Introduction
Each year approximately 650,000 new cases of head
and neck carcinomas are registered and approximately 350,000 deaths
are documented. These tumours of the sinuses, oral cavity, the
pharynx and larynx (1) are almost
exclusively squamous cell carcinomas (SCC). Alcohol and tobacco
abuse are the most important risk factors (2). The 5-year survival rate, considering
all tumour stages, is approximately 60%. Due to a high incidence of
metastases hypopharyngeal carcinomas have a significantly poorer
prognosis (3). To better predict
the prognosis of cancer patients and thereby adjust the therapeutic
concept, several molecular prognostic factors are discussed in the
literature (4). Connexins are
components of gap junction (GJ) hemi channels (connexons), which
are formed by homomeric or heteromeric connexin hexamers in the
plasma membrane. Two connexons of adjacent cells can form a
GJ-channel and allow gap junctional intercellular communication
(GJIC) by promoting the passage of small molecules like ions or
second messengers (5). GJIC plays
a central role in maintaining tissue homoeostasis, cell growth
control and development (5). The
association between GJIC and an increased contact inhibition was
first described in cultured hepatoma cells (6). GJIC has a different function
depending on the stage of tumour progression. Connexins possibly
act on cell growth by controlling the expression of cell cycle
regulatory genes such as cyclin A, D1, D2, and cyclin-dependent
kinases (CDKs) through a variety of mechanisms (7). Cx43 transfected cells suppress
degradation of p27, which inhibits the enzymatic activity of CDK.
The hypophosphorylated retinoblastoma gene product (Rb) thereby
accumulates in the cell, which characterizes the G1 phase (7). The absence of GJIC can lead to an
accumulation of growth factors in the cell (6) and the suppression of contact
inhibition, resulting in cell proliferation (8). King et al described a
correlation between the endogenous Cx43 expression and an increased
growth control, showing that the growth capacity was decreased in
HeLa cells of cervical cancer (9).
Cx43 knockout in mice leads to astrocytes with altered expression
of genes associated with apoptosis, cell growth and transcription
factors (10,11) and an increased susceptibility of
mice to pulmonary neoplasia (12).
Similar results have been published for Cx26 and Cx43 expression in
mammary MDA-MB-231 cells (13).
Cx26 is responsible for contact growth inhibition in HeLa and HepG2
cells (14,15). Because Cx45 can form altered
heteromeric gap junctions in cooperation with Cx43, Cx45
overexpression may affect intercellular contacts during
carcinogenesis (16–18). Some connexin subtypes are also able
to increase the attachment of tumour cells to the stroma during
invasion and migration (7).
Therefore, they can likely promote invasion by increasing
communication with the endothelial barrier (19). Cx26 was detected in melanoma cells,
surrounding small vessel endothelia (20), in squamous cell lung carcinoma
(SCLC) and its associated lymph node metastases (21). Cx26 and Cx43 negative primary
breast cancers developed Cx26 and Cx43 positive lymph node
metastases (22). Cx43 enabled
glioma cells to interact and establish functional GJ with
astrocytes in the adult brain and facilitated direct parenchymal
invasion (23). Data on connexin
expression in OSCC are rare and conflicting observations were
reported by Ozawa et al and Villaret et al, who
described Cx26 overexpression in tissue samples of OSCC and lymph
node metastases (24,25).
In the present study we analysed in detail the
expression and subcellular localization of Cx26, Cx43 and Cx45 in
tumour epithelia of OSCC, matching oral mucosa free of dysplasia,
and lymph node metastases using a subtle immunoreactive score. We
found that the expression of Cx26 and Cx45 had no prognostic value.
Cx43 was upregulated in tumour epithelia and membrane Cx43
expression was associated with short OS.
Materials and methods
Patients
Tissue samples of 35 patients were screened and
connexin expression levels were evaluated using
immunohistochemistry. All patients suffered from a primary OSCC and
were scheduled for surgical therapy in the Department of Oral and
Maxillofacial Surgery of the University Medical Centre Goettingen
without previous radiation or chemotherapy. The initial
histopathological diagnosis was made by a separate biopsy before
tumour ablation. The extent of resection and lymph node metastases
were diagnosed histologically. Metastases of lung, liver and bone
marrow were evaluated for all patients by chest radiography,
abdominal ultrasound examination and 99mTc-MDP-scintigraphy
(Table I). Patients gave written
informed consent before they were included in this study. The study
was conducted according to the ethical standards approved by the
local ethics committee of the University of Goettingen (vote number
07/06/09).
 | Table I.The patient data. |
Table I.
The patient data.
| N | Gender | Age (years) | Death | Survival (years) | pT | AJCC stage | Localisation |
|---|
| 1 | Woman | 56 | No | 5.85 | 2 | 2 | Right |
| 2 | Woman | 62 | No | 2.32 | Tis | 0 | Median |
| 3 | Men | 77 | No | 4.98 | 2 | 2 | Left |
| 4 | Men | 60 | No | 4.64 | 2 | 2 | Right |
| 5 | Men | 61 | Yes | 1.01 | 4a | 4 | Median |
| 6 | Men | 53 | No | 6.12 | 2 | 2 | Right |
| 7 | Men | 50 | No | 4.79 | 4 | 4 | Right |
| 8 | Men | 49 | No | 4.22 | 4 | 4 | Left |
| 9 | Woman | 79 | No | 4.20 | 4 | 4 | Left |
| 10 | Men | 67 | No | 5.72 | 4 | 4 | Right |
| 11 | Men | 39 | Yes | 0.10 | 4 | 4 | Median |
| 12 | Woman | 58 | Yes | 1.44 | 4 | 4 | Median |
| 13 | Woman | 62 | Yes | 1.62 | 4 | 4 | Right |
| 14 | Men | 31 | No | 5.73 | 2 | 2 | Left |
| 15 | Men | 45 | Yes | 0.97 | 4 | 4 | Left |
| 16 | Woman | 61 | Yes | 0.06 | 4a | 4 | Left |
| 17 | Woman | 45 | Yes | 0.70 | 4a | 4 | Median |
| 18 | Men | 47 | Yes | 1.75 | 4a | 4 | Median |
| 19 | Woman | 66 | Yes | 0.64 | 4a | 4 | Left |
| 20 | Woman | 64 | Yes | 1.93 | 4a | 4 | Right |
| 21 | Men | 40 | No | 7.02 | 2 | 3 | Right |
| 22 | Men | 49 | No | 14.68 | 2 | 3 | Right |
| 23 | Woman | 64 | No | 8.94 | 2 | 4 | Left |
| 24 | Men | 71 | Yes | 1.56 | 4a | 4 | Left |
| 25 | Men | 49 | Yes | 2.13 | 4a | 4 | Right |
| 26 | Men | 70 | Yes | 3.56 | 1 | 1 | Median |
| 27 | Men | 46 | Yes | 4.94 | 1 | 1 | Median |
| 28 | Men | 52 | Yes | 1.19 | 3 | 3 | Right |
| 29 | Woman | 69 | No | 4.12 | 1 | 1 | Left |
| 30 | Men | 61 | No | 4.43 | 3 | 3 | Right |
| 31 | Men | 57 | Yes | 5.15 | 4a | 4 | Right |
| 32 | Men | 65 | Yes | 2.38 | 4a | 4 | Median |
| 33 | Men | 62 | Yes | 1.51 | 2 | 2 | Right |
| 34 | Men | 43 | No | 5.58 | 1 | 1 | Right |
| 35 | Woman | 49 | No | 6.56 | 1 | 1 | Left |
Tissue samples
Tissue samples of primary OSCC, matching oral mucosa
free of dysplasia, and associated lymph node metastasis were
obtained immediately after tumour resection, fixed in neutrally
buffered 4% formalin and embedded in paraffin. Immunohistochemical
reactions were performed on 2-μm tissue sections. The
staining procedures are summarized in Table II. Sections were counterstained
with Meyer’s haematoxylin. Two independent investigators evaluated
all tissue sections by light microscopy (Olympus, Tokyo),
considering nuclear, membrane and cytoplasmic connexin staining by
using an immunoreactive staining score (IRS). The intensity of
staining was evaluated on a graded scale (0, negative; 1, weak; 2,
intermediate; 3, strong). A total of 100% of positively stained
cells was distributed on every density. For the final IRS, the
scores of intensity and staining were multiplied and the mean value
was calculated by forming the sum of the individual products. Total
values ranged between 0 and 300. The application of the score is
demonstrated in Table III.
 | Table II.Staining protocol. |
Table II.
Staining protocol.
| Antigen | Antibody (type,
dilution) | Pre-treatment | Detection
method | Source |
|---|
| Cx26 | Rabbit, polyclonal,
1/200; 30 min | EDTA (pH 9) |
Envision-peroxidase, Dako | Abcam,
Cambridge |
| Cx43 | Rabbit, polyclonal,
1/50; 30 min | EDTA (pH 9) |
Streptavidin-alkaline phosphatase,
Dako | Cell Signalling,
Danvers |
| Cx45 | Rabbit, polyclonal,
1/100; 30 min | Citrate (pH 6) |
Streptavidin-alkaline phosphatase,
Dako | Millipore,
Temecula |
 | Table III.Calculation of the immunoreactive
scores. |
Table III.
Calculation of the immunoreactive
scores.
| Localisation
(nucleus, membrane, cytoplasm) | Staining intensity
(0, negative to 3, strong) | Percentage (%) | IRS |
|---|
| e.g.
membrane | 1 | 80 |
80+(2×15)+(3×5)=125 |
| 2 | 15 | |
| 3 | 5 | |
Statistical analysis
The influence of general clinical parameters, such
as gender, age at first diagnosis, nicotine and alcohol abuse,
limiting systemic diseases, AJCC criteria and -stages, radio- and
chemotherapy, localization of the primary tumour, extent of neck
dissection and type of reconstruction, on the overall survival time
was analysed using Cox proportional hazard regressions. The
strength of the influence was described by the hazard ratio (with
an additional 95% confidence interval). Connexin expression was
correlated with survival time using the Kruskal-Wallis test and the
associated baseline characteristics described above. The influence
of the type of tissue (oral mucosa, primary cancer, lymph node
metastasis and the subcellular localization (nucleus, cytoplasm,
plasma membrane) and their interaction with the expression of each
protein was analysed by non-parametric analysis of variance for
data with repeated measurements (26). If significant interactions were
observed, all tissue types and subcellular localization were also
compared pairwise with each other using non-parametric analysis of
variance. All tests were performed at a significance level of α=5%
using the statistical software R (version 2.15, www.r-project.org).
Results
Connexin 26
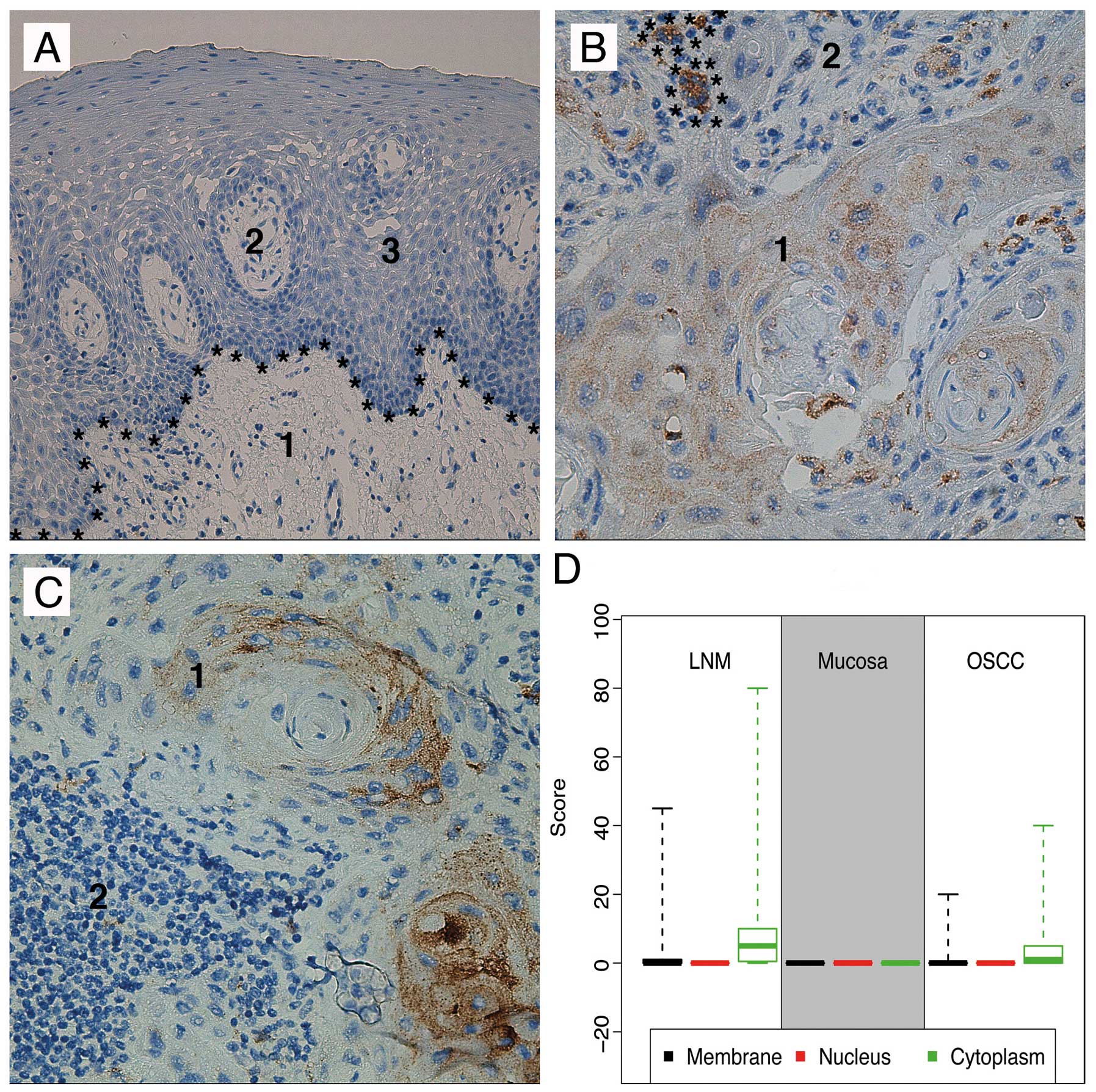
No Cx26 expression was detected in dysplasia-free
oral mucosa in any of the cellular compartments (Fig. 1A). Cx26 expression was
significantly detected in the cytoplasm and membrane of primary
OSCC (P<0.01). However, no nuclear expression was observed in
primary OSCC tissue (Fig. 1B).
Nevertheless, the signal strength was often at the lower limit of
detection. Compared to primary OSCC, cytoplasmic (P<0.01) and
membrane (P<0.01) Cx26 expression was significantly increased in
lymph node metastases (Fig. 1C).
No nuclear expression was detected in local metastases. The
morphological distributions of Cx26 in the analysed tissues are
shown in Fig. 1D. The data from
the pairwise comparisons are summarized in Tables IV and V.
 | Table IV.Pairwise comparisons of connexin
expression between the different localizations, separated by tissue
type. |
Table IV.
Pairwise comparisons of connexin
expression between the different localizations, separated by tissue
type.
| Antigen | Tissue | Cell location
comparison | P-value |
|---|
| Cx26 | LNM | Membrane vs.
nucleus | 0.13 |
| Membrane vs.
cytoplasm | <0.01 |
| Nucleus vs.
cytoplasm | <0.01 |
| Oral mucosa | Membrane vs.
nucleus | NA |
| Membrane vs.
cytoplasm | NA |
| Nucleus vs.
cytoplasm | NA |
| OSCC | Membrane vs.
nucleus | <0.01 |
| Membrane vs.
cytoplasm | <0.01 |
| Nucleus vs.
cytoplasm | <0.01 |
| Cx43 | LNM | Membrane vs.
nucleus | 0.47 |
| Membrane vs.
cytoplasm | <0.01 |
| Nucleus vs.
cytoplasm | <0.01 |
| Oral mucosa | Membrane vs.
nucleus | <0.01 |
| Membrane vs.
cytoplasm | 0.80 |
| Nucleus vs.
cytoplasm | <0.01 |
| OSCC | Membrane vs.
nucleus | <0.01 |
| Membrane vs.
cytoplasm | <0.01 |
| Nucleus vs.
cytoplasm | <0.01 |
| Cx45 | LNM | Membrane vs.
nucleus | 0.04 |
| Membrane vs.
cytoplasm | <0.01 |
| Nucleus vs.
cytoplasm | <0.01 |
| Oral mucosa | Membrane vs.
nucleus | 0.31 |
| Membrane vs.
cytoplasm | <0.01 |
| Nucleus vs.
cytoplasm | <0.01 |
| OSCC | Membrane vs.
nucleus | 0.67 |
| Membrane vs.
cytoplasm | <0.01 |
| Nucleus vs.
cytoplasm | <0.01 |
 | Table V.Pairwise comparisons of connexin
expression between the different tissue types, separated by
localizations. |
Table V.
Pairwise comparisons of connexin
expression between the different tissue types, separated by
localizations.
| Antigen | Cell location | Tissue
comparison | P-value |
|---|
| Cx26 | Membrane | LNM vs. oral
mucosa | <0.01 |
| LNM vs. OSCC | <0.01 |
| Oral mucosa vs.
OSCC | <0.01 |
| Nucleus | LNM vs. oral
mucosa | <0.01 |
| LNM vs. OSCC | <0.01 |
| Oral mucosa vs.
OSCC | NA |
| Cytoplasm | LNM vs. oral
mucosa | <0.01 |
| LNM vs. OSCC | <0.01 |
| Oral mucosa vs.
OSCC | <0.01 |
| Cx43 | Membrane | LNM vs. oral
mucosa | <0.01 |
| LNM vs. OSCC | <0.01 |
| Oral mucosa vs.
OSCC | 0.24 |
| Nucleus | LNM vs. oral
mucosa | <0.01 |
| LNM vs. OSCC | <0.01 |
| Oral mucosa vs.
OSCC | NA |
| Cytoplasm | LNM vs. oral
mucosa | <0.01 |
| LNM vs. OSCC | <0.01 |
| Oral mucosa vs.
OSCC | <0.01 |
| Cx45 | Membrane | LNM vs. oral
mucosa | <0.01 |
| LNM vs. OSCC | <0.01 |
| Oral mucosa vs.
OSCC | 0.53 |
| Nucleus | LNM vs. oral
mucosa | <0.01 |
| LNM vs. OSCC | <0.01 |
| Oral mucosa vs.
OSCC | 0.07 |
| Cytoplasm | LNM vs. oral
mucosa | <0.01 |
| LNM vs. OSCC | <0.01 |
| Oral mucosa vs.
OSCC | 0.26 |
Connexin 43
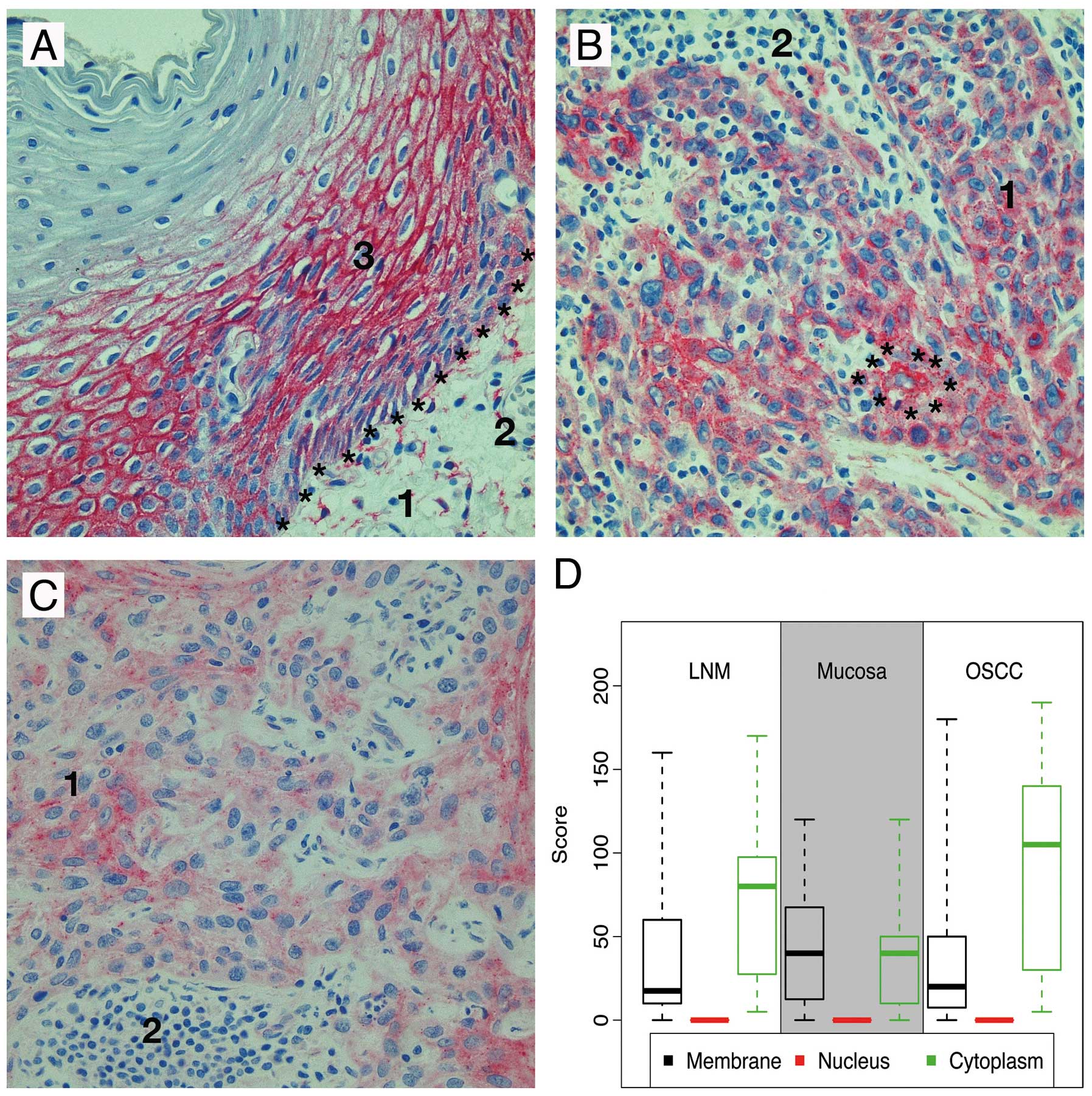
In dysplasia-free oral mucosa the strongest
Cx43-signals were detected within the plasma membrane and at a
lower level nearly exclusively in the lower half of the stratum
spinosum (Fig. 2A). Compared to
the matching oral mucosa tumour cells showed an upregulation of
cytoplasmic Cx43 expression within tumour cells of the primary
tumour and to a lower extent in lymph node metastases (P<0.01),
whereas membrane expression was not significantly altered (P=0.24)
(Fig. 2B–D). Pairwise comparisons
are summarized in Tables IV and
V.
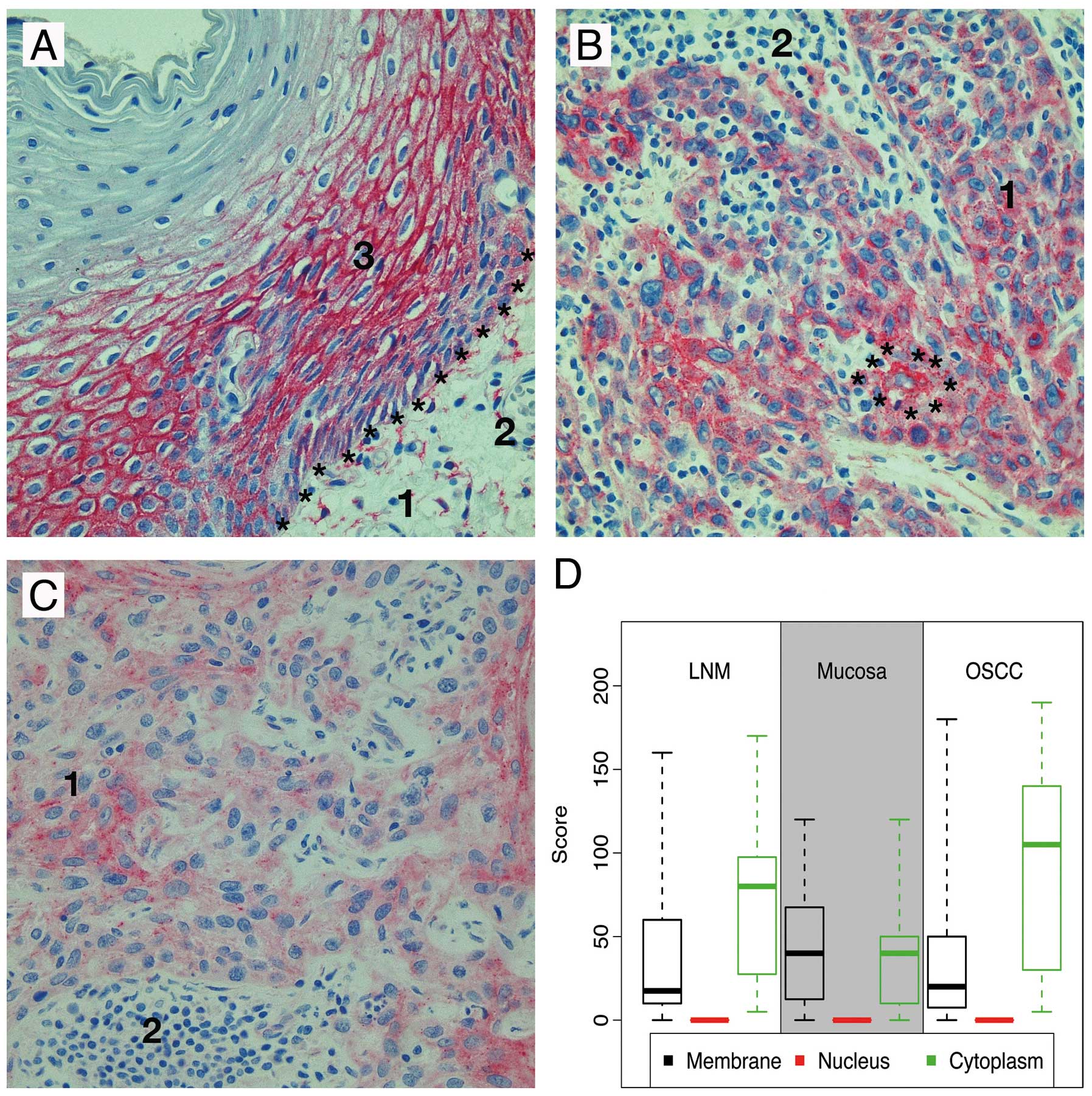 | Figure 2.Illustration of Cx43
immunohistochemistry; (A) Oral mucosa (magnification factor ×20)
(1, submucosa; 2, blood vessel; *, basal membrane; 3,
mucosa); (B) OSCC, original magnification ×40 (1, tumour cells; 2,
stroma; *, perinuclear Cx43 enrichment); (C) LNM,
original magnification ×40 (1, tumour cells; 2, stroma); (D)
Morphological distribution pattern. |
Connexin 45
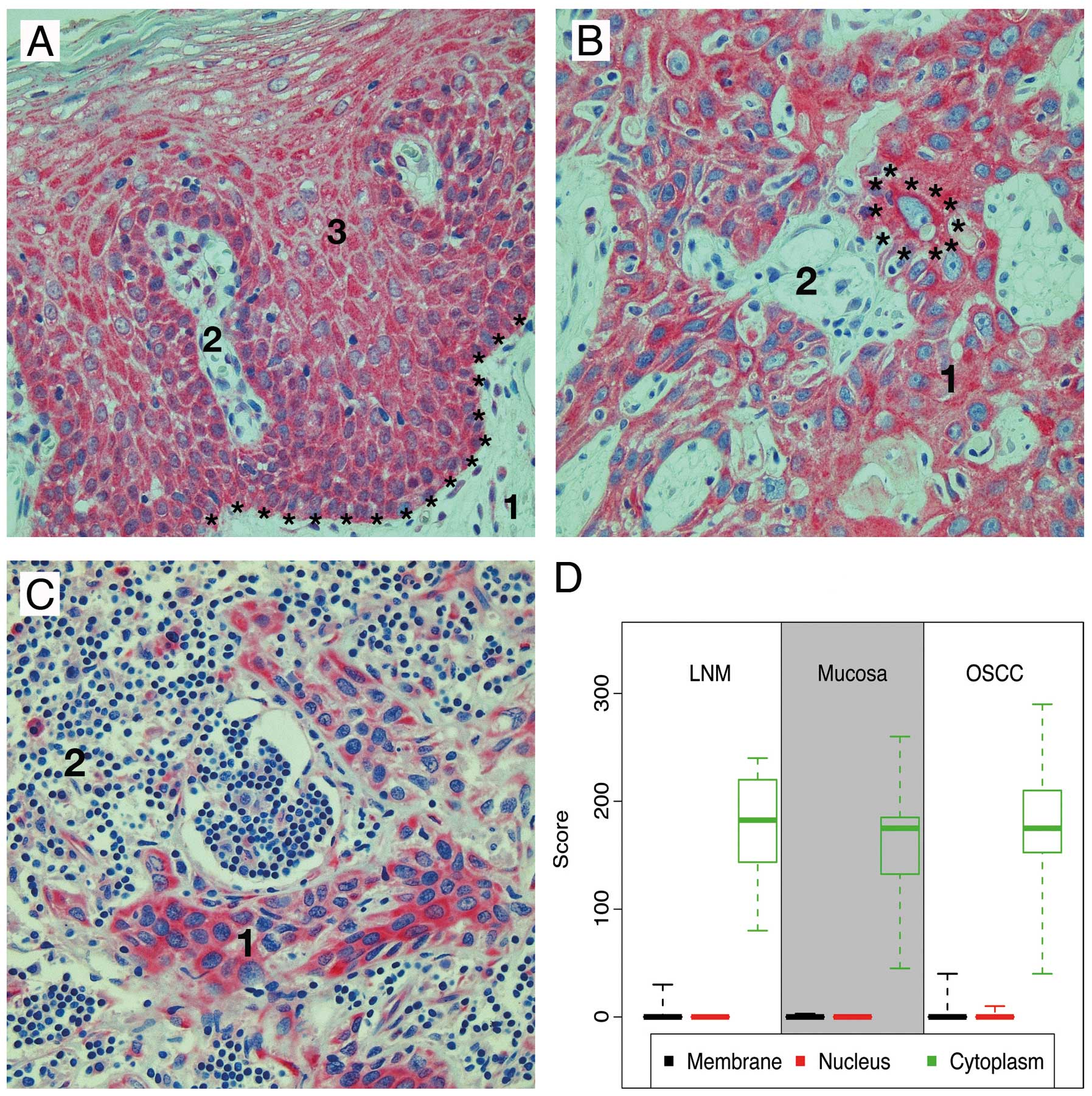
In contrast to Cx43, Cx45 expression increased from
the basal to the superficial layers of the squamous oral mucosa.
Parakeratosis was Cx45-negative. Cx45 was almost exclusively
expressed in the cytoplasm and weak signals were seen in the
membrane (Fig. 3A). The Cx45
distribution pattern did not change between dysplasia-free oral
mucosa, OSCC and associated lymph node metastases. In OSCC, the
cytoplasmic Cx45 expression was not significantly different from
the healthy oral mucosa (P=0.26) (Fig.
3B). In lymph node metastases, intracellular Cx45 expression
increased significantly compared to primary OSCC (P<0.01)
(Fig. 3C). The strongest signals
in both types of tissue could be seen in the perinuclear region.
The morphological distributions of Cx45 in the examined tissue
types are shown in Fig. 3D.
Pairwise comparisons are summarized in Tables IV and V.
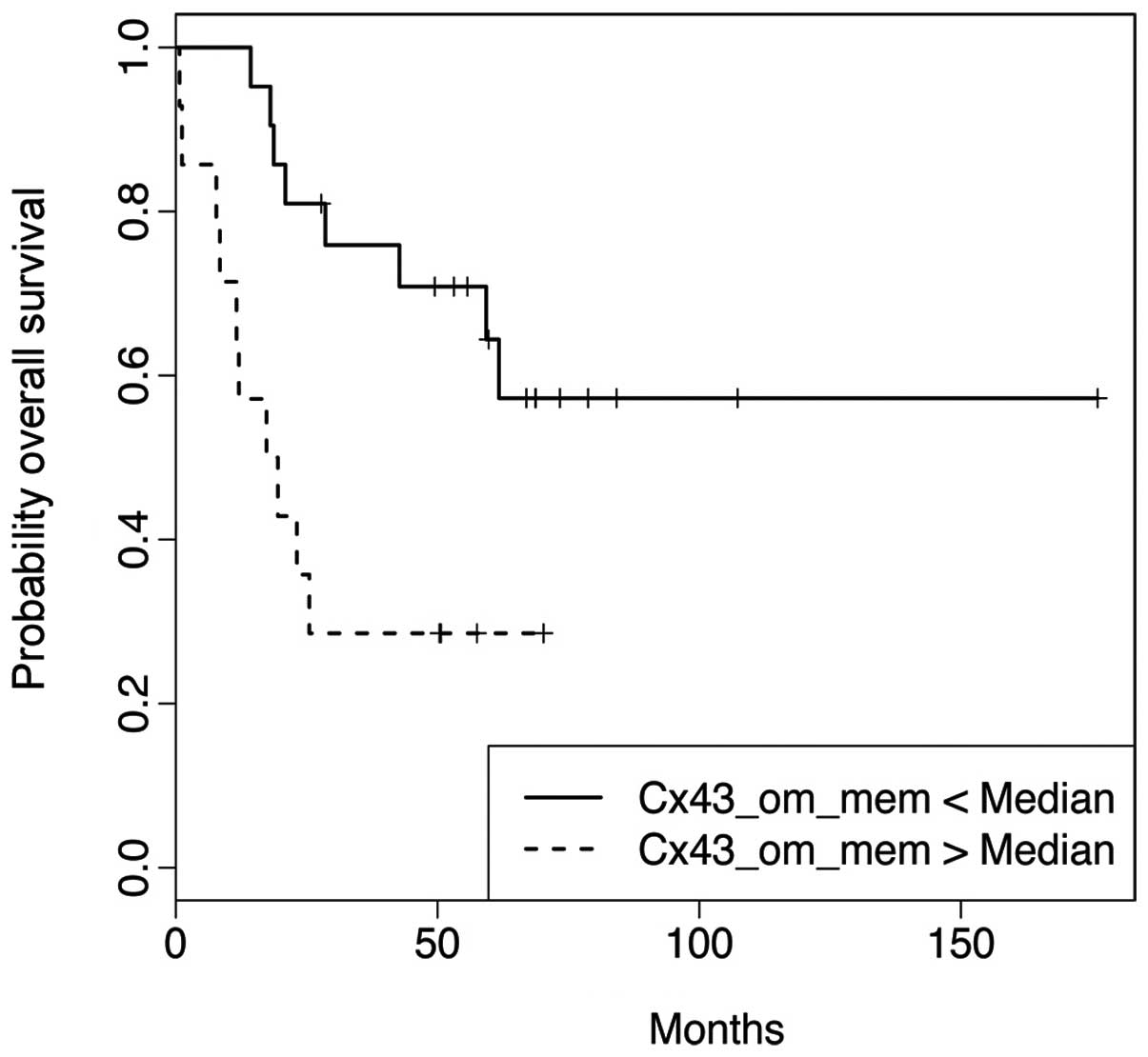
Connexins and survival of patients
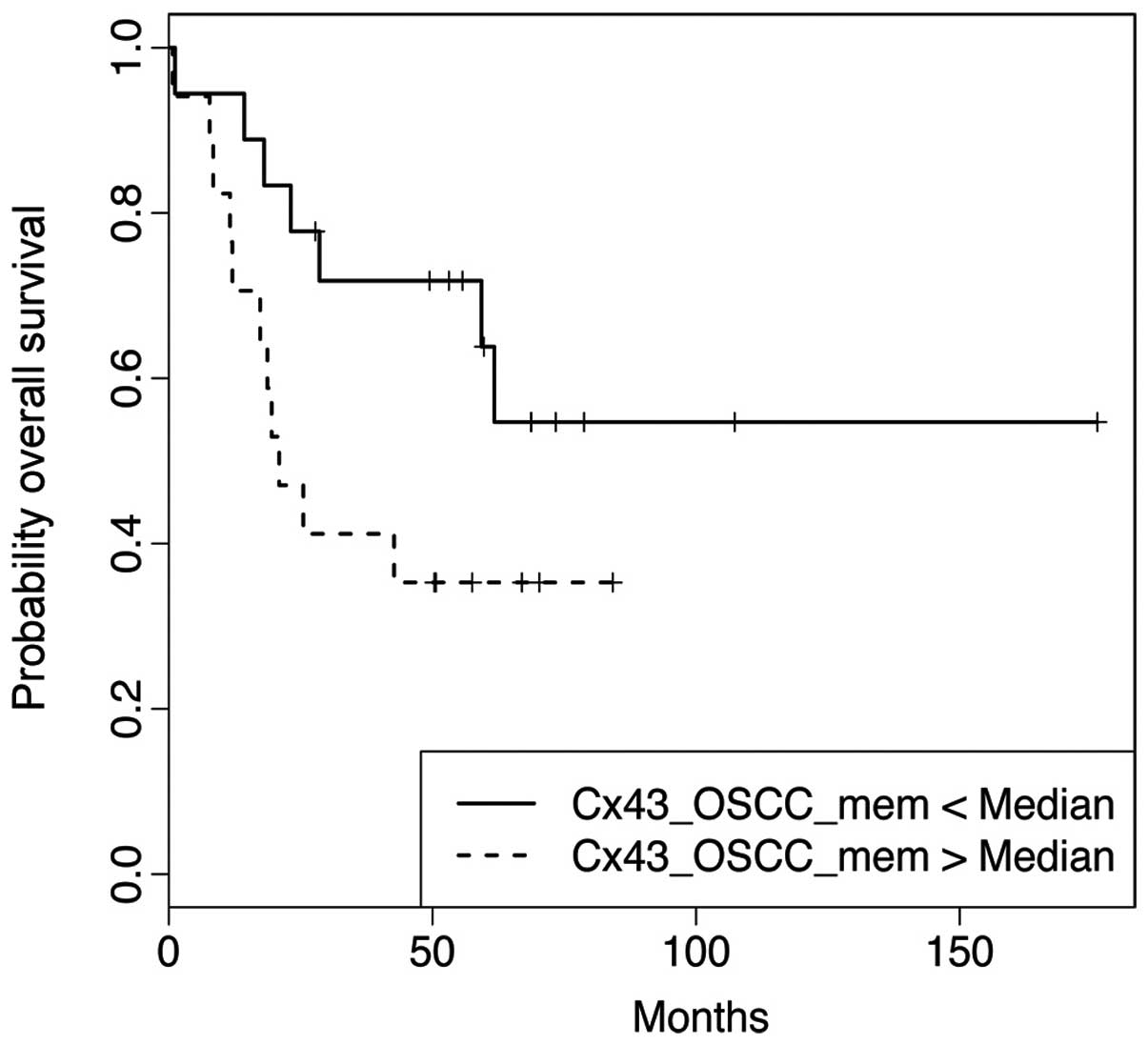
Cx26- and Cx45 expressions did not influence
survival. High membrane expression of Cx43 was significantly
associated with a shortened overall survival time (P=0.0088)
(Fig. 4). Additionally, a high
expression level in the cell membrane of matching dysplasia-free
oral mucosa showed a nearly significant association (P= 0.0596)
(Fig. 5). Correlation analysis is
shown in Table VI.
 | Table VI.Influence of connexin expression on
overall survival. |
Table VI.
Influence of connexin expression on
overall survival.
| Expression | HR | HR.lower | HR.upper | P-value |
|---|
| Cx26_OSCC_nuc | 1.00 | 1.00 | 1.00 | NA |
| Cx26_OM_nuc | 1.00 | 1.00 | 1.00 | NA |
| Cx26_LNM_nuc | 1.00 | 1.00 | 1.00 | NA |
| Cx43_OSCC_nuc | 1.00 | 1.00 | 1.00 | NA |
| Cx43_OM_nuc | 1.00 | 1.00 | 1.00 | NA |
| Cx43_LNM_nuc | 1.00 | 1.00 | 1.00 | NA |
| Cx45_OSCC_nuc | 0.96 | 0.79 | 1.18 | 0.6986 |
| Cx45_OM_nuc | 1.00 | 1.00 | 1.00 | NA |
| Cx45_LNM_nuc | 1.00 | 1.00 | 1.00 | NA |
| Cx26_OSCC_mem | 1.04 | 0.94 | 1.15 | 0.4648 |
| Cx26_OM_mem | 1.00 | 1.00 | 1.00 | NA |
| Cx26_LNM_mem | 0.99 | 0.94 | 1.04 | 0.7483 |
| Cx43_OSCC_mem | 1.02 | 1.00 | 1.03 | 0.0088 |
| Cx43_OM_mem | 1.01 | 1.00 | 1.02 | 0.0596 |
| Cx43_LNM_mem | 0.99 | 0.97 | 1.01 | 0.1984 |
| Cx45_OSCC_mem | 0.98 | 0.88 | 1.09 | 0.6877 |
| Cx45_OM_mem | 1.48 | 0.74 | 2.95 | 0.2637 |
| Cx45_LNM_mem | 0.91 | 0.71 | 1.16 | 0.4298 |
| Cx26_OSCC_cyto | 0.98 | 0.92 | 1.04 | 0.5562 |
| Cx26_OM_cyto | 1.00 | 1.00 | 1.00 | NA |
| Cx26_LNM_cyto | 0.99 | 0.95 | 1.03 | 0.5186 |
| Cx43_OSCC_cyto | 1.00 | 1.00 | 1.01 | 0.4277 |
| Cx43_OM_cyto | 1.01 | 0.99 | 1.02 | 0.3379 |
| Cx43_LNM_cyto | 1.02 | 1.00 | 1.03 | 0.1195 |
| Cx45_OSCC_cyto | 1.00 | 0.99 | 1.00 | 0.2803 |
| Cx45_OM_cyto | 1.00 | 0.98 | 1.01 | 0.6068 |
| Cx45_LNM_cyto | 1.01 | 0.99 | 1.03 | 0.2083 |
To investigate the association of general clinical
parameters with Cx43 expression levels, we performed correlation
tests. Expression of Cx43 correlated with clinical parameters,
which correlated with the overall survival time, such as the T
stage, the AJCC stage and the localisation of the primary tumour.
Membranous Cx43 expression in dysplasia-free oral mucosa showed a
significant association with the T stage (P<0.01) and AJCC stage
(P<0.01), but not with the localisation of the primary OSCC
(P=0.89). Cx43 expression within the tumour cell membrane was
independent of the T stage (P=0.06), the AJCC stage (P=0.07) and
the localisation of the primary tumour (P=0.79). Correlation
analysis is summarized in Table
VII.
 | Table VII.Correlation between Cx34_OSCC_mem and
Cx43_OM_mem to parameters, which are also correlated with overall
survival. |
Table VII.
Correlation between Cx34_OSCC_mem and
Cx43_OM_mem to parameters, which are also correlated with overall
survival.
| Parameter | Cx43_OSCC_mem | P-value | Cx43_OM_mem | P-value |
|---|
| Tis | 20.0 (20.0,
20.0) | 0.06 | 10.0 (10.0,
10.0) | <0.01 |
| T1 | 10.0 (0.0,
60.0) | | 15.0 (0.0,
40.0) | |
| T2 | 10.0 (0.0,
40.0) | | 30.0 (0.0,
110.0) | |
| T3 | 6.0 (2.0,
10.0) | | 0.0 (0.0, 0.0) | |
| T4 | 47.5 (0.0,
180.0) | | 62.5 (0.0,
120.0) | |
| Stage | 0 | 20.0 (20.0,
20.0) | 0.07 | 10.0 (10.0,
10.0) | <0.01 |
| 1 | 10.0 (0.0,
60.0) | | 15.0 (0.0,
40.0) | |
| 2 | 10.0 (0.0,
30.0) | | 30.0 (10.0,
110.0) | |
| 3 | 7.5 (2.0,
40.0) | | 0.0 (0.0,
20.0) | |
| 4 | 45.0 (0.0,
180.0) | | 60.0 (0.0,
120.0) | |
| Side | Left | 25.0 (0.0,
180.0) | 0.79 | 40.0 (0.0,
120.0) | 0.89 |
| Right | 15.0 (2.0,
100.0) | | 30.0 (0.0,
110.0) | |
| Median | 35.0 (0.0,
90.0) | | 40.0 (0.0,
120.0) | |
Discussion
Connexin 26
Although Cx26 was not expressed in dysplasia-free
oral mucosa, expression was increased in primary OSCC. Because of
its almost exclusive intracellular expression there is no
morphologic evidence for the involvement of Cx26 in the formation
of gap junctions. Compared to oral mucosa and primary OSCC, an
increased cytoplasmic and membrane Cx26 expression was measured in
lymph node metastases. Similar results have been reported by
Kanczuga-Koda et al, who studied the expression of Cx26 in
the tumour cells of mammary carcinoma and associated lymph node
metastases and detected overexpression of Cx26 in lymph node
metastases compared to the primary carcinoma (22). Saito-Katsuragi et al
investigated the involvement of Cx26 during the metastasis of human
malignant melanoma and observed a distinct Cx26 expression in the
tumour cells and in tumour-associated microvessel endothelia. Cx26
expression was not detected in control tissue from healthy dermis
nor nevus cell nevi (20).
Therefore, the tumour cells are likely to induce Cx26 in
tumour-associated microvessel endothelia and form homomeric gap
junctions between the two cell types furthering perivascular
accumulation of tumour cells and extravasation. This hypothesis is
supported by the recent results of membrane Cx26 expression in
lymph node metastases, which was not detectable at the primary
tumour site.
Connexin 43
In dysplasia-free oral mucosa Cx43 was predominantly
expressed at the membrane in the stratum spinosum. The expression
decreased with increasing keratinization. The course of
keratinization leads to a reduction of the cell membrane (27), which likely leads to the
internalization and degradation of Cx43 containing connexons. In
primary OSCCs a significant increase of cytoplasmic Cx43 expression
was detected compared to matching oral mucosa. Membrane Cx43
expression was not significantly different between these two types
of tissue. Tada and Hashimoto (27), who examined the localisation of
Cx43 by immunofluorescence and immune electron microscopy in normal
human skin, basal cell carcinoma and squamous cell carcinoma,
described similar results. In these two cancer types, Cx43 was
mainly intra cellular. Also Dubina et al (28) investigated the involvement of Cx43
in advanced stages of colorectal carcinoma and identified several
mutations that led to a frame shift and were localized in the
carboxyl group of the protein. The expression of these mutant
proteins was detected only in the invasive components of the
tumours.
These results suggest that gap junctions, composed
of Cx43, are lost during carcinogenesis and thereby cause a loss of
GJIC. Thus far, however, is not entirely clear whether this loss is
due to an increased degradation of intercellular channels or faulty
transcription and post-transcriptional modifications within the
connexins. An aberrant cytoplasmic localization and connexin
related disruption of GJIC might be important events during
tumourigenesis, invasion and metastasis. In the recent study we
found a relatively high expression of Cx43 in dysplasia-free
matched mucosa and, unexpectedly, an association of a significantly
shortened post-operative survival time of patients with a high Cx43
expression in the plasma membrane. We speculate that Cx43
expression is upregulated at a very early stage of promotion in
morphologically dysplasia-free mucosa because of its association
with an advanced T stage and AJCC stage and the trend to a
shortened OS. However, this cannot be proved, due to the fact that
it is almost impossible to obtain unaffected oral mucosa. The
association of increased membranous Cx43 expression on tumour cells
with a worse prognosis indicates that Cx43 acts as a tumour
promoter in OSCC in contrast to other cancer types. It should also
be kept in mind that there are no standardised quantitative
immunohisto-chemical Cx expression procedures developed so far
regarding the antibodies, the detection systems and the
immunoreactive scores. The particular characteristic of the recent
study is an immunoreactive staining score that includes every level
of staining intensity for each subcellular localisation that allows
a very detailed quantification. This is an important difference
from many other studies in which the scores were calculated on the
basis of an average staining intensity.
Connexin 45
Cx45 has been extensively studied with regards to
its co-expression with Cx43 resulting in altered GJIC. In heart
failure, Cx45 is upregulated compared to Cx43 (29). The diffusion capacity of cationic
fluorescent dyes over gap junction function is reduced when Cx45 is
overexpressed and forms heteromeric gap junctions in
co-localization with Cx43 (18),
leading to altered intercellular voltage gating mechanisms
(17). The relative upregulation
of Cx45 compared to Cx43 was shown to cause an increased
susceptibility for cardiac arrhythmias in vivo (16). There is only slight evidence on the
relevance of Cx45 expression in malignant tumours. It has been
shown, that Cx45 is variably expressed in human lung fibroblasts
and human lung carcinoma cells (30). Cx45 is also expressed in normal
lung tissue and advanced stages of mouse lung carcinomas (31). GJIC-dependent contact inhibition
can block cell proliferation (8).
Decreased GJIC may therefore enhance cell growth of an initiated
cell clone.
In the present study, Cx45 was almost exclusively
expressed intracellularly in dysplasia-free oral mucosa and primary
OSCC, without any difference between these two tissues. The
strongest Cx45 expression was measured in the lymph node
metastases. In addition to the cytoplasmic expression, membrane
Cx45 expression increased significantly in lymph node metastasis to
a very low level in a few tumour cells. Therefore, the formation of
homo- or heteromeric gap junctions is unlikely.
High membrane Cx43 expression is an independent
marker of poor prognosis of OSCC. Membrane expression of Cx43 in
matching tumour-free mucosa is also associated with poor prognosis.
This provides evidence for a relevant expression of Cx43 at very
early stage of tumour promotion in damaged mucosa. The recent data
are suggestive of homodimeric Cx43 containing GJs. The mechanisms
of the turnover of high cytoplasmic Cx43 levels without prognostic
relevance and lower membrane Cx43 levels with prognostic relevance
remain to be elucidated. Due to their expression levels and
dominant cytoplasmic expression pattern Cx26 and Cx45 seem to be of
minor relevance for tumour progression.
References
|
1.
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar
|
|
2.
|
Argiris A and Eng C: Epidemiology,
staging, and screening of head and neck cancer. Cancer Treat Res.
114:15–60. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Ries LAG, Melbert D and Krapcho M: SEER
Cancer Statistics Review, 1975–2004. National Cancer Institute;
Bethesda, MD: 2007
|
|
4.
|
Massano J, Regateiro FS, Januário G and
Ferreira A: Oral squamous cell carcinoma: review of prognostic and
predictive factors. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 102:67–76. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Willecke K, Eiberger J, Degen J, et al:
Structural and functional diversity of connexin genes in the mouse
and human genome. Biol Chem. 383:725–737. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Loewenstein WR and Penn RD: Intercellular
communication and tissue growth. II Tissue regeneration. J Cell
Biol. 33:235–242. 1967. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Cronier L, Crespin S, Strale PO, Defamie N
and Mesnil M: Gap junctions and cancer: new functions for an old
story. Antioxid Redox Signal. 11:323–338. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Trosko JE, Chang CC, Upham BL and Tai MH:
Ignored hallmarks of carcinogenesis: stem cells and cell-cell
communication. Ann N Y Acad Sci. 1028:192–201. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
King TJ, Fukushima LH, Donlon TA, Hieber
AD, Shimabukuro KA and Bertram JS: Correlation between growth
control, neoplastic potential and endogenous connexin43 expression
in HeLa cell lines: implications for tumor progression.
Carcinogenesis. 21:311–315. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Iacobas DA, Urban-Maldonado M, Iacobas S,
Scemes E and Spray DC: Array analysis of gene expression in
connexin-43 null astrocytes. Physiol Genomics. 15:177–190.
2003.PubMed/NCBI
|
|
11.
|
Iacobas DA, Scemes E and Spray DC: Gene
expression alterations in connexin null mice extend beyond the gap
junction. Neurochem Int. 45:243–250. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Avanzo JL, Mesnil M, Hernandez-Blazquez
FJ, et al: Increased susceptibility to urethane-induced lung tumors
in mice with decreased expression of connexin43. Carcinogenesis.
25:1973–1982. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
McLachlan E, Shao Q, Wang HL, Langlois S
and Laird DW: Connexins act as tumor suppressors in
three-dimensional mammary cell organoids by regulating
differentiation and angiogenesis. Cancer Res. 66:9886–9894. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Mesnil M, Krutovskikh V, Piccoli C, et al:
Negative growth control of HeLa cells by connexin genes: connexin
species specificity. Cancer Res. 55:629–639. 1995.PubMed/NCBI
|
|
15.
|
Yano T, Hernandez-Blazquez FJ, Omori Y and
Yamasaki H: Reduction of malignant phenotype of HEPG2 cell is
associated with the expression of connexin 26 but not connexin 32.
Carcinogenesis. 22:1593–1600. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Betsuyaku T, Nnebe NS, Sundset R,
Patibandla S, Krueger CM and Yamada KA: Overexpression of cardiac
connexin45 increases susceptibility to ventricular tachyarrhythmias
in vivo. Am J Physiol Heart Circ Physiol. 290:H163–H171. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Bukauskas FF, Angele AB, Verselis VK and
Bennett MV: Coupling asymmetry of heterotypic connexin 45/connexin
43-EGFP gap junctions: properties of fast and slow gating
mechanisms. Proc Natl Acad Sci USA. 99:7113–7118. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Koval M, Geist ST, Westphale EM, et al:
Transfected connexin45 alters gap junction permeability in cells
expressing endogenous connexin43. J Cell Biol. 130:987–995. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Ogawa K, Pitchakarn P, Suzuki S, et al:
Silencing of connexin 43 suppresses invasion, migration and lung
metastasis of rat hepatocellular carcinoma cells. Cancer Sci.
103:860–867. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Saito-Katsuragi M, Asada H, Niizeki H, et
al: Role for connexin 26 in metastasis of human malignant melanoma:
communication between melanoma and endothelial cells via connexin
26. Cancer. 110:1162–1172. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Ito A, Koma Y, Uchino K, et al: Increased
expression of connexin 26 in the invasive component of lung
squamous cell carcinoma: significant correlation with poor
prognosis. Cancer Lett. 234:239–248. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Kanczuga-Koda L, Sulkowski S, Lenczewski
A, et al: Increased expression of connexins 26 and 43 in lymph node
metastases of breast cancer. J Clin Pathol. 59:429–433. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Lin JH, Takano T, Cotrina ML, et al:
Connexin 43 enhances the adhesivity and mediates the invasion of
malignant glioma cells. J Neurosci. 22:4302–4311. 2002.PubMed/NCBI
|
|
24.
|
Ozawa H, Matsunaga T, Kamiya K, et al:
Decreased expression of connexin-30 and aberrant expression of
connexin-26 in human head and neck cancer. Anticancer Res.
27:2189–2195. 2007.PubMed/NCBI
|
|
25.
|
Villaret DB, Wang T, Dillon D, et al:
Identification of genes overexpressed in head and neck squamous
cell carcinoma using a combination of complementary DNA subtraction
and microarray analysis. Laryngoscope. 110:374–381. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Brunner E, Domhof S and Langer F:
Nonparametrich Analysis of Longitudinal Data in Factorial
Experiments. John Wiley and Sons; New York: 2002
|
|
27.
|
Tada J and Hashimoto K: Ultrastructural
localization of gap junction protein connexin 43 in normal human
skin, basal cell carcinoma, and squamous cell carcinoma. J Cutan
Pathol. 24:628–635. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Dubina MV, Iatckii NA, Popov DE, Vasil’ev
SV and Krutovskikh VA: Connexin 43, but not connexin 32, is mutated
at advanced stages of human sporadic colon cancer. Oncogene.
21:4992–4996. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Yamada KA, Rogers JG, Sundset R, Steinberg
TH and Saffitz J: Up-regulation of connexin45 in heart failure. J
Cardiovasc Electrophysiol. 14:1205–1212. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Zhang ZQ, Hu Y, Wang BJ, Lin ZX, Naus CC
and Nicholson BJ: Effective asymmetry in gap junctional
intercellular communication between populations of human normal
lung fibroblasts and lung carcinoma cells. Carcinogenesis.
25:473–482. 2004. View Article : Google Scholar
|
|
31.
|
Udaka N, Miyagi Y and Ito T: Connexin
expression in mouse lung tumor. Cancer Lett. 246:224–229. 2007.
View Article : Google Scholar : PubMed/NCBI
|