Introduction
Subarachnoid hemorrhage (SAH) is a severe subtype of
stroke that affects individuals at an average age of 55 years and
leads to the death of several patients (1). Rupture of an intracranial aneurysm is
the primary cause of SAH in 85% of patients. Intracranial aneurysm
is a common intracranial cerebrovascular disease. The rupture of an
intracranial aneurysm leads to SAH, with a high mortality rate of
40% (2). However, 50-80% of
patients with aneurysms in their intracranial arteries show no
symptoms. After rupture, patients commonly present with headache,
dizziness, nausea, vomiting, neck stiffness, and, in severe cases,
aphasia, hemiplegia and disturbance of consciousness. There is a
small number of reports of acute paraplegia secondary to hemorrhage
(3,4). It has also been reported that
subarachnoid hemorrhage after spinal anesthesia causes paraplegia
(5). The present case report
describes the preoperative and postoperative conditions and
postoperative recovery of a patient with acute paraplegia following
a ruptured aneurysm. The muscle strength of both lower extremities
of the patient was grade I prior to the operation and grade 0 after
the operation. After active treatment and rehabilitation exercises,
the muscle strength of the lower extremities gradually
recovered.
Case report
A 40-year-old male patient with a history of
hypertension presented to the emergency department of Peking
University People's Hospital (Beijing, China) in December 2019 with
the complaint of headache for one day, sudden onset of nausea,
vomiting and loss of consciousness for 4 h. Neurological
examination revealed a Glasgow Coma Scale (GCS) score of 14
(E3V6M5). The patient was a habitual drinker and reported that no
immediate family members had experienced any similar
cerebrovascular events. The patient had no history of trauma,
lumbar puncture or bleeding disorders. The patient was admitted to
the emergency department of Peking University People's Hospital
(Beijing, China). His blood pressure was controlled through the
infusion of urapidil hydrochloride (2-4 ml/h) and his vital signs
were stabilized using monitoring equipment and nimodipine
administration (2-4 ml/h, 14 days), as described previously
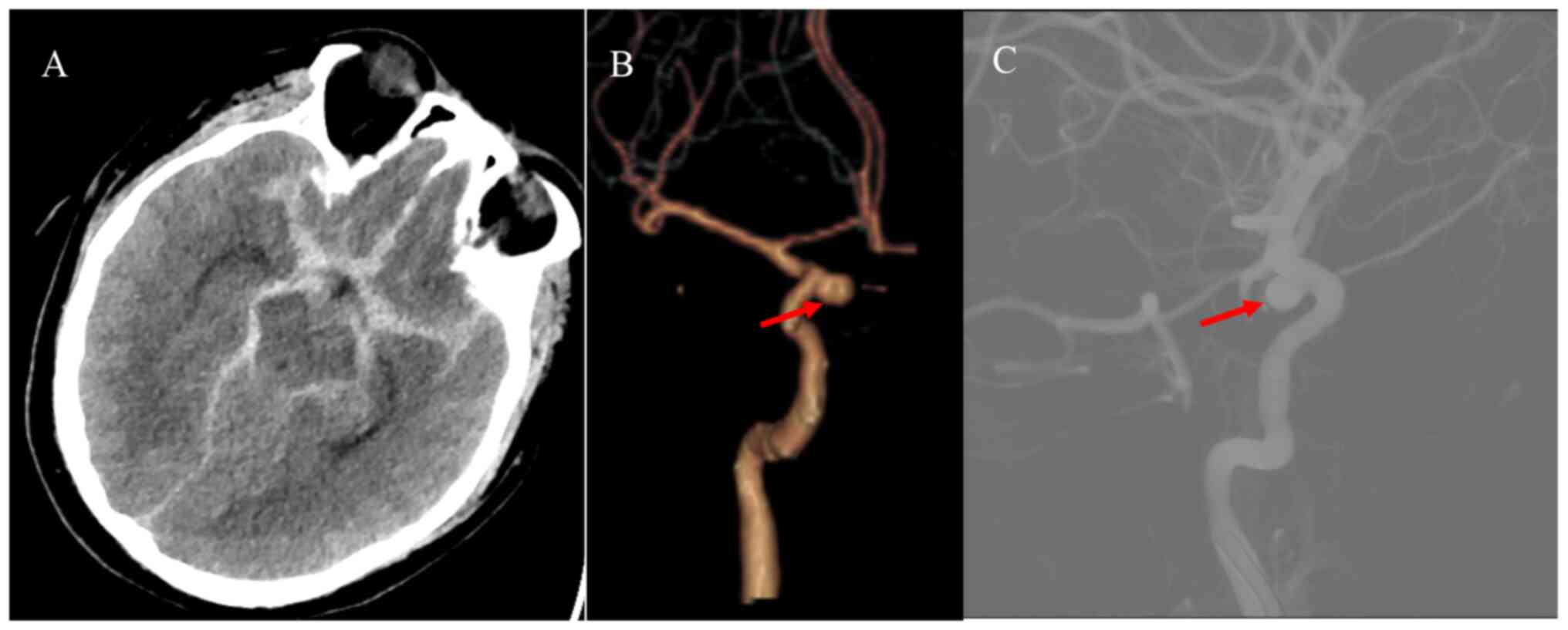
(6,7). Cranial computed tomography (CT) and
CT angiography (CTA) were performed at the earliest. Brain CT and
CTA (Fig. 1A and B) indicated diffuse SAH and an aneurysm
in the right internal carotid artery. Thus, a digital subtraction
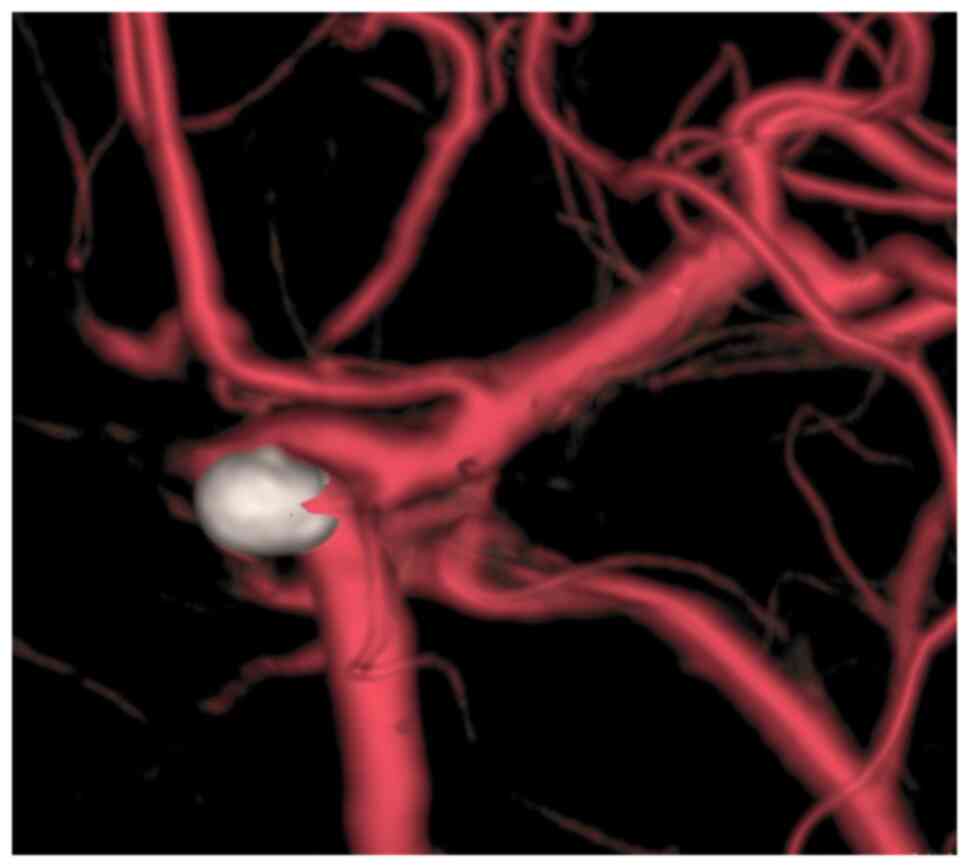
angiography (DSA) examination was scheduled immediately. DSA
revealed that the aneurysm was located in the inferior wall of the
C5 segment of the right internal carotid artery, with the following
characteristics: Aneurysm neck 3 mm and diameter 4x6 mm (Fig. 1C). The patient was placed under
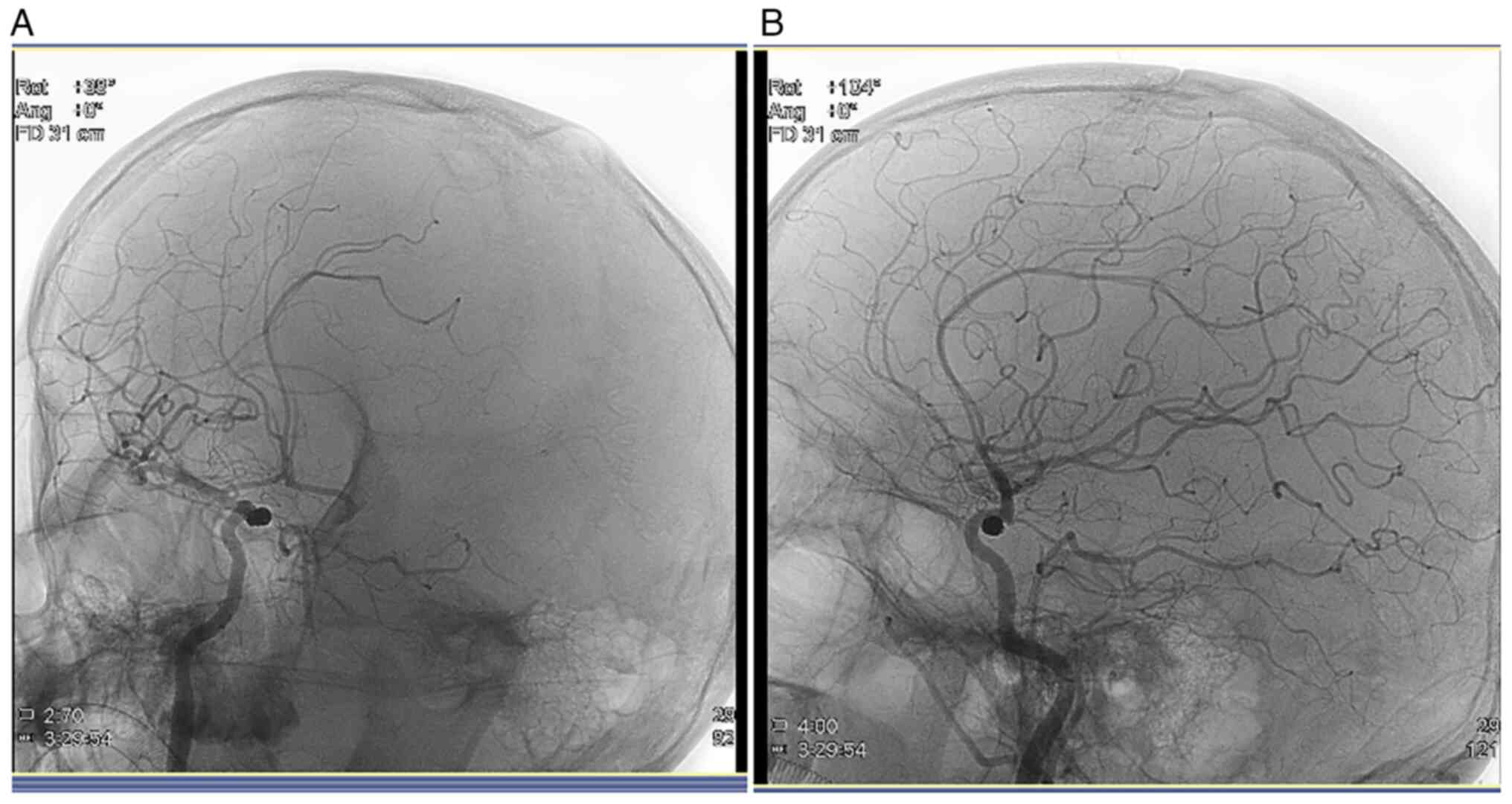
general anesthesia 9 h after the bleeding occurred and the
intracranial aneurysm was embolized using a coil interventional
embolization technique. DSA indicated that the patient's aneurysm
was densely packed without contrast retention (Fig. 2A and B). The patient was diagnosed with a right
internal carotid artery aneurysm and hypertension.
After the operation, the patient was transferred to
the intensive care unit with tracheal intubation. Following
regaining of consciousness and stability of vital signs, the
tracheal intubation was removed and the patient was transferred to
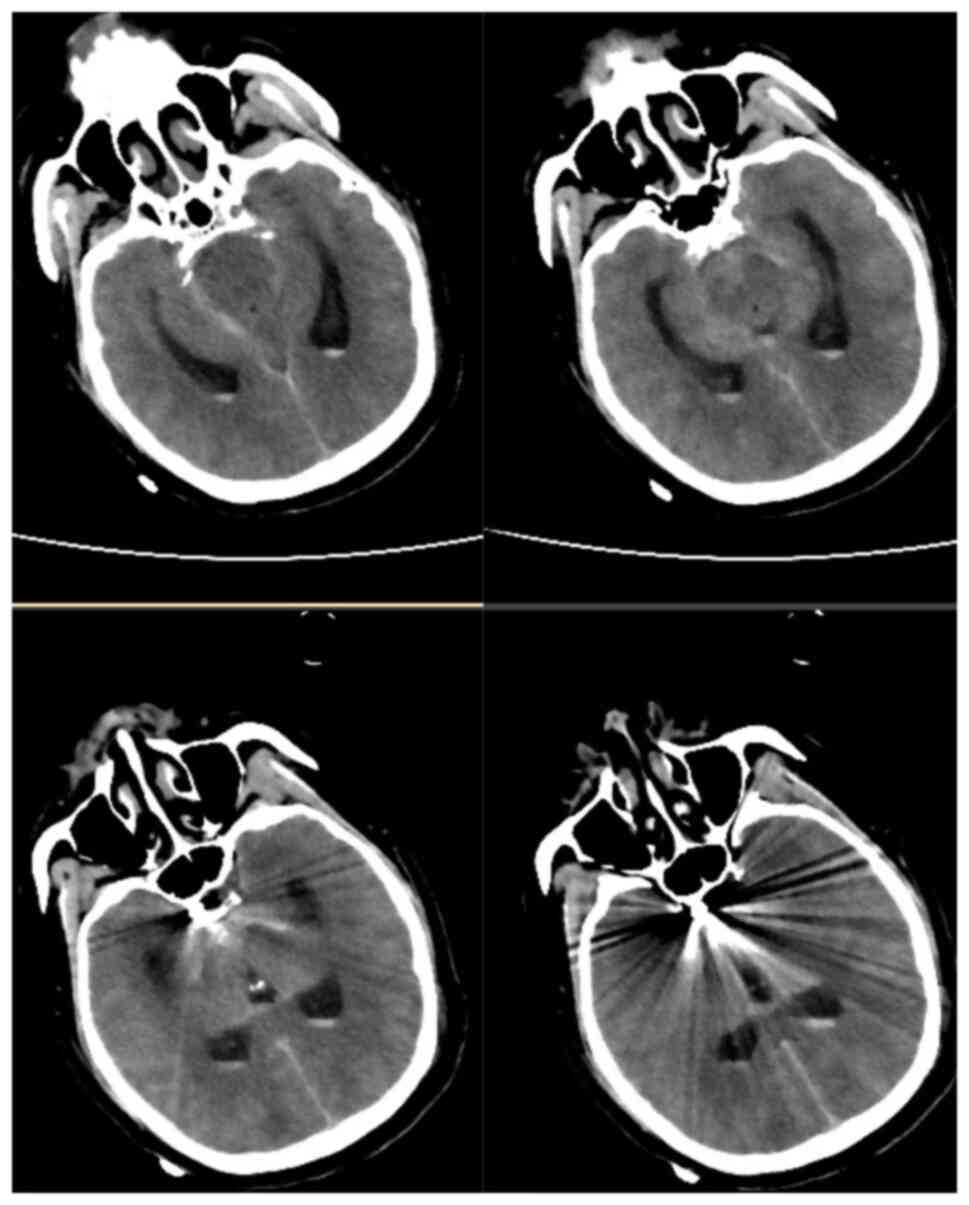
the general ward on the second day after the operation. The patient
was awake and his GCS score was 15 points. The muscle strength
assessment was using Lovett's grading approach (8), the muscle strength of both upper
limbs of the patient was normal, while the muscle strength of both
lower limbs was grade 0, but leg sensation of the patient was
normal. No new hemorrhage was detected in the re-examined head CT
area on the first day after surgery (Fig. 3). To determine whether the
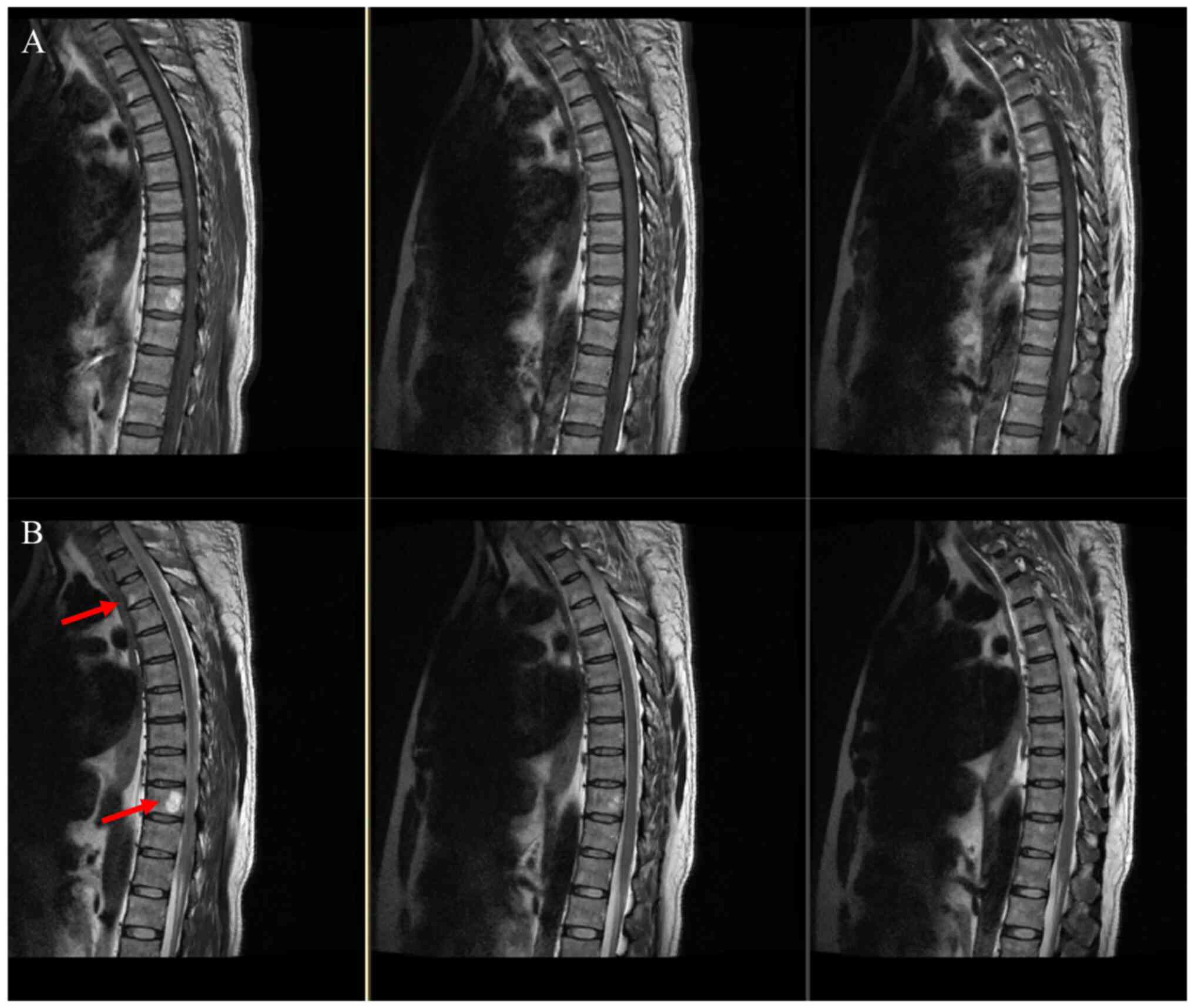
patient's paraplegia was related to the thoracolumbosacral spine,
the patient underwent thoracic spine (5 days after the surgery) and
lumbosacral spine (4 days after the surgery) magnetic resonance
imaging (MRI) examination and lower extremity venous
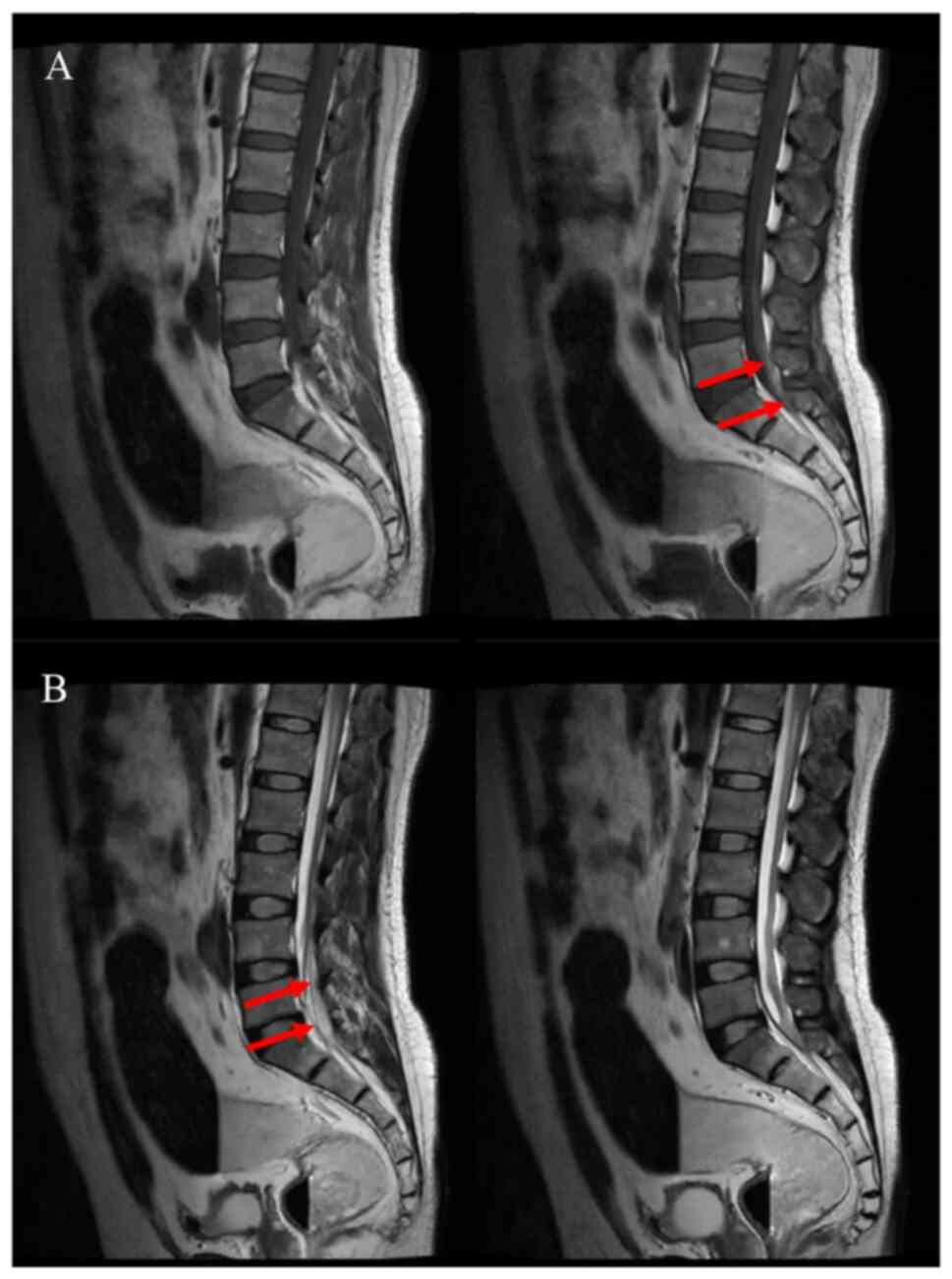
ultrasonography (10 days after the surgery). The thoracic spine MRI
scan indicated mild degeneration of the thoracic spine, mild
kyphosis of the T4/5 and T5/6 intervertebral discs and mild right
kyphosis of the T7/8 intervertebral disc. T3 and T10 vertebral
hemangiomas were suspected, as indicated by the red arrow in
Fig. 4. The lumbosacral spine MRI
scan revealed slight hematoma in the subarachnoid space below the
L2 level, as indicated by the red arrow in Fig. 5.
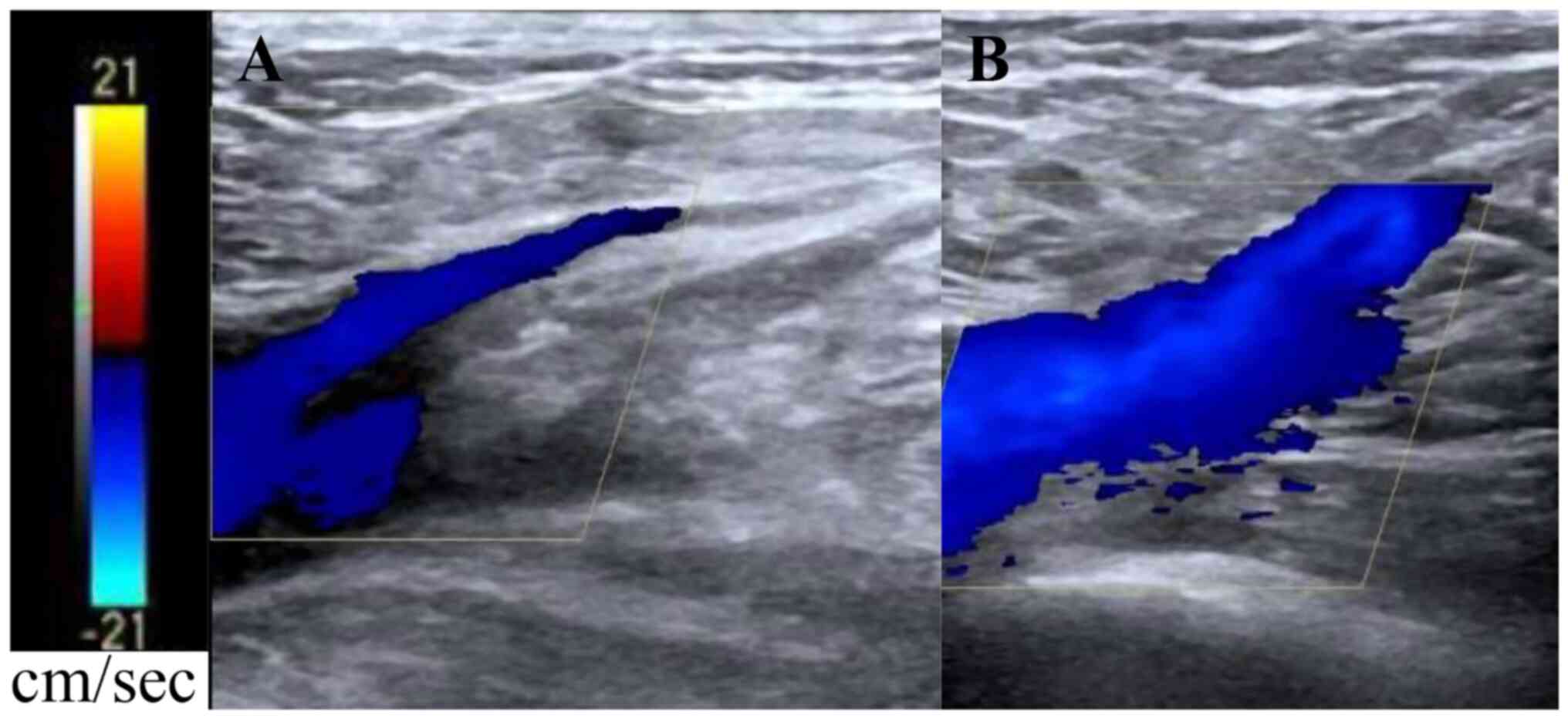
No apparent venous thrombosis was found by lower
extremity venous ultrasonography 10 days after the surgery
(Fig. 6A and B). To clear the SAH in the patient,
lumbar spinal catheter drainage was performed on the first day
after the operation. On the fourth day after the operation, the
catheter was removed and a lumbar puncture was performed once a day
for seven consecutive days to release the cerebrospinal fluid
(CSF). The CSF became transparent and clear, while the patient was
conscious and responsive. The muscle strength of both lower
extremities returned to grade II two weeks after the operation. The
patient was discharged three weeks after the operation and
transferred to a rehabilitation hospital for further treatment. The
patient was treated with cognitive and physical exercise in the
rehabilitation hospital. The muscle strength of the patient's lower
extremities was grade III one month after the operation and
returned to grade V 60 days after the operation. The patient
revisited the hospital for re-examination six months after the
operation and his nerve function was found to be normal. A two-year
follow-up cranial DSA indicated satisfactory embolization of the
aneurysm (Fig. 7).
Discussion
Acute paraplegia secondary to intracranial
aneurysmal SAH is a rare complication that, to the best of our
knowledge, is scarcely reported in the literature. Its pathogenesis
remains unclear and the incidence of paraparesis after the rupture
of an aneurysm in the anterior communicating artery is as high as
4.5-9.5% (9-11).
Spinal arachnoiditis after aneurysmal SAH may cause paralysis of
the lower extremities (12,13).
The manifestations of spinal arachnoiditis depend on the extent of
involvement and compression of the spinal cord. Common
presentations are sensory disturbances with leg pain, progressive
weakness and sphincter dysfunction. Klekamp (13) reported that subarachnoid
inflammatory disease secondary to SAH was due to blockage of the
basal cistern by blood. The accumulation of blood in the
subarachnoid space and further hemolysis may lead to meningeal
irritation and eventually arachnoiditis (14). Previous studies have reported that
the risk of developing spinal arachnoiditis is significantly
increased following SAH associated with the rupture of the
posterior inferior cerebellar artery or posterior communicating
artery aneurysms (15-17).
In these aforementioned studies, it was noted that posterior fossa
SAH secondary to spontaneous aneurysm rupture may lead to severe
spinal arachnoiditis.
Ovali et al (17) reported the case of a patient with a
ruptured aneurysm in the V4 segment of the right vertebral artery
who presented with bilateral buttock and leg numbness, as well as
severe back pain, possibly due to the diffusion of hemorrhage into
the spinal subarachnoid space. Long-term irritation of the pia
mater by blood in the subarachnoid space following a ruptured
aneurysm may lead to arachnoiditis, but the disease generally has a
longer course and persists for a long time (18). Chiang et al (4) reported the case of a patient with
paraplegia after the rupture of a basilar artery aneurysm and
subsequent hemorrhage. After placing a lumbar drainage tube, the
patient's paraplegia disappeared immediately.
The patient of the present case report was a
middle-aged overweight male and was a habitual drinker.
Consequently, atherosclerosis may be the etiology of SAH in this
patient (19,20). Furthermore, the patient had a
history of hypertension and irregular control of blood pressure may
be one of the factors for inducing aneurysm rupture (21,22).
In the present case, acute paraplegia developed immediately after
the onset of aneurysmal SAH and the possibility of hemorrhage
causing spinal vasospasm was considered. To further clarify the
reasons for the decreased muscle strength of the patient's lower
extremities, a head CT scan and lumbosacral and thoracic MRI scans
were performed after the surgery. No lesions related to the
hemorrhage were found. After lumbar cistern drainage and multiple
lumbar punctures, the blood in the subarachnoid space was cleared
and the drug nimodipine was administered immediately after the
operation for two weeks to control vasospasm. However, the muscle
strength of the patient's lower extremities recovered only to grade
II after two weeks. After active neurological rehabilitation, the
muscle strength of the patient's lower extremities returned to
grade V 60 days after the operation; thus, vasospasm combined with
chronic arachnoid inflammation cannot be excluded. The anterior
two-thirds and the posterior one-third of the spinal cord are
supplied by the anterior and posterior spinal arteries,
respectively (23). As the blood
supply is the weakest in the transition area supplied by the
superior and posterior spinal arteries, the lower thoracic spinal
cord is an area with a latent risk of developing vasogenic
paraplegia (24). This finding
corresponds to the paraplegic condition of the patient of the
present study. It may be speculated that his paraplegia may be
related to spinal cord edema caused by hypertension and increased
intracranial pressure. The symptoms of paraplegia disappeared
gradually following the reduction of spinal cord edema after the
operation.
It is worth noting that during the inpatient
physical examination, the leg circumference of the patient's right
calf was found to be significantly smaller than that on the
contralateral side. The patient's family recalled that the patient
had suffered from polio as a child, but there were no remaining
complications. In patients with polio, after injury to the anterior
horn cells of the spinal cord, muscle atrophy and weakness occur
due to the loss of motor neuron regulation in the muscle (25). To the best of your knowledge, the
present study reported on the first case of acute paraplegia after
SAH in a patient with a polio history. It may be speculated that in
vascular events, patients with polio may be more prone to spasms of
spinal vessels. The propensity for ischemic changes in the
thoracolumbar region is significantly higher, as it is mainly
supplied by a single vessel, namely the Adamkiewicz artery
(26,27). A ruptured spinal aneurysm also
causes paralysis (28). Of note,
the present study has certain limitations: Spinal angiography was
not performed to preclude paraplegia due to spinal vascular
disease.
Based on the patient's onset characteristics and the
postoperative recovery period, it may be considered that the
paraplegia of the patient was possibly associated with vasospasm of
the spinal arterioles and arachnoid inflammation. This case report
concludes that such patients have a high likelihood of recovering
from paralysis through the lumbar puncture and active
rehabilitation exercises following surgical treatment.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by Peking University
People's Hospital Research and Development Fund (grant no.
RS2021-12).
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JO and RL conceived and designed the study. JO and
JZ wrote the manuscript. BH, BW and RL reviewed and edited the
manuscript. JO and JZ acquired the data. BH, BW and ZL collated and
analyzed the data. JO and JZ confirm the authenticity of all the
raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
the Peking University People's Hospital (Beijing, China; approval
no. 2021PHE039). Written informed consent was obtained from the
patient.
Patient consent for publication
The patient provided written informed consent for
the publication of the data and the images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Macdonald RL and Schweizer TA: Spontaneous
subarachnoid haemorrhage. Lancet. 389:655–666. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
van Gijn J, Kerr RS and Rinkel GJ:
Subarachnoid haemorrhage. Lancet. 369:306–318. 2007.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Hernández-Fernández F, Cámara-González N,
Pedrosa-Jiménez MJ and Alcahut-Rodríguez C: Subarachnoid hemorrhage
due to intradural cerebral aneurysm and simultaneous spinal
subdural hematoma: Illustrative case. J Neurosurg Case Lessons.
1(CASE21123)2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Chiang YC, Lee CH, Chen WH and Tsuei YS:
Acute paraplegia after aneurysmal SAH: A case report of a rare
complication and review of the literature. World Neurosurg.
88:695.e11–695.e14. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Olivei MC, Tamanti P, Giachetti A, Nespoli
P, Berta G and Caironi P: Transient paraplegia due to subarachnoid
haemorrhage following spinal anaesthesia. Anaesth Rep. 8:40–43.
2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Etminan N and Macdonald RL: Management of
aneurysmal subarachnoid hemorrhage. Handb Clin Neurol. 140:195–228.
2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Schattlo B, Fathi AR and Fandino J:
Management of aneurysmal subarachnoid haemorrhage. Swiss Med Wkly.
144(w13934)2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lovett RW: The treatment of infantile
paralysis. J Am Med Association. LXIV(2118)1915.
|
|
9
|
Endo H, Shimizu H and Tominaga T:
Paraparesis associated with ruptured anterior cerebral artery
territory aneurysms. Surg Neurol. 64:135–139. 2005.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Greene KA, Marciano FF, Dickman CA, Coons
SW, Johnson PC, Bailes JE and Spetzler RF: Anterior communicating
artery aneurysm paraparesis syndrome: Clinical manifestations and
pathologic correlates. Neurology. 45:45–50. 1995.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Logue V: Surgery in spontaneous
subarachnoid haemorrhage; operative treatment of aneurysms on the
anterior cerebral and anterior communicating artery. Br Med J.
1:473–479. 1956.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kok AJ, Verhagen WI, Bartels RH, van Dijk
R and Prick MJ: Spinal arachnoiditis following subarachnoid
haemorrhage: report of two cases and review of the literature. Acta
Neurochir (Wien). 142:795–798. 2000.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Klekamp J: Treatment of syringomyelia
related to nontraumatic arachnoid pathologies of the spinal canal.
Neurosurgery. 3:376–389. 2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Okuno S, Touho H, Ohnishi H and Karasawa
J: Falx meningioma presenting as acute subdural hematoma: Case
report. Surg Neurol. 52:180–184. 1999.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Parker F, Aghakhani N and Tadié M:
Non-traumatic arachnoiditis and syringomyelia. A series of 32
cases. Neurochirurgie. 45 (Suppl 1):S67–S83. 1999.PubMed/NCBI(In French).
|
|
16
|
Silva N Jr, Januel AC, Sabatier J, Demonet
JF, Tall P and Cognard C: Delayed medullar syndrome after
aneurysmal subarachnoid haemorrhage. A case report of cystic
arachnoiditis! Interv Neuroradiol. 13:201–204. 2007.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ovali GY, Adam G, Çınar C, Bozkaya H,
Çallı C, Kitiş Ö and Oran İ: . Symptomatic Spinal Migration of
Subarachnoid Hemorrhage due to Ruptured Intradural Vertebral Artery
Aneurysm. Journal of Neuroimaging: Official Journal of the American
Society of Neuroimaging. 4:668–670. 2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Nakanishi K, Uchiyama T, Nakano N, Fukawa
N, Yamada K, Yabuuchi T and Kato A: Spinal syringomyelia following
subarachnoid hemorrhage. J Clin Neurosci. 19:594–597.
2012.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Can A, Castro VM, Ozdemir YH, Dagen S, Yu
S, Dligach D, Finan S, Gainer V, Shadick NA, Murphy S, et al:
Association of intracranial aneurysm rupture with smoking duration,
intensity, and cessation. Neurology. 89:1408–1415. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Can A, Castro VM, Ozdemir YH, Dagen S,
Dligach D, Finan S, Yu S, Gainer V, Shadick NA, Savova G, et al:
Alcohol consumption and aneurysmal subarachnoid hemorrhage. Transl
Stroke Res. 9:13–19. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Medetov Y, Babi A, Makhambetov Y,
Menlibayeva K, Bex T, Kaliyev A and Akshulakov S: Risk factors for
aneurysm rupture among Kazakhs: Findings from a national tertiary.
BMC Neurol. 22(357)2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Nahed BV, DiLuna ML, Morgan T, Ocal E,
Hawkins AA, Ozduman K, Kahle KT, Chamberlain A, Amar AP and Gunel
M: Hypertension, age, and location predict rupture of small
intracranial aneurysms. Neurosurgery. 57:676–683. 2005.PubMed/NCBI
|
|
23
|
Bai S, Wang Z, Zhang L, Fu H, Zhuang H,
Cao X, Liang L and Yang Y: Successful surgical treatment of
descending aorta interruption in a 29-year-old woman with acute
paraplegia and subarachnoid hemorrhage: A case report. J
Cardiothorac Surg. 10(80)2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Santillan A, Nacarino V, Greenberg E,
Riina HA, Gobin YP and Patsalides A: Vascular anatomy of the spinal
cord. J Neurointerv Surg. 4:67–74. 2012.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kosaka T, Kuroha Y, Tada M, Hasegawa A,
Tani T, Matsubara N, Koike R, Toyoshima Y and Takahashi H: A fatal
neuromuscular disease in an adult patient after poliomyelitis in
early childhood: Consideration of the pathology of post-polio
syndrome. Neuropathology. 33:93–101. 2013.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Singh U, Silver JR and Welply NC:
Hypotensive infarction of the spinal cord. Paraplegia. 32:314–322.
1994.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Verhey LH and Banwell BL: Inflammatory,
vascular, and infectious myelopathies in children. Handb Clin
Neurol. 112:999–1017. 2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Cadieux M, Tso M, Fox S and Jacobs WB:
Spontaneous spinal subarachnoid hemorrhage from a ruptured
radiculopial artery aneurysm. World Neurosurg. 145:114–118.
2021.PubMed/NCBI View Article : Google Scholar
|