| 4 | + |
| + |
| + |
|
| 5 | + |
| + |
| + |
|
| 6 | + |
| + |
| + |
|
| 7 | + |
| + |
| + |
|
| 8 | + |
| + |
| + |
|
| 9 | + |
| + |
| + |
|
| 10 | + |
| + |
| + |
|
| Total | 10 | 0 | 10 | 0 | 10 | 0 |
Estimation of fracture risk levels for
cracked teeth
With reference to the de facto fracture modes of
cracked teeth, the endodotists and dental restoration specialists
formulated the fracture risk estimation scale (Table VI) of cracked teeth, which embodied
findings from relevant studies (13)
and provided practicable therapeutic options. Table VII illustrates the fracture risk
scores in the four groups by the estimation scale. There were
significant statistical differences in the fracture risk levels in
group III and IV as compared with the other groups, respectively
(P<0.05); the differences between groups I and II were
insignificant (P>0.05). The fracture risk levels were similar in
groups I and II; the fracture risk levels in group III were diverse
and complicated, with higher scores for fracture risk levels and
higher susceptibility of severe fractures. Group IV had the lowest
scores for fracture risk levels and were the least susceptible for
severe fractures.
 | Table VI.Scale for fracture risk levels of CTS
and regimens. |
Table VI.
Scale for fracture risk levels of CTS
and regimens.
| Levels | Criteria | Regimens |
|---|
| I | Coronal fracture
with intact dental pulp | Occlusal
adjustment; filling treatment; indirect pulp capping; full crown
capping |
| II | Coronal fracture
involving dental pulp | Direct pulp
capping; root canal treatment and full crown capping |
| III | Coronoradical
fracture ≥2 mm above DEJ | Root canal
treatment and full crown capping |
| IV | Coronoradical
fracture at upper 1/3 portion of root, the radical length ≥18
mm | Dental crown
lengthening, root canal treatment and full crown capping |
| V | Coronoradical
fracture at upper 1/3 portion of root, the radical length <18
mm | Poor results, there
is only a part of them can be treated as level IV |
| VI | Coronoradical
fracture at middle and lower 2/3 portion of root | Poor results, all
of them should be extracted |
 | Table VII.Scores for fracture risk levels of
CTS. |
Table VII.
Scores for fracture risk levels of
CTS.
| Group | I | II | III | IV | V | VI |
|---|
| I | 0 | 3 | 6 | 1 | 0 | 0 |
| II | 0 | 1 | 6 | 3 | 0 | 0 |
| III | 0 | 0 | 1 | 4 | 2 | 3 |
| IV | 4 | 6 | 0 | 0 | 0 | 0 |
Discussion
Dental anatomy could partially account for its
susceptibility to fracture (19),
with cusp inclination being one of the critical etiologies.
Measurements of the cuspal inclinations on the radiograms of
histological sections in each of the five posterior teeth samples
revealed that cuspal inclination played a pivotal role in fracture
potential and in the incidence of complete or incomplete cuspal
fractures (20). Moreover, for the
compromised teeth with CTS, steeper cuspal inclination frequently
reportedly leads to an increment in tensile stress at the center
groove and cervical region, predisposing to fracture formation
(21). Three-dimensional finite
element model (3-DFEM) has been applied in CTS study (22) and is well acknowledged for its
advantages in evaluation of cuspal morphology with respect to
mechanical analysis of stress distribution, whereas 3-DFEM is also
noted for its limitations in terms of functional analysis, in which
the majority of studies in CTS are restricted to loading stress
analysis and studies of fracture modality is largely restrained
(23). Given the status quo of
3-DFEM, our experiment was focused on the ex vivo teeth and
simulated with endeavor the de facto endodontic environment so as
to compensate for the drawbacks of 3-DFEM in CTS study.
Our experiment, with all the stress loading and
fracture procedures visually recorded with high resolution,
obtained the detailed data of the fracture modality of all the
samples, which is unprecedented in CTS study. As for the sites of
fracture onset, the cracks in CTS and control groups extended from
pre-crack site and stress loading area, respectively. The
difference in crack-onset sites is attributable to the distinctions
in stress focus distribution. Based on the analysis of mechanics of
materials, the stress-focused areas are the sites with defects of
the materials per se or the stress-loaded, i.e. in the CTS group,
the stress-focus was the pre-crack site, or rather, the area of
dental defect, whereas in the control group, the contact site of
the stress loader. The more complex and severe root fractures of
the samples often occur in the CTS groups compared with control
group. Cracked tooth always suffer splitting while the normal tooth
have enamel defect clinically. The experimental results agree with
the clinical observation. In the CTS groups, the sites of tooth
fractures have the trend to move toward the root apex with the
gradient increase of the cupsal inclinations, this may indicate
that the steeper cupsal inclinations could lead to the more complex
fracture pattern and more rugged splitting path, thus it plays an
important role in the choice of treatment plan and prognosis.
Observation and analysis of the crack extension
process revealed a multitude of oblique fractures with uneven
routes characterized by deflection in arch or complex zig-zags,
which is correlated with the heterogeneity in dental composition
and resilience involved. Intraenamel protein composites contribute
to the diminished stress focus on the tip of enamel crack and
enhanced resistance to crack and fracture (21). In addition, crack extension is
typically countered with the increment in resistance of enamel, and
the route of crack extension mainly rests on the extension
interface with enamel and its microstructure (24), and there may be prism decussation
adjacent to the EDJ (3), all of
which contribute to the complexity of crack extension. All these
findings of intradental microstructure may well account for the
crack extension modality in our experiment, in which fracture is
characteristically vertical or oblique, coupled with enamel
exfoliation. Our results were consistent with the reports on dental
defoliation and splitting that overload on the teeth would result
in higher risk for fracture: longitudinal loading would extend the
vertical crack downward to the dentin and penetrate to the dental
base, causing splitting of a molar or premolar; chipping cracks can
extend to the enamel-dentin interface, causing a partial
fragmentation of a tooth; transverse cracks most notably in canines
under lateral loading can directly penetrate into the subterranean
dentin, rendering the tooth impaired (25).
In our experiment, enamel stripping is predominant
in the control group, whereas the CTS group was dominated by
crown-root fracture, which proportionally increases with the
increment of cusp inclination, and the ultimate fracture site may
exhibit a tendency of shifting towards the radical tip. We thus
postulated that the cracked teeth are more prone to perpendicular
fracture with the increment of cusp inclination to a certain angle,
coupled with the enhanced complexity of fracture modes and
routes.
Numerous clinical therapeutic regimens are available
regarding the CTS, such as occlusal adjustment, orthodontics and
annulation, cusp and crown capping, depending on the clinical
manifestations (26). In the case of
fractures, however, cracked teeth should be evaluated for the value
of conservation according to the severity. Accordingly, we
formulated the fracture risk scale and provided relevant
recommendations on the regimen options. Our experiment revealed
that the control group had a high prevalence of coronal fractures,
with fracture risks of I and II, for which unelaborated regimens
suffice and the prognosis is good. The CTS group had a majority of
crown-root fractures, which were categorized as high risks. The
cusp inclinations in groups I and II were of relative minor angles,
with the fracture risk of III in the majority of samples; group III
had the greatest cusp inclinations, which had higher fracture risks
and even risk of VI, i.e. complete vertical fracture till the root
apex. The increment of cusp inclination to certain angles in CTS
would increase the susceptibility to fracture of higher risks,
which greatly hamper the therapeutic regimens and prognosis. In the
case of severe fractures in CTS, particularly those beneath
alveolar ridge crest, clinicians should meticulously evaluate the
fracture sites and radical lengths and in certain cases, subsequent
to root canal treatment, periodontal surgery is required prior to
restorative therapy. Our experiment may provide recommendations to
clinicians in examinations of CTS in addressing cusp inclinations.
In cases of steeper cusp inclinations, adjustments for reduction
should be made to obviate severe consequences as fracture.
Additionally, our fracture risk scale may benefit clinicians in
decision making as to rapid estimation of tooth conservation and
provide patients with optimal regimen options.
This study has limitations in that our experiment
utilized static stress algorithms to simulate the endodontic
stress, which may create certain bias versus the de facto profiles.
Moreover, our credibility and reliability are discounted due to the
present sample size, which needs to be addressed in a future
study.
Acknowledgements
In the present study, the pathogenesis and clinical
research on cracked teeth of the innovation team was supported by
the Health and Family Planning Commission of Xuzhou Municipal
Government, Jiangsu Province, China (no. XWCX201609).
References
|
1
|
DeGusta D, Everett MA and Milton K:
Natural selection on molar size in a wild population of howler
monkeys (Alouatta palliata). Proc Biol Sci. 270 Suppl 1:pp.
S15–S17. 2003, View Article : Google Scholar : PubMed/NCBI
|
|
2
|
King SJ, Arrigo-Nelson SJ, Pochron ST,
Semprebon GM, Godfrey LR, Wright PC and Jernvall J: Dental
senescence in a long-lived primate links infant survival to
rainfall. Proc Natl Acad Sci USA. 102:pp. 16579–16583. 2005,
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chai H, Lee JJ, Constantino PJ, Lucas PW
and Lawn BR: Remarkable resilience of teeth. Proc Natl Acad Sci
USA. 106:pp. 7289–7293. 2009, View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sui T, Lunt AJ, Baimpas N, Sandholzer MA,
Li T, Zeng K, Landini G and Korsunsky AM: Understanding nature's
residual strain engineering at the human dentine-enamel junction
interface. Acta Biomater. 32:256–263. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lee JJ, Constantino PJ, Lucas PW and Lawn
BR: Fracture in teeth: A diagnostic for inferring bite force and
tooth function. Biol Rev Camb Philos Soc. 86:959–974. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Geurtsen W, Schwarze T and Günay H:
Diagnosis, therapy, and prevention of the cracked tooth syndrome.
Quintessence Int. 34:409–417. 2003.PubMed/NCBI
|
|
7
|
Lubisich EB, Hilton TJ and Ferracane J:
Northwest Precedent: Cracked teeth: A review of the literature. J
Esthet Restor Dent. 22:158–167. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim SY, Kim SH, Cho SB, Lee GO and Yang
SE: Different treatment protocols for different pulpal and
periapical diagnoses of 72 cracked teeth. J Endod. 39:449–452.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lynch CD and McConnell RJ: The cracked
tooth syndrome. J Can Dent Assoc. 68:470–475. 2002.PubMed/NCBI
|
|
10
|
Davis R and Overton JD: Efficacy of bonded
and nonbonded amalgam in the treatment of teeth with incomplete
fractures. J Am Dent Assoc. 131:469–478. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Griffin JD Jr: Efficient, conservative
treatment of symptomatic cracked teeth. Compend Contin Educ Dent.
27(93–102): quiz 103. 1122006.
|
|
12
|
Ratcliff S, Becker IM and Quinn L: Type
and incidence of cracks in posterior teeth. J Prosthet Dent.
86:168–172. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Geurtsen W and García-Godoy F: Bonded
restorations for the prevention and treatment of the cracked-tooth
syndrome. Am J Dent. 12:266–270. 1999.PubMed/NCBI
|
|
14
|
Chong BS: Bilateral cracked teeth: A case
report. Int Endod J. 22:193–196. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Khers SC, Carpenter CW, Vetter JD and
Staley RN: Anatomy of cusps of posterior teeth and their fracture
potential. J Prosthet Dent. 64:139–147. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Qian Y, Zhou X and Yang J: Correlation
between cuspal inclination and tooth cracked syndrome: a
three-dimensional reconstruction measurement and finite element
analysis. Dent Traumatol. 29:226–233. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sadasiva K, Ramalingam S, Rajaram K and
Meiyappan A: Cracked tooth syndrome: A report of three cases. J
Pharm Bioallied Sci. 7 Suppl 2:S700–S703. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Banerji S, Mehta SB and Millar BJ: Cracked
tooth syndrome. Part 2: Restorative options for the management of
cracked tooth syndrome. Br Dent J. 208:503–514. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bader JD, Shugars DA and Martin JA: Risk
indicators for posterior tooth fracture. J Am Dent Assoc.
135:883–892. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Seo DG, Yi YA, Shin SJ and Park JW:
Analysis of factors associated with cracked teeth. J Endod.
38:288–292. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Barani A, Chai H, Lawn BR and Bush MB:
Mechanics analysis of molar tooth splitting. Acta Biomater.
15:237–243. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Imanishi A and Nakamura T, Ohyama T and
Nakamura T: 3-D Finite element analysis of all-ceramic posterior
crowns. J Oral Rehabil. 30:818–822. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ji B and Gao H: A study of fracture
mechanisms in biological nano-composites via the virtual internal
bond model. Mater Sci Eng A. 366:96–103. 2004. View Article : Google Scholar
|
|
24
|
Padmanabhan SK, Balakrishnan A, Chu MC,
Kim TN and Cho SJ: Micro-indentation fracture behavior of human
enamel. Dent Mater. 26:100–104. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chai H, Lee JJ and Lawn BR: On the
chipping and splitting of teeth. J Mech Behav Biomed Mater.
4:315–321. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Turp JC and Gobetti JP: The cracked tooth
syndrome: An elusive diagnosis. J Am Dent Assoc. 127:1502–1507.
1996. View Article : Google Scholar : PubMed/NCBI
|