Introduction
Breast cancer (BC) is the most frequent cancer in
women and the second most common cancer in the general population
worldwide, with approximately two million new cases in 2018
(1). BC mortality rates have
recently decreased in high-income countries, and this declining
trend is likely explained by the early detection and improved
treatment of this cancer (2). The
average 5-year survival rate for women with invasive BC is about
90%, and, since BC is considered a chronic condition, and since
this disorder has a substantial impact on health (3,4), the
long-term follow-up of patients with BC is of particular
importance.
The management of BC survivors is multidisciplinary
and involves a wide range of health professionals (e.g.,
physicians, nurses, psychologists). The specialist in charge of BC
management can be either the oncologist or the gynecologist,
depending on the country in question (5–7).
Although the specific role of general practitioners (GPs) in the
care of individuals with BC is not well defined, the importance of
GPs has increased steadily in recent years. A cross-sectional
questionnaire study including 317 GPs from Norway reported that 17
and 62% of them provided follow-up care to women with BC on a
regular basis less than and more than five years after treatment
respectively (8). More recently, a
survey of 740 cancer patients showed that a substantial proportion
of them visited GP practices for several reasons (e.g., blood test,
complaints and side effects, comorbidities) during their cancer
therapy, and that 54% of participants reported being satisfied with
their primary care physician (9).
These studies have advanced our knowledge about the role played by
GPs in the management of people affected by BC.
Epidemiological studies using survival analyses may
benefit from data obtained from GP practices. However, in order to
be methodologically valid, these studies require the survival time
to be similar to the follow-up time. Unfortunately, little is known
about the duration of follow-up in BC patients in GP practices
after the diagnosis of cancer, and it is possible that BC survivors
change doctors more frequently than people with other conditions
(e.g., osteoporosis, diabetes, hypertension). This may be due to
several reasons, such as the primary care physician's lack of
experience with cancer or his/her lack of empathy (10,11).
Therefore, the goal of this study was to investigate
the suitability of data obtained from general practices in the UK,
France, and Germany for survival analyses in the field of BC.
Materials and methods
Database
This retrospective study was based on data from the
Disease Analyzer database (IQVIA). This database compiles
demographic, clinical, and pharmaceutical data obtained in an
anonymous format from the computer systems used in clinical
practices (2). The quality and
accuracy of the data (e.g., diagnoses, drug prescriptions) are
regularly assessed by IQVIA. Using prescription statistics for
several drugs and age groups for several diagnoses, the Disease
Analyzer database was shown to be representative of clinical
practices in Germany (12). Finally,
this database has already been used for several studies focusing on
BC (13,14).
Patients and outcomes
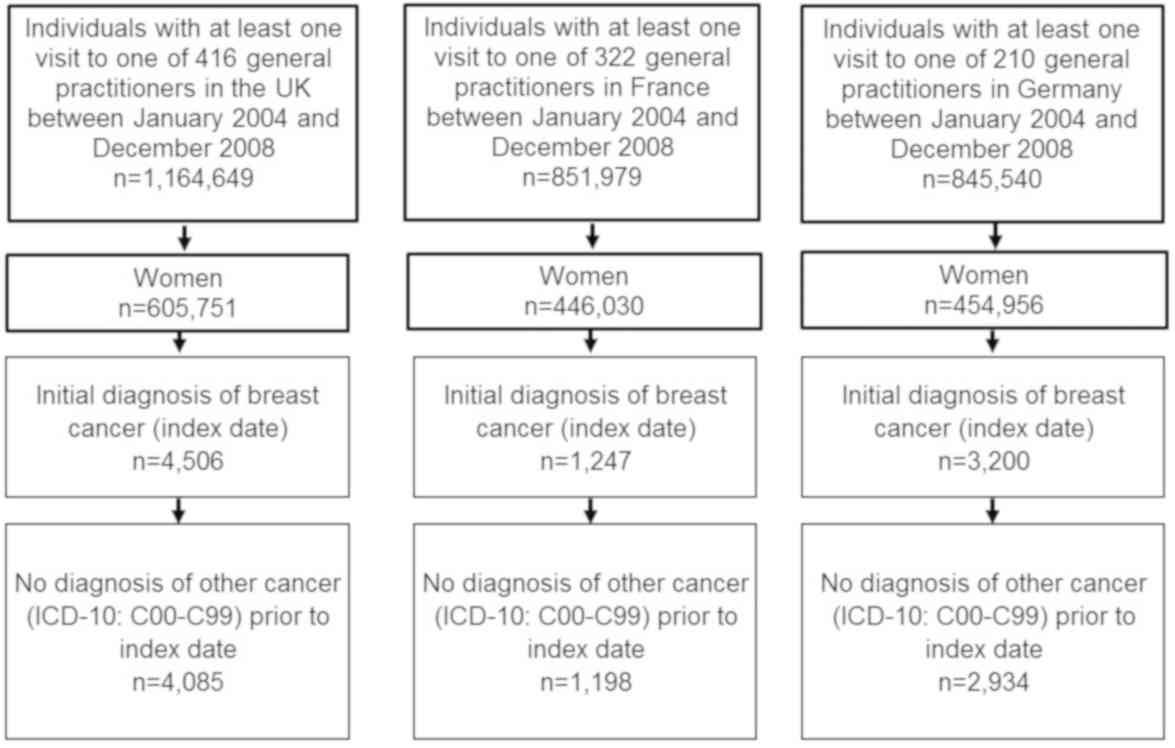
This study included data obtained from women
diagnosed for the first time with BC (International Classification
of Diseases, 10th revision: C50) between 2004 and 2008 in 416, 322,
and 210 GP practices in the UK, France, and Germany respectively
(index year). Women were selected only if they had not been
diagnosed with another cancer (C00-C99) (Fig. 1).
The outcomes of the study were the mean duration of
follow-up in years and the proportion of women with BC followed for
at least five years. These outcomes were studied in different age
subgroups (i.e., ≤50, 51–60, 61–70, >70 years).
Statistical analysis
The present retrospective study used descriptive
statistics only. Differences in the mean follow-up time between the
three countries were tested using Kruskal-Wallis tests (data were
not normally distributed). P<0.05 was considered to indicate a
statistically significant difference. All analyses were carried out
using SAS 9.4 (SAS Institute, Cary, USA).
Results
The study included 4,085 women from the UK, 1,198
from France, and 2,934 from Germany (Table I). The mean age was 60.0 years
(SD=4.7 years) in the UK, 61.7 years (SD=12.6 years) in France and
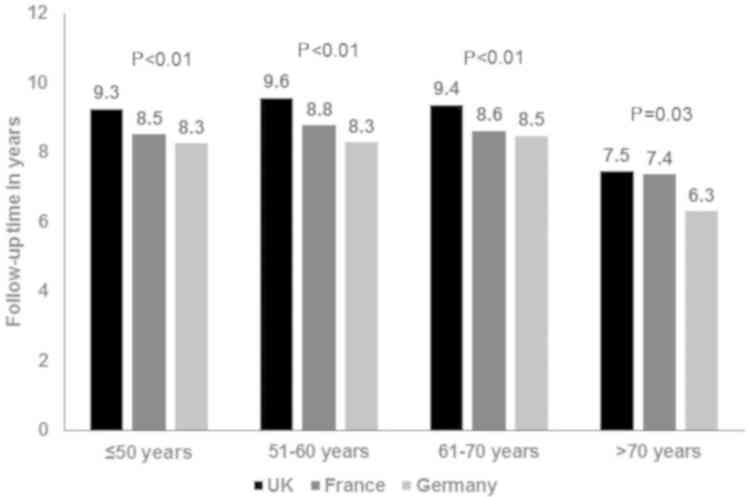
62.5 years (SD=12.4 years) in Germany. The mean duration of
follow-up was 7.5–9.6 years in the UK, 7.4–8.8 years in France and
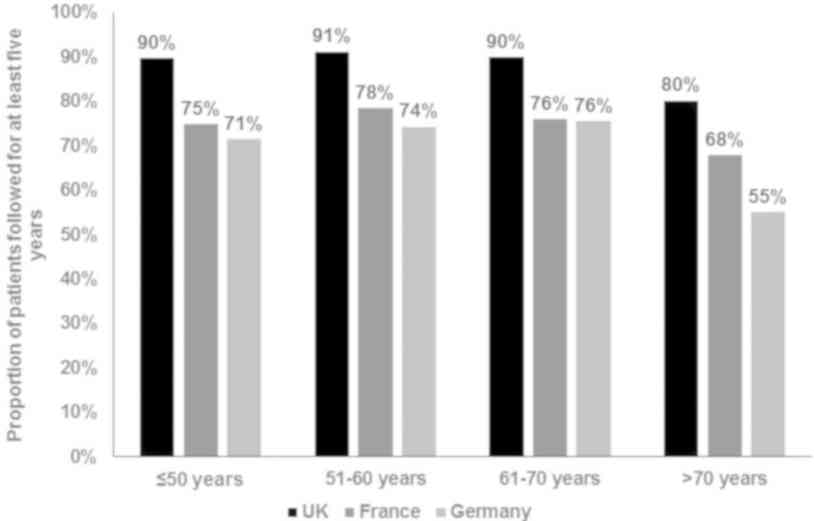
6.3–8.5 years in Germany (P<0.03) (Fig. 2). The proportion of patients followed
for at least five years was 80–91% in the UK, 68–78% in France, and
55–76% in Germany (Fig. 3). Women
aged >70 had the shortest duration of follow-up.
 | Table I.Baseline characteristics of study
patients. |
Table I.
Baseline characteristics of study
patients.
| Variables | UK | France | Germany |
|---|
| Total n | 4,085 | 1,198 | 2,934 |
| Age in years, mean
(SD) | 60.0 (4.7) | 61.7 (12.6) | 62.5 (12.4) |
| Age, years |
| ≤50 | 27.8 | 22.4 | 18.8 |
|
51–60 | 26.2 | 26.4 | 22.9 |
|
61–70 | 21.9 | 23.2 | 30.9 |
|
>70 | 24.1 | 28.0 | 27.5 |
| Year of initial
diagnosis (index year) |
| 2004 | 19.7 | 12.8 | 23.2 |
| 2005 | 19.9 | 18.8 | 20.2 |
| 2006 | 20.5 | 22.8 | 19.2 |
| 2007 | 19.2 | 22.8 | 18.8 |
| 2008 | 20.7 | 22.8 | 18.6 |
Discussion
This is the first study investigating the
suitability of data obtained in general practices for survival
analyses in the field of BC. We found that a substantial proportion
of participants with this cancer were followed for less than five
years in France and Germany. Therefore, the data obtained from
general practices in these two countries may not be appropriate for
survival analyses in the context of BC. By contrast, more than 80%
of BC patients were followed for at least five years in the UK.
Survival analyses, also known as time-to-event
analyses, are a branch of statistics focusing on data where the
dependent variable is the time until the occurrence of an event of
interest (e.g., death, metastasis, depression). One major
characteristic of survival analyses is that data are usually
censored, meaning that the information about the survival time of
some individuals is incomplete (15). Although there are several statistical
methods that take censoring into account, censored samples can
undermine the findings of survival analyses, and one should bear in
mind that not all data are suitable for this type of analysis.
There are several hypotheses that could explain why
the mean duration of follow-up was relatively short and the
proportion of participants followed for more than five years
relatively low in general practices in Germany. For example, a
recent study including 464 Danish GPs reported substantial
variation in empathy between physicians, and this variation was
significantly associated with several factors, such as the
physician-patient relationship and physicians' interactions with
their colleagues (11). Since the
diagnosis of BC has major psychological effects (16), women with BC may be more likely than
women with other chronic conditions (e.g., osteoporosis,
hypertension, diabetes) to change doctors when they identify a lack
of empathy in their physician. Another survey of primary care
physicians showed that lack of formal training with regard to
cancer was a problem for almost half of the responders (47%) when
treating cancer survivors (10).
Therefore, a lack of experience with BC may sometimes motivate
general practitioners to refer women suffering from this condition
to other primary care physicians or specialists (e.g.,
gynecologists, oncologists). In addition, the occurrence of
complications requiring specialized care may explain the
discrepancy between the proportion of participants with BC who were
followed for at least five years in general practices in both
Germany and France (i.e. <80%) and the proportion of BC
survivors five years after cancer diagnosis (i.e. >80%)
(17). For example, a prospective
study of Canadian women with BC estimated that the prevalence of
bone metastases is around 6.5% five years after BC diagnosis
(18), while heart failure and
cardiomyopathy are frequent after adjuvant therapy for this cancer
(19).
Our findings indicate that, although the data
obtained from general practices are important for the improvement
of our understanding of the epidemiology of BC, one major point
should be considered before conducting survival analyses using
these data. Researchers should ensure that the mean follow-up of
patients is sufficient and that it is not vastly different from the
mean survival time. If this is not the case, it may affect the
validity of studies with long-term outcomes, such as mortality at
five years or metastases at 10 years. Since a substantial
proportion of the individuals censored may have simply changed
doctors, using an unique personal identification number for each
patient may help overcome this issue in the future (20). Finally, further research is needed to
gain a better understanding of the factors that may impact the
follow-up of BC survivors in general practices in Europe and other
areas of the world.
The major strengths of this study are the use of
data from three countries and the number of patients available for
analysis. However, the results of this study should be interpreted
in light of several limitations. Firstly, if a participant visited
another GP, this visit would not have been documented in the
database and this participant would have been censored. Secondly,
there was no information on the factors that potentially impacted
the follow-up of women with BC (e.g., lack of empathy displayed by
the primary care physician, a physician's lack of experience with
cancer, development of complications). Finally, it is possible that
there were differences in terms of data completeness between the
UK, France, and Germany, which could explain the discrepancy in the
findings that were observed between these three countries.
Overall, the data obtained from general practices in
France and Germany may be inappropriate for survival analyses in
the field of BC. Future studies are needed to corroborate or refute
the present findings and to investigate the potential factors
impacting the follow-up of women with BC in general practices.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LJ designed the study, interpreted the data, and
drafted and revised the manuscript. KK conceived and designed the
study, performed statistical analysis, interpreted the data, and
revised the manuscript. MK and GH interpreted the data, and revised
the manuscript. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
World cancer research fund. Breast cancer
statistics. https://www.wcrf.org/dietandcancer/cancer-trends/breast-cancer-statistics2018
|
|
2
|
Torre LA, Siegel RL, Ward EM and Jemal A:
Global cancer incidence and mortality rates and trends-an update.
Cancer Epidemiol Biomarkers Prev. 25:16–27. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tian Y, Schofield PE, Gough K and Mann GB:
Profile and predictors of long-term morbidity in breast cancer
survivors. Ann Surg Oncol. 20:3453–3460. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jacob L, Kalder M and Kostev K: Incidence
of depression and anxiety among women newly diagnosed with breast
or genital organ cancer in Germany. Psychooncology. 26:1535–1540.
2017. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lebeau M, Mathoulin-Pélissier S, Bellera
C, Tunon-de-Lara C, Daban A, Lipinski F, Jaubert D, Ingrand P and
Migeot V; REPERES Group, : Breast cancer care compared with
clinical guidelines: An observational study in France. BMC Public
Health. 11:452011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wallwiener M, Brucker SY and Wallwiener D;
Steering Committee, : Multidisciplinary breast centres in Germany:
A review and update of quality assurance through benchmarking and
certification. Arch Gynecol Obstet. 285:1671–1683. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zollman C, Walther A, Seers HE, Jolliffe
RC and Polley MJ: Integrative whole-person oncology care in the UK.
J Natl Cancer Inst Monogr 2017. 2017. View Article : Google Scholar
|
|
8
|
Fidjeland HL, Brekke M and Vistad I:
General practitioners' attitudes toward follow-up after cancer
treatment: A cross-sectional questionnaire study. Scand J Prim
Health Care. 33:223–232. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lang V, Walter S, Fessler J, Koester MJ,
Ruetters D and Huebner J: The role of the general practitioner in
cancer care: A survey of the patients' perspective. J Cancer Res
Clin Oncol. 143:895–904. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bober SL, Recklitis CJ, Campbell EG, Park
ER, Kutner JS, Najita JS and Diller L: Caring for cancer survivors:
A survey of primary care physicians. Cancer 115 (18 Suppl).
S4409–S4418. 2009. View Article : Google Scholar
|
|
11
|
Charles JA, Ahnfeldt-Mollerup P,
Søndergaard J and Kristensen T: Empathy variation in general
practice: A survey among general practitioners in Denmark. Int J
Environ Res Public Health. 15(pii): E4332018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rathmann W, Bongaerts B, Carius H-J,
Kruppert S and Kostev K: Basic characteristics and
representativeness of the German disease analyzer database. Int J
Clin Pharmacol Ther. 56:459–466. 2018. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kostev K, Jacob L and Kalder M: Risk of
depression, anxiety, and adjustment disorders in women with a
suspected but unconfirmed diagnosis of breast or genital organ
cancer in Germany. Cancer Causes Control. 28:1021–1026. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jacob L, Scholten PC, Kostev K and Kalder
M: Association between sleep disorders and the presence of breast
cancer metastases in gynecological practices in Germany: A
case-control study of 11,412 women. Breast Cancer Res Treat.
171:443–448. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Leung KM, Elashoff RM and Afifi AA:
Censoring issues in survival analysis. Annu Rev Public Health.
18:83–104. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Glanz K and Lerman C: Psychosocial impact
of breast cancer: A critical review. Ann Behav Med. 14:204–212.
1992.
|
|
17
|
Holleczek B, Jansen L and Brenner H:
Breast cancer survival in Germany: A population-based high
resolution study from Saarland. PLoS One. 8:e706802013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Liede A, Jerzak KJ, Hernandez RK, Wade SW,
Sun P and Narod SA: The incidence of bone metastasis after
early-stage breast cancer in Canada. Breast Cancer Res Treat.
156:587–595. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chen J, Long JB, Hurria A, Owosu C,
Steingart RM and Gross CP: Incidence of heart failure or
cardiomyopathy after adjuvant trastuzumab therapy for breast
cancer. J Am Coll Cardiol. 60:2504–2512. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ludvigsson JF, Otterblad-Olausson P,
Pettersson BU and Ekbom A: The Swedish personal identity number:
Possibilities and pitfalls in healthcare and medical research. Eur
J Epidemiol. 24:659–667. 2009. View Article : Google Scholar : PubMed/NCBI
|