Introduction
With the continuous improvement of living standards
in China, the incidence of non-alcoholic fatty liver disease
(NAFLD), a disease previously almost exclusive of Western
countries, has been increasing year by year, and it has become one
of the most common liver diseases affecting human health (1,2). Studies
have shown that NAFLD can lead to metabolic disorders and diseases,
which are closely related to hypertension and coronary heart
disease (3). Cardiac bypass surgery
and coronary stent implantation are common effective surgical
treatments for coronary heart disease. But a series of adverse
cardiovascular events after surgery still seriously threaten the
life and health of those patients. Studies have shown that the
bypass surgery induces the production and release of inflammatory
factors in patients with coronary heart disease, affecting the
prognosis of patients with coronary heart disease after surgery
(4–6). At present, there are few studies on the
relationship between the changes in inflammatory factors and the
prognosis of coronary heart disease patients complicated with NAFLD
after bypass surgery. In this study, the changes in expressions
levels of inflammatory factors in peripheral blood of coronary
heart disease patients complicated with NAFLD at different
time-points before and after bypass surgery were investigated and
their relationship to the patient prognosis were assessed, in order
to provide a theoretical basis for clarifying mechanisms at
play.
Patients and methods
Patients
The subjects in this study were a total of 68
patients were admitted to Xinjiang Hospital due to stable angina
pectoris from August 2013 to August 2015 scheduled to undergo
coronary artery bypass grafting (CABG). There were 30 males and 38
females aged 53–87 years. Diagnostic criteria for stable angina
pectoris included the fact that the conditions of onset did not
change within 1–3 months, the daily and weekly onset frequencies
were roughly similar, the fatigue and degree of pain were stable,
and the nature and site of pain were the same in every attack.
Diagnostic criteria for NAFLD included histological changes in
liver biopsy conformed to the pathological or imaging criteria of
fatty liver disease, and the fact that patients had no alcohol
drinking history or an alcohol consumption per week of <140 g;
and other fatty liver-specific diseases caused by viral hepatitis
or drug-induced hepatitis had been ruled out. A total of 68
patients undergoing CABG were divided into the NAFLD and the
non-NAFLD control group. Other consumptive diseases were excluded
in all patients enrolled and they all signed informed consent
forms. All patients had complete clinical and pathological data and
completed the treatment regimen. The patients were followed-up for
6 months after the procedure and the major adverse cardiac events
were recorded, including death, myocardial infarction and angina
pectoris. The study was approved by the Ethics Committee of the
Second Affiliated Hospital of Xinjiang Medical University.
CABG
All the patients enrolled received routine treatment
for coronary heart disease, they all took a sufficient dose of
enteric-coated aspirin and clopidogrel before the operation and the
same dose of unfractionated heparin during the procedure, and they
all underwent the multi-position projection after CABG to ensure
the procedure had been successful.
Collection and storage of samples
Peripheral venous blood (5 ml) were drawn from
patients before and at 24 h and 1 month after the operation. After
natural coagulation, the samples were centrifuged at 1,700 × g for
10 min. The serum was separated, quickly frozen, and stored in the
freezer at −80°C for subsequent processing.
Instruments and reagents
Innova-3100 full digital cardiovascular angiographic
system (Thermo Fisher Scientific, Waltham, MA, USA).
Detection of high-sensitivity
C-reactive protein (hsCRP), soluble CD40 ligand (sCD40L),
intercellular adhesion molecule-1 (ICAM-1) and matrix
metalloproteinase-9 (MMP-9) in peripheral blood by enzyme-linked
immunosorbent assay (ELISA)
Serum samples obtained from the patients were
diluted 100 times in preparation for conventional ELISA tests.
Standard and diluted serum samples (10 µl) were added onto each
labeled reaction plate according to the instructions of the
high-sensitivity hsCRP detection kit and the sCD40L detection kit
(both from R&D Systems, Inc., Minneapolis, MN, USA), the ICAM-1
detection kit or the MMP-9 detection kit (both from Invitrogen;
Thermo Fisher Scientific, Inc., Waltham, MA, USA). Briefly, 100 µl
conjugate reagent were added into each well, shaken slightly for 30
sec and incubated for 60 to 90 min at room temperature. The liquid
in the reaction plate was shaken dry and phosphate-buffered saline
(PBS; self-prepared by our laboratory) was added to wash the
reaction plate 5 times. Horseradish peroxidase (HRP) was added and
shaken slightly for 30 sec and incubated for 30 min at room
temperature. The liquid in the reaction plate was shaken dry again,
and PBS was added to wash the reaction plate 5 times. Then
tetramethylbenzidine (TMB) developing solution was added for
incubation at room temperature for 20 min. Finally, 100 µl of stop
solution were added and shaken slightly for 30 sec, and the
absorbance values of samples were measured using the microplate
reader (450 nm). The contents of hsCRP, sCD40L, ICAM-1 and MMP-9 in
samples in each group were calculated.
Statistical analysis
The data in this study were presented as mean ±
standard deviation. SPSS 19.0 software (SPSS, Inc., Chicago, IL,
USA) was used for data analysis. t-test was used for intergroup
comparisons, and analysis of variance was used for comparisons
among groups. The homogeneity test of variance was performed and
logistic regression analysis was used for the relationship between
levels of inflammatory factors and the presence of postoperative
adverse cardiovascular events. P<0.05 was considered to indicate
a statistically significant difference.
Results
General data analysis
The clinicopathology data and treatment plans of
patients before the CABG procedure were summarized. The results on
Table I showed that there were no
statistically significant differences in terms of age, sex, smoking
history or preventive drug use between the patients in the NAFLD
and the non-NAFLD groups (p>0.05). Average alanine
aminotransferase (ALT) levels in the NAFLD group were significantly
higher than those in the non-NAFLD group, and the difference was
statistically significant (p<0.01).
 | Table I.Comparisons of general data of
patients in the two groups before operation (mean ± standard
deviation). |
Table I.
Comparisons of general data of
patients in the two groups before operation (mean ± standard
deviation).
| Index | NAFLD group | Non-NAFLD group | P-value |
|---|
| Sex
(male/female) | 14/17 | 16/21 | 0.382 |
| Age (years) | 65.3±8.9 | 67.8±10.6 | 0.295 |
| History of smoking
(%) | 45.6% | 42.7% | 0.423 |
| Hypertension (%) | 77.4% | 67.6% | 0.076 |
| Aspirin | 93.5% | 94.6% | 0.589 |
| ACEI drugs | 51.6% | 51.3% | 0.657 |
| Statins | 96.8% | 94.6% | 0.569 |
| ALT (U/l) | 69.32±11.26 | 25.65±7.52 | 0.008a |
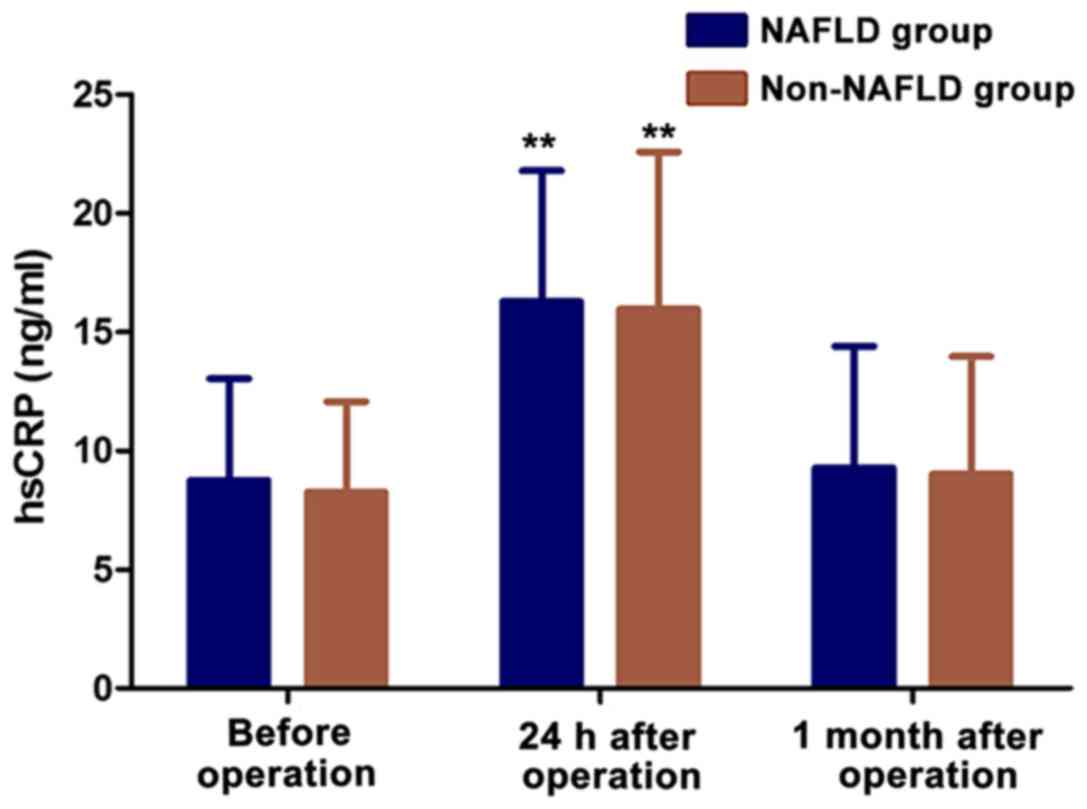
Expression level of hsCRP in peripheral blood. The
expression level of hsCRP in peripheral blood of patients was
detected using an hsCRP kit. The results on Table II and Fig. 1 show that the expression levels of
hsCRP in the NAFLD and non-NAFLD groups were significantly higher
at 24 h after the CABG operation than before or one month after the
procedure in each group (p<0.01). However, there were no
statistically significant differences in the expression levels of
hsCRP before and at 1 month after the operation (p>0.05); and
also there were no statistically significant differences in the
expression levels of hsCRP between the NAFLD and non-NAFLD groups
(p>0.05).
 | Table II.Average hsCRP expression levels in
peripheral blood of patients in the two groups. |
Table II.
Average hsCRP expression levels in
peripheral blood of patients in the two groups.
|
| hsCRP (ng/ml) |
|---|
|
|
|
|---|
| Detection time | NAFLD group | Non-NAFLD group |
|---|
| Before operation |
8.76±4.27 |
8.25±3.82 |
| 24 h after
operation |
16.27±5.52a |
15.96±6.26a |
| 1 month after
operation |
9.27±5.13 |
9.02±4.95 |
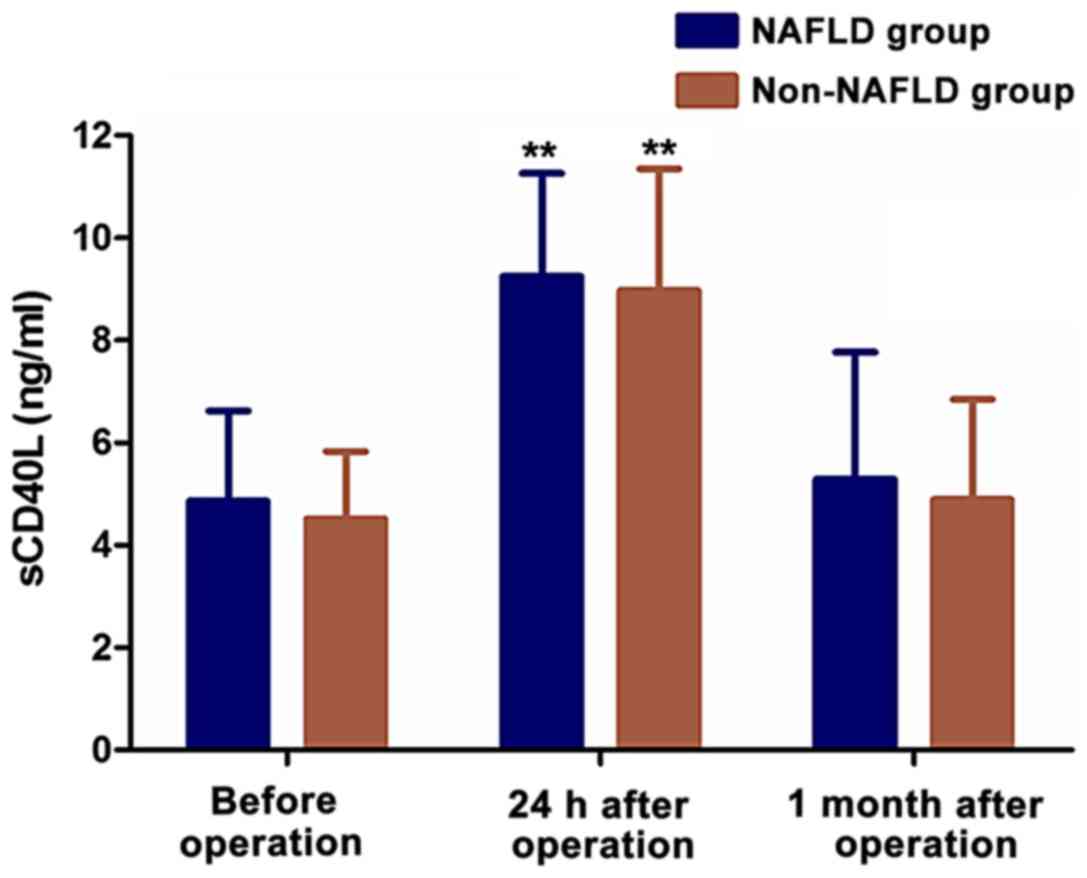
Expression level of sCD40L in
peripheral blood
The expression level of sCD40L in peripheral blood
of patients was detected using a sCD40L kit. The results on
Table III and Fig. 2 show that the expression levels of
sCD40L in NAFLD group and non-NAFLD group were highest at 24 h
after operation in both groups (p<0.01). However, there were no
statistically significant differences in the expression levels of
sCD40L before and at one month after the operation (p>0.05); and
there were no statistically significant differences in the
expression levels of sCD40L between the NAFLD and non-NAFLD groups
(p>0.05).
 | Table III.sCD40L expression levels in peripheral
blood of patients in the two groups. |
Table III.
sCD40L expression levels in peripheral
blood of patients in the two groups.
|
| sCD40L (ng/ml) |
|---|
|
|
|
|---|
| Detection time | NAFLD group | Non-NAFLD group |
|---|
| Before operation |
4.86±1.76 |
4.51±1.32 |
| 24 h after
operation |
9.25±2.01a |
8.97±2.38a |
| 1 month after
operation |
5.29±2.48 |
4.89±1.96 |
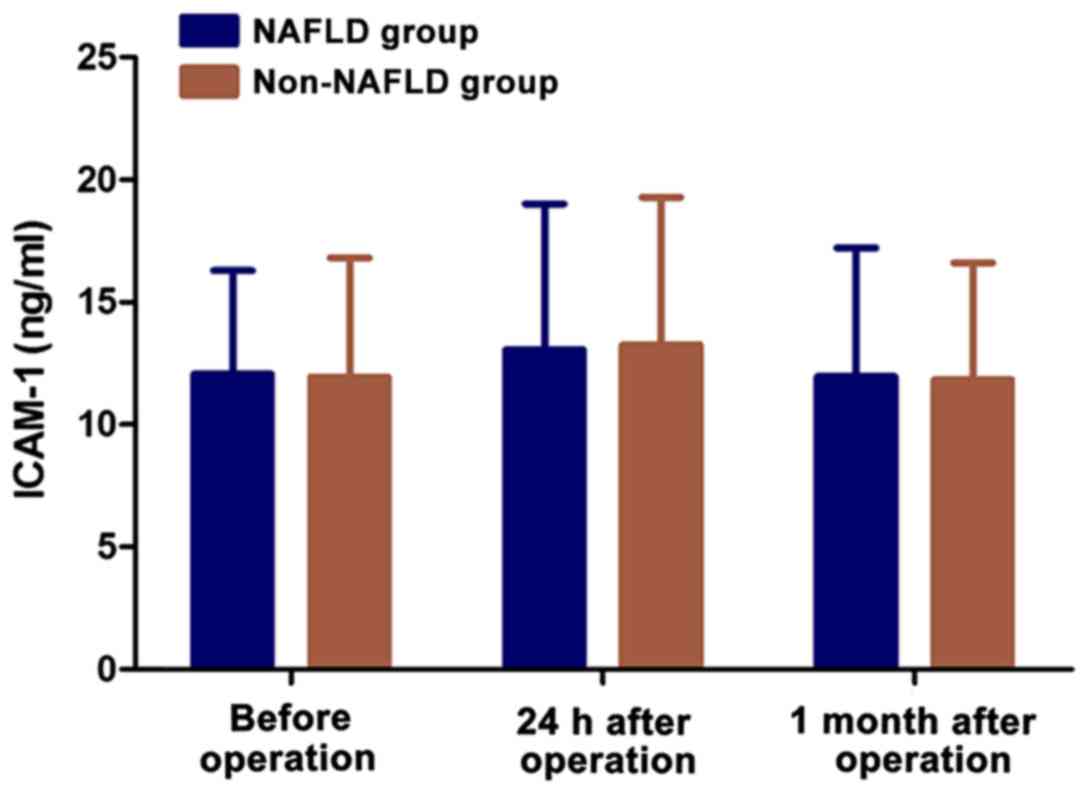
Expression level of ICAM-1 in
peripheral blood
The expression level of ICAM-1 in peripheral blood
of patients was detected using an ICAM-1 ELISA kit. The results
shown on Table IV and Fig. 3 reveal a slight increase in the
expression levels of ICAM-1 one day after the CABG procedure in the
two groups. But there was no statistically significant difference
in the expression levels between the two groups before and after
the operation (p>0.05).
 | Table IV.ICAM-1 expression levels in peripheral
blood of patients in the two groups. |
Table IV.
ICAM-1 expression levels in peripheral
blood of patients in the two groups.
|
| ICAM-1 (ng/ml) |
|---|
|
|
|
|---|
| Detection time | NAFLD group | Non-NAFLD group |
|---|
| Before operation |
12.06±4.23 |
11.95±4.86 |
| 24 h after
operation |
13.67±5.95 |
13.25±6.03 |
| 1 month after
operation |
11.96±5.26 |
11.83±4.77 |
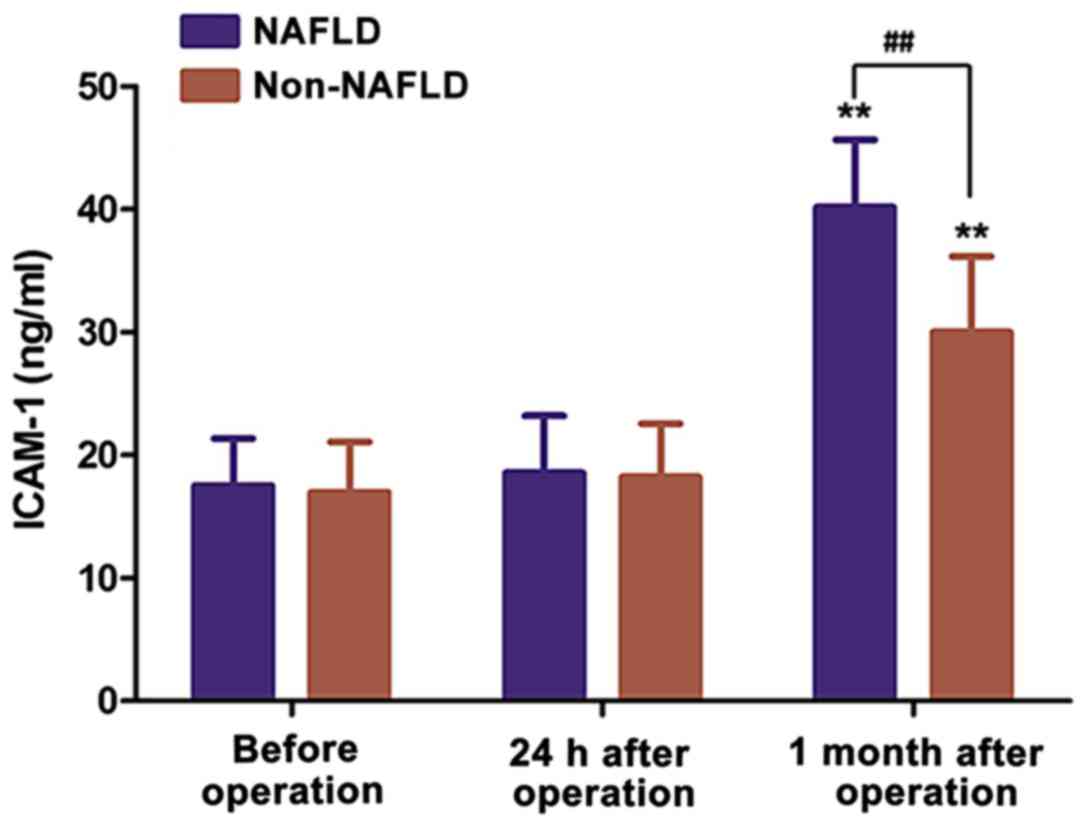
Expression level of MMP-9 in
peripheral blood
The expression level of MMP-9 in peripheral blood of
patients was detected using an MMP-9 kit. The results in Table V and Fig.
4 show the expression levels of MMP-9 increased significantly
after the operation and reached a peak one month after the
procedure (p<0.01). Importantly, the expression levels of MMP-9
in peripheral blood in the NAFLD group at 1 month after the CABG
procedure were significantly higher than those in the non-NAFLD
group (p<0.01).
 | Table V.MMP-9 expression levels in peripheral
blood of patients in the two groups. |
Table V.
MMP-9 expression levels in peripheral
blood of patients in the two groups.
|
| MMP-9 |
|---|
|
|
|
|---|
| Detection time | NAFLD group | Non-NAFLD group |
|---|
| Before operation |
17.52±3.86 |
16.97±4.11 |
| 24 h after
operation |
18.56±4.67 |
18.22±4.35 |
| 1 month after
operation |
40.18±5.51a,b |
30.02±6.15a |
Relationship between inflammatory
factor levels in peripheral blood and prognosis
The number of adverse cardiovascular events was
recorded for 6 months after the CABG operation through follow-up of
patients. The results can be seen on Table VI. The total incidence of adverse
cardiovascular events of patients in the non-NAFLD group was
significantly lower than that of patients in the NAFLD group
(p=0.029). Logistic regression analysis was used to analyze the
expression levels of hsCRP, sCD40L, ICAM-1 and MMP-9 in peripheral
blood of patients and the rates of adverse cardiovascular events
within 6 months after operation, and the results showed that the
expression level of MMP-9 was an important influencing factor of
cardiovascular events after CABG (OR=1.182, p<0.05).
 | Table VI.Percentages of adverse cardiovascular
events in the two groups. |
Table VI.
Percentages of adverse cardiovascular
events in the two groups.
| Adverse
cardiovascular events | NAFLD group | Non-NAFLD group | P-value |
|---|
| Death (%) | 3.2% | 0 | 0.356 |
| Angina pectoris | 9.7% | 8.1% | 0.187 |
| Myocardial
infarction | 6.5% | 5.4% | 0.276 |
| Total adverse
cardiovascular events | 19.4% | 13.5% | 0.029a |
Discussion
NAFLD can significantly increase the morbidity and
mortality rates of coronary heart disease patients (7–9). The
inflammatory response in vessels gets activated after bypass
operation or coronary stenting, and leads to platelet aggregation
and adhesion and further release of inflammatory mediators. Current
studies have found that hsCRP, sCD40L, ICAM-1 and MMP-9 are
commonly affected inflammatory factors (10–12).
Investigating the relationship between the expression levels of
inflammatory factors in peripheral blood after coronary bypass
operation and the treatment outcomes in patients is important to be
able to provide the patients with a more accurate prognosis.
CRP, an acute response albumin in the body, is an
important factor in the inflammatory process, and is considered to
be closely related to the occurrence, development and prognosis of
coronary artery diseases. Studies have shown that CABG can cause
vascular endothelial injury, and a series of cytokines get
expressed during the process, such as CRP (13). CD40L is a surface glycoprotein that
can be expressed in human atherosclerotic plaques and vascular
endothelial cells (14). It was
found in this study that hsCRP and sCD40L levels in peripheral
blood of patients were increased 24 h after the CABG operation, and
the levels were significantly higher than those before and at 1
month after the procedure (p<0.01). This is consistent with a
different study where it was found that after stenting, patients
with coronary artery disease had increased expression levels of
hsCRP in peripheral blood (15).
Likewise, Napoleão et al (16) found that the expression levels of
sCD40L were significantly increased in peripheral blood within 10
min after CABG compared with those before operation, suggesting
that the levels may be associated with postoperative systemic
inflammatory responses. Ma et al (17) showed that the expression levels of
ICAM-1 increased slightly in peripheral blood of patients in the
two groups after operation, but the differences were not
statistically significant. The expression level of ICAM-1 of
patients in NAFLD group almost had no change. This is inconsistent
with literature reports where it was found that the ICAM-1 levels
were increased when using a coronary artery injury model after CABG
(may be due to the vascular damage response), or that the levels
were low in other conditions (may be because of a negative feedback
regulation mechanisms) (18,19). Then again, it was found in this study
that the expression levels of MMP-9 in peripheral blood of patients
in the two groups were highest one day after the CABG procedure,
and that the levels in the NAFLD group were significantly higher
than those in the non-NAFLD group (p<0.01). Furthermore,
regression analysis showed that MMP-9 is an important influencing
factor for adverse cardiovascular events after the bypass
operation. These results are not surprising given that animal
experiments had already proved that MMP-9 inhibitors can reduce
restenosis after stenting, so it was suggested that MMP-9 and its
inhibitors are involved in the development of in-stent restenosis
(20). Based on these data, we
believe that MMP-9 may be an important inflammatory mediator after
coronary stenting, which is increased for a long time after the
bypass operation for coronary heart disease in patients complicated
with NAFLD, so it can be used as an inflammatory marker to predict
adverse events of coronary heart disease in these patients.
In conclusion, the expression levels of inflammatory
factors in peripheral blood of patients complicated with NAFLD
undergoing CABG are different from those of non-complicated
patients, and high levels of MMP-9 are associated with higher risk
of adverse cardiovascular events after the operation. MMP-9 should
be useful as an inflammatory marker for predicting the risk of
adverse events for coronary heart disease patients complicated with
NAFLD undergoing CABG procedures.
References
|
1
|
Sun X, Duan X, Wang C, Liu Z, Sun P, Huo
X, Ma X, Sun H, Liu K and Meng Q: Protective effects of
glycyrrhizic acid against non-alcoholic fatty liver disease in
mice. Eur J Pharmacol. 806:75–82. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yahagi M, Tsuruta M, Hasegawa H,
Okabayashi K and Kitagawa Y: Non-alcoholic fatty liver disease
fibrosis score predicts hematological toxicity of chemotherapy
including irinotecan for colorectal cancer. Mol Clin Oncol.
6:529–533. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chan WK, Nik Mustapha NR, Wong GL, Wong VW
and Mahadeva S: Controlled attenuation parameter using the
FibroScan® XL probe for quantification of hepatic
steatosis for non-alcoholic fatty liver disease in an Asian
population. United European Gastroenterol J. 5:76–85. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Morimoto T, Mineharu Y, Ono K and
Nakatochi M: Significant association of RNF213 p.R4810K, a moyamoya
susceptibility variant, with coronary artery disease. PLoS One.
12:e01756492017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Silveira de Souza VV, Soares Torres F,
Hochhegger B, Watte G, Sartori G, Lucchese F and Azambuja Gonçalves
B: Performance of ultra-low-dose CT for the evaluation of coronary
calcification: A direct comparison with coronary calcium score.
Clin Radiol. 72:745–750. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Raman SV and Zareba KM: Coronary artery
disease testing: Past, present, and future. JACC Cardiovasc
Imaging. 16:285–297. 2017.
|
|
7
|
Verna EC: Non-alcoholic fatty liver
disease and non-alcoholic steatohepatitis in patients with HIV.
Lancet Gastroenterol Hepatol. 2:211–223. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Degasperi E and Colombo M: Distinctive
features of hepatocellular carcinoma in non-alcoholic fatty liver
disease. Lancet Gastroenterol Hepatol. 2:156–164. 2017.PubMed/NCBI
|
|
9
|
Maurice JB, Patel A, Scott AJ, Patel K,
Thursz M and Lemoine M: Prevalence and risk factors of
non-alcoholic fatty liver disease in HIV-monoinfection: A
systematic review and meta-analysis. AIDS. 12:487–491. 2017.
|
|
10
|
Sandri A, Petersen RH, Decaluwé H, Moons
J, Ferguson MK, Hansen HJ and Brunelli A: Coronary artery disease
is associated with an increased mortality rate following
video-assisted thoracoscopic lobectomy. J Thorac Cardiovasc Surg.
154:352–357. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Schmidt B, Frölich S, Dragano N, Frank M,
Eisele L, Pechlivanis S, Forstner AJ, Nöthen MM, Mahabadi AA, Erbel
R, et al: Socioeconomic status interacts with the genetic effect of
a chromosome 9p21.3 common variant to influence coronary artery
calcification and incident coronary events in the Heinz Nixdorf
Recall study (risk factors, evaluation of coronary calcium, and
lifestyle). Circ Cardiovasc Genet. 10:e0014412017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ebell MH: PCI has more benefits and harms
than CABG for selected patients with left main coronary artery
disease. Am Fam Physician. 95:455–456. 2017.PubMed/NCBI
|
|
13
|
Kodama R, Muraki S, Iidaka T, Oka H,
Teraguchi M, Kagotani R, Asai Y, Hashizume H, Yoshida M, Kawaguchi
H, et al: Serum levels of matrix metalloproteinase-3 and
autoantibodies related to rheumatoid arthritis in the general
Japanese population and their association with osteoporosis and
osteoarthritis: The ROAD study. J Bone Miner Metab. 6:435–447.
2017.
|
|
14
|
Gudbrandsdottir S, Ghanima W, Nielsen CH,
Feng X, Hasselbalch HC and Bussel J: Effect of
thrombopoietin-receptor agonists on circulating cytokine and
chemokine levels in patients with primary immune thrombocytopenia
(ITP). Platelets. 28:478–483. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yoo HJ, Hwang SY, Choi JH, Lee HJ, Chung
HS, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, et al: Association of
leukocyte cell-derived chemotaxin 2 (LECT2) with NAFLD, metabolic
syndrome, and atherosclerosis. PLoS One. 12:e01747172017.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Napoleão P, Potapova E and Moleirinho S:
Soluble CD40 ligand profiles in patients with septic shock. Clin
Hemorheol Microcirc. 9:25–32. 2014.
|
|
17
|
Ma S, Chen X, Wang L and Wei Y: Repairing
effects of ICAM-1-expressing mesenchymal stem cells in mice with
autoimmune thyroiditis. Exp Ther Med. 7:25–32. 2012.
|
|
18
|
Abo-Hagar HH, Abo-Elezz AA, Mehrez M,
Mabrouk MM and Elshora OA: Diagnostic efficacy of serum amyloid A
protein and soluble intercellular adhesion molecule 1 in pediatric
ventilator-associated pneumonia. J Intensive Care Med.
83:8850666177025982017. View Article : Google Scholar
|
|
19
|
Walker DG, Lue LF, Tang TM and Adler CH:
Changes in CD200 and intercellular adhesion molecule-1 (ICAM-1)
levels in brains of Lewy body disorder cases are associated with
amounts of Alzheimer's pathology not α-synuclein pathology.
Neurobiol Aging. 15:97–110. 2013.
|
|
20
|
Mahmoodi K, Kamali K and Karami E: Plasma
concentration, genetic variation, and gene expression levels of
matrix metalloproteinase 9 in Iranian patients with coronary artery
disease. J Res Med Sci. 4:328–335. 2010.
|