Introduction
Venous thromboembolic diseases comprise pulmonary
embolism (PE) and deep venous thrombosis (DVT) (1–3);
untreated DVT may lead to a potentially fatal PE (4). DVT and PE have increasingly been
considered as a single disease, known as venous thromboembolism
(VTE) (5), and an asymptomatic PE
is present in approximately half the patients presenting with
symptomatic proximal DVT (6).
Moreover, DVT and PE share a number of risk factors, including age,
immobilization, major surgery or trauma, active cancer, pregnancy,
oral contraceptive use and hormone replacement therapy. Iliac vein
compression syndrome (IVCS) remained relatively unknown until 1957,
when May and Thurner (7)
characterized three types of intraluminal bands, or ‘spurs’ within
the compressed iliac vein that were hypothesized to be probable
risk factors for the development of left-sided iliofemoral DVT
(7).
With the advent of catheter-directed thrombolysis,
iliac vein compression has been observed to be frequently
associated with DVT following iliofemoral vein thrombolysis
(8). The management of iliofemoral
DVT remains a challenge due to the fact that the symptoms and signs
of DVT are unspecific. It has been shown that <25% of patients
with clinically suspected DVT actually have the disease (9,10),
which emphasizes the importance of accurate diagnostic strategies.
The correct diagnosis and prompt treatment are therefore crucial.
Several clinical prediction rules have been developed to simplify
and improve the diagnostic procedures for patients with suspected
DVT in a number of populations (11–15).
Diagnostic strategies based on combining pretest
probability with D-dimer measurements have been shown to be safe
and cost-effective (16), leading
to a significant reduction in the number of ultrasound examinations
(12,17,18).
As a result of the ability to acquire processed data sets with
spiral computed tomography (CT), different techniques are available
for accurate diagnosis. A series of robust and reproducible
measurements for DVT is likely to be beneficial for the
establishment of spiral CT as a clinical tool.
The aim of the present study was to assess the
optimal digital image processing and combination techniques for the
diagnosis of DVT, PE and IVCS, and to evaluate their accuracy.
Patients and methods
Patients
Although this examination was performed for accepted
clinical indications and was considered suitable for patient care,
approval was obtained from the institutional review board of the
Municipal Hospital of Taizhou (Taizhou, China). Informed consent
was obtained from each patient once the nature of the procedure had
been explained fully.
A cohort of 110 consecutive patients (47 males and
63 females; mean age, 55±9 years; range, 27–84 years) was recruited
from January 2010 to April 2012. All patients were suspected to
have lower limb deep vein thrombosis (LVT) following B-mode
ultrasonography. The patient population was composed of inpatients
and outpatients whose physicians had ordered combined pulmonary CT
and lower limb angiography, as well as indirect CT venography
(CTV), for the diagnosis of VTE. For patients with no IVCS, an
inferior vena cava filter was implanted prior to interventional
treatment in order to reduce the further risk of DVT or PE.
CT acquisition protocol
All coronary CT angiographic examinations were
performed on a 128-slice spiral CT scanner (GE LightSpeed 7.0 CT
Scanner System; GE Medical Systems, Waukesha, WI, USA). The
patients were scanned in the lateral position, with their feet
placed into the CT scanner first. On the basis of the patients’
weights, 120–150 ml (2 ml/kg) nonionic contrast medium (Optiray
350; Tyco Healthcare, Montreal, QC, Canada) was injected into the
antecubital vein at a mean flow rate of 4 ml/sec using a
high-pressure syringe. This was followed by a chaser bolus of 30 ml
saline at the same flow rate using a dual-head injector
(Stellant® D Dual Syringe CT Injection System; Medrad,
Warrendale, PA, USA). To optimize the starting time for
acquisition, a contrast agent auto-tracking technique was used
(19). A prescan was performed at
the level of the aortic root, and a circular region of interest
measuring 10 mm in diameter was placed on the ascending aorta. As
soon as the signal density in the region of interest was obtained,
image acquisition was initiated.
A spiral pulmonary CT angiography (PCTA) check was
performed, prior to a CTV being conducted 2 min later, combined
with the time-density curves (20,21).
All image data were processed by Wizard workstation (GE advantage
windows 4.0; GE Healthcare, Wood Dale, IL, USA), including
multi-planar reconstruction (MPR), maximum intensity projection
(MIP) imaging and volume rendering (VR).
These digital subtraction angiography (DSA)
techniques were used to diagnose thrombosis of the pulmonary blood
vessels, LVT and IVCS. The pulmonary subsegments and branches were
further observed by adjusting the window width and level from 40 to
80 HU (22,23). The examinations were preselected
for adequate contrast enhancement of the pulmonary arteries, which
was judged subjectively.
CT image postprocessing and results
analysis
Two groups of radiologists (experienced attending
physicians, practicing for >10 years, three in each group) read
the imaging results; the PCTA and CTV image results were read by
the radiologists in group 1, and then the postprocessing techniques
of MPR, MIP and VR were conducted for each image. The processed
images were read by the second group of radiologists. According to
the interpretation of the results, the patients were diagnosed with
thrombosis of the pulmonary blood vessels, LVT and IVCS by the
reviewers. The detection results of group 1 were considered as the
standard to assess the accuracy of the image processing in group 2.
In addition, a 12-month follow-up with PCTA and CTV was conducted
to evaluate the credibility of the diagnoses.
Results
Enhancement CT diagnosis results
The enhancement CT value of the normal pulmonary
artery in our hospital (Municipal Hospital of Taizhou) was 270±22
HU and the main pulmonary artery and its branches were uniformly
distributed on the image. The CT value of the pulmonary artery
embolism was 65±7 HU and the image showed typical filling defects
within the vascular cavity, which were clearly revealed by PCTA.
The enhancement CT value of the normal lower extremity vein was
115±11 HU, while that of the LVT was 70±7 HU. The image of the LVT
showed a filling defect.
Following the diagnostic procedure, 75 out of the
110 patients were diagnosed with LVT; IVCS was observed in 31
patients; and four patients were negative for embolisms. Out of the
75 patients diagnosed with LVT, 34 patients also presented with PE.
In the patients with IVCS, the thrombosis extended to the iliac
vein, inferior vena cava and renal vein in 10 of the 31 patients.
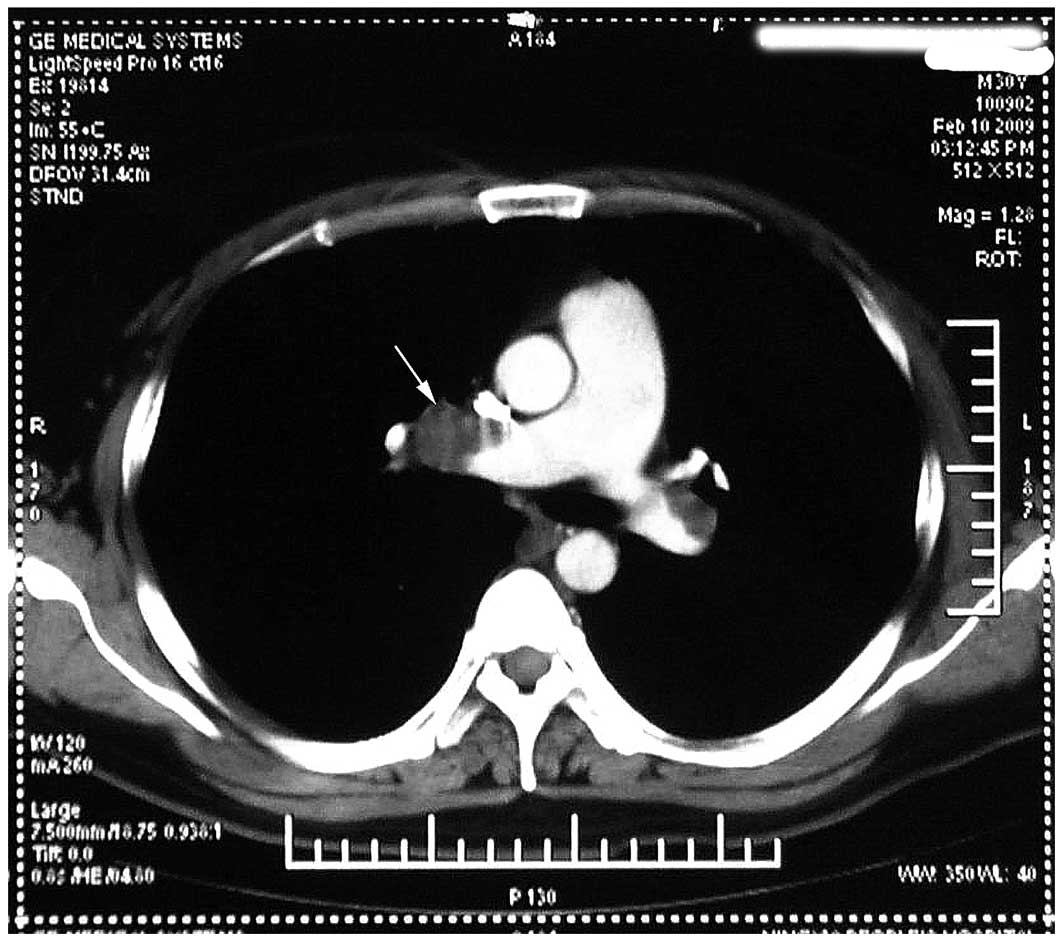
Fig. 1 shows the filling defect
within the pulmonary vascular cavity of an unprocessed CT
image.
Credibility results of the postprocessed
images
When the credibilities of the three modes of image
postprocessing were compared, as shown in Table I, compared with the VR processing
technology, MPR and MIP were more effective at showing thrombosis
in the pulmonary artery, and clearly revealed the presence and
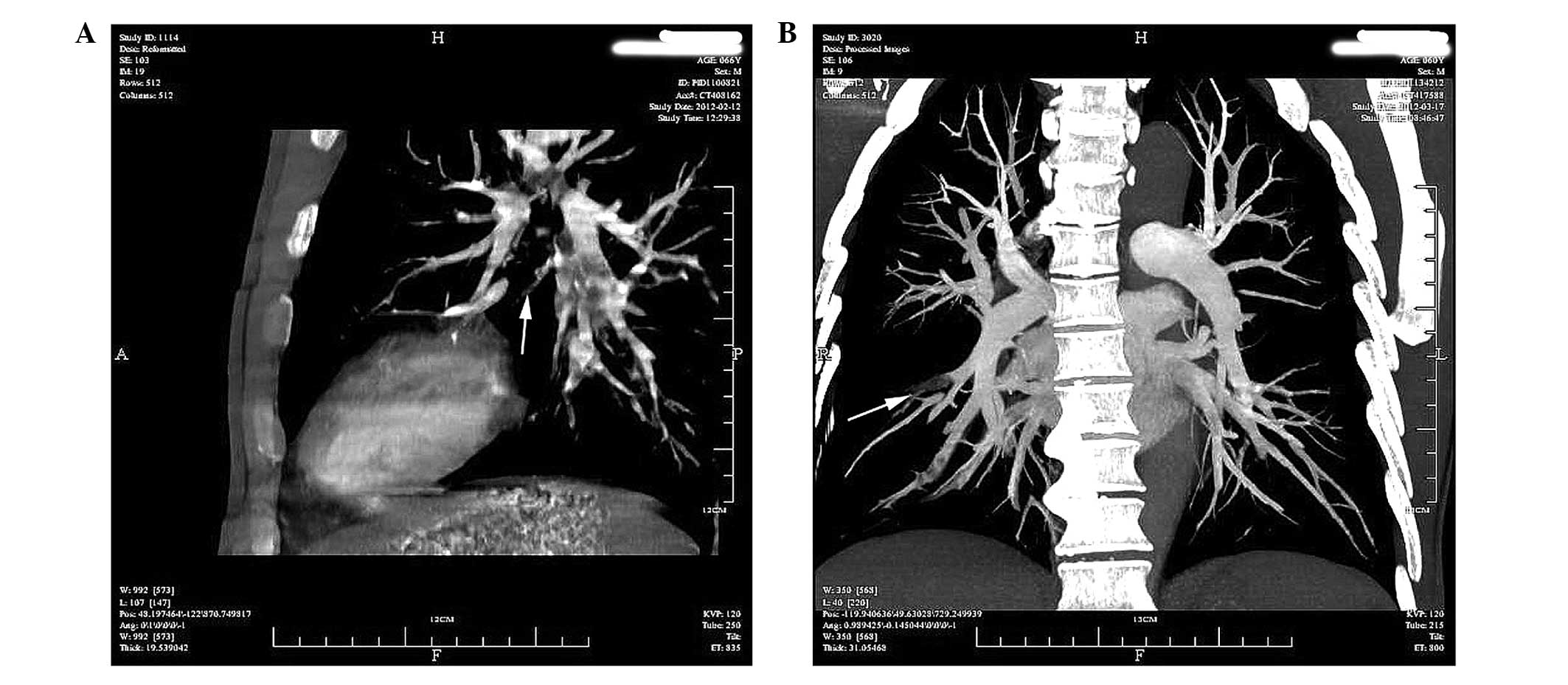
range of the thrombosis. Fig. 2
shows two MPR images of the right pulmonary artery, in which the
central artery (Fig. 2A) and lower
pulmonary branch (Fig. 2B) show
filling defects. Due to the concentration of the contrast medium,
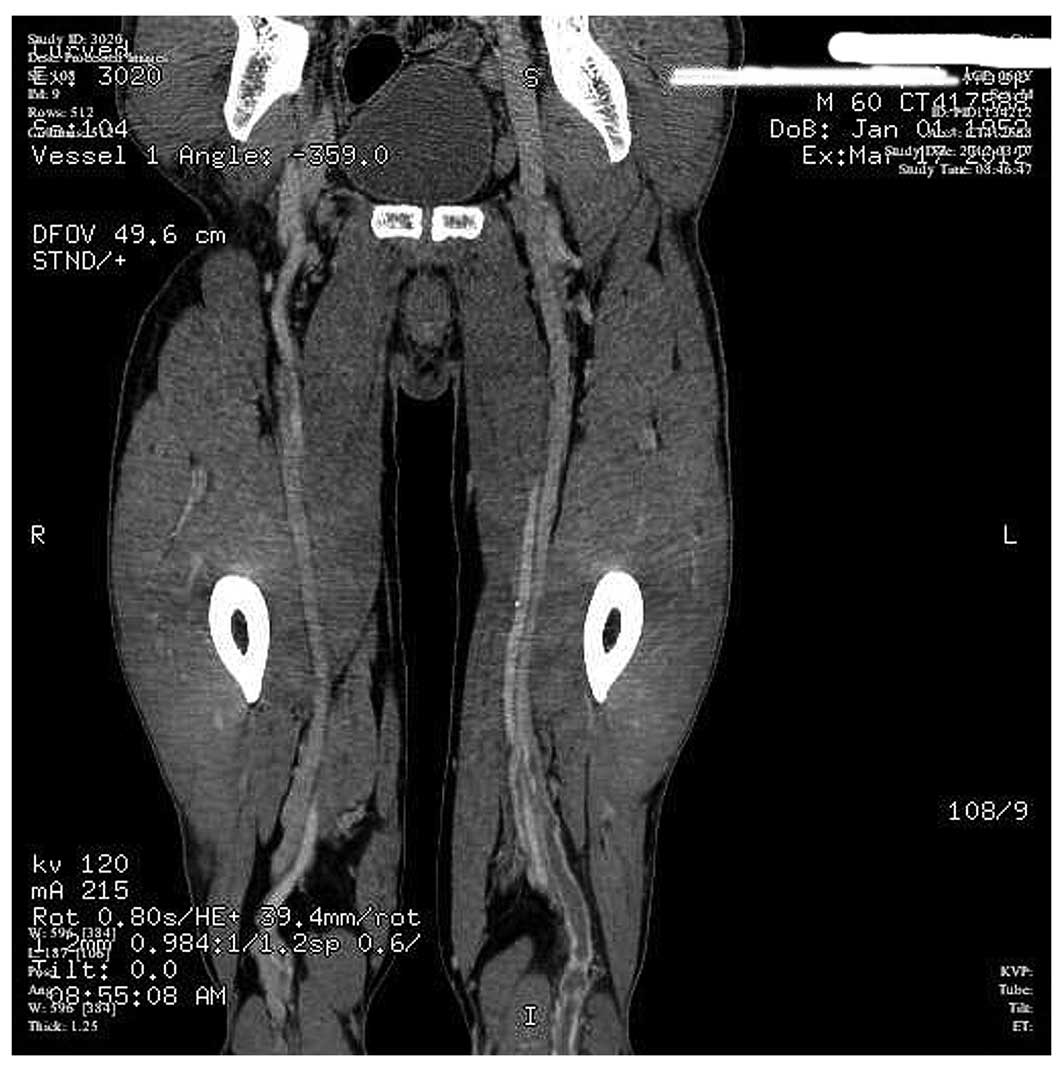
MIR and VR (Fig. 3) showed the
thrombosis image of the lower limb deep vein clearly when combined
with the original CT image.
 | Table ICredibility of diagnostic results from
postprocessed images compared with the results of direct CT in 110
patients. |
Table I
Credibility of diagnostic results from
postprocessed images compared with the results of direct CT in 110
patients.
| | Postprocessing
positive rate, n (%) | |
|---|
| |
| |
|---|
| PCTA/CTV | Condition | MPR | MIP | VR | Positive by direct
CT, na |
|---|
| PCTA | PE+LVT | 34 (100) | 34 (100) | 22 (65) | 34 |
| CTV | LVT | 41 (100) | 25 (61) | 20 (49) | 41 |
| CTV | IVCS | 31 (100) | 31 (100) | 31 (100) | 31 |
Compared with the display rate of the original CT
image (100%), the display rates of MPR, MIP and VR were 100%
(34/34), 100% (34/34) and 65% (22/34) for PE with LVT; 100%
(41/41), 61% (25/41) and 49% (20/41) for LVT alone; and 100%
(31/31), 100% (31/31) and 100% (31/31) for IVCS, respectively. MPR
was a more effective DSA technique than MIP and VR in the present
evaluation, and the difference was statistically significant
(P=0.001).
All 75 patients finished the outpatient follow-ups
12 months later, and the CT follow-up results confirmed the
diagnosed results.
Discussion
Traditional lower extremity studies that assess and
review the entire lower extremity vasculature are performed by an
ultrasound technologist. However, ultrasound examinations are not
always available and have been shown to delay the time to diagnosis
and potential treatment of a DVT by ~2 h (24,25).
The ‘one-stage’ examination for the pulmonary artery and lower limb
deep veins simultaneously, using high-speed spiral CT imaging
technology, significantly reduces the total dose of contrast agent
used. The procedure is relatively simple (pulmonary scanning time,
6 sec; time of moving patients, 5 sec; lower limb deep vein
scanning time, 15–20 sec), and offers a convenient option for
ambulatory patients.
The conventional time-delay for a PCTA inspection is
15–17 sec (26). The contrast
agent auto-tracking technology is able to correctly evaluate the
delay-time. However, the time-delay range for a lower extremity CTV
is relatively longer and measures 120–150 sec, depending on the
condition of the patients, with a delay of 150 sec in cases of
cardiac insufficiency or varicose veins of the lower extremity and
a delay of 120 sec in cases without dysfunction or varicose veins.
In the present study, the time-density curves combined with MPR
images clearly showed the LVT in the 75 diagnosed patients.
The production of near-isotropic data sets with
128-slice spiral CT has enabled the introduction and/or refinement
of numerous image processing techniques, avoiding the inherent
distortion associated with non-isotropic data. CTV of the iliac
vein is capable of effectively assessing the nature of thrombosis,
particularly for the diagnosis of IVCS. The correct diagnosis
contributes to the correct treatment, in addition to reducing
unnecessary economic burden on the patients.
The advantages of 128-layer spiral pulse CT scanning
are that it is noninvasive, scans at a high speed and generates
images simultaneously. The results of the present study
demonstrated that the diagnosis of LVT using 128-slice spiral CT
combination scanning was accurate when compared with the original
CT image. In the diagnosis of PE, the DSA techniques of MPR and MIP
showed the image clearly, while MPR also clearly displayed the
image of LVT. Combined with the original images, MIP and VR were
able to diagnose LVT efficiently, while all of the three DSA
techniques showed the images of IVCS clearly. This novel scanning
technique has significant potential to improve upon the present
diagnosis and management of patients with LVT.
References
|
1
|
Perrier A, Roy PM, Sanchez O, et al:
Multidetector-row computed tomography in suspected pulmonary
embolism. N Engl J Med. 352:1760–1768. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Elias A, Cazanave A, Elias M, et al:
Diagnostic management of pulmonary embolism using clinical
assessment, plasma D-dimer assay, complete lower limb venous
ultrasound and helical computed tomography of pulmonary arteries. A
multicentre clinical outcome study. Thromb Haemost. 93:982–988.
2005.
|
|
3
|
Wildberger JE, Mahnken AH, Das M, Küttner
A, Lell M and Günther RW: CT imaging in acute pulmonary embolism:
diagnostic strategies. Eur Radiol. 15:919–929. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Engelberger RP, Aujesky D, Calanca L,
Staeger P, Hugli O and Mazzolai L: Comparison of the diagnostic
performance of the original and modified Wells score in inpatients
and outpatients with suspected deep vein thrombosis. Thromb Res.
127:535–539. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Perrier A: Deep vein thrombosis and
pulmonary embolism: a single disease entity with different risk
factors? Chest. 118:1234–1236. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Moser KM, Fedullo PF, LitteJohn JK and
Crawford R: Frequent asymptomatic pulmonary embolism in patients
with deep venous thrombosis. JAMA. 271:223–225. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
May R and Thurner J: The cause of the
predominantly sinistral occurrence of thrombosis of the pelvic
veins. Angiology. 8:419–427. 1957. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Narayan A, Eng J, Carmi L, et al: Iliac
vein compression as risk factor for left- versus right-sided deep
venous thrombosis: case-control study. Radiology. 265:949–957.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Goodacre S, Sutton AJ and Sampson FC:
Meta-analysis: The value of clinical assessment in the diagnosis of
deep venous thrombosis. Ann Intern Med. 143:129–139. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wells PS, Owen C, Doucette S, Fergusson D
and Tran H: Does this patient have deep vein thrombosis? JAMA.
295:199–207. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Constans J, Nelzy ML, Salmi LR, et al:
Clinical prediction of lower limb deep vein thrombosis in
symptomatic hospitalized patients. Thromb Haemost. 86:985–990.
2001.PubMed/NCBI
|
|
12
|
Wells PS, Anderson DR, Rodger M, et al:
Evaluation of D-dimer in the diagnosis of suspected deep-vein
thrombosis. N Engl J Med. 349:1227–1235. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wells PS, Anderson DR, Bormanis J, et al:
Value of assessment of pretest probability of deep-vein thrombosis
in clinical management. Lancet. 350:1795–1798. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Constans J, Boutinet C, Salmi LR, et al:
Comparison of four clinical prediction scores for the diagnosis of
lower limb deep venous thrombosis in outpatients. Am J Med.
115:436–440. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Subramaniam RM, Snyder B, Heath R, Tawse F
and Sleigh J: Diagnosis of lower limb deep venous thrombosis in
emergency department patients: performance of Hamilton and modified
Wells scores. Ann Emerg Med. 48:678–685. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Perone N, Bounameaux H and Perrier A:
Comparison of four strategies for diagnosing deep vein thrombosis:
a cost-effectiveness analysis. Am J Med. 110:33–40. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Anderson DR, Kovacs MJ, Kovacs G, et al:
Combined use of clinical assessment and d-dimer to improve the
management of patients presenting to the emergency department with
suspected deep vein thrombosis (the EDITED Study). J Thromb
Haemost. 1:645–651. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schutgens RE, Ackermark P, Haas FJ, et al:
Combination of a normal D-dimer concentration and a non-high
pretest clinical probability score is a safe strategy to exclude
deep venous thrombosis. Circulation. 107:593–597. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cademartiri F, Nieman K, van der Lugt A,
et al: Intravenous contrast material administration at 16-detector
row helical CT coronary angiography: test bolus versus
bolus-tracking technique. Radiology. 233:817–823. 2004. View Article : Google Scholar
|
|
20
|
Hartmann IJ and Prokop M: Pulmonary
embolism: is multislice CT the method of choice? For Eur J Nucl Med
Mol Imaging. 32:103–107. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Schuemichen C: Pulmonary embolism: is
multislice CT the method of choice? Against Eur J Nucl Med Mol
Imaging. 32:107–112. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Johnson TR, Krauss B, Sedlmair M, et al:
Material differentiation by dual energy CT: initial experience. Eur
Radiol. 17:1510–1517. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Habis M and Paul JF: Multidetector
computed tomography of right ventricular acute myocardial
infarction. Arch Cardiovasc Dis. 103:131–132. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Frederick MG, Hertzberg BS, Kliewer MA, et
al: Can the US examination for lower extremity deep venous
thrombosis be abbreviated? A prospective study of 755 examinations.
Radiology. 199:45–47. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Theodoro D, Blaivas M, Duggal S, Snyder G
and Lucas M: Real-time B-mode ultrasound in the ED saves time in
the diagnosis of deep vein thrombosis (DVT). Am J Emerg Med.
22:197–200. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhou C, Chan HP, Sahiner B, et al:
Automatic multiscale enhancement and segmentation of pulmonary
vessels in CT pulmonary angiography images for CAD applications.
Med Phys. 34:4567–4577. 2007. View Article : Google Scholar : PubMed/NCBI
|