Introduction
Lipomas are the most common soft tissue tumors with
a prevalence rate of 2.1 per 1,000 people (1). Lipomas are benign tumors of
mesenchymal origin composed of mature lipocytes (2) and may be localized in any region of
the body, superficial or deep (3).
Generally, lipomas are subcutaneous, small, multiple and weigh only
a few grams (4), their preferable
locations being the thigh, shoulder and trunk (5). However, a small number of lipomas may
also be subfascial and further classified as parosteal,
interosseous or visceral, as well as infiltrating lipomas (6) [including inter- and intramuscular
lipomas, with an estimated incidence of 1.8 and 0.3%, respectively
(7)]. Intermuscular lipomas are
thought to arise from the intermuscular septa and to enlarge
between muscle bundles, while the lesions are usually
well-circumscribed and easily separated during surgery.
Intramuscular lipomas, however, arise between muscle fibers, pass
through the intermuscular septa and infiltrate the surrounding
tissues, rendering removal of the lesion from the nearby muscles
difficult (8–10). Liposarcomas are malignant soft
tissue tumors reported in radiological as well as histological
findings to comprise 7–27% of the soft tissue sarcomas (11), and be able to mimic inter- and
intramuscular lipomas, rendering the diagnosis and choice of
treatment difficult (12).
The aim of this study was to report a giant
deep-seated intermuscular lipoma of the hip, and discuss the
epidemiology, histopatholgy, imaging characteristics, differential
diagnosis and management of the intermuscular lipomas.
Materials and methods
Identification of patients with
intermuscular lipoma
The Chinese Biological and Medicine Database
(between January, 1992 and May, 2012), the China Hospital Knowledge
Database and the Chinese Science and Technology Periodical Database
were searched. An additional search was carried out regarding the
Chinese journals that were not included in the network database and
4 patients were identified. Duplicate reports were identified and
excluded from further analysis to avoid overrepresentation. Twelve
cases reported in China were identified. Informed consent was
obtained from the patients and the study was approved by the
Research Ethics Committee of the Zhejiang University.
Case report
A 50-year-old female patient was treated in our
outpatient clinic with a complaint of post-traumatic swelling of
the left hip. The patient had a history of a car accident and an
injury of the left hip. She did not seek for medical treatment
until she felt a swollen mass 20 days later. Physical examination
showed a 12×12 cm lump located in the left hip, on the post-lateral
side of the greater trochanter of the femur bone. The lump was
smooth-surfaced, immobile, had increased skin tension and was
non-pulsatile with mild tenderness, which radiated towards the
lower limb. The laboratory examinations were normal. The
ultrasonographic examination showed a 5.0-cm liquid dark area deep
in the muscular layer, with tiny high-level echo spots floating
inside. No significant blood flow signals were detected by color
Doppler flow imaging (CDFI). Based on the present history, clinical
presentations and ultrasonographic outcome, the patient was
admitted for post-traumatic hematoma. However, further examination
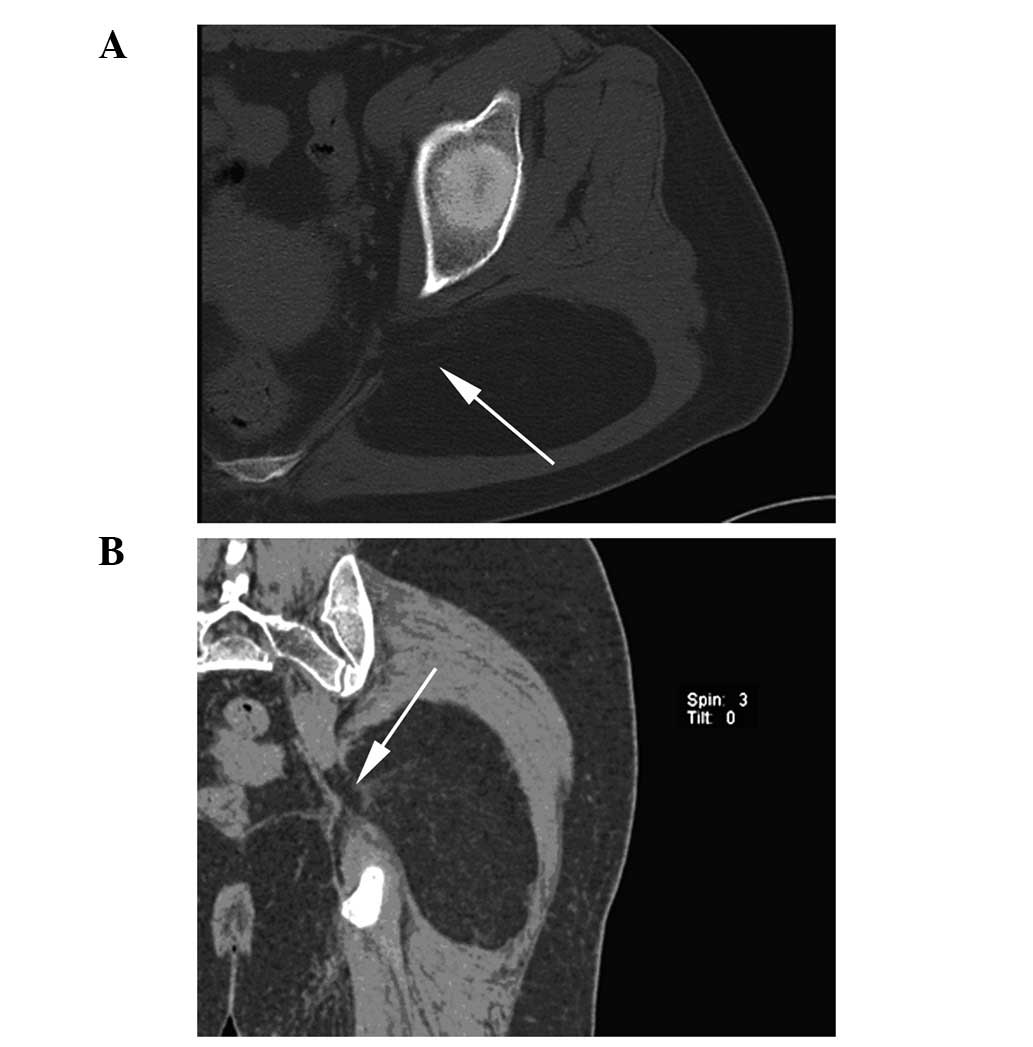
of computed tomography (CT) demonstrated a 10.4×5.3×13-cm diameter
fat density mass [CT value-95 Hounsfield Units (HU)], accompanied
by slightly higher density streaky structures with obscure
boundaries under the left gluteus maximus, possibly infiltrating
the anteromedial muscle (Fig.
1).
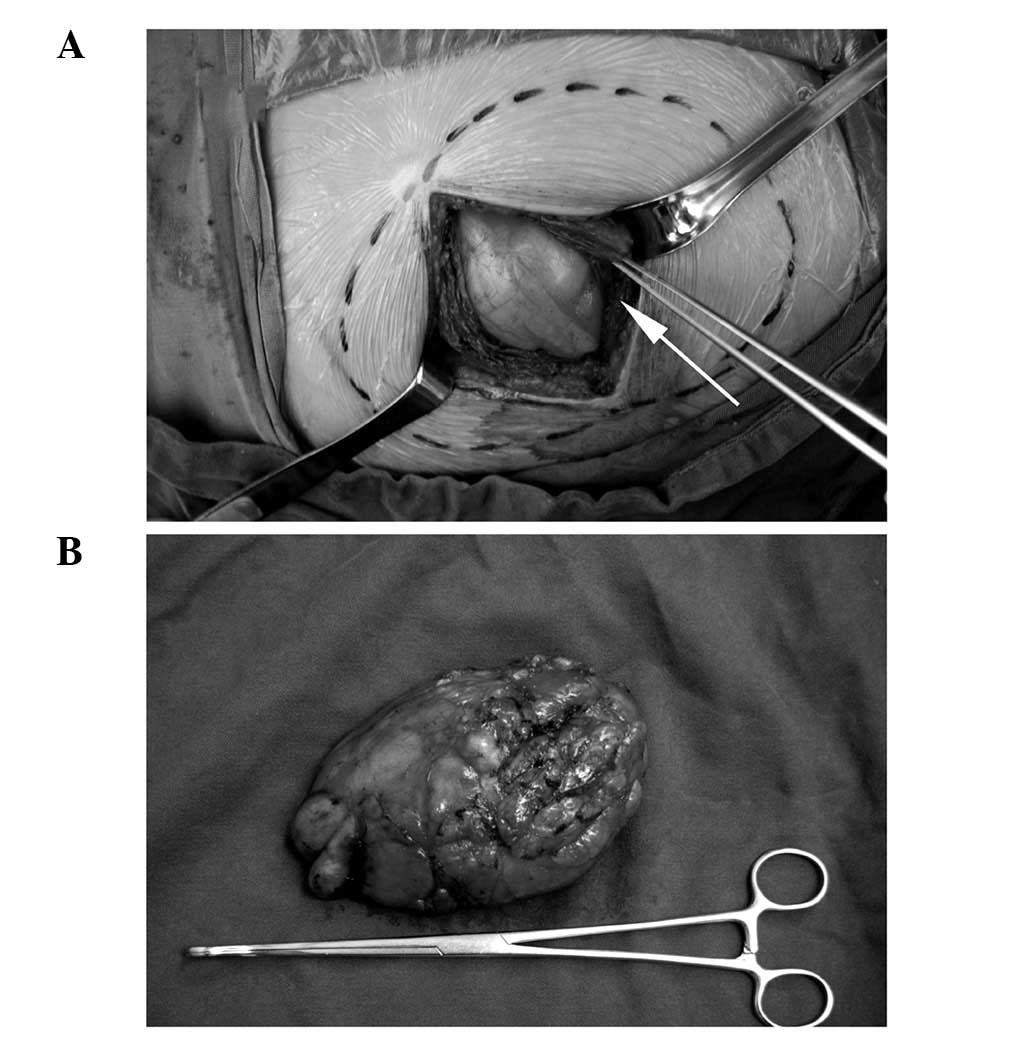
During surgery, an incision parallel with the muscle
fiber of the gluteus maximus was selected. A circumscribed mass
with intact capsule was noted beneath the gluteus maximus,
compressing the surrounding muscles (the gluteus maximus and
piriformis muscle), and partly protruding through the
infra-piriform foramen, although no vessels or nerves were involved
(Fig. 2). The mass was removed en
bloc, while protecting the sciatic nerve.
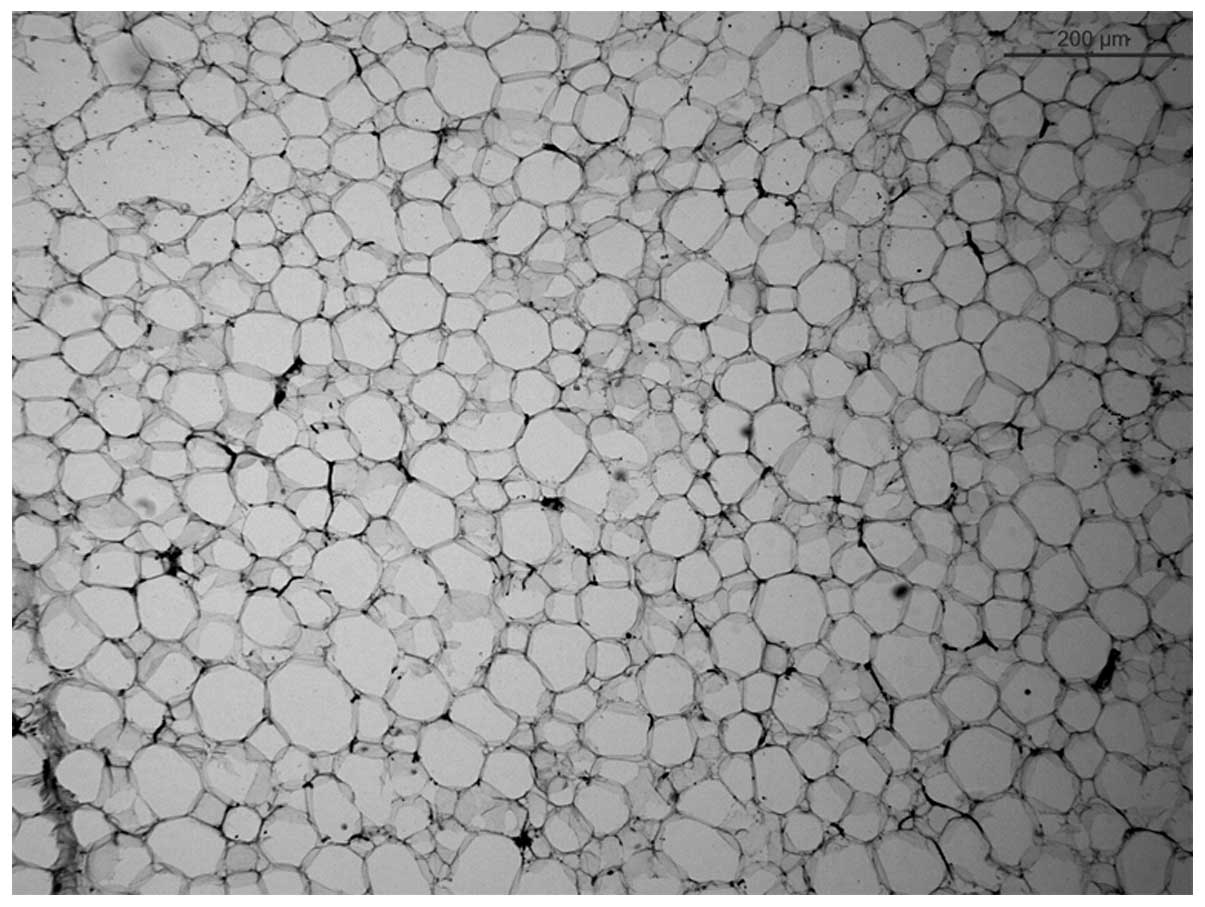
The histopathologic examination showed a giant
intermuscular lipoma of the left hip (10×13×6 cm), comprising
mature fat cells without the involvement of muscle fibers, with no
evidence of cellular atypia, mitosis or necrosis (Fig. 3). The patient recovered and was
discharged 3 days after surgery without any complications. A
6-month follow-up was carried out and no recurrence was
detected.
Results
Twelve reported cases of intermuscular lipoma,
surgically treated in China between January, 1992 and May, 2012
were retrospectively reviewed. The detailed information is shown in
Table I. There were 8 (66.7%)
males and 4 females (33.3%), indicating that intermuscular lipoma
occurred more frequently in men, which was consistent with the
findings reported in the study by Nishida et al (12). The patients had an average age of
39.7 years (range, 11–70), with a symptom duration between 1 month
and 10 years (mean, 41.8 months). The most common site of tumor
origin was the thigh (6 patients, 50%), followed by the forearm (2
patients, 16.7%). Additional sites, such as the neck, submental,
buttock and midpalmar space were also reported. As for symptoms, an
asymptomatic mass was the most frequent presentation (6 patients,
50%), followed by swelling mass (4 patients, 33.3%). Movement
disorder and numbness were also reported, possibly generated by
compression of the tumor to the surrounding nerves. Moreover, the
clinical presentations were not closely correlated with the tumor
size. For instance, patient 1 on the list had a small-sized lipoma
(5×3×1.5 cm) that generated movement disorder, while patient 10 had
the largest lesion reviewed, with no neuromuscular dysfunctions.
Thus, a critically located lesion may induce a mass effect
regardless of its size. The 12 patients underwent surgery following
admission and recovered successfully.
 | Table ICharacteristics of intermuscular
lipomas reported in China during the past 20 years. |
Table I
Characteristics of intermuscular
lipomas reported in China during the past 20 years.
| Patient | Gender | Age (years) | Duration of
symptoms | Dimensions (cm) | Localization | Symptoms |
|---|
| 1 | M | 45 | 3 months | 5×3×1.5 | Forearm | Movement
disorder |
| 2 | M | 46 | 6 years | 15×10×8 | Neck | Painless mass |
| 3 | M | 11 | 5 years | 1.5×3.0 | Submental | Painless mass |
| 4 | F | 51 | 2 months | 15×15×6 | Buttock | Painless mass |
| 5 | F | 40 | 4 years | 14×6.5×8 | Thigh | Numbness and
mass |
| 6 | F | 52 | 1 month | 25×10×8 | Thigh | Swelling and
mass |
| 7 | M | 70 | 10 years | 6×5 | Forearm | Painless mass |
| 8 | M | 26 | 2 years | 14.6×13.5×6.1 | Thigh | Swelling and
mass |
| 9 | M | 20 | 6 months | 13×13×6 | Thigh | Painless mass |
| 10 | M | 60 | 5 years | 29×20×3.5 | Thigh | Swelling and
mass |
| 11 | M | 29 | 9 months | 20×16×7 | Thigh | Swelling and
mass |
| 12 | F | 26 | 8 years | 5×5×2 | Midpalmar space | Painless mass |
Discussion
Lipomas are the most common benign soft tissue
tumors that may occur anywhere in the body, and are mostly found
within the subcutaneous areas. However, compared to common
inter-muscular lipomas, giant, deep-seated lipomas of the hip are
even more infrequent and thus easily misdiagnosed. In this study,
we presented an adult female patient with an unusually large, deep
intermuscular lipoma in the left hip that led the initial
misdiagnosis.
Due to the rare location, intermuscular giant
lipomas are easily overlooked when making primary diagnosis upon
admission. To differentiate from other soft tissue tumors,
auxiliary examinations including ultrasonography, CT and magnetic
resonance imaging (MRI) are needed, which may improve the
diagnosis, as well as an appropriate staging of the tumor extension
and involved structures. Ultrasonography of the lipomas is often
the initial diagnostic procedure due to its availability and
cost-effectiveness, when compared with CT and MRI. Generally,
lipomas have been described as being homogeneous in echotexture and
typically slightly hyperechoic to subcutaneous fat (13), although exceptions have frequently
been observed (14). This may be
caused by different compositions of the tumor since pure fatty
tumors have less acoustic impedance due to fewer interfaces
compared with tumors with a mixed composition of fat and water
(15). Ultrasonography alone is
not definitive, thus CT and MRI should be considered to further
assess the nature of the lesion. Fat has low attenuation on CT,
i.e., less than −20 HU and typically between −65 and −120 HU (−95
HU in the present case) (16). As
for intermuscular lipomas, CT shows a fat density mass, usually
accompanying thin streaky densities (66.7% reported), which are
fibrous tissues of the intermuscular space. The thickness of these
streaks is uniform and they are usually uninterrupted (12). On the MRI, intermuscular lipomas
show a fat signal intensity mass similar to CT on T1- and
T2-weighted images, although the thin streaky densities are less
distinctive on MRI compared with the CT (12,16).
Giant intermuscular lipomas should be differentiated
from liposarcomas, malignant fibrous histiocytomas, metastatic
carcinomas or other benign soft-tissue lesions, such as a cyst,
hematoma, muscle herniation, cystic hygroma or fibrous myositis
(8,17). Intermuscular lipomas should also be
distinguished from liposarcomas in terms of malignancy. The
possibility of liposarcoma should be considered when a fatty tumor
with a dimension of >10 cm has shown rapid growth (11). Imaging examinations may be of
crucial importance in the differentiation between the two tumors.
On CT, a liposarcoma shows a fat density mass with areas of unclear
amorphous density, usually accompanied by thick and thin streaky
soft tissue densities, with occasionally interrupted streaks. On
MRI, signal intensity of fat is evident, however, the intensity is
lower compared with normal fat in certain areas, and the thick
streaky structures are less distinctive when compared with the CT
(12). Moreover, despite a proven
negative imaging, a liposarcoma may still be malignant. Therefore,
careful histopathologic evaluation is required, and the presence of
nuclear pleomorphism and multinuclear giant cells may help to
distinguish lipomas from malignant liposarcomas (18).
In the present case, the patient with post-traumatic
hematoma was diagnosed initially based on her clinical symptoms
(swelling for 20 days), trauma history and ultrasonography (liquid
dark area in the muscular layer and no blood signal evident).
Deep-seated lipomas should always be taken into consideration when
dealing with soft tissue masses. The mechanism for intermuscular
lipomas remains unclear, and trauma was reported as a related
factor (4,19,20).
It was suggested that after a blunt trauma, rupture of the fibrous
septa, which prevent the migration of fat, accompanied by tears of
the anchorage between the skin and the deep fascia likely resulted
in the proliferation of adipose tissue (20). However, in the present patient, the
tumor was believed to have already existed prior to the accident
and became evident after being extruded from the surrounding
tissues by the trauma, given the limited time period between the
trauma and mass formation (20 days).
The treatment for this type of tumor is complete
excision. However, indications of the surgery may be discomfort by
fascial compartment syndrome, the necessity of differential
diagnosis from malignant tumors and the possible development of
malignant alterations. Generally, intermuscular lipomas have a
well-defined pseudo-capsule (3,12,21),
thus, dissection around these benign neoplasms is not particularly
difficult. The surgical removal of the tumor ought to be complete
since residual disease may lead to recurrence and additional
surgical procedures with added risk and complications (22). Therefore, a thorough anatomic
knowledge and experience must be obtained prior to attempting an
excision. In the surgical operation, however, the extent of the
resection is sometimes modified to avoid injuring important
surrounding neurovascular or muscular tissues and causing
functional impairment. This compromise between adequate surgical
margins and functional disability may lead to incomplete resection
and an obviously higher local recurrence rate. Following excision,
the recurrence rate of intermuscular lipoma was described as
modest, with the lowest rate at 3% and the highest at 62.5%
(23), which was most likely due
to incomplete surgical excision. Thus, the possibility of
recurrence after long lipoma-free intervals are probable, while an
extended period of long-term follow-up is mandatory.
In conclusion, intermuscular lipomas are rare benign
tumors, with giant lesions being even more infrequent, and are
generally presented with painless mass or swelling for years. It is
important for clinicians to be aware of the infiltrating lipomas
when dealing with deep-seated soft tissue masses. To make an
accurate diagnosis, imaging techniques (ultrasonography, CT and
MRI) may be helpful and useful, particularly when making
differential diagnosis. Surgical removal is the treatment of choice
providing a definite diagnosis, while a complete resection of the
lesions is vital to avoid recurrences.
References
|
1
|
Silistreli OK, Durmus EU, Ulusal BG, Oztan
Y and Gorgu M: What should be the treatment modality in giant
cutaneous lipomas? Review of the literature and report of 4 cases.
Br J Plast Surg. 58:394–398. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bispo Junior RZ and Guedes AV: Parosteal
lipoma of the femur with hyperostosis: case report and literature
review. Clinics (Sao Paulo). 62:647–652. 2007.PubMed/NCBI
|
|
3
|
Hakim E, Kolander Y, Meller Y, Moses M and
Sagi A: Gigantic lipomas. Plast Reconstr Surg. 94:369–371. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Terzioglu A, Tuncali D, Yuksel A, Bingul F
and Aslan G: Giant lipomas: a series of 12 consecutive cases and a
giant liposarcoma of the thigh. Dermatol Surg. 30:463–467.
2004.PubMed/NCBI
|
|
5
|
Copcu E, Sivrioglu N and Culhaci N:
Axillary giant lipoma. Plast Reconstr Surg. 114:1982–1983. 2004.
View Article : Google Scholar
|
|
6
|
Gonzalez-Crussi F, Enneking WF and Arean
VM: Infiltrating angiolipoma. J Bone Joint Surg Am. 48:1111–1124.
1966.
|
|
7
|
Fletcher CD and Martin-Bates E:
Intramuscular and inter-muscular lipoma: neglected diagnoses.
Histopathology. 12:275–287. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pelissier A, Sawaf MH and Shabana AH:
Infiltrating (intramuscular) benign lipoma of the head and neck. J
Oral Maxillofac Surg. 49:1231–1236. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lerosey Y, Choussy O, Gruyer X, et al:
Infiltrating lipoma of the head and neck: a report of one pediatric
case. Int J Pediatr Otorhinolaryngol. 47:91–95. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ozcan C, Gorur K, Talas D and Aydin O:
Intramuscular benign lipoma of the sternocleidomastoid muscle: a
rare cause of neck mass. Eur Arch Otorhinolaryngol. 262:148–150.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Celik C, Karakousis CP, Moore R and
Holyoke ED: Liposarco mas: prognosis and management. J Surg Oncol.
14:245–249. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nishida J, Morita T, Ogose A, et al:
Imaging characteristics of deep-seated lipomatous tumors:
intramuscular lipoma, inter-muscular lipoma, and lipoma-like
liposarcoma. J Orthop Sci. 12:533–541. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lin J, Jacobson JA, Fessell DP, Weadock WJ
and Hayes CW: An illustrated tutorial of musculoskeletal
sonography: part 4, musculoskeletal masses, sonographically guided
interventions, and miscellaneous topics. AJR Am J Roentgenol.
175:1711–1719. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Volta A, Bonazzi M, Gnudi G, Gazzola M and
Bertoni G: Ultrasonographic features of canine lipomas. Vet Radiol
Ultrasound. 47:589–591. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Inampudi P, Jacobson JA, Fessell DP, et
al: Soft-tissue lipomas: accuracy of sonography in diagnosis with
pathologic correlation. Radiology. 233:763–767. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Munk PL, Lee MJ, Janzen DL, et al: Lipoma
and liposarcoma: evaluation using CT and MR imaging. AJR Am J
Roentgenol. 169:589–594. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Harrington AC, Adnot J and Chesser RS:
Infiltrating lipomas of the upper extremities. J Dermatol Surg
Oncol. 16:834–837. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dionne GP and Seemayer TA: Infiltrating
lipomas and angiolipomas revisited. Cancer. 33:732–738. 1974.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Simon HE and Senturia HR: Intermuscular
lipoma of the thigh, with roentgenologic findings. South Med J.
39:624–626. 1946. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Meggitt BF and Wilson JN: The battered
buttock syndrome - fat fractures. A report on a group of traumatic
lipomata. Br J Surg. 59:165–169. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Higgs PE, Young VL, Schuster R and Weeks
PM: Giant lipomas of the hand and forearm. South Med J. 86:887–890.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Echenique-Elizondo M: Intermuscular
lipoma. J Am Coll Surg. 193:4522001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Weiss SW: Lipomatous tumors. Monogr
Pathol. 38:207–239. 1996.
|