Introduction
Colorectal adenocarcinoma synchronously metastatic
to the skin and breast is extremely rare. A survey reported that
secondary neoplasms of the breast account for 0.43% of all breast
malignancies (1), and the colorectum
as the primary site is even rarer. Cutaneous metastasis from
colorectal cancer is also a rare (3%) event (2). The majority of cutaneous or breast
metastases indicate widely disseminated disease and are associated
with poor clinical outcome. Breast cancer frequently metastasizes
to the skin in women (3), and the
clinical manifestations of cutaneous metastasis vary widely. Breast
metastasis may be mistakenly considered as the primary lesion,
leading to misdiagnosis and inappropriate therapeutic strategy,
such as unnecessary surgical intervention and chemotherapy regimen
(4). We herein present the case of
an 68-year-old female patient with synchronous cutaneous and breast
metastases as the initial presentation of recurrent colorectal
adenocarcinoma, without visceral organ metastasis.
Case report
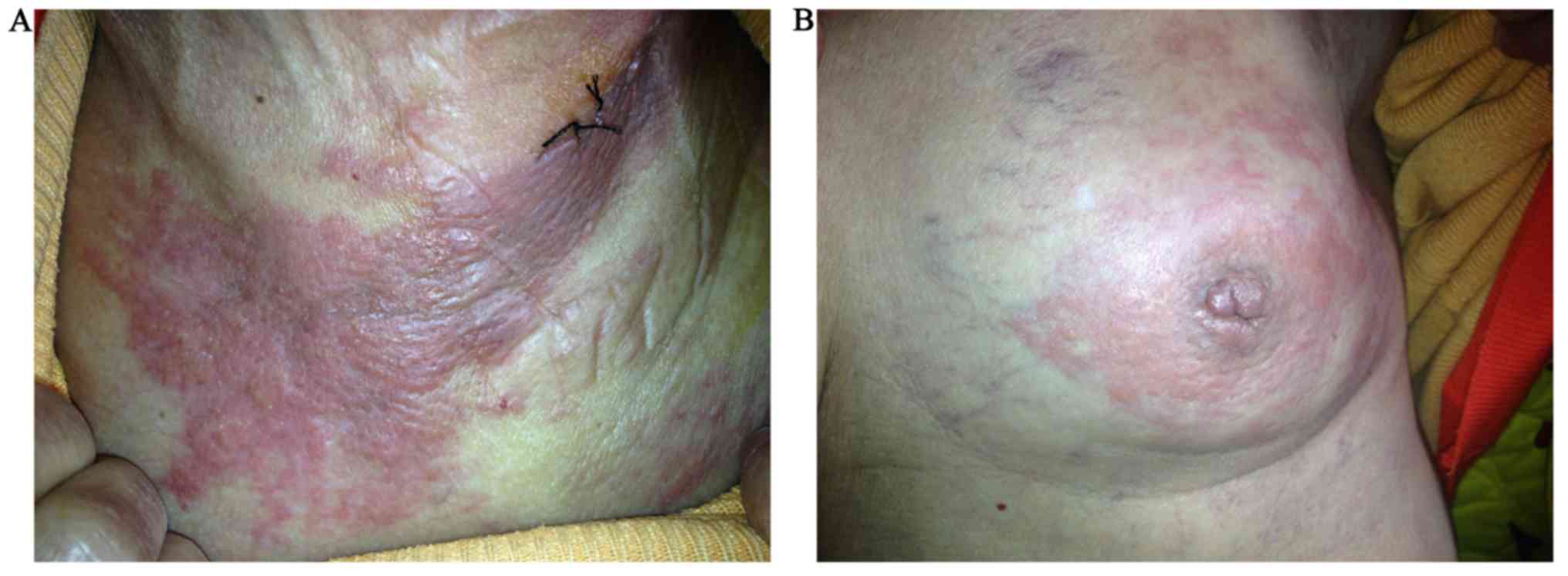
A 68-year-old woman visited a dermatologist in
February 2017 with rapidly progressing pruritic skin lesions on her
chest and neck for 1 month (Fig.
1A). The patient reported no melena, nausea, headache, cough,
chest pain or weight loss. Physical examination revealed multiple
painless, crimson, irregular, indurated papules and plaques
distributed along the upper chest and anterolateral aspect of the
left neck. On physical examination, there was diffuse redness on
the left breast and thickening of the skin with nipple retraction.
A palpable, painless isolated tumor measuring 4×3×3 cm with
irregular borders was detected in the inner upper quadrant of the
left breast, at a distance of 1.5 cm from the nipple (Fig. 1B). No masses were detected on
computed tomography scans of the chest, abdomen and other
organs.
The patient had a history of colorectal
adenocarcinoma in September 2010, initially manifesting as
hematochezia for 6 months. Colonoscopy revealed a friable,
cauliflower-like mass occupying 40% of the rectal circumference.
The patient was diagnosed with stage IIA (Dukes' A) rectal cancer
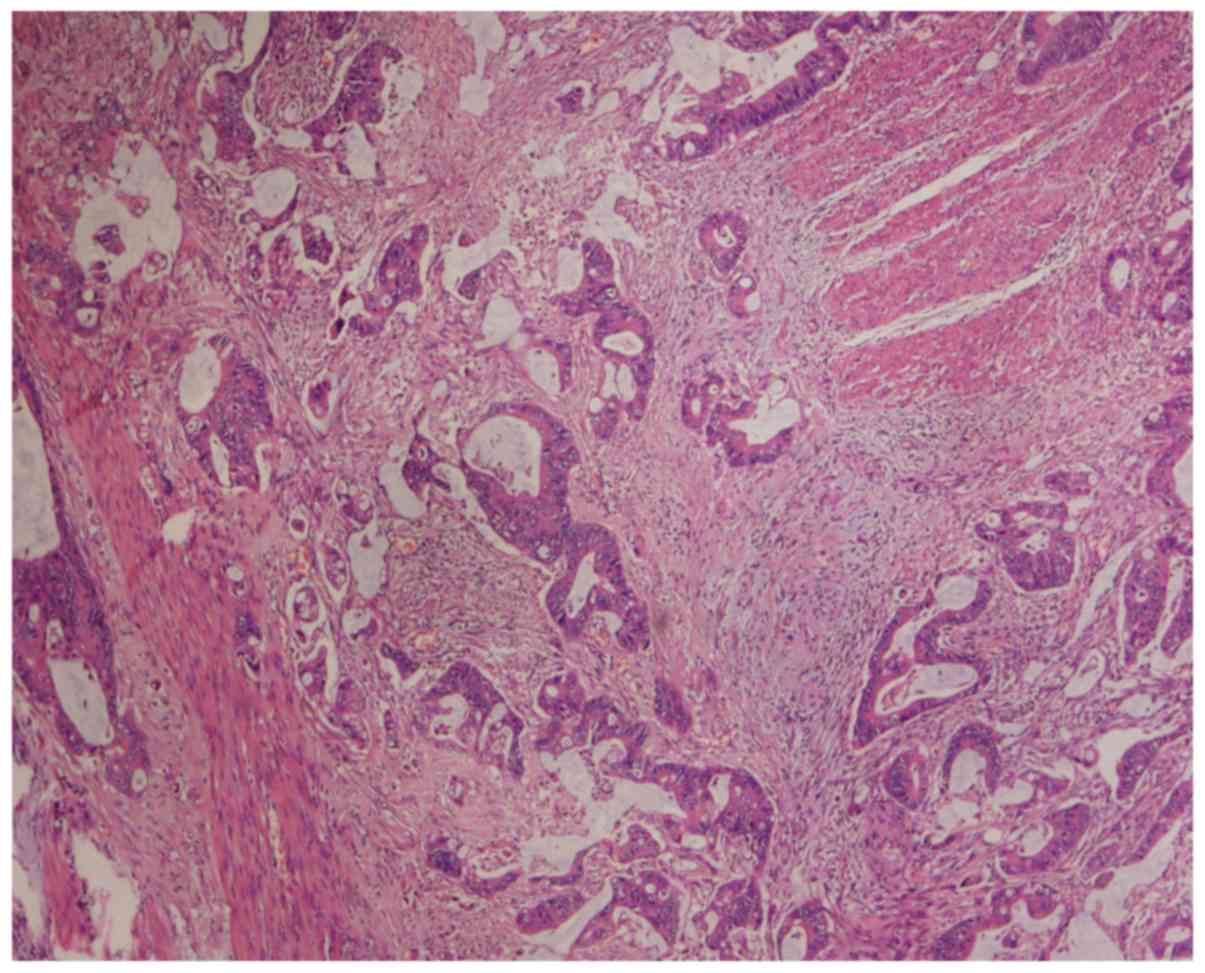
and abdominoperineal resection was performed. Histopathological
examination revealed tubular adenocarcinoma (Fig. 2). The patient had a progression-free
survival of 6 years after receiving 6 cycles of oxaliplatin,
5-fluorouracil and leucovorin treatment (FOLFOX regimen).
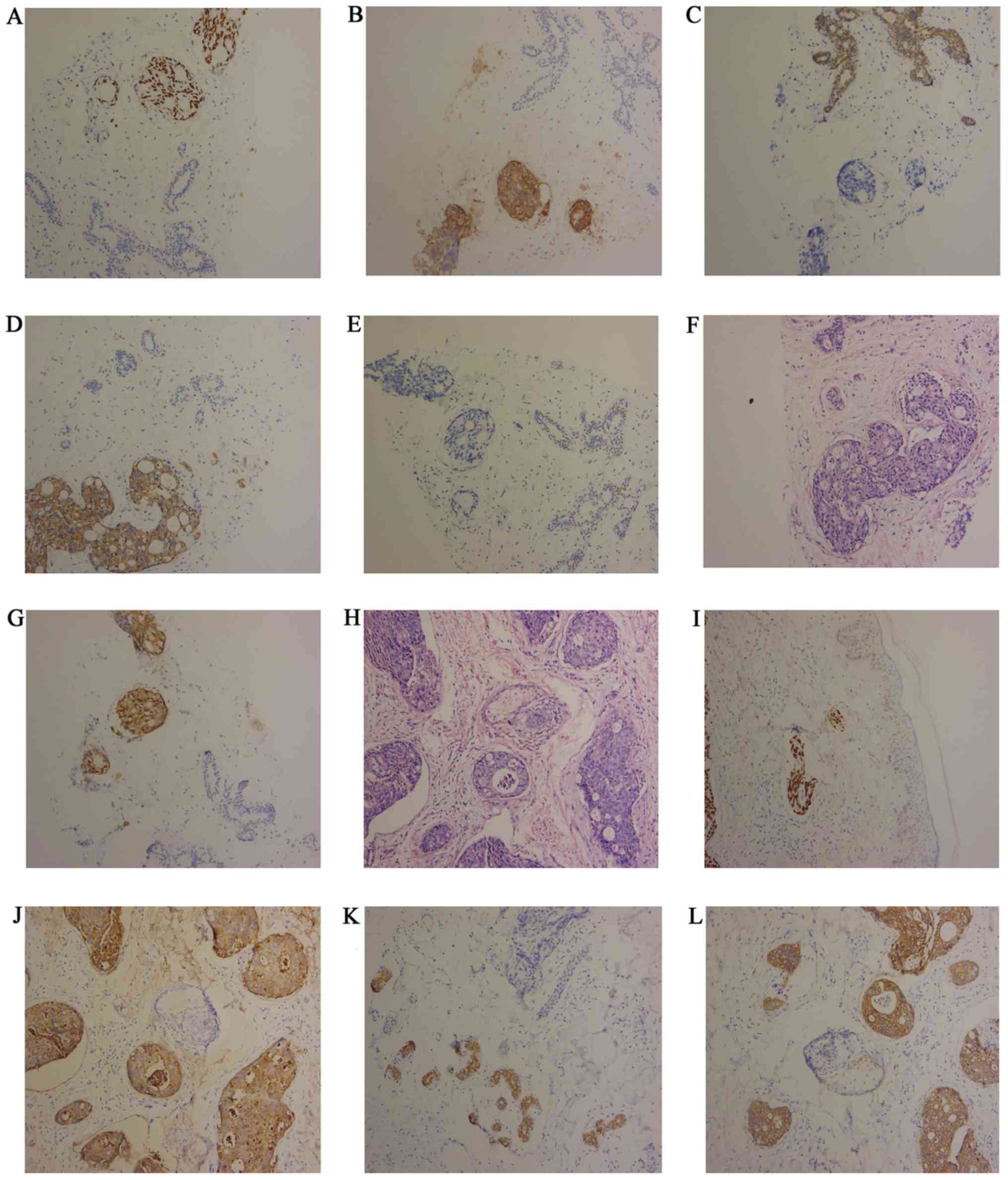
Cutaneous lesion specimens and 4-mm punch biopsies
were obtained from the left neck and breast in February 2017,
respectively. The results of the immunohistochemical examination
were negative for estrogen receptor (ER), progesterone receptor
(PR) and cytokeratin (CK)7, and positive for CK20, CDX2, villin and
carcinoembryonic antigen (CEA), with a MIB-1 labeling index of 90%
(Fig. 3A-L). A diagnosis of
metastatic rectal adenocarcinoma to the breast and skin was thus
confirmed. The patient received four cycles of FOLFIRI
chemotherapy, with marked improvement of the breast tumor and
cutaneous lesions on the chest and neck. Unfortunately, the patient
suffered grade IV adverse effect include nausea and diarrhea during
chemotherapy with resulting poor compliance. Alternative
chemotherapy regimen such as FOLFOX was refused. The patient
eventually succumbed to multiple visceral metastases after
treatment discontinuation in May 2017.
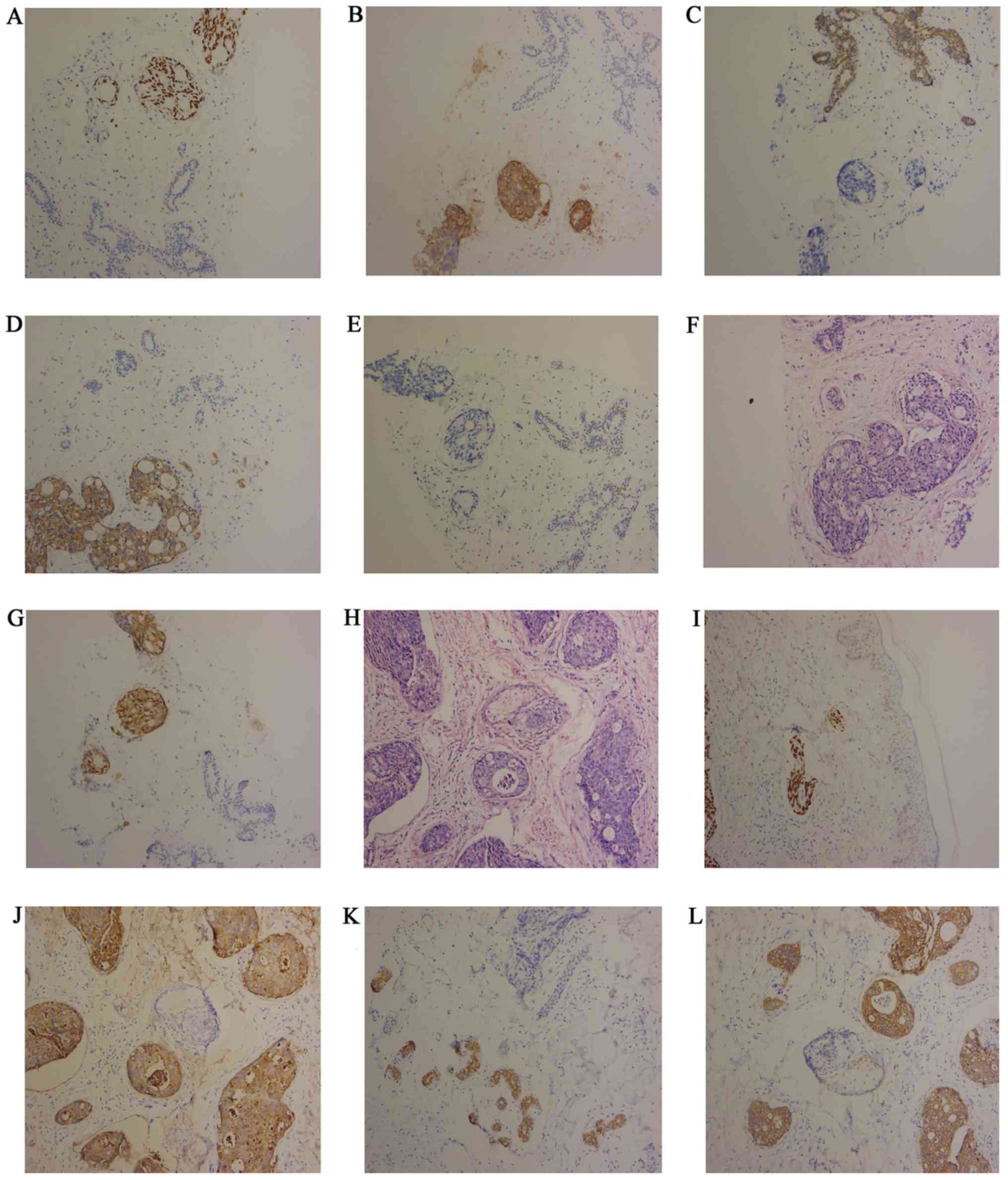 | Figure 3.Immunohistochemical analysis of left
breast 4-mm punch biopsies: (A) CDX2, (B) CEA, (C) CK7, (D) CK20,
(E) ER, (F) H&E stain, (G) villin. Immunohistochemical analysis
of left neck cutaneous lesion specimens: (H) H&E, (I) CDX2, (J)
CEA, (K) CK7, (L) CK20 (magnification, ×100). CEA, carcinoembryonic
antigen; CK, cytokeratin; ER, estrogen receptor; H&E,
hematoxylin and eosin staining. |
Discussion
Breast metastases most frequently originate from
cancers of the contralateral breast, followed by the skin, lung,
ovary, melanoma and lymphoma (1).
The majority of breast metastases manifest as palpable, painless
tumors with rapid growth that are not accompanied by red thickened
skin or nipple retraction (4). Ota
et al (5), described a rare
case of breast metastasis from lung adenocarcinoma with redness of
the overlying skin. These patients commonly have a poor outcome.
DeLair et al (6), reported a
study including 85 cases of non-mammary metastases to the breast
between 1990 and 2010, with a median survival of only 15 months
after diagnosis. Zhou et al (7) reported 28 cases of non-mammary
malignancies metastatic to the breast; on average, breast
metastasis was reported to appear 32 months (range, 0–228 months)
following primary diagnosis. Schaekelford et al (8) reported that, in the majority of the
cases (55%), the metastases were to the left breast, with 6 (30%)
cases metastatic to the right breast; localization in the upper
outer quadrant accounted for 53% of the cases. When a breast lump
is detected, mammography and magnetic resonance imaging should
first be performed. However, differentiating between primary and
metastatic breast cancer mainly relies on immunohistochemistry. The
immunohistochemical characteristics of primary breast cancer are
CK20−, CK7+, and other markers (ER, PR and
human epidermal growth factor receptor 2) may vary (9).
Cutaneous metastases can be the first manifestation,
presenting as rapidly growing painless subcutaneous or dermal
nodules, inflammatory dermatosis, macules and plaques (10). The most common skin metastatic sites
are the abdomen and perineum. Cutaneous metastases differ between
men and women; lung cancer and melanoma are the main primary tumors
in men, while breast and colorectal cancer are the predominant
types in women. Visceral cancer metastasis to the skin is often
associated with a poor prognosis. Dehal et al (11) reported a mean recurrence time of
cutaneous metastasis from rectal adenocarcinoma of 18 months and a
mean survival of ~10 months after the appearance of metastases
(median, 4 months; range, 1–56 months). On average, cutaneous
metastasis is reportedly associated with a survival of 7.5 months
following the diagnosis of cancer (12). The majority of cutaneous metastases
present as painless nodules, and can be mistaken for sebaceous
cysts, lipomyomas or neurofibromas. The ultimate diagnosis of
cutaneous metastasis relies on pathological and morphological
characteristics. The immunohistochemical properties are often
consistent with the primary tumor (13).
In the present case, during follow-up chest,
abdominal CT, and pelvic MRI every 3–6 months for 2 years, then
every 6 months for a total of 5 years in Department of Oncology,
Chongqing Qiangjiang Central Hospital, no distant metastases or
lacal recurrence was found. The patient was lost to follow-up after
the fifth year for economic reasons. The initial presentation was
the skin lesions and, on subsequent physical examination, a breast
mass was detected. The dermatosis raised the suspicion of breast
malignancy. In all cases, diagnosis must be confirmed by
pathological examination. Radiological imaging, such as mammography
or magnetic resonance imaging, may be applied.
Fluorodexyglucose-positron emission tomography combined with CEA
measurement can be useful for determining malignant characteristics
of tumor lesions (14). In the
present case, a skin excisional specimen and punch biopsy were
obtained from the neck and the left breast, respectively.
Differentiating between breast and colorectal carcinoma as the
primary malignancy may be difficult based on histomorphology alone.
On immunohistochemical examination, the biopsy specimen was
CK7−, CK20+, CDX2+,
villin+, ER− and PR−. Therefore,
the malignancy was considered to originate from the
gastrointestinal tract; combined with the patient's medical
history, the diagnosis of colorectal cancer with breast and skin
metastasis was confirmed. CK7, CK20, CDX2 and villin are specific
immunohistochemical markers used for the identification of breast
and colorectal adenocarcinoma. The great majority of breast tumors
are CK7+ and CK20−, while colorectal
adenocarcinomas are usually CK7− and CK20+.
Gastric carcinoma is also usually CK7+. CDX2 expression
is more common in gastrointestinal tumors, and 97% of all
colorectal carcinomas are CDX2-positive (15), whereas thus far there has been no
report of CDX2-positive breast cancer. The first-line palliative
chemotherapy for metastatic colorectal cancer includes
irinotecan/5-fluorouracil (FOLFIRI), FOLFOX or XELOX combination
regimens with targeted agents. Our patient received an
irinotecan-based regimen, but developed severe diarrhea.
Second-line treatment should include oxaliplatin (FOLFOX and CAPOX)
and an anti-VEGF (bevacizumab) or anti-EGFR (cetuximab) antibody in
cases in which RAS mutation has been excluded.
Cutaneous metastasis from extramammary cancer may be
mistaken as primary breast tumor metastatic to the skin, leading to
misdiagnosis and mistreatment. The management of colorectal
metastases differ from that of primary breast cancer, and
mastectomy may be unnecessary. Distinguishing between a primary and
metastatic breast tumor may be difficult. The main points are
listed as follows: i) A prior or current medical history of
malignancy should prompt referral to an oncologist and
multidisciplinary team; ii) it need to have a high suspicion of
metastatic breast lump especially malignant tumor medical history,
and iii) excisional or punch biopsy with histological and
immunochemical evaluation are the most reliable diagnostic
methods.
In conclusion, when abnormal changes are detected in
the skin and breast, they should raise the suspicion of metastatic
tumor, particularly in patients with a history of malignancy.
Timely and accurate diagnosis can reduce misdiagnosis and
mistreatment, and improve patient outcome. Biopsy followed by
pathological and immunohistochemical examination is the most
reliable method for distinguishing between primary and metastatic
lesions. A multidisciplinary approach is crucial for avoiding
unnecessary surgical procedures and ensuring optimal patient
management.
Acknowledgements
Not applicable.
Funding
The present study was supported by ChongQing
QianJiang District Science Foundation of China (grant no. Qiankeji
2017033).
Availability of data and materials
Not applicable.
Authors' contributions
XYL and TZ participated in the conception and design
of the case report, and wrote the manuscript. JRD evaluated the
patient and participated in the therapy. LBL evaluated pathological
images. CYL and TZ critically reviewed the manuscript for important
intellectual content. All authors have read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
A signed written consent form was obtained from the
patient's family regarding the publication of the case details and
associated images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Georgiannos SN, Chin J, Goode AW and
Sheaff M: Secondary neoplasms of the breast: A survey of the 20th
Century. Cancer. 92:2259–2266. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nambiar S and Karippot A: Multiple
cutaneous metastases as initial presentation in advanced colon
cancer. Case Rep Gastrointest Med. 2018:80329052018.PubMed/NCBI
|
|
3
|
Seyfried TN and Huysentruyt LC: On the
origin of cancer metastasis. Crit Rev Oncog. 18:43–73. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Vakili S, Sharbatdaran M, Noorbaran A,
Siadati S, Moslemi D and Shafahi S: A case of colon cancer with
breast metastasis and krukenberg tumor. Int J Hematol Oncol Stem
Cell Res. 8:46–50. 2014.PubMed/NCBI
|
|
5
|
Ota T, Hasegawa Y, Okimura A, Sakashita K,
Sunami T, Yukimoto K, Sawada R, Sakamoto K and Fukuoka M: Breast
metastasis from EGFR-mutated lung adenocarcinoma: A case report and
review of the literature. Clin Case Rep. 6:1510–1516. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
DeLair DF, Corben AD, Catalano JP, Vallejo
CE, Brogi E and Tan LK: Non-mammary metastases to the breast and
axilla: A study of 85 cases. Mod Pathol. 26:343–349. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhou S, Yu B, Cheng Y, Xu X, Shui R, Bi R,
Lu H, Tu X and Yang W: Metastases to the breast from non-mammary
malignancies: A clinicopathologic study of 28 cases. Zhonghua Bing
Li Xue Za Zhi. 43:231–235. 2014.(In Chinese). PubMed/NCBI
|
|
8
|
Shackelford RE, Allam-Nandyala P, Bui MM,
Kiluk JV and Esposito NN: Primary colorectal adenocarcinoma
metastatic to the breast: Case report and review of nineteen cases.
Case Rep Med. 2011:7384132011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Noh KT, Oh B, Sung SH, Lee RA, Chung SS,
Moon BI and Kim KH: Metastasis to the breast from colonic
adenocarcinoma. J Korean Surg Soc. 81 (Suppl 1):S43–S46. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nashan D, Müller ML, Braun-Falco M,
Reichenberger S, Szeimies RM and Bruckner-Tuderman L: Cutaneous
metastases of visceral tumours: A review. J Cancer Res Clin Oncol.
135:1–14. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dehal A, Patel S, Kim S, Shapera E and
Hussain F: Cutaneous metastasis of rectal cancer: A case report and
literature review. Perm J. 20:74–78. 2016.PubMed/NCBI
|
|
12
|
Saeed S, Keehn CA and Morgan MB: Cutaneous
metastasis: A clinical, pathological, and immunohistochemical
appraisal. J Cutan Pathol. 31:419–430. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wong CY, Helm MA, Kalb RE, Helm TN and
Zeitouni NC: The presentation, pathology, and current management
strategies of cutaneous metastasis. N Am J Med Sci. 5:499–504.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Van Cutsem E, Cervantes A, Nordlinger B
and Arnold D; ESMO Guidelines Working Group, : Metastatic
colorectal cancer: ESMO Clinical Practice Guidelines for diagnosis,
treatment and follow-up. Ann Oncol. 25 (Suppl 3):iii1–iii9. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bayrak R, Haltas H and Yenidunya S: The
value of CDX2 and cytokeratins 7 and 20 expression in
differentiating colorectal adenocarcinomas from extraintestinal
gastrointestinal adenocarcinomas: Cytokeratin 7-/20+ phenotype is
more specific than CDX2 antibody. Diagn Pathol. 7:92012. View Article : Google Scholar : PubMed/NCBI
|