Introduction
The composite repair material, such as metallic,
ceramic and resin material, as well as glass-ionomer cement, is one
of the numerous achievements in the research on modern biomaterials
(1,2); its biocompatibility is so good that it
is comparable to biological tissues, providing great convenience
for the mechanical property, in situ immobilization and
beautiful outlook of the prostheses (3). However, when these materials are
utilized for dental restoration treatment in current clinical
practices, phenomena such as abnormal hyperplasia, swelling and
aching, and increased secretion at gingival crevice often occur in
the gingiva adjacent to the repair materials (4,5).
Therefore, searching for safe and effective dental restorative
materials has become an urgent issue that needs to be addressed. In
this research, the novel nano-composite resin researched and
developed by the College of Materials Science and Engineering,
Nanjing University (Nanjing, China) was applied and compared with
conventional silver amalgam, glass-ionomer cement and nichrome to
study the efficacy and cytotoxicity in clinical patients, and to
determine the safety and effect of novel nano-composite resin
material.
Patients and methods
Clinical data
One hundred and ninety-two patients (240 diseased
teeth), who received dental restoration in the Department of
Stomatology of Xuzhou Stomatology Hospital (Xuzhou, China) from
March 2014 to March 2015, were selected and randomly divided into
four groups, with 60 teeth in each group. With regard to different
dental restorative materials applied, the groups were called silver
amalgam group, glass-ionomer cement group, nichrome group and novel
nano-composite resin group, respectively. The novel nano-composite
resin material was researched and developed by the College of
Materials Science and Engineering, Nanjing University, and the
glass-ionomer cement, silver amalgam and nichrome materials were
purchased from Shanghai Huifeng Medical Instrument Co., Ltd.
(Shanghai, China).
Inclusion criteria of participants: i) patients with
at least one defect tooth after oral examination, on which dental
restoration needed to be performed; and ii) after root canal
therapy, patients without apparent periodontal pain, percussion
pain and shadow at the tooth root as well as notable widening
around the root through X-ray examination (6). The side effects and complications of
the patients were evaluated through follow-up at 1 month and 2
years later. Informed consent was signed by all the patients or the
guardians. The study was approved by the Ethics Committee of Xuzhou
Stomatology Hospital.
Preparation of water extracts
Four kinds of materials (silver amalgam,
glass-ionomer cement, nichrome and novel nano-composite resin) were
made into round pieces with a diameter of 10 mm and thickness of 1
mm, respectively, followed by polishing, ultrasonic cleaning,
disinfection with 75% alcohol and overnight ultraviolet radiation;
later, 1 piece of each kind was placed in a 6-well plate for cell
culture. According to China's national standard GB/T16886.521997
(‘Biological evaluation criteria for medical devices - Part 5:
Tests for in vitro cytotoxicity’), the ratio of the surface
area of the material to the volume of the extraction medium should
be 0.5–6 cm2/ml (7). In
this study, this ratio was 1 cm2/ml. Extract was DMEM
containing 5% fetal bovine serum. Based on previous studies, 6-well
plate was put in an incubator at 37°C and incubated for 1 week
(8). In negative control group, DMEM
containing 5% fetal bovine serum, without any treatment, was
adopted.
Cell culture
Human fibroblast cell line L-929 was purchased from
the Cell Bank of the American Type Culture Collection (ATCC;
Manassas, VA, USA). Cell culture was conducted in the high-glucose
DMEM containing 10% fetal bovine serum, to which 100 µg/ml
streptomycin and 100 IU/ml penicillin were added. The cell culture
flask was placed in an incubator containing 5% CO2 at
37°C with a humidity of 95%.
Detection of the expression of
apoptosis-related indexes [B-cell lymphoma-2 (Bcl-2) and
Bcl-2-associated X protein (Bax)] via reverse transcription
quantitative polymerase chain reaction (RT-qPCR)
After the cells were cultured in the four kinds of
water extracts for 24 h, respectively, RNeasy kit (Qiagen GmbH,
Hilden, Germany) was used to extract the total messenger RNA
(mRNA). Total mRNA (1.0 µg) was synthesized into complementary DNA
(cDNA) using the reverse transcription kit (SuperScript®
VILO™ cDNA Synthesis Kit and Master Mix; Thermo Fisher Scientific,
Inc., Waltham, MA, USA). The expression of Bax and Bcl-2 was
detected via the qRT-PCR kit (Guangzhou FulenGen Co., Ltd.,
Guangdong, China) and fluorescence-based RT-qPCR instrument (Thermo
Fisher Scientific, Inc.). Glyceraldehyde-3-phosphate dehydrogenase
(GAPDH) was adopted as the internal control of calibration for each
sample. The formula for the relative mRNA expression of each index
was 2−ΔΔCq [ΔCq = Cq (target gene) - Cq (GAPDH)]
(9). All the primers were
synthesized by Sangon Biotech (Shanghai) Co., Ltd (Shanghai,
China). The corresponding primer sequences are shown in Table I.
 | Table I.Primer sequences for RT-qPCR. |
Table I.
Primer sequences for RT-qPCR.
| Gene name | Primer sequence |
|---|
| Bax | F: 5′-3′
AGACAGGGGCCTTTTTGCTAC |
|
| R: 3′-5′
AATTCGCCGGAGACACTCG |
| Bcl-2 | F: 5′-3′
GCTACCGTCGTGACTTCGC |
|
| R: 3′-5′
CCCCACCGAACTCAAAGAAGG |
| GAPDH | F: 5′-3′
TGACTTCAACAGCGACACCCA |
|
| R: 3′-5′
CACCCTGTTGCTGTAGCCAAA |
Detection of the expression of
apoptosis-related indexes (Bcl-2 and Bax) via western blotting
After culturing in the four kinds of water extracts
for 24 h, respectively, the cells were lysed on ice with
radio-immunoprecipitation assay (RIPA) lysis buffer (Beyotime
Biotechnology, Guangzhou, China) for 1 h, followed by extraction of
protein supernatant through centrifugation at 13,000 × g, 4°C for
30 min. Bicinchoninic acid (BCA) protein assay kit was applied to
measure the protein concentration, and then an appropriate amount
of loading buffer (both from Beyotime Biotechnology) was added for
denaturation at 100°C for 5 min. Every sample at an equal loading
of 40 µg, underwent electrophoresis. Later, the proteins were
transferred to the polyvinylidene fluoride (PVDF) membrane. Then
the membrane was blocked in 5% skim milk at room temperature for 1
h, followed by incubation of rabbit anti-human Bax, Bcl-2 and GAPDH
monoclonal antibodies (1:2,000; cat nos. ab32503, ab32124 and
ab181602; all from Abcam, Cambridge, UK). The membrane was washed
with Tris-buffered saline and Tween-20 (TBST), and incubated with
corresponding horseradish peroxidase-conjugated goat anti-rabbit
secondary polyclonal antibody (1:5,000; cat no. A0208; Beyotime
Biotechnology, Shanghai, China). Later, an enhanced
chemiluminescence (ECL) detection system (Bio-Rad Laboratories,
Inc., Hercules, CA, USA) was utilized to visualize the membrane,
and a gel analyzer (GraphPad Prism 5; GraphPad Software, Inc., La
Jolla, CA, USA) was applied for gray analysis. The relative content
of the target protein was the ratio of the target protein to gray
value of the corresponding internal control band.
Detection of the cell apoptosis level
via flow cytometer
The apoptosis level of cells in each group was
measured using an apoptosis kit (BD Biosciences, Franklin Lakes,
NJ, USA). After the cells were treated with different water
extracts for 48 h, the cell culture fluids were absorbed and
reserved, which were centrifuged at 850 × g for 5 min together with
the digested cells, followed by washing with phosphate-buffered
saline (PBS) and centrifugation twice. After that, the samples were
resuspended in 100 µl 1X binding buffer, to which 5 µl propidium
iodide (PI) and 5 µl Annexin V were added, followed by incubation
in the dark at room temperature for 15 min. Then the samples were
sent to the scientific research center of the hospital within 1 h
for detection by a flow cytometer (FACSCalibur; BD Biosciences,
Detroit, MI, USA). Cell apoptosis rate = early apoptosis rate +
late apoptosis rate.
Statistical methods
GraphPad Prism software (version 5.01) was used for
the statistical analysis of the experimental results. The data were
expressed as mean ± SD. The one-way analysis of variance (ANOVA)
was applied to compare the differences in indexes among multiple
groups and the least significant difference (LSD) test was the post
hoc test used. P<0.05 was considered to indicate a statistically
significant difference.
Results
General information of patients
As shown in Table
II, there was no statistically significant difference in age,
sex and tooth structure among the four groups of patients
(P>0.05).
 | Table II.General information of patients (mean
± SD). |
Table II.
General information of patients (mean
± SD).
| Items | Silver amalgam group
(n=60) | Novel nano-composite
resin group (n=60) | Glass-ionomer cement
group (n=60) | Nichrome group
(n=60) | P-value |
|---|
| Age (years) | 37.34±12.83 | 35.48±14.02 | 36.16±14.23 | 37.15±15.03 | 0.765 |
| Sex |
|
|
|
| 0.926 |
| Male | 33 | 31 | 26 | 32 |
|
|
Female | 27 | 29 | 34 | 28 |
|
| Anterior tooth
(n) | 18 | 21 | 18 | 20 | 0.738 |
| Premolar (n) | 22 | 17 | 19 | 19 | 0.815 |
| Molar (n) | 20 | 22 | 23 | 21 | 0.892 |
Patient complications at 1 month after
repair
The follow-up results at 1 month after the treatment
of the patients showed (Table III)
that in silver amalgam group, there were 3 cases of bleeding, 2
cases of local anaphylaxis, 3 cases of gingival inflammation and 2
cases of toothache; in novel nano-composite resin group, there was
1 case of bleeding and toothache, respectively; in glass-ionomer
cement group, there was 1 case of bleeding, 2 cases of gingival
inflammation and 3 cases of toothache; in nichrome group, the cases
of bleeding, local anaphylaxis, gingival inflammation, oral ulcer
and toothache were 3, 3, 1, 1 and 4, respectively. At 1 month after
the treatment there was no statistically significant difference in
the total number of diseased teeth between nichrome group and
control group (P>0.05); the total number of diseased teeth in
novel nano-composite resin group and glass-ionomer cement group was
significantly decreased compared with that in control group
(P<0.05), of which the total number of diseased teeth in novel
nano-composite resin group was smaller than that in glass-ionomer
cement group (P<0.05).
 | Table III.Patient complications at 1 month after
repair. |
Table III.
Patient complications at 1 month after
repair.
| Items | Silver amalgam group
(n=60) | Novel nano-composite
resin group (n=60) | Glass-ionomer cement
group (n=60) | Nichrome group
(n=60) |
|---|
| Bleeding | 3 | 1 | 1 | 3 |
| Local
anaphylaxis | 2 | 0 | 0 | 3 |
| Gingival
inflammation | 3 | 0 | 2 | 1 |
| Oral ulcer | 0 | 0 | 0 | 1 |
| Toothache | 2 | 1 | 3 | 4 |
| Total cases | 10 (16.7%) | 2 (3.3%) | 6 (10%) | 12 (20%) |
Conditions of diseased teeth at 2
years after repair
The follow-up results at 2 years after the treatment
of the patients showed (Table IV)
that in silver amalgam group, there were 9 cases of marginal black
line, 4 cases of secondary caries and 1 case of tooth fracture; in
novel nano-composite resin group, there was 1 case of looseness and
loss of tooth as well as 1 case of fracture; in glass-ionomer
cement group, there were 3 cases of marginal black line, 3 cases of
looseness and loss, 1 case of tooth fracture and 2 cases of dental
abnormality; in nichrome group, there were 8 cases of marginal
black line, 5 cases of secondary caries and 2 cases of looseness
and loss. At 2 years after treatment there was no statistically
significant difference in the total number of diseased teeth
between nichrome group and control group (P>0.05); the total
number of diseased teeth in novel nano-composite resin group and
glass-ionomer cement group was significantly decreased compared
with that in control group (P<0.05), of which the total number
of diseased teeth in novel nano-composite resin group was smaller
than that in glass-ionomer cement group (P<0.05).
 | Table IV.Conditions of diseased teeth at 2
years after repair. |
Table IV.
Conditions of diseased teeth at 2
years after repair.
| Items | Silver amalgam group
(n=60) | Novel nano-composite
resin group (n=60) | Glass-ionomer cement
group (n=60) | Nichrome group
(n=60) |
|---|
| Marginal black
line | 9 | 0 | 3 | 8 |
| Secondary caries | 4 | 0 | 0 | 5 |
| Looseness and
loss | 0 | 1 | 3 | 2 |
| Fracture | 1 | 1 | 1 | 0 |
| Abnormality | 0 | 0 | 2 | 0 |
| Total cases | 14 (23.3%) | 2 (3.3%) | 9 (15%) | 15 (25%) |
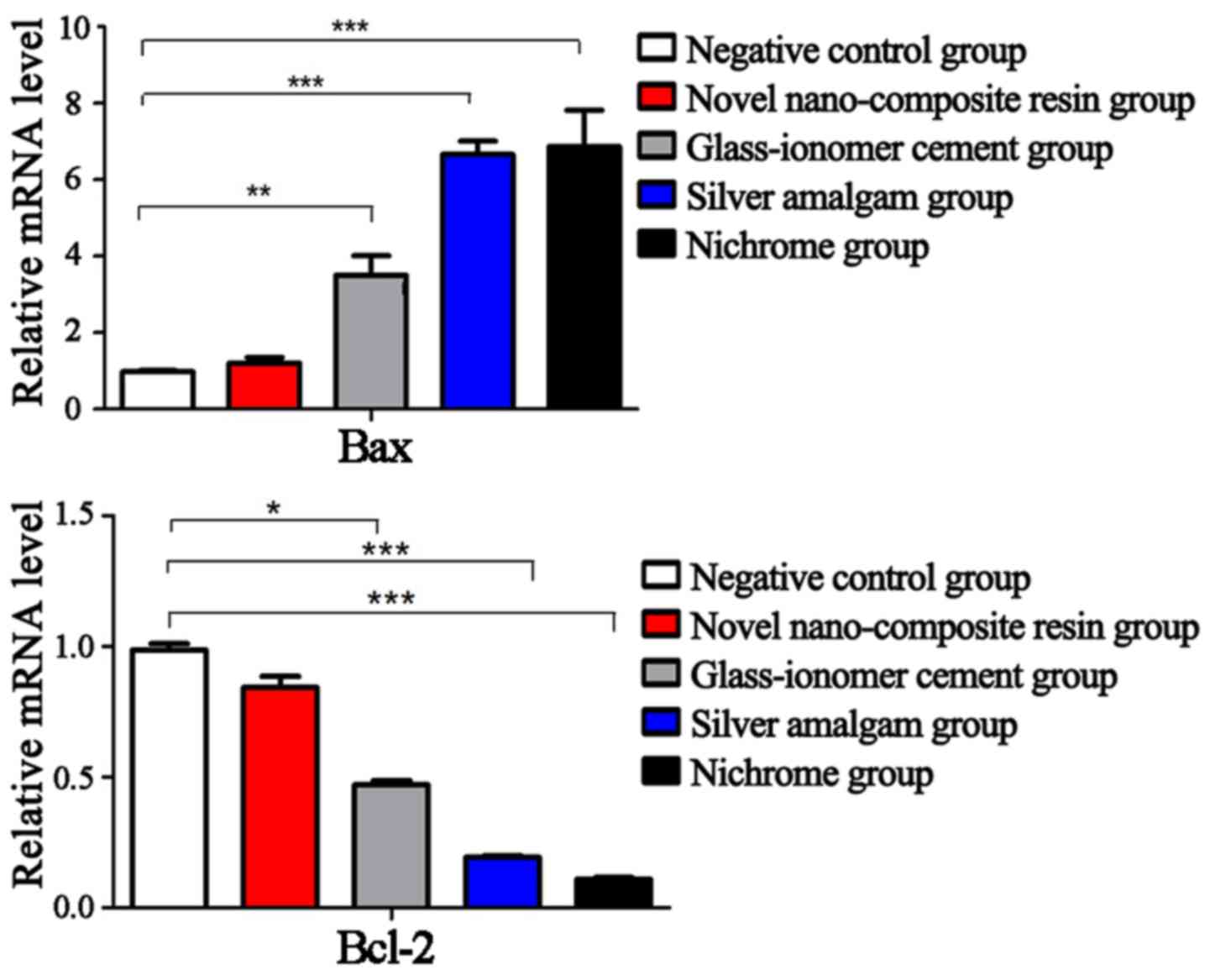
Detection of the apoptosis-related
indexes via RT-qPCR
As shown in Fig. 1,
there was no statistically significant difference in the mRNA
expression levels of Bax and Bcl-2 between the cells in novel
nano-composite resin group and negative control group (P>0.05).
Compared with those in the negative control group, the mRNA
expression levels of the pro-apoptotic index Bax were remarkably
upregulated in glass-ionomer cement group, silver amalgam group and
nichrome group, from the lowest to the highest (P<0.05).
However, the mRNA expression of the anti-apoptotic index Bcl-2 in
glass-ionomer cement group was higher than that in silver amalgam
group and nichrome group, which were notably downregulated
(P<0.05).
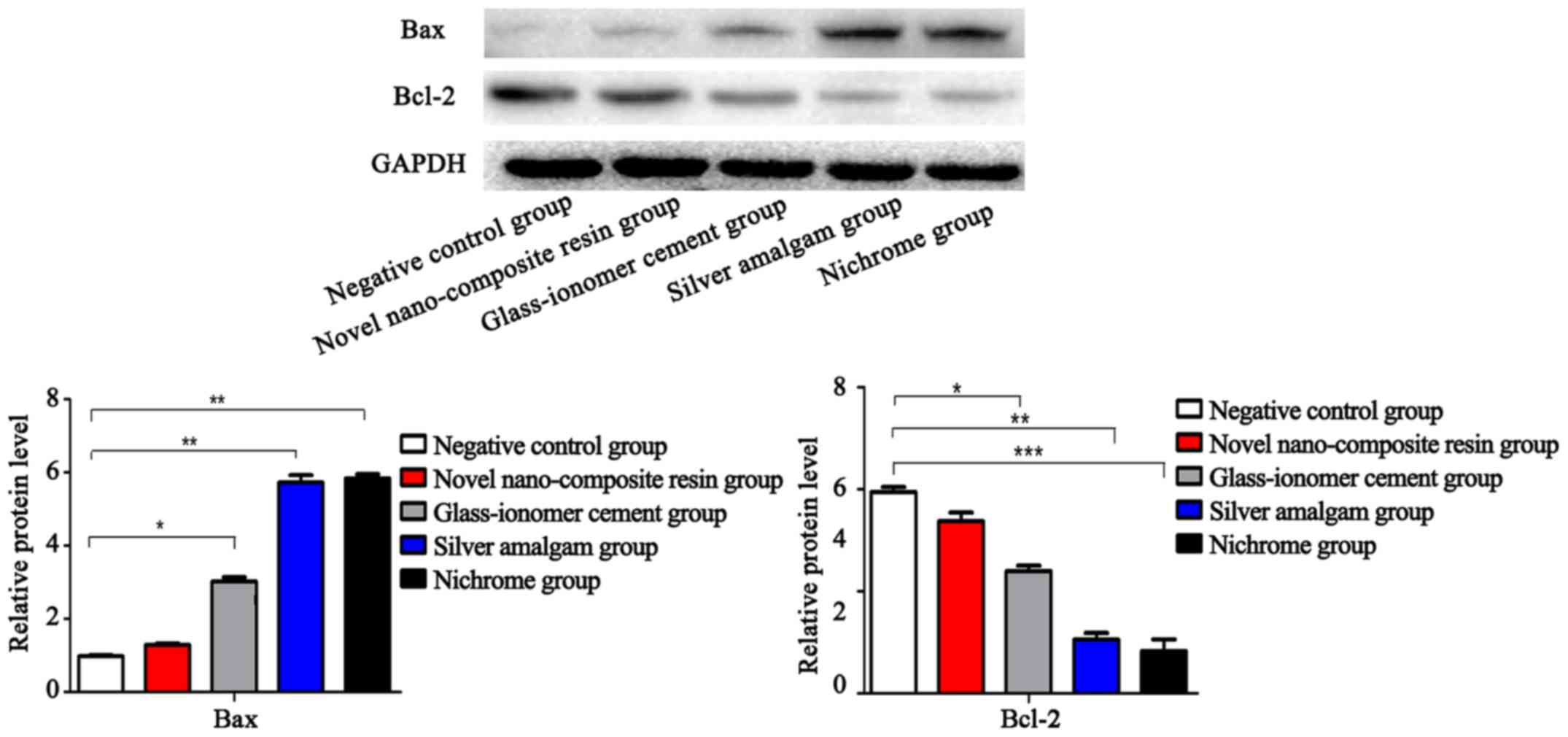
Detection of the apoptosis-related
indexes via western blotting
As indicated in Fig.
2, the protein trends and mRNA trends of Bax and Bcl-2 in the
five treatment groups of cells were the same. The differences in
the protein levels of Bax and Bcl-2 between the cells in novel
nano-composite resin group and negative control group were no
statistically significant (P>0.05). Compared with those in the
negative control group, the protein levels of the pro-apoptotic
index Bax were remarkably upregulated in glass-ionomer cement
group, silver amalgam group and nichrome group, from the lowest to
the highest (P<0.05). However, the protein level of the
anti-apoptotic index Bcl-2 in glass-ionomer cement group was higher
than that in silver amalgam group and nichrome group, which were
notably downregulated (P<0.05).
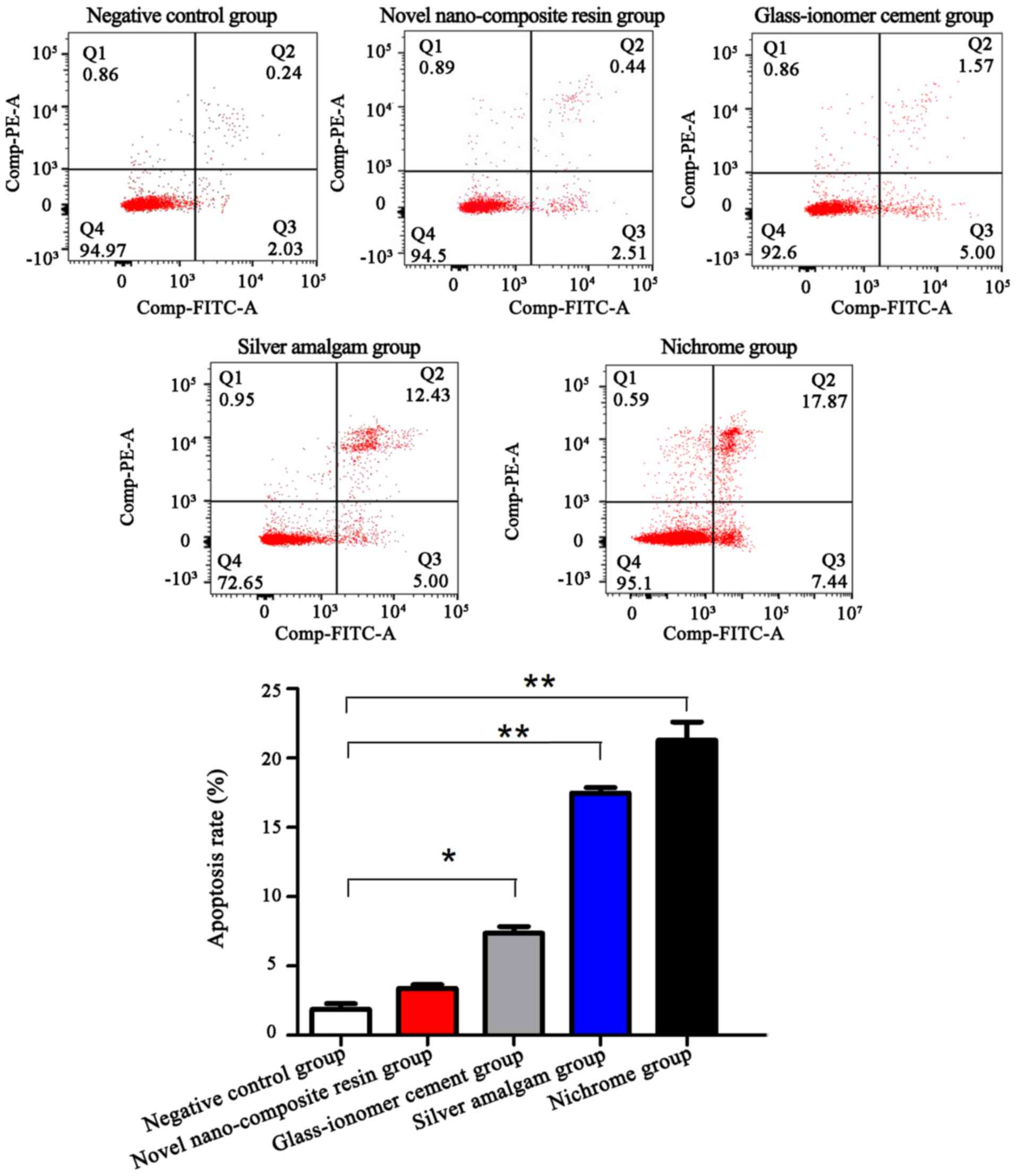
Detection of cell apoptosis via the
flow cytometer
The Annexin V/PI double staining was applied to
label the early and late apoptotic cells. The results indicated
that the cell apoptosis level in novel nano-composite resin group
was not statistically different from that in the negative control
group (P>0.05). Compared with that in the negative control
group, the cell apoptosis level in glass-ionomer cement group,
silver amalgam group and nichrome group was increased (P<0.05)
(Fig. 3).
Discussion
Dentistry is gradually developing into a complex
biomedical discipline (10,11), and materials such as silver amalgam
and glass-ionomer cement have made great contribution to clinical
practices over the past decades (12). The color of silver amalgam is similar
to that of the teeth, so that this kind of material is still widely
used by dentists at present. Studies published so far have revealed
that silver amalgam clearly does not meet the requirements for
safety and longevity, and that the physical, chemical and
biological characteristics of the materials currently utilized in
restorative dentistry need to be re-evaluated (13). The conventional glass-ionomer cement
is made of glass (e.g., calcium-aluminosilicate glass) and
polycarbonate (propylene carbonate). These materials were once
considered as possible substitutes for silver amalgam filling due
to their good biocompatibility (14). Although the newly developed composite
materials have improved their physicochemical properties, in
vitro studies have indicated that the intrinsic toxicity of
glass-ionomer cement is still very high (15).
Firstly, the free monomers released by the
conventional dental restorative materials (glass-ionomer cement and
nichrome) are conducive to the proliferation of bacteria,
especially the microorganisms related to the formation of dental
caries, which are helpful in the occurrence of secondary caries
(16). Secondly, the cellular and
molecular mechanisms of cytotoxicity are triggered by the monomers,
which lead to dental pulp changes and marginal gingival recession
(17). Thirdly, some literature
reports have revealed that silver amalgam can cause local and
systemic anaphylaxis (18). In our
research, there were 2 cases of local anaphylaxis in silver amalgam
group.
However, the major side effect of conventional
dental restorative materials is cytotoxicity. Specifically, the
mechanism of cytotoxicity is firstly correlated with the short-term
release of free monomers in the monomer-polymer transformation
process. Relevant studies have revealed that the molecular
mechanism that involves the glutathione depletion and reactive
oxygen species (ROS) generation is the key factor for apoptosis of
dental pulp or gingiva (19–21). Rai et al identified that
glass-ionomer cement can produce cytotoxicity to human dental pulp
and gingiva cells (18).
Stanislawski et al found that some nichrome materials have
toxic effects on the primary fibroblasts of rabbit pulp (19). The study of Geurtsen et al
indicated that the release of metal ions may be a reason for silver
amalgam generating toxicity to cells in vitro (22). Consistent with these research
results, the anti-apoptotic index Bcl-2 and pro-apoptotic index Bax
were examined via western blotting. It was discovered that the
protein levels of Bcl-2 were obviously decreased in the water
extracts of glass-ionomer cement group, silver amalgam group and
nichrome group, and those of Bax were elevated. The results through
flow cytometer suggested that the water extracts of glass-ionomer
cement, silver amalgam and nichrome also significantly promoted the
apoptosis of fibroblast L-929. The patients' complications at 1
month and 2 years after the dental restoration in the three groups
were remarkably higher than those in novel nano-composite resin
group; however, the water extract from novel nano-composite resin
had no significant impact on the Bcl-2 and Bax protein levels of
L-929 cells, and there was no statistically significant difference
in apoptosis level of L-929 cells compared with that in negative
control group.
In addition, secondary caries is the most common
complication after dental restoration (23). Conventional resin materials shrink
during the polymerization process, leaving a space surrounded by
bacteria between the material and cavity wall, while the so-called
mixing layer even has bacteria infiltrating, which is conducive to
the occurrence of secondary caries (24,25). The
novel nano-composite resin utilized in this experiment was the
nano-repair material made of silicon dioxide and zirconium oxide
which had stable chemical properties, hard texture and luster and
quality of natural enamel. It was manifested in this experiment
that the conditions of bleeding, local anaphylaxis, gingival
inflammation, toothache, oral ulcer and other diseases at 1 month
and 2 years after the use of the novel nano-composite resin to
patients, as well as its service conditions, were superior to those
of the other three kinds of conventional materials.
In conclusion, the impacts of silver amalgam,
glass-ionomer cement, nichrome and novel nano-composite resin on
the toxicity of fibroblasts, as well as the effects of their use on
clinical patients, were mainly compared in this study. The results
showed that the novel nano-composite resin has no toxic effect on
the fibroblast L-929, and its clinical side effects are remarkably
fewer than those of conventional materials; due to these
advantages, it is worthy of application and generalization in
clinical practice.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YW and JS conceived and designed the study. YW, QM
and XT were responsible for the collection and analysis of the
patient data. JS and QM interpreted the data and drafted the
manuscript. YW revised the manuscript critically for important
intellectual content. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Xuzhou Stomatology Hospital (Xuzhou, China). Signed informed
consents were obtained from the patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wang Y, He J, Li Q and Shen J: Preparation
of sodium alginate-nanohydroxyapatite composite material for bone
repair and its biocompatibility. Hua Xi Kou Qiang Yi Xue Za Zhi.
32:27–31. 2014.(In Chinese). PubMed/NCBI
|
|
2
|
Kawajiri H, Yamanami M, Mizuno T, Kanda K,
Yaku H and Nakayama Y: Feasibility of connective tissue membrane
(bio-sheet) prepared in the body as cardiovascular repair material
as a substitute for self-pericardium. Circulation.
128:A129102013.
|
|
3
|
Croll TP, Berg JH and Donly KJ: Dental
repair material: A resin-modified glass-ionomer bioactive ionic
resin-based composite. Compend Contin Educ Dent. 36:60–65.
2015.PubMed/NCBI
|
|
4
|
Cvar JF and Ryge G: Reprint of criteria
for the clinical evaluation of dental restorative materials. 1971.
Clin Oral Investig. 9:215–232. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhou HM, Shen Y, Wang ZJ, Li L, Zheng YF,
Häkkinen L and Haapasalo M: In vitro cytotoxicity evaluation of a
novel root repair material. J Endod. 39:478–483. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sang Z, Liu ZY, Gu YD and Feng JN:
Evaluation and analysis on clinical effects of different dental
restorative materials. J Taishan Med Coll. 37:907–909. 2016.
|
|
7
|
Abedi G, Jahanshahi A, Fathi MH, Haghdost
IS and Veshkini A: Study of nano-hydroxyapatite/zirconia stabilized
with yttria in bone healing: Histopathological study in rabbit
model. Pol J Pathol. 65:40–47. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wataha JC, Nelson SK and Lockwood PE:
Elemental release from dental casting alloys into biological media
with and without protein. Dent Mater. 17:409–414. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Livak KJ and Schmittgen TD: Analysis of
relative geneexpression data using real-time quantitative PCR and
the2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Anusavice K, Shen C and Rawls HR:
Phillips' Science of Dental Materials. 12th edition. Saunders;
2012, View Article : Google Scholar
|
|
11
|
Feinberg M, Garcia LT, Polverini PJ, Fox
CH and Valachovic RW: The vital role of research funding in
preserving the oral health of the public and the dental profession.
J Am Dent Assoc. 146:355–356. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mickenautsch S: Are high-viscosity
glass-ionomer cements inferior to silver amalgam as restorative
materials for permanent posterior teeth? A Bayesian analysis. BMC
Oral Health. 15:1182015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Saghiri MA, Banava S, Sabzian MA, Gutmann
JL, Asatourian A, Ramezani GH, Garcia-Godoy F and Sheibani N:
Correlation between long-term in vivo amalgam restorations and the
presence of heavy elements in the dental pulp. J Trace Elem Med
Biol. 28:200–204. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mickenautsch S: Retention of GIC versus
Amalgam as restorations [October 06, 2015]. J Minim Inter Dent.
9:28–30. 2016.
|
|
15
|
Chen S, Mestres G, Lan WH, Xia W and
Engqvist H: In vitro cytotoxicity of dental cements on odontoblast
cells. Presented at Towards Future Regenerative Therapies TERMIS-EU
2016 Conference. (abstract P87). 2016.http://ecmconferences.org/abstracts/2016/Collection1/c1_poster.html
|
|
16
|
Kuper NK, Montagner AF, van de Sande FH,
Bronkhorst EM, Opdam NJ and Huysmans MC: Secondary caries
development in in situ gaps next to composite and amalgam. Caries
Res. 49:557–563. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
De Munck J, Van Landuyt K, Peumans M,
Poitevin A, Lambrechts P, Braem M and Van Meerbeek B: A critical
review of the durability of adhesion to tooth tissue: Methods and
results. J Dent Res. 84:118–132. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rai R, Dinakar D, Kurian SS and Bindoo YA:
Investigation of contact allergy to dental materials by patch
testing. Indian Dermatol Online J. 5:282–286. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Stanislawski L, Soheili-Majd E, Perianin A
and Goldberg M: Dental restorative biomaterials induce glutathione
depletion in cultured human gingival fibroblast: Protective effect
of N-acetyl cysteine. J Biomed Mater Res. 51:469–474. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Goldberg M, Stanislawski L, Bonte E,
Daniau X, Bonte E, Daniau X and Lasfargues JJ: Biocompatibility of
glass-ionomer cementsAdvances in Glass-Ionomer Cements. Davidson CL
and Mjör IA: 1st edition. Quintessence Publishing Co.; Chicago: pp.
103–120. 1999
|
|
21
|
Szep S, Kunkel A, Ronge K and Heidemann D:
Cytotoxicity of modern dentin adhesives - in vitro testing on
gingival fibroblasts. J Biomed Mater Res. 63:53–60. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Geurtsen W, Lehmann F, Spahl W and
Leyhausen G: Cytotoxicity of 35 dental resin composite
monomers/additives in permanent 3T3 and three human primary
fibroblast cultures. J Biomed Mater Res. 41:474–480. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Fontana M and González-Cabezas C:
Secondary caries and restoration replacement: An unresolved
problem. Compend Contin Educ Dent. 21(15–18): 21–24, 26 passim,
quiz 30. 2000.
|
|
24
|
Zhang N, Melo MA, Chen C, Liu J, Weir MD,
Bai Y and Xu HH: Development of a multifunctional adhesive system
for prevention of root caries and secondary caries. Dent Mater.
31:1119–1131. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Schwendicke F, Kern M, Blunck U, Dörfer C,
Drenck J and Paris S: Marginal integrity and secondary caries of
selectively excavated teeth in vitro. J Dent. 42:1261–1268. 2014.
View Article : Google Scholar : PubMed/NCBI
|