Introduction
Chronic renal failure is a kind of clinical syndrome
originated from chronic renal diseases. China ranks in chronic
renal disease, and according to a survey of epidemics, the
incidence of chronic renal disease is more than 10% (1,2).
Although the damaged renal function in renal failure patients
cannot be reversed, effective ameliorations can be gained via
effecatious treatment, which can prolong the survival time and
improve the quality life of patients (3).
Currently, persistent dialysis remains the main
method for the treatment of chronic renal failure. Nevertheless
patients are susceptible to the complications of microinflammation,
disorders in immune functions, and secondary infections after
long-term dialysis. The combination treatment of traditional
Chinese medicine (TCM) and Western medicine has been widely
recognized as the major treatment, and the rational application of
TCM combined with dialysis, not only delays the onset of renal
failure and increases the efficacy of dialysis, but also decreases
inflammation and enhances immune functions, thereby improving the
life quality of patients (4,5).
In the present study, renal failure patients
undergoing dialysis received the combination therapy of Western
medicine and treatment of astrogaloside, and the results can be
considered as reliable evidence for improving the long-term
survival rate and life quality of patients using this method.
Materials and methods
General material
We randomly selected 92 renal failure patients
receiving maintenance dialysis who were admitted to the Dezhou
Peaple's Hospital (Shandong, China) for treatment between May, 2015
and April, 2016. These patients were randomly divided into the
control (n=46) and observation (n=46) groups. Inclusion criteria
for the study were: i) Patients who met the criteria in the
Clinical Practice Guidelines for Chronic Kidney Disease stipulated
by the National Kidney Foundation (6); ii) patients who received regular
dialysis for >3 months; iii) patients with a serum creatinine
level of <177 µmol/l and urine volume ≥200 ml; and iv) patients
who signed the written informed consent. Exclusion criteria were:
i) Patients who were complicated with severe diseases in heart,
brain or liver, or with mental diseases; ii) patients with a
medication history, such as glucocorticoid or cytotoxic drugs, or
were in gestation or lactation period. Comparisons of general
material between the two groups showed no statistically significant
difference (P>0.05) (Table
I).
 | Table I.General material of subjects. |
Table I.
General material of subjects.
| Item | Control group
(n=46) | Observation group
(n=46) | t/χ2 | P-value |
|---|
| Sex
(male/female) | 26/20 | 28/18 | 0.179 | 0.672 |
| Age (year) | 30–60 | 30–65 |
|
|
| Average age
(year) | 45.36±5.69 | 46.85±5.78 | 1.246 | 0.216 |
| Disease course
(month) | 52.62±7.46 | 52.25±7.37 | 0.239 | 0.811 |
| Total cholesterol
(mmol/l) | 5.72±0.84 | 5.81±0.85 | 0.511 | 0.611 |
| Triglyceride
(mmol/l) | 2.78±1.04 | 2.82±0.83 | 0.204 | 0.839 |
| Body mass index (BMI,
kg/m2) | 23.43±3.27 | 22.87±3.58 | 0.783 | 0.435 |
| Systolic pressure
(mmHg) | 113.35±6.46 | 112.94±6.35 | 0.307 | 0.759 |
| Diastolic pressure
(mmHg) | 73.72±3.83 | 74.34±4.76 | 0.668 | 0.493 |
Regular treatment
Pressures of patients in the two groups were
strictly controlled using drugs, such as β2 receptor blockers and
calcium antagonist. Additionally, the diet of patients was under
strict supervision, whereby patients received the high-quality
protein diet according to the criteria of 0.8–1.2 g/kg•day, and
corrections for electrolyte disturbance and imbalance between acid
and base were carried out.
Hemodialysis for treatment
Patients in the two groups persistently received
regular hemodialysis, using the hemodialysis machine manufactured
by Braun Co., Ltd. (Melsungen, Germany). During hemodialysis, the
volume of blood flow was set as 250 ml/min, while the volume of
reverse osmosis water and bicarbonate dialysing fluid was set as
500 ml/min, and the polysulfone membrane was used as the dialysis
membrane (area of 1.2–1.5 m2). Each week, the patients
received hemodialysis three times (4 h/time) with the
low-molecular-weight heparin as the anticoagulant.
Combination therapy of TCM and Western
medicine
Patients in the control group only received the
dialysis as treatment, while those in the observation group
additionally received treatment using astrogaloside, in which
Astragalus Injection (Shanghai Xinya Pharmaceutical Gaoyou
Co., Ltd.; Chinese drug approval no. Z32021256) was administered
via intravenous injection with the dose set as 10–20 ml/time and
injection rate as 30 gtt/min. Treatment lasted 6 months.
Detection of indexes
Before treatment and after 6 months since treatment,
we detected the indexes of patients using the following apparatus:
Flow cytometer (BD Biosciences, San Jose, CA, USA); automatic
multifunctional microplate reader (Thermo Fisher Scientific,
Shanghai, China); auto-balancing centrifuge (Beijing Medical
Centrifuge Factory, Beijing, China); and low-temperature
refrigerator (Sanyo, Tokyo, Japan). The reagents used in this study
included the hs-CRP, human serum IL-6, human serum IL-17 and human
serum TNF-α kits, which were all produced by Adlitteram Diagnostic
Laboratories (San Diego, CA, USA). Rabbit monoclonal antibodies of
CD3 (cat no. ab16669), CD4 (cat no. ab133616) and CD8 (cat no.
ab4055) (all from Shanghai Biotechnology Co., Ltd., Shanghai,
China) were also used. Fasting venous blood (3 ml) was drawn from
patients in the two groups, and separated for the extraction of
serum. CD3, CD4 and CD8 antibodies were then added into the serum
for 30 min of incubation at 4°C in the dark, and a flow cytometer
(BD Biosciences) was used to detect and calculate the
CD4+/CD8+ ratio. Detection was carried out
via an enzyme-linked immunosorbent assay (ELISA) in strict
accordance with the instructions of the hs-CRP, IL-6, IL-17 and
TNF-α kits. After 15 min of incubation at 20°C in the dark, 50 µl
stop buffer was added followed by reading the optical density (OD)
value at a wavelength of 450 nm for 15 min using the microplate
reader. Concentrations of hs-CRP, IL-6, IL-17 and TNF-α were then
calculated.
Evaluation indexes
Using the TCM symptom integral, the symptoms of
patients including insufficiency of qi and strength, lusterless
complexion, loss of appetite, and anorexia, were assessed according
to the following criteria: i) 0 point, no such symptom; ii) 1
point, occasionally but not affecting regular life and work; iii) 2
points, frequently, and slightly affecting regular life and work;
iv) 3 points, permanently, and severely affecting regular life and
work. Efficacy standard: i) Cured: After treatment, all the
symptoms disappeared with a decreased rate of symptom integral of
>90%; ii) excellently effective: After treatment, most of the
symptoms disappeared with a decreased rate of symptom integral of
>70%; iii) effective: After treatment, some of the symptoms
disappeared with a decreased rate of symptom integral of >30%;
iv) invalid: After treatment, no improvement or aggravation was
seen in clinical symptoms with a decreased rate of symptom integral
of <30%.
Variations of RRF and urine volume of patients in
both groups before and after treatment, were detected and
calculated as: RRF = [(concentration of urea nitrogen in
urine/concentration of urea nitrogen in serum); urine volume in 24
h/1440 + (concentration of creatinine in urine/concentration of
creatinine in serum); urine volume in 24 h/1440]/2. A decreased
rate of RRF was calculated as (RRF before treatment - RRF after
treatment)/observation duration. A decreased rate of urine volume
was calculated as: (urine volume before treatment - urine volume
after treatment)/observation duration.
Prior to treatment and 6 months after treatment, 3–5
ml fasting venous blood was collected from patients in the two
groups to extract the serum. The levels of hs-CRP, IL-6, IL-17 and
TNF-α in serum of patients were assayed via ELISA. Six months after
treatment, the levels of T-lymphocyte subgroups CD3+,
CD4+, CD8+ and
CD4+/CD8+ were detected using a flow
cytometer (BD Biosciences).
Statistical analysis
Statistical package for social science 19.0 (SPSS;
SPSS Inc., Chicago, IL, USA) software was used for data processing.
Measurement data were presented by mean ± standard deviation (mean
± SD), Chi-squared test and the t-test were used for comparison of
data. P<0.05 suggested that the difference had statistical
significance.
Results
Comparison of TCM symptom integral and
efficacy of patients between the two groups
After treatment, the TCM symptom integral of
patients in the observation group was (3.34±0.82), which was
significantly lower than that of the control group (4.48±1.27). The
total effective rate of the observation group was 86.96%, which was
significantly higher than that in the control group (60.87%).
Differences in comparisons were statistically significant
(P<0.05) (Tables II and III).
 | Table II.Comparison of TCM symptom integral of
patients between the two groups. |
Table II.
Comparison of TCM symptom integral of
patients between the two groups.
|
|
| TCM symptom
integral |
|---|
|
|
|
|
|---|
| Group | Case | Before treatment | After treatment | t-value | P-value |
|---|
| Observation
group | 46 | 7.36±1.22 | 3.34±0.82 | 18.548 | <0.001 |
| Control group | 46 | 7.35±1.33 | 4.48±1.27 | 10.585 | <0.001 |
| t-value |
| 0.376 | 5.115 |
|
|
| P-value |
| 0.970 | <0.001 |
|
|
 | Table III.Comparison of efficacy of patients
between the two groups (n, %). |
Table III.
Comparison of efficacy of patients
between the two groups (n, %).
| Group | N | Cured | Excellently
effective | Effective | Invalid |
|---|
| Observation
group | 46 | 21 (38.88) | 10 (30.55) | 9
(19.44) | 6
(13.04) |
| Control group | 46 | 9
(16.66) | 7
(22.22) | 12 (27.77) | 18 (39.13) |
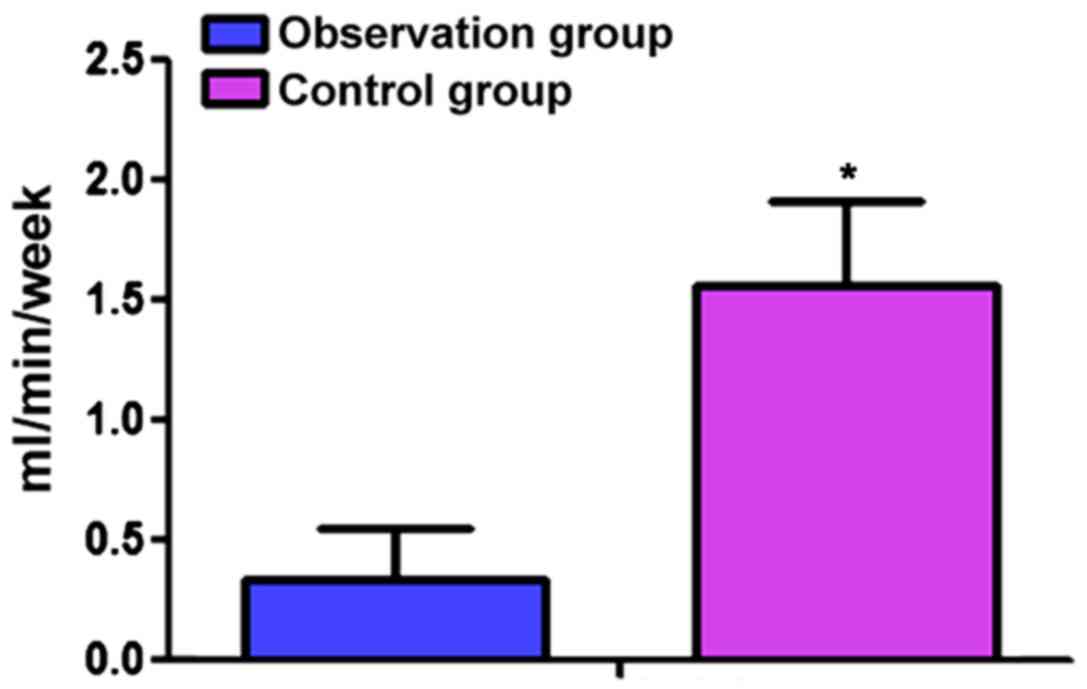
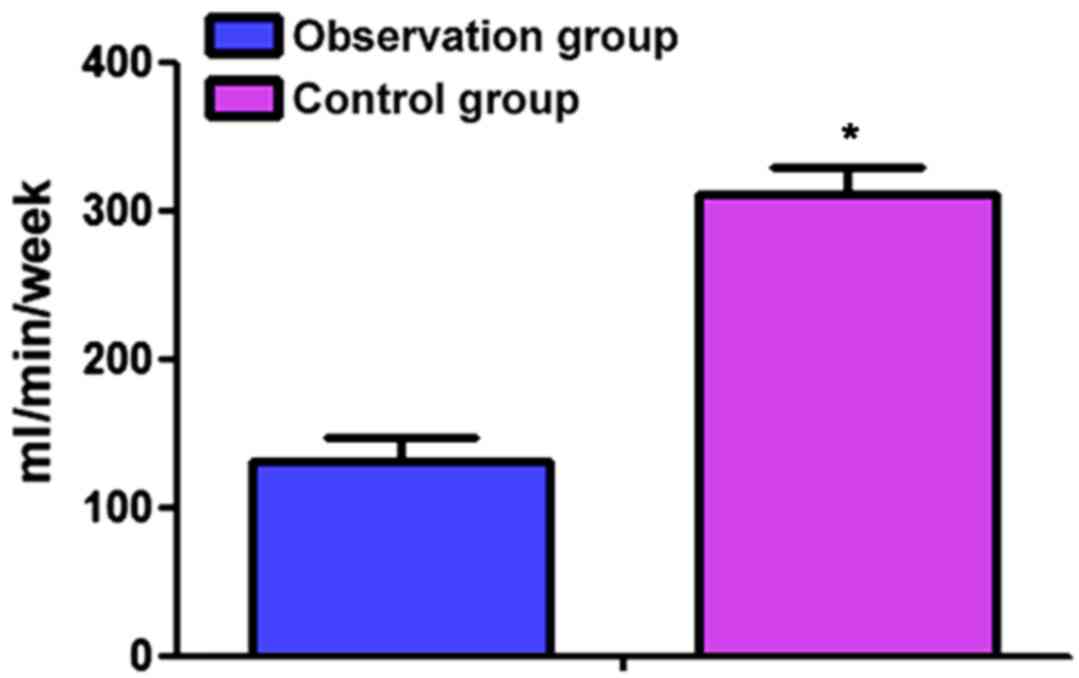
Comparisons on RRF and urine volume of
patients in the two groups before and after treatment
After treatment, RRF and urine volume of patients in
the two groups were decreased when compared with the levels before
treatment, and the differences were statistically significant
(P<0.05). Differences in the comparisons of RRF and urine volume
of patients between the two groups showed statistical significance
(P<0.05). In the observation group, the decreased rate of RRF
was 0.34±0.23 ml/min/week, and that of urine volume was 132.25±6.13
ml/week, while for patients in the control group, the decreased
rate of RRF was 1.57±0.83 ml/min/week, and that of urine volume was
312.34±8.54 ml/week. Decreased rates in RRF and urine volume of
patients in the observation group were lower than those in the
control, and the differences were statistically significant
(P<0.05) (Table IV; Figs. 1 and 2).
 | Table IV.Comparisons on RRF and urine volume of
patients in the two groups before and after treatment. |
Table IV.
Comparisons on RRF and urine volume of
patients in the two groups before and after treatment.
|
| RRF (ml/min) | Urine volume
(ml) |
|---|
|
|
|
|
|---|
| Group | Before treatment | After treatment | t-value | P-value | Before treatment | After
treatment | t-value | P-value |
|---|
| Observation
group | 2.13±1.32 | 1.14±0.98 | 4.084 | <0.001 | 589.64±21.73 | 455.41±11.62 | 36.945 | <0.001 |
| Control group | 2.12±1.28 | 0.58±0.57 | 7.454 | <0.001 | 590.56±22.64 | 317.35±11.45 | 73.037 | <0.001 |
| t-value | 0.037 | 6.940 |
|
| 0.199 | 57.399 |
|
|
| P-value | 0.971 | <0.001 |
|
| 0.843 | <0.001 |
|
|
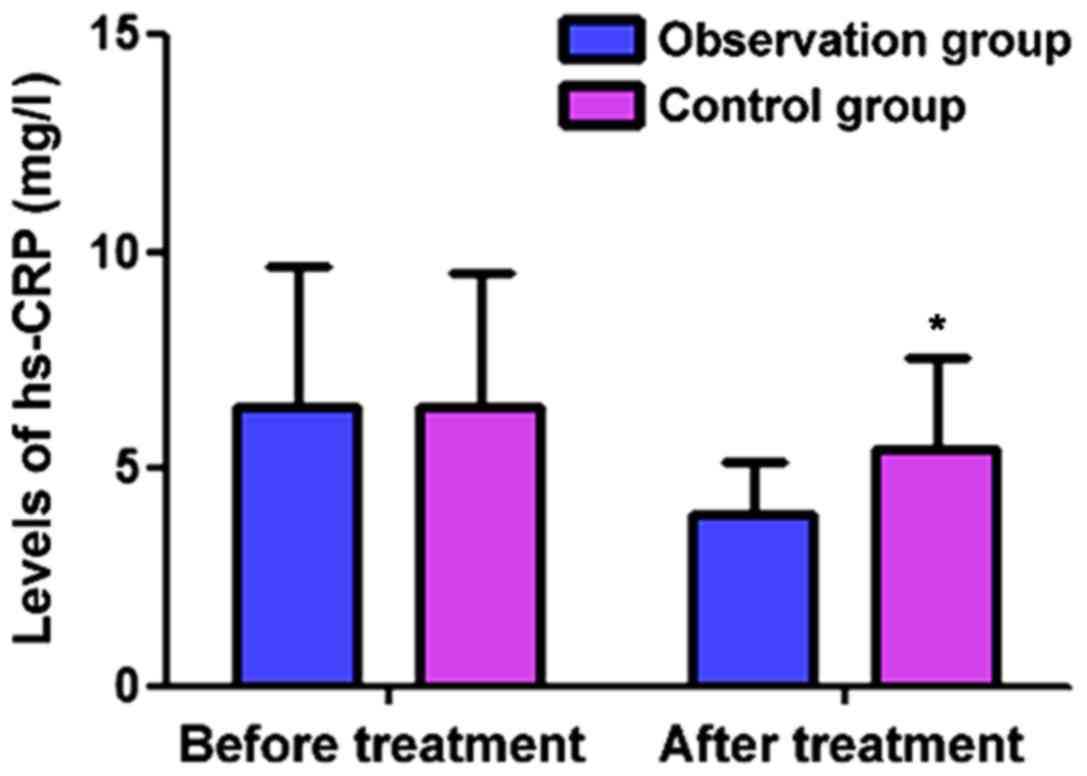
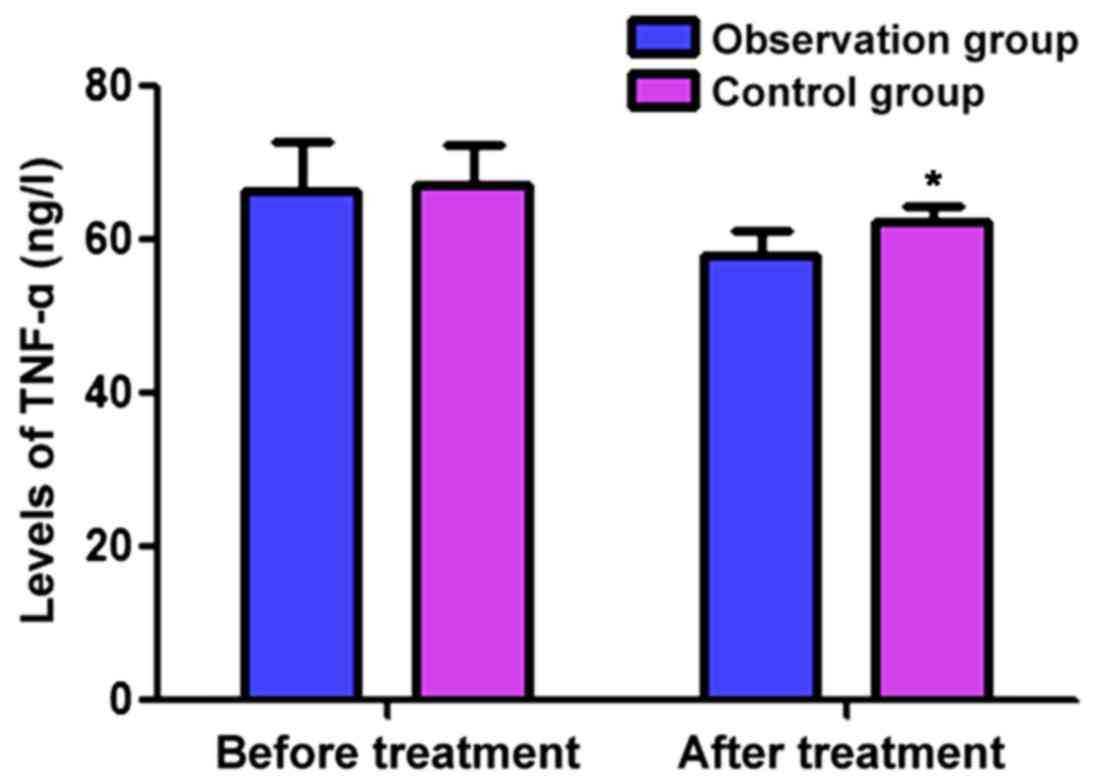
Comparisons of levels of hs-CRP, IL-6,
IL-17 and TNF-α of patients between the two groups
Prior to and after 6 months since treatment, the
levels of hs-CRP, IL-6, IL-17 and TNF-α in the observation group
were, respectively, 6.43±3.24 vs. 3.67±1.23 mg/l, 36.43±4.24 vs.
29.67±3.23 ng/l, 24.43±6.24 vs. 17.67±3.23 ng/l, and 66.43±5.24 vs.
57.67±3.23 ng/l. Before and after 6 months since treatment, the
levels of hs-CRP, IL-6, IL-17 and TNF-α in the control group were,
respectively, 6.65±3.35 vs. 5.63±2.15 mg/l, 37.24±4.36 vs.
34.58±3.74 ng/l, 24.68±6.58 vs. 21.67±3.23 ng/l and 67.36±5.17 vs.
62.85±4.43 ng/l. After treatment, the levels of CRP, IL-6, IL-17
and TNF-α of patients in the two groups were significantly
decreased compared to the levels before treatment, and at different
time points, decreases in the observation group, were more
significant than those in the control group (P<0.05) (Figs. 3–6).
Comparisons of T-cell subgroup levels
between the two groups after 6 months since treatment
The levels of CD3+, CD4+ and
CD4+/CD8+ of patients in the observation
group were higher than those in the control group, and the level of
CD8+ was lower than that in the control group
(P<0.05) (Table V).
 | Table V.Comparisons of T-cell subgroup levels
between the two groups after 6 months since treatment. |
Table V.
Comparisons of T-cell subgroup levels
between the two groups after 6 months since treatment.
| Item | Case |
CD3+ |
CD4+ |
CD8+ |
CD4+/CD8+ |
|---|
| Observation
group | 46 | 71.52±6.73 | 42.75±7.26 | 23.47±6.35 | 1.83±0.56 |
| Control group | 46 | 64.36±6.42 | 37.43±7.63 | 27.22±6.15 | 1.45±0.53 |
| t-value |
| 5.221 | 3.426 | 2.877 | 3.343 |
| P-value |
| <0.001 | 0.001 | 0.005 | 0.001 |
Discussion
General profile of renal failure. The disease course
of chronic renal failure is generally characterized by
irreversibility, progressive development and aggravation, which can
be divided into 4 phases: renal insufficiency compensation phase,
decompensation phase of chronic renal failure, renal failure phase,
and end-phase of renal failure (i.e., the phase of uremia)
(7). At present, the pathogenesis of
chronic renal failure remains unclear, and the potential
pathogenesis in kidney is injured by various pathogens, resulting
in the loss of regular functions in some nephrons. Thus, remaining
normal nephrons should compensate for the loss in functions of
normal nephrons to meet regular demand by working intensively. At
the same time, renal tubules experience continuous dilation,
resulting in an increase in the volume of crude urine with an
increse of the load in reabsorption. Renal damage, once
persistently progressing to a certain degree, may lead to
continuous decrease in renal functions, which causes glomerular
hypertrophy and platelet coagulation, thus inducing the formation
of microthrombus and facilitating glomerular sclerosis.
Consequently, glomerular permeability increases at an increment in
proteinuria, which can further damage the tubulointerstitium. Such
a vicious circle leads to excacerbation of the symptoms of renal
failure (8,9). Results of TCM, suggest renal failure is
caused by internal and external factors, with internal factors
refering to qi of kidney, while external factors refer to the
‘evil’ of pain and toxin, exogenous diseases caused by six
excessive atmospheric factors and nephrotoxic drugs. Deficiency in
qi of kidney, plus the evil of pain and toxin, and the invasion of
six external excessive atmospheric factors, and irregular excessive
administration of nephrotoxic drugs, contribute to renal failure
(10).
Treatment of renal failure. In Western medicine,
treatment methods include limitations in intake of protein and
calorically dense food, controlling high pressure within glomerulus
and systemic hypertension via dialysis, supplementation of amino
acid and renal transplantation (11). Through considerable clinical data, it
has been confirmed that the life of patients can be prolonged
through persistent and rational dialysis, and most patients can
survive for over 20 years (12).
Despite the promising efficacy, renal transplantation is bound by
difficulties involved in finding an appropriate source of kidney.
In addition, renal transplantation results in financial burden on
the patients and their family, leading to more obstacles in
spreading and promoting the application of renal transplantation
(13). However, in TCM treatment,
progression in renal failure is delayed mainly by maintaining the
essence of nephron (14). In this
study, promising efficacy was obtained through astrogaloside
medication for patients, where in the observation group, the TCM
symptom integral was significantly lower than that in the control
group, and the total effective rate was significantly higher than
that in the control group (P<0.05). This difference occured
because astrogaloside injection, which is prepared through the
extractions of astrogalus has the effects of antiperspirant,
detoxification, replenishment of qi, consolidation of exterior,
diuresis, tissue regeneration and detumescence, which can
effectively inhibit the aggregation of tubulointerstitial
extracellular matrix, improve the microcirculation, increase the
blood flow volume in kidney and protect the endothelium, thus
enhancing the efficacy of dialysis and delaying progression of the
disease (15,16). The results of this study have shown
that after 6 months since treatment, the decrease rates in RRF and
urine volume of patients in the observation group were lower than
those in the control group (P<0.05). This reduction is because
the decrease in RRF is caused by gradual asthenia in qi of kidney
according to TCM, while astrogaloside can supplement the acquired
qi of the body, thereby nourishing the congenital qi, to reach the
purpose of invigorating the qi of kidney. In addition, TCM believes
that qi can govern the blood, and astrogaloside can supplement the
qi of kidney to prevent the loss of nutrient substances in
hemodialysis, and improve the glomerular filtrating barrier to
protect the residual urine of patients (17).
Effect of astrogaloside on inflammation and immune
functions. In renal failure patients, conditions, such as
proteinuria and hyperactivity of the renin-angiotensin system, can
activate in vivo inflammatory responses, and inhibition of
the immune functions of T lymphocytes, resulting in the disorders
in immune functions (18). Results
of the present study indicated that after 6 months since treatment,
the levels of hs-CRP, IL-6, IL-17 and TNF-α of patients in the two
groups were significantly decreased when compared with the levels
before treatment, and the decrease in the observation group was
more significant than that in the control group (P<0.05).
CD3+, CD4+ and
CD4+/CD8+ levels in the observation group
were higher than those in the control group, and the
CD8+ level was lower than that in the control group
(P<0.05) because CD4+, a subgroup of the inductive T
cell, has a positive effect on immune regulation, while
astrogaloside can modulate the disorder in immune functions, thus
reducing the transformation of CD4+ to Th17 cells and
the release of inflammatory factors in serum, such as IL-17.
CD8+ belongs to a subgroup of inhibitory T cells, and
under the activated state, it can destroy and kill the affected
cells, and inhibit the activity of CD4+, which can cause
disorder in the immune functions. Thus, the
CD4+/CD8+ ratio can reflect the status of
cellular immune and immune responses of the body to a certain
degree (19). The disorder of immune
functions can induce the persistent activation of Th17 cells,
resulting in an excessive release of IL-17, which can activate the
nuclear factor-κB (NF-κB) signal pathway of the resident cells in
kidney. NF-κB can modulate the activities of hs-CRP, IL-6, IL-17
and TNF-α in inflammatory responses, which further induce high
expressions to aggravate the inflammatory responses and accelerate
the progress of renal failure (20).
Astrogaloside has distinct regulatory effects on humoral immune and
non-specific immune, and the effective anti-inflammation
capability.
In conclusion, astrogaloside can protect renal
functions, prevent renal fibrosis, delay the progression of chronic
renal failure, effectively ameliorate the status of inflammatory
responses, and modulate the immune functions of patients.
References
|
1
|
Zhang L, Wang F, Wang L, Wang W, Liu B,
Liu J, Chen M, He Q, Liao Y, Yu X, et al: Prevalence of chronic
kidney disease in China: A cross-sectional survey. Lancet.
379:815–822. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chawla LS, Eggers PW, Star RA and Kimmel
PL: Acute kidney injury and chronic kidney disease as
interconnected syndromes. N Engl J Med. 371:58–66. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Carville S, Wonderling D and Stevens P;
Guideline Development Group, : Early identification and management
of chronic kidney disease in adults: Summary of updated NICE
guidance. BMJ. 349:g45072014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Guan Y, Wu XX, Duan JL, Yin Y, Guo C, Wei
G, Wang YH, Zhu YR, Weng Y, Xi MM, et al: Effects and mechanism of
combination of Rhein and Danshensu in the treatment of chronic
kidney disease. Am J Chin Med. 43:1381–1400. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Teschke R, Zhang L, Long H, Schwarzenboeck
A, Schmidt-Taenzer W, Genthner A, Wolff A, Frenzel C, Schulze J and
Eickhoff A: Traditional Chinese medicine and herbal hepatotoxicity:
A tabular compilation of reported cases. Ann Hepatol. 14:7–19.
2015.PubMed/NCBI
|
|
6
|
KDOQI, . KDOQI Clinical Practice
Guidelines and Clinical Practice Recommendations for Diabetes and
Chronic Kidney Disease. Am J Kidney Dis. 49:12–154. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gámez-Méndez AM, Vargas-Robles H,
Arellano-Mendoza M, Cruz-Laguna E, Rios A and Escalante B: Early
stage of obesity potentiates nitric oxide reduction during the
development of renal failure. J Nephrol. 27:281–287. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ninomiya T, Perkovic V, Turnbull F, Neal
B, Barzi F, Cass A, Baigent C, Chalmers J, Li N, Woodward M, et al
Blood Pressure Lowering Treatment Trialists' Collaboration, : Blood
pressure lowering and major cardiovascular events in people with
and without chronic kidney disease: Meta-analysis of randomised
controlled trials. BMJ. 347:f56802013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Huang SH, Filler G and Lindsay RM:
Residual renal function calculated from serum cystatin C
measurements and knowledge of the weekly standard Kt/V urea. Perit
Dial Int. 32:102–104. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li JY, Yu JS, Hu WH, Du YJ and Liu XY:
Study on the characteristics of syndrome distribution of
malnutrition in chronic renal failure in traditional Chinese
medicine. World J Integr Trad West Med. 724–726. 2009.
|
|
11
|
Coresh J and Jafar TH: Disparities in
worldwide treatment of kidney failure. Lancet. 385:1926–1928. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nistor I, Palmer SC, Craig JC, Saglimbene
V, Vecchio M, Covic A and Strippoli GF: Convective versus diffusive
dialysis therapies for chronic kidney failure: An updated
systematic review of randomized controlled trials. Am J Kidney Dis.
63:954–967. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pihlstrøm H, Mjøen G, Dahle DO, Pilz S,
Midtvedt K, März W, Abedini S, Holme I, Fellström B, Jardine A, et
al: Symmetric dimethylarginine as predictor of graft loss and
all-cause mortality in renal transplant recipients.
Transplantation. 98:1219–1225. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gao H, Wang T and Yu RH: A cohort study on
delaying the progress of chronic renal failure mainly with Modified
Shenqi Dihuang Decoction. Zhongguo Zhong Xi Yi Jie He Za Zhi.
32:39–42. 2012.(In Chinese). PubMed/NCBI
|
|
15
|
Lv L, Wu SY, Wang GF, Zhang JJ, Pang JX,
Liu ZQ, Xu W, Wu SG and Rao JJ: Effect of astragaloside IV on
hepatic glucose-regulating enzymes in diabetic mice induced by a
high-fat diet and streptozotocin. Phytother Res. 24:219–224.
2010.PubMed/NCBI
|
|
16
|
Gui D, Guo Y, Wang F, Liu W, Chen J, Chen
Y, Huang J and Wang N: Astragaloside IV, a novel antioxidant,
prevents glucose-induced podocyte apoptosis in vitro and in vivo.
PLoS One. 7:e398242012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Qi W, Niu J, Qin Q, Qiao Z and Gu Y:
Astragaloside IV attenuates glycated albumin-induced
epithelial-to-mesenchymal transition by inhibiting oxidative stress
in renal proximal tubular cells. Cell Stress Chaperones.
19:105–114. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Norouzi J, Yadollahpour A, Mirbagheri SA,
Mazdeh MM and Hosseini SA: Predicting renal failure progression in
chronic kidney disease using integrated intelligent fuzzy expert
system. Comput Math Methods Med. 2016:60808142016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Moutaftsi M, Tscharke DC, Vaughan K,
Koelle DM, Stern L, Calvo-Calle M, Ennis F, Terajima M, Sutter G,
Crotty S, et al: Uncovering the interplay between CD8, CD4 and
antibody responses to complex pathogens. Future Microbiol.
5:221–239. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Noack M and Miossec P: Th17 and regulatory
T cell balance in autoimmune and inflammatory diseases. Autoimmun
Rev. 13:668–677. 2014. View Article : Google Scholar : PubMed/NCBI
|