Introduction
Locally advanced cervical cancer without distant
metastasis [International Federation of Gynecology and Obstetrics
(FIGO) stage IIB, IIIA, IIIB or IVA] is usually treated with
definitive pelvic radiation and concurrent chemotherapy. However,
increased acute toxicity involving hematological, gastrointestinal
or genitourinary systems by the addition of concurrent chemotherapy
to radiotherapy has been reported (1–3). In
Kirwan's meta-analysis, late grade 3 or 4 toxicity (cystitis,
proctitis, or intestinal obstruction) was observed in 23.3% in the
chemoradiotherapy group (4).
According to the NCCN clinical practice guidelines
for cervical cancer, version 1.2017, intensity-modulated radiation
therapy (IMRT) and similar highly conformed methods of dose
delivery may be helpful in minimizing the dose to the bowel and
other critical structures in the IMRT post-hysterectomy setting and
in treating the para-aortic nodes when necessary. In the Japan
Society of Gynecologic Oncology (JSGO) guidelines 2017 for the
treatment of uterine cervical cancer, it is stated that the dose to
the bowel, bladder, or bone marrow may be reduced by using IMRT
compared with conventional radiotherapy, which may lead to a lower
rate of complications in the post-hysterectomy setting. According
to the Japanese guidelines, appropriate treatment planning is
necessary considering the dose limitation to normal organs and the
volume change in the bladder or rectum during IMRT. Gandhi et
al (5) previously reported the
toxicity and clinical outcome in patients with locally advanced
cervical cancer treated with whole pelvic conventional radiation
therapy and IMRT, and concluded that definitive whole pelvic IMRT
was associated with significantly less toxicity compared with whole
pelvic conventional radiation therapy and had a comparable clinical
outcome.
Helical tomotherapy is a novel radiotherapy method
for IMRT combined with image guided radiation therapy based on
computed tomography. Using this method, high conformity and
critical organ sparing ability are expected. However, there are
still a small number of institutions practically using helical
tomotherapy. Although IMRT for the treatment of uterine cervical
cancer has been described in practical guidelines from the USA and
Japan as well as in the reports mentioned above, there are only a
few reports on helical tomotherapy as definitive radiotherapy for
cervical cancer. Herein, we analyzed the feasibility and efficacy
of helical tomotherapy during concurrent chemoradiotherapy for
cervical cancer.
Materials and methods
We retrospectively reviewed the medical records of
13 patients who underwent concurrent chemoradiotherapy using
helical tomotherapy (Tomo HD system; Accuray, Inc., Madison, WI,
USA) for cervical cancer at Wakayama Medical University Hospital
between 2013 and 2015. More than 2 years have passed since the
beginning of each patient's treatment. We also examined 15 patients
who underwent concurrent chemoradiotherapy using conventional
radiotherapy (CRT) between 2008 and 2013 at our institution for
comparison. We included all patients who underwent concurrent
chemoradiotherapy in the period. Patients undergoing hysterectomy
before concurrent chemoradiotherapy were excluded. The data of age,
clinical stage, histological subtype, tumor size, and
chemotherapy/radiotherapy regimen were extracted from patients'
files and analyzed. Written informed consent was obtained from the
patients, and patient anonymity was preserved.
Radiotherapy
The radiotherapy was composed of external beam
radiotherapy (EBRT) and high dose rate intracavity brachytherapy
(ICBT). We used 3-dimensional conformal radiotherapy based on CT
planning as the conventional radiotherapy. In the CRT group,
4-field technique was performed while anteroposterior-
posteroanterior technique was used in center split. The prescribed
dose for PTV, received by 95% of the volume, was 45–50 Gy for the
whole pelvis and 5–10 Gy for para-aortic lymph nodes in the
tomotherapy group. The dose of ICBT was 11.5 Gy in the tomotherapy
group. On the other hand, the dose of irradiation was 45–50 Gy, for
the whole pelvis including the center split irradiation and 12–14
Gy for para-aortic lymph nodes, and the dose of ICBT was 23 Gy at
point A in the CRT group. The distribution of irradiation dose in
the CRT group was determined in compliance with General Rules for
Clinical and Pathological Study of Uterine Cervical Cancer in Japan
(1997). Para-aortic irradiation was carried out for patients with
common iliac lymph node metastases in both groups. The biologically
effective dose was 71.2–79.2 Gy in the tomotherapy group and
72.2–72.3 Gy in the conventional radiotherapy group. The cumulative
equivalent dose (EQD2) was 59.3–66 Gy in the tomotherapy group, and
60.2–60.3 Gy at point A in the conventional radiotherapy group.
Chemotherapy
The regimens of chemotherapy concurrent with
irradiation were cisplatin: 40 mg/m2 weekly for 6
cycles, nedaplatin: 30 mg/m2 weekly for 6 cycles, and
cisplatin + fluorouracil: cisplatin 70 mg/m2 +
fluorouracil 2.8 g/m2/96 h every 3 weeks for 4 cycles in
the helical tomotherapy group. The regimens of the chemotherapy
were cisplatin: 40 mg/m2 weekly for 6 cycles and
nedaplatin: 30 mg/m2 weekly for 6 cycles in the CRT
group.
Statistics
Fisher's exact test was used to compare each
parameter of patients' characteristics, adverse effect, and overall
response between both groups. Progression-free survival (PFS) was
analyzed by the Kaplan-Meier method and significance was determined
by the log-rank test. P<0.05 was considered to indicate a
statistically significant difference. All statistical analyses were
carried out using the software JMP Pro version 13 (SAS Institute,
Inc., Cary, NC, USA).
Results
Patients characteristics
The characteristics of patients are shown in
Table I. The median age of patients
treated with helical tomotherapy was 60 (range, 35–71) and median
age of patients treated with CRT was 57 (range, 43–77). The median
follow-up period was 27 months (range, 3–46) for the patients
treated with helical tomotherapy and 35 months (range, 7–88) for
the patients treated with CRT. There were significant differences
between the helical tomotherapy group and the CRT group in the
methods of chemotherapy (P=0.04) and radiotherapy (P=0.02). The
single agent regimen of cisplatin was carried out for 14 out of 15
patients in the CRT group. There were significantly more patients
who underwent ICBT in the CRT group than in the tomotherapy group.
There were no significant differences between the groups with
regard to the clinical stage, histological subtypes, or tumor
size.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
|
| Tomotherapy
(n=13) | CRT (n=15) |
|
|---|
|
|
|
|
|
|---|
| Variables | n (%) | n (%) | P-value |
|---|
| Age median
(range) | 60 (35–71) | 57 (43–77) | 0.47 |
| FIGO stage |
|
| 0.35 |
| IB | 1 (7.7) | 0 |
|
| IIA | 0 | 1 (6.7) |
|
| IIB | 4 (30.8) | 4 (26.7) |
|
| IIIA | 2 (15.4) | 0 |
|
| IIIB | 4 (30.8) | 7 (46.7) |
|
| IVA | 1 (7.7) | 3 (20) |
|
| IVB | 1 (7.7) | 0 |
|
| Histological
subtype |
|
| 0.34 |
| SCC | 13 (100) | 14 (93.3) |
|
|
Adenocarcinoma | 0 | 1 (6.7) |
|
| Tumor size |
|
| 0.75 |
| ≤40
mm | 2 (15.4) | 3 (20.0) |
|
| >40
mm | 11 (84.6) | 12 (80.0) |
|
| Chemotherapy |
|
| 0.04 |
| CDDP | 7 (53.8) | 14 (93.3) |
|
| CDGP | 3 (23.1) | 1 (6.7) |
|
| CDDP
+5-Fu | 3 (23.1) | 0 |
|
| Radiotherapy |
|
| 0.02 |
| With
ICBT | 9 (69.2) | 15 (100.0) |
|
| Without
ICBT | 4 (30.8) | 0 |
|
Adverse effect and overall
response
There was a significant difference between the
helical tomotherapy group and the CRT group in the frequency of
G3/4 thrombocytopenia (P=0.049) (Table
II). However, the platelet count spontaneously recovered
without transfusion. There were no significant differences between
the groups in the frequency of G3/4 neutropenia, diarrhea, or
intestine injury (Table II).
Patients with G3/4 thrombocytopenia tended to have undergone
extended-field irradiation of the para-aortic lymph nodes as an
initial treatment, but it was not significant (P=0.0675). Two out
of three patients with G3/4 thrombocytopenia underwent combination
chemotherapy consisting of two anticancer agents. In both groups,
complete response (CR) or partial response (PR) was achieved by all
patients. The rates of CR in the tomotherapy group and the CRT
group were 84.6 and 73.3%, respectively. The rates of PR in the
tomotherapy group and the CRT group were 15.4 and 26.7%,
respectively. There were no statistically significant differences
between the helical tomotherapy group and the CRT group in the
ratio of CR and PR (Table
III).
 | Table II.Adverse effects. |
Table II.
Adverse effects.
|
| Tomotherapy
(n=13) | CRT (n=15) |
|---|
|
|
|
|
|---|
| Variables | Grade 3 | Grade 4 | Grade 3 | Grade 4 | P-value |
|---|
| Acute toxicity |
|
|
|
|
|
|
Neutropenia | 6 (46.2%) | 0 | 5 (33.3%) | 1 (6.7%) | 0.74 |
|
Thrombocytopenia | 3 (23.1%) | 0 | 0 | 0 | 0.049 |
|
Diarrhea | 0 | 0 | 3 (20%) | 0 | 0.088 |
| Late toxicity |
|
|
|
Small/large intestine | 0 | 0 | 0 | 1 (6.7%) | 0.34 |
 | Table III.Overall response. |
Table III.
Overall response.
|
| Tomotherapy
(n=13) | CRT (n=15) |
|
|---|
|
|
|
|
|
|---|
| Response | n (%) | n (%) | P-value |
|---|
| Complete | 11 (84.6) | 11 (73.3) | 0.468 |
| Partial | 2 (15.4) | 4 (26.7) |
|
Clinical outcome
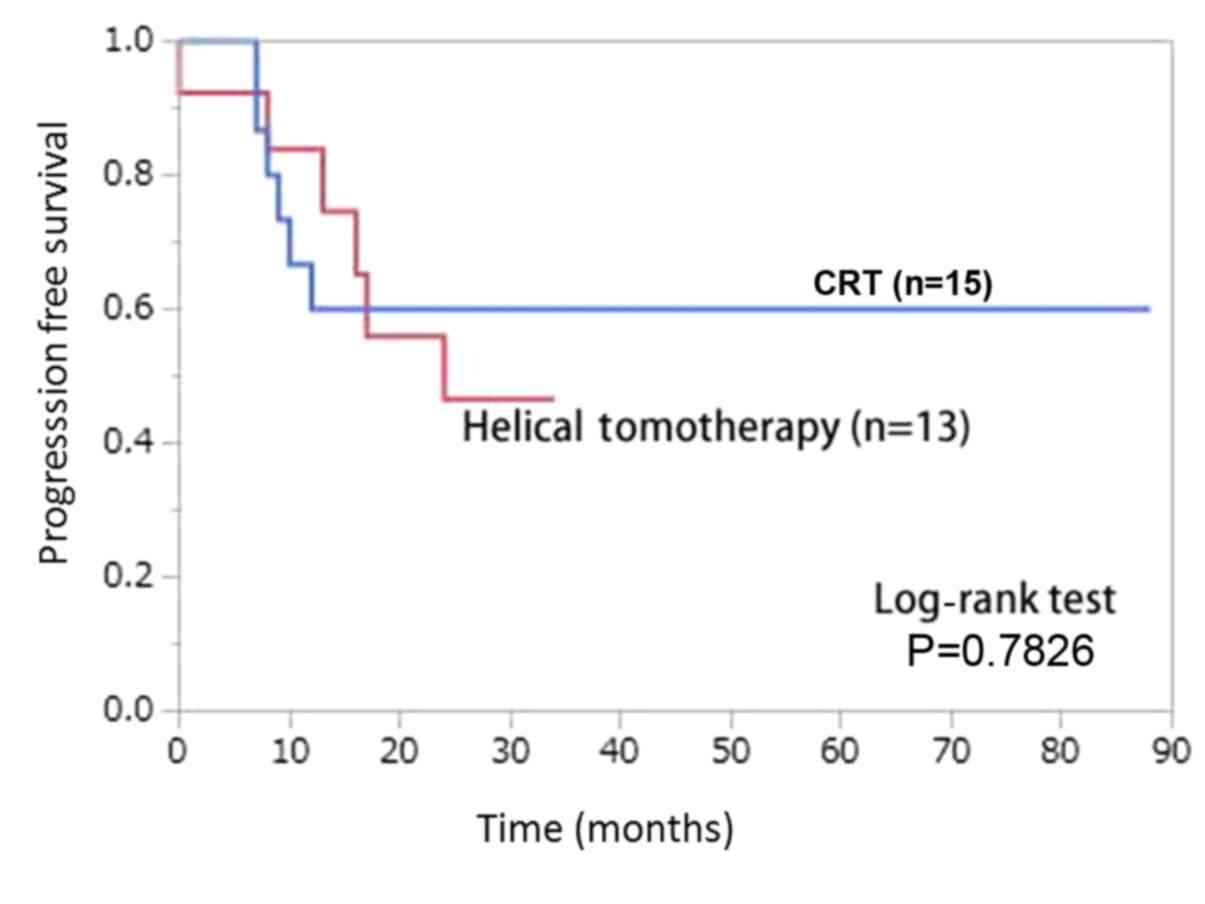
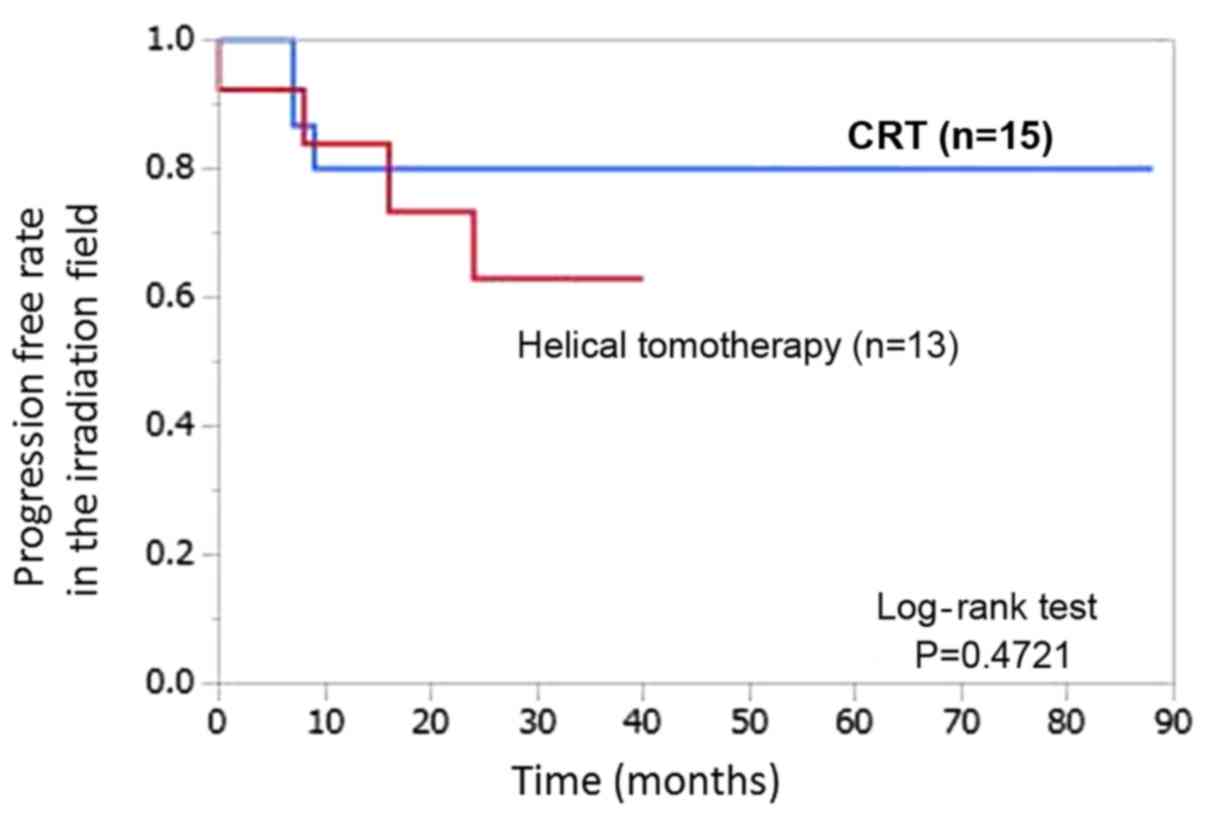
There were no significant differences in PFS
(P=0.7826; Fig. 1) or PFS in the
irradiation field (P=0.4721; Fig. 2)
between the helical tomotherapy group and the CRT group. In the
helical tomotherapy group, 4 patients had recurrence in the
irradiation field: Primary lesion in 1, corpus uteri in 1, pelvic
lymph node in 1, and supraclavicular lymph node in 1. In the
helical tomotherapy group, 2 patients had pulmonary metastases. In
the helical tomotherapy group, no patient died of cervical cancer.
In the CRT group, 3 patients had recurrence of the primary lesion
in the irradiation field. In the CRT group, 2 patients had
metastases in the para-aortic lymph node, and one patient had
hepatic metastasis.
Discussion
Although IMRT for the treatment of uterine cervical
cancer has been described in the practical guidelines by the USA
and Japan as well as in the studies mentioned above, there are only
a few reports on helical tomotherapy as definitive radiotherapy for
cervical cancer. Schwarz et al (6) reported that postoperative external IMRT
for cervical cancer delivered with helical tomotherapy and high
dose rate brachytherapy with or without chemotherapy was feasible,
and had acceptable acute and chronic toxicity. Chang et al
(7) described that IMRT delivered
with helical tomotherapy and high dose rate brachytherapy with or
without chemotherapy for definitive treatment of cervical cancer
was feasible, with acceptable levels of chronic toxicity. Jouglar
et al (8) found that
extended-field helical tomotherapy to the para-aortic nodes was
associated with low rates of acute gastrointestinal and
genitourinary toxicities, with early survival and locoregional
control similar with in other published series. Marnitz et
al (9) compared IMRT delivered
by helical tomotherapy with conventional IMRT for primary
chemoradiation in cervical cancer patients, and concluded that both
helical tomotherapy and conventional IMRT provided optimal
treatment of cervical cancer patients, and that the helical
tomotherapy technique was significantly favorable regarding
conformity, homogeneity, and small bowel sparing.
Problems due to motion of the target and surrounding
organs at risk have interfered with IMRT becoming the definitive
treatment for cervical cancer. However, helical tomotherapy has the
advantage of image guided radiation therapy based on daily 3D
megavoltage CT imaging, and this advantage may overcome the issues
with motion of the target and surrounding organs in the definitive
treatment of cervical cancer.
In this analysis, there was a significant difference
in the method of chemotherapy and the frequency of ICBT. We
administered nedaplatin to patients with poor renal function or
hydronephrosis in both groups. Cisplatin and fluorouracil were
administered to 3 patients in the helical tomotherapy group; one
with a bulky stage IIB tumor, one with para-aortic and mediastinal
metastases of T2BN1M1, and the other with stage IVB pulmonary
metastases. Seven out of 13 patients received paraaortic
irradiation and 9 out of 13 patients received ICBT in the helical
tomotherapy group. Of the 4 patients without ICBT, 3 had
non-para-aortic distant metastases, and one patient had too bulky
of a tumor to insert the ICBT tandem in the helical tomotherapy
group. In contrast, 4 out of 15 patients received para-aortic
irradiation and all patients received ICBT in the CRT group.
Although patients with distant metastases, excluding the
para-aortic lymph nodes, were not treated with concurrent
chemoradiotherapy during CRT, advanced disease with distant
metastases is recently treated with concurrent chemoradiotherapy
using helical tomotherapy. The disease progression was thought to
be related with the differences in chemotherapy and ICBT between
the groups, although there were no significant differences in
clinical stage between them. There was a significant difference
between the helical tomotherapy group and the CRT group in the
frequency of G3/4 thrombocytopenia (P=0.049; Table II). However, the platelet count
spontaneously recovered without transfusion. There was a tendency
for patients with G3/4 thrombocytopenia to have undergone
extended-field irradiation of the para-aortic lymph nodes as an
initial treatment, but it was not significant (P=0.0675). Two out
of three patients with G3/4 thrombocytopenia underwent combination
chemotherapy with cisplatin and fluorouracil. In the helical
tomotherapy group, there were more advanced cases with distant
metastases compared with in the CRT group, and disease progression
led to the selection of multiagent chemotherapy. In our study,
there were no patients with acute or late gastrointestinal adverse
effects in the tomotherapy group. Chang et al (7) previously reported that one out of 15
patients who underwent definitive chemoradiotherapy delivered with
helical tomotherapy developed a chronic grade 3 gastrointestinal
complication. Gandhi et al (5) reported that one out of 22 patients who
underwent definitive chemoradiotherapy delivered with IMRT
developed an acute ≥grade 3 gastrointestinal complication and no
patient developed acute ≥grade 3 genitourinary complications.
In the present study, there were no significant
differences in PFS (P=0.7826) or progression-free rate in the
irradiation field (P=0.4721) between the helical tomotherapy group
and the CRT group. The 2-year progression-free rate was 46.6 and
60.0% in the helical tomotherapy and CRT groups, respectively. The
2-year progression-free rate in the irradiation field was 62.9 and
80.0% in the helical tomotherapy and CRT groups, respectively. In
the helical tomotherapy group, 6 out of 13 patients had recurrence;
two with para-aortic metastases, two with distant metastases not in
the para-aortic lymph nodes, and the remaining two had bulky stage
IIB tumors before the start of the therapy. In the CRT group, 6 out
of 15 patients had recurrence; three had stage IIIB tumors, two had
stage IVA tumors, and the other had a bulky stage IIB tumor before
the start of the therapy. In both groups, careful observation was
necessary in terms of recurrence of stage III, IV, and bulky IIB
tumors. There were no significant differences in the prognosis
between both groups, but the helical tomotherapy group included
more patients with distant metastases. If those with distant
metastases, including para-aortic lymph nodes, are excluded from
the helical tomotherapy group, the prognosis based on the data may
improve.
In conclusion, adverse events from concurrent
chemoradiotherapy using helical tomotherapy were acceptable and
clinically controllable. Helical tomotherapy is efficient during
concurrent chemoradiotherapy for advanced cervical cancer.
Prospective studies involving more patients for longer follow-up
periods are needed to assess the difference in oncological outcome
and toxicity between helical tomotherapy and conventional
radiotherapy.
Acknowledgements
The authors thank Dr Takahiro Chiba (Department of
Radiation Oncology, Wakayama Medical University) for his assistance
of data management on radiotherapy planning.
Funding
No funding was received.
Availability of data and materials
The datasets analyzed during the current study are
available from the corresponding author on reasonable request.
Authors' contributions
All authors participated in the conception and
design of the study. YM, YT, TY, MM, NS, NO and SM obtained the
data. YM analyzed the data and drafted the manuscript. KI revised
the manuscript prior to submission. In addition, KI and YM were
major contributors in designing the study. All authors have read
and approved the final version of the manuscript.
Ethics approval and consent to
participate
The current study was approved by the ethical
committee of Wakayama Medical University (reference no. 2337).
Patient consent was also obtained.
Patient consent for publication
The patients provided written informed consent for
the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Keys HM, Bundy BN, Stehman FB, Muderspach
LI, Chafe WE, Suggs CL III, Walker JL and Gersell D: Cisplatin,
radiation and adjuvant hysterectomy compared with radiation and
adjuvant hysterectomy for bulky stage IB cervical carcinoma. N Engl
J Med. 340:1154–1161. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tseng CJ, Chang CT, Lai CH, Soong YK, Hong
JH, Tang SG and Hsueh S: A randomized trial of concurrent
chemoradiotherapy versus radiotherapy in advanced carcinoma of the
uterine cervix. Gynecol Oncol. 66:52–58. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Peters WA III, Liu PY, Barrett RJ II,
Stock RJ, Monk BJ, Berek JS, Souhami L, Grigsby P, Gordon W Jr and
Alberts DS: Concurrent chemotherapy and pelvic radiation therapy
compared with pelvic radiation therapy alone as adjuvant therapy
after radical surgery in high-risk early-stage cancer of the
cervix. J Clin Oncol. 18:1606–1613. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kirwan JM, Symonds P, Green JA, Tierney J,
Collingwood M and Williams CJ: A systematic review of acute and
late toxicity of concomitant chemoradiation for cervical cancer.
Radiother Oncol. 68:217–226. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gandhi AK, Sharma DN, Rath GK, Julka PK,
Subramani V, Sharma S, Manigandan D, Laviraj MA, Kumar S and
Thulkar S: Early clinical outcomes and toxicity of intensity
modulated versus conventional pelvic radiation therapy for locally
advanced cervix carcinoma: A prospective randomized study. Int J
Radiat Oncol Biol Phys. 87:542–548. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Schwarz JK, Wahab S and Grigsby PW:
Prospective phase I–II trial of helical tomotherapy with or without
chemotherapy for postoperative cervical cancer patients. Int J
Radiat Oncol Biol Phys. 81:1258–1263. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chang AJ, Richardson S, Grigsby PW and
Schwarz JK: Split-field helical tomotherapy with or without
chemotherapy for definitive treatment of cervical cancer. Int J
Radiat Oncol Biol Phys. 82:263–269. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jouglar E, Thomas L, de la Rochefordière
A, Noël G, Le Blanc-Onfroy M, Delpon G, Campion L and Mahé MA:
Toxicity and early clinical outcomes in cervical cancer following
extended field helical tomotherapy to para-aortic lymph nodes.
Cancer Radiother. 20:794–800. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Marnitz S, Lukarski D, Köhler C,
Wlodarczyk W, Ebert A, Budach V, Schneider A and Stromberger C:
Helical tomotherapy versus conventional intensity-modulated
radiation therapy for primary chemoradiation in cervical cancer
patients: An intraindividual comparison. Int J Radiat Oncol Biol
Phys. 81:424–430. 2011. View Article : Google Scholar : PubMed/NCBI
|