Introduction
Colorectal cancer is the third most common
malignancy and a leading cause of cancer-related deaths worldwide
(1). Along with an aging of the
population, the number of elderly patients who receive surgical
treatment for colorectal cancer has gradually increased. The median
age at diagnosis of colorectal cancer is 69–72 years, with 60–70%
of all cases diagnosed in patients over the age of 65 (2). Approximately, 17.5% of colorectal
cancer patients are diagnosed when they are over 80 years old
(1). Unfortunately, most elderly
patients have comorbidities, such as cardiovascular or pulmonary
diseases, and reduced functional reserve, which may increase their
risks of postoperative morbidity and mortality and subsequently
influence the treatment choice (e.g., avoiding curative
resection).
In recent years, preoperative chemoradiotherapy
(CRT) with fluorouracil-based chemotherapy and at least 45.0 Gy of
pelvic radiation, followed by surgical treatment, has been widely
used for treating patients with resectable locally advanced rectal
adenocarcinoma, because this approach facilitates tumor
downstaging, increases sphincter preservation, and decreases
locoregional recurrence (3–5). Most studies have used cutoff ages of 60
or 70 years old; therefore, few studies with elderly patients over
80 years, which occupy one sixth of colorectal cancer patients,
have been published. The safety and effectiveness of preoperative
CRT in octogenarians with locally advanced rectal cancer has not
been determined.
The purpose of this study was to evaluate if
preoperative CRT is efficacious and safe for the treatment of
locally advanced rectal cancer in patients older than 80 years.
Materials and methods
Patients and methods
From 2007 to 2017, a total of 293 patients with
histologically confirmed non-metastatic, primary adenocarcinoma of
the lower rectum below the peritoneal reflection invading further
than the muscularis propria (cT3-T4, any N), who received
preoperative CRT, were studied retrospectively at the University of
Tokyo Hospital. All patients, except those with obstruction,
received a total colonoscopy with a biopsy. All patients were
preoperatively evaluated with thoracic and abdominal computed
tomography, pelvic magnetic resonance imaging (MRI) and positron
emission tomography, if needed. Patients who received prior
chemotherapy for rectal cancer or any prior pelvic irradiation,
patients with inflammatory bowel disease, patients with a history
of malignant disease within five years of diagnosis with rectal
cancer and patients who received palliative CRT were excluded from
this study. The study was conducted in accordance with the ethical
guidelines of the Declaration of Helsinki and approved by the
Ethics Committee of the University of Tokyo [no.3252-(7)].
Preoperative CRT
Radiotherapy (RT) was administered five times per
week with a daily fraction of 1.8 Gy. A total dose of 50.4 Gy was
delivered with photons using a 10 MV X-ray accelerator in 28
fractions over the course of 5.6 weeks, using a 3- or 4-field
technique. Preoperative chemotherapy was started simultaneously
with RT. Patients received 5-fluorouracil-based chemotherapy.
Surgery, including total mesorectal excision or tumor-specific
mesorectal excision techniques, was performed 6 to 8 weeks after
the completion of CRT. Lateral pelvic lymph node dissection was
selectively performed in cases suspected of lateral pelvic lymph
node metastasis in the preoperative MRI before CRT regardless of
its response to CRT. In this study, lymph nodes with diameter of 8
mm or larger in MRI were considered as suspect of metastasis. No
short-course RT was performed in the study period.
Study assessments
We investigated comorbidities, short-term outcomes
(i.e., adverse events during CRT, curative resection rate,
pathological complete response (pCR), morbidity, and mortality),
and long-term outcomes (i.e., recurrence rate and site) in elderly
(≥80 years old) and younger patients (<80 years old) and
compared the two groups. Robotic surgery was considered as a
laparoscopic technique and included in laparoscopic surgery.
Curative resection was defined as the macroscopically complete
removal of the tumor and lymph nodes with a microscopically
tumor-free resection margin and no peritoneal spread or distant
metastasis. In laparoscopic surgery, the resected specimen was
retrieved from a small incision at the umbilicus port site, which
was made according to the tumor size, or from the perineal
incision. Conversion of laparoscopic surgery to open surgery was
defined as an abdominal incision different from that planned at the
start of the operation. The results of examination were classified
according to the TNM classification of The International Union
Against Cancer (UICC) (6). Adverse
events were evaluated using the National Cancer Institute's Common
Terminology Criteria for Adverse Events, version 4.0 (7). The tumor regression grade was
determined according to the general rules for clinical and
pathological studies on cancer of the colon, rectum, and anus of
the Japanese Society for Cancer of the Colon and Rectum (8). pCR (grade 3) was defined as the absence
of viable cancer cells in the primary tumor and lymph nodes. Other
grades were defined as: i) grade 1a, less than one third of the
cancer had degraded, necrotized, or disappeared; ii) grade 1b, from
one third to two thirds of the cancer had degraded; and iii) grade
2, more than two thirds of the cancer had degraded. Patients were
discharged when they had sufficient oral intake, no complications
or well-controlled complications, and no excessive anxiety about
leaving the hospital. Short-term morbidity and mortality was
defined as 30-day or in-hospital morbidity and mortality according
to the Clavien-Dindo classification. As follow-up, a blood test was
performed every three months after the surgery, and computed
tomography of the pelvis combined with imaging of the liver and the
chest was performed every six months after the surgery. Recurrence
was defined as the presence of locoregional recurrence, the
presence of distant metastases, or death from colorectal
cancer.
Statistical analysis
For categorical variables, data were presented as
frequencies and percentage, and Fisher's exact probability test was
applied to evaluate the significance of differences in proportions.
Continuous variables such as ‘Days hospitalized after surgery’
shown as median were estimated using the Mann-Whitney U test.
Differences in survival between groups were assessed using the
log-rank test. Associations were considered significant when
P<0.05.
Results
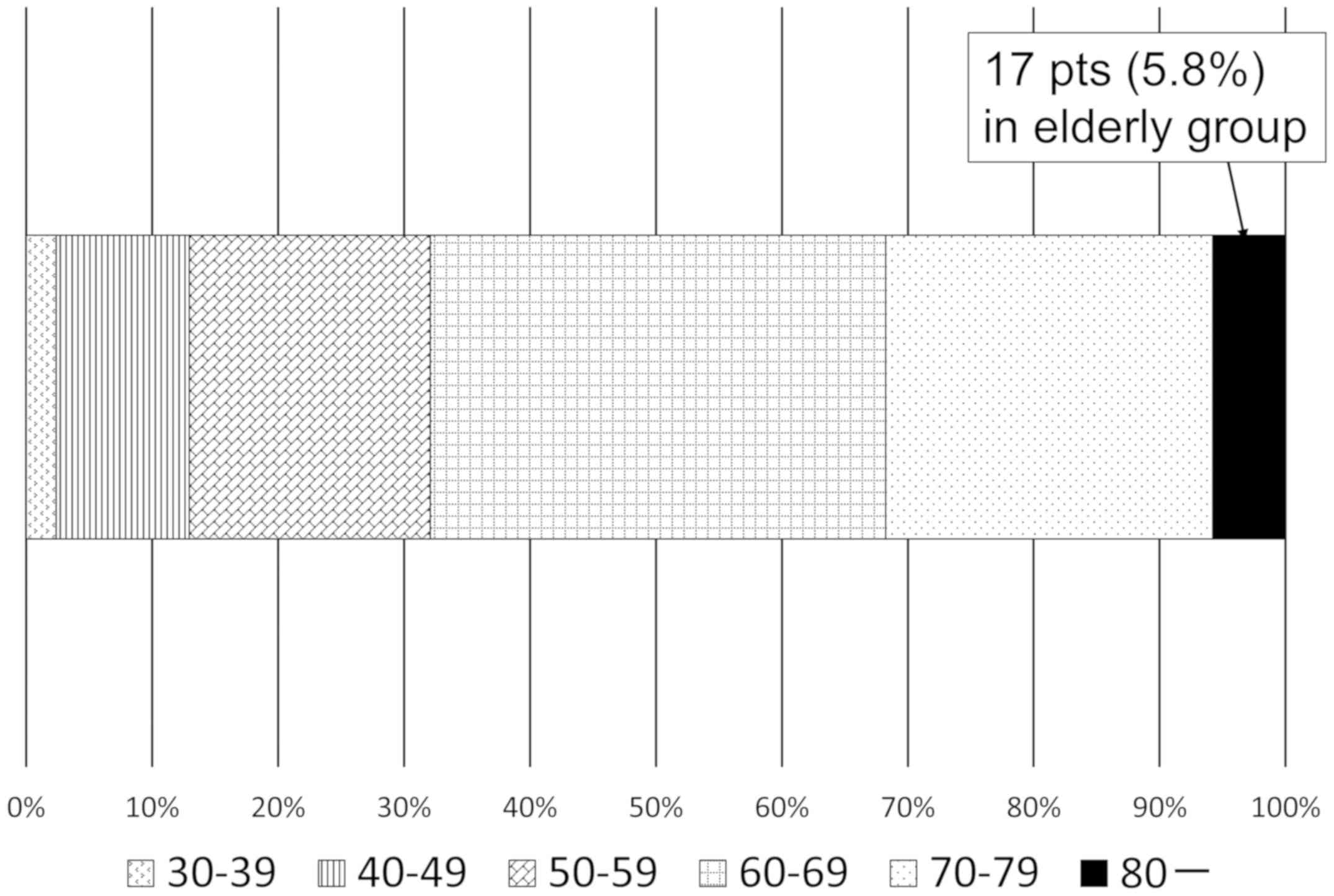
From 2007 to 2017, a total of 293 patients with
locally advanced rectal cancer received preoperative CRT. The
distribution of age groups is shown in Fig. 1. The percentage of patients was
highest in the 60–69-year-old age group (5.8%). In the group
comprised of octogenarians (elderly group) were 17 patients, and
the younger group had 276 patients. The oldest patient was 88 years
old. In elderly group, four patients did not receive preoperative
CRT during the study period.
Patient characteristics and chemotherapy regimens
are shown in Table I. The percentage
of males in elderly and younger groups was 29 and 67%, respectively
(P=0.003). There was no statistical difference between the two
groups regarding comorbidities. Nearly 60% of the patients in the
elderly group presented with comorbidities; pulmonary comorbidity
was the most common one in that group (23.5%). We found a
statistically significant difference between elderly and younger
groups in preoperative therapy. Elderly patients were more likely
to receive RT due to their age (P=0.0008). In the younger group,
only five patients (1.8%) received RT because of patient selection,
renal dysfunction, or liver dysfunction in two, two, and one
patient, respectively. The following regimens were employed as
chemotherapy: Oral tegafur-uracil and leucovorin (n=245), oral S-1
(n=10), oral tegafur-uracil and leucovorin with intravenous
irinotecan (n=24) and oral S-1 with intravenous oxaliplatin (n=5)
(9). There was no statistical
difference between the two groups regarding the distance of the
tumor from the anal verge and clinical stage.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Variable | Elderly group
(n=17) | Younger group
(n=276) | P-value |
|---|
| Sex |
|
| 0.003 |
| Male | 5 | 185 |
|
|
Female | 12 | 91 |
|
| Treatment before
CRT |
|
|
|
|
Colostomy/Ileostomy | 0 | 8 | 1.0 |
| Comorbidities |
|
|
|
| Overall
(%) | 10 (58.8%) | 127 (46.0%) | 0.33 |
|
Cardiovascular | 1 (5.9) | 25 (9.1) | 1.0 |
|
Hypertension | 3 (17.6) | 71 (25.7) | 0.57 |
|
Pulmonary | 4 (23.5) | 43 (15.6) | 0.49 |
|
Liver | 2 (11.8) | 10 (3.6) | 0.15 |
|
Renal | 1 (5.9) | 9 (3.3) | 0.44 |
|
Cerebrovascular | 3 (17.6) | 16 (5.8) | 0.09 |
| Diabetes
mellitus | 1 (5.9) | 36 (13.0) | 0.71 |
| Preoperative
therapy |
|
| 0.0008 |
| CRT | 13 | 271 |
|
| RT | 4 | 5 |
|
|
Tegafur-uracil/leucovorin | 13 | 232 |
|
| S-1 |
| 10 |
|
| CPT-11 +
tegafur-uracil/leucovorin |
| 24 |
|
| Oxaliplatin +
S-1 |
| 5 |
|
| The distance of the
tumor from the anal verge |
|
| 0.13 |
| ≤4
cm | 12 | 145 |
|
| 4.1–8
cm | 5 | 119 |
|
| 8.1–10
cm |
| 12 |
|
| Clinical stage |
|
| 0.27 |
| 2a | 10 | 138 |
|
| 2b |
| 2 |
|
| 2c | 2 | 1 |
|
| 3b | 3 | 92 |
|
| 3c | 2 | 9 |
|
| 4 |
| 34 |
|
Adverse events during CRT are shown in Table II. There was no statistical
difference between the two groups related to the rate of
completeness of CRT (P=0.26). Adverse events occurred in 88.2% of
the elderly group including grade 1–3, but there was no significant
difference between the two groups (P=0.17). Diarrhea was the most
common side effect in the elderly group (seven cases). Pneumonia
occurred in three patients in this study. Grade 3 adverse events
occurred in three patients of the elderly group (diarrhea in two,
pneumonia in one) and in five patients of the younger group
(diarrhea in three, radiation dermatitis in one, proctitis in one).
No death during preoperative CRT occurred in either group.
 | Table II.Adverse events during CRT. |
Table II.
Adverse events during CRT.
| Variable | Elderly group
(n=17) | Younger group
(n=276) | P-value |
|---|
| Result of CRT |
|
| 0.26 |
|
Complete | 15 (88.2%) | 261 (94.6%) |
|
| Dose
reduction | 1 | 13 |
|
|
Cessation | 1 | 2 |
|
| Adverse event |
|
Overall | 15 (88.2%) | 197 (71.4%) | 0.17 |
|
Diarrhea | 7 | 67 | 0.15 |
| Anal
pain | 5 | 114 | 0.45 |
|
Radiation dermatitis | 1 | 27 | 1.0 |
|
Cystitis | 1 | 6 | 0.34 |
|
Pneumonia | 1 | 2 | 0.16 |
|
Proctitis |
| 5 | 1.0 |
|
Gonitis |
| 1 | 1.0 |
|
Backache |
| 1 | 1.0 |
|
Neutropenia |
| 5 | 1.0 |
|
Melena |
| 2 | 1.0 |
|
Anorexia | 1 | 1 | 0.11 |
|
Nausea |
| 3 | 1.0 |
|
Fatigue | 1 |
| 0.06 |
|
Appetite loss | 1 | 1 | 0.11 |
|
Death | 0 | 0 | 1.0 |
The surgical procedures performed are shown in
Table III. Curative resection was
performed in fourteen patients (82.4%) in the elderly group and no
treatment was performed in the remaining three patients because of
poor general condition. On the other hand, curative resection was
performed in 91.3% of the patients in the younger group and
non-curative treatment or no treatment was performed in twenty-four
patients, because of refusal of resection by seven patients, and
poor general condition in four patients, and various reasons in the
remaining 13 patients. The curative resection rate was similar
between the two groups (P=0.20). The general condition after CRT
was worse in the elderly group than in the younger group; the rate
of poor general condition in elderly group was significantly higher
than that in younger patients (P=0.005). In total seven patients
from both groups could not receive curative resection due to poor
general condition during or after CRT, four patients (three in the
younger and one in the elderly group) had decreased lower
respiratory function due to pneumonia in three patients and Chronic
obstructive pulmonary disease (COPD) in one, and one patient each
suffered from severe appetite loss or fatigue. Laparoscopic surgery
was a preferred procedure in the elderly group (P=0.052). No
conversion to open surgery was required in either group. Lateral
lymph node dissection was performed in 39 patients in the younger
group, but in none of the patients in the elderly group (P=0.23).
The rate of diverting stoma construction was similar in both groups
(P=0.39). The closure ratio of diverting stoma was not
statistically different between elderly and younger groups (66.7%
vs. 62.0%, P=0.55).
 | Table III.Surgical procedure. |
Table III.
Surgical procedure.
|
| Elderly group
(n=17) | Younger group
(n=276) | P-value |
|---|
| Curative
resection | 14 (82.4%) | 252 (91.3%) | 0.2 |
| Worse general
condition | 3 | 4 | 0.0049 |
| Approach |
|
| 0.051 |
|
Laparoscopic surgery
(robot) | 12 (3) | 148 (37) |
|
| Open
surgery | 2 | 104 |
|
|
Conversion to open
surgery | 0 (0%) | 0 (0%) |
|
| Types of
operation |
|
| 0.046 |
| Low
anterior resection | 5 | 149 |
|
|
Intersphincter resection | 1 | 42 |
|
|
Hartmann's operation | 2 | 3 |
|
|
Abdominoperineal
resection | 6 | 56 |
|
| Total
pelvic exenteration | 2 |
|
|
| Lateral
lymph node dissection | 0 | 39 | 0.23 |
| Diverting
stoma |
|
Construction | 3 (21.4%) | 92 (36.5%) | 0.39 |
|
Closure | 2 (66.7%) | 57 (62.0%) | 0.55 |
Postoperative course is shown in Table IV. We observed pCR in one patient
(7.1%) in the elderly group and in 27 patients (10.7%) in the
younger group (P=0.20). There was no statistical difference between
the two groups regarding pathological stage. The morbidity rate,
higher than Clavien-Dindo classification grade 2, was similar in
elderly and younger groups (35.7% vs. 27.0%, respectively, P=0.54);
the mortality rate after surgery was zero in both groups. Patients
in the elderly group were associated with a longer hospital stay
compared to the younger group (23.5 days vs. 19 days, respectively,
P=0.07), because patients were discharged when they had no
excessive anxiety about leaving the hospital. Adjuvant chemotherapy
was given to three patients in the elderly group. Two patients
received tegafur-uracil/leucovorin and one received capecitabine.
Although a smaller percentage of elderly patients received adjuvant
chemotherapy, there was no significant difference between elderly
and younger groups (21.4% vs. 37.3%, P=0.12). No significant
difference was found in the recurrence rate between the two groups
(P=1.00). Three patients in the elderly group, and 60 patients in
the younger group developed recurrences including lymph node
metastases outside the pelvis. Among the 3 cases of the elderly
group, one recurred with lung metastasis and lymph node metastasis
outside the pelvis, one had lung metastasis, and one had lymph node
metastasis outside the pelvis. Among the 60 cases of the younger
group, 10 recurred with lymph node metastases, and 7 of them were
outside the pelvis.
 | Table IV.Postoperative course. |
Table IV.
Postoperative course.
|
| Elderly group
(n=14) | Younger group
(n=252) | P-value |
|---|
| Pathological
complete response (pCR) | 1 (7.1%) | 27 (10.7%) | 0.2 |
| Pathological
stage |
|
| 0.8 |
| 0 | 2 | 27 |
|
| 1 | 3 | 61 |
|
| 2a | 4 | 71 |
|
| 2b |
| 2 |
|
| 2c | 1 | 3 |
|
| 3a |
| 13 |
|
| 3b | 2 | 38 |
|
| 3c | 1 | 5 |
|
| 4 | 1 | 32 |
|
| Morbidity
overall | 5 (35.7%) | 68 (27.0%) | 0.54 |
| Wound
infection | 2 | 11 | 0.14 |
|
Intra-abdominal abscess | 1 | 10 | 0.45 |
|
Anastomotic leakage |
| 2 | 1.0 |
|
Infection via catheter |
| 9 | 1.0 |
| Urinary
tract infection |
| 2 | 1.0 |
|
Pneumonia |
| 1 | 1.0 |
|
Enterocolitis |
| 2 | 1.0 |
|
Delirium |
| 3 | 1.0 |
| Bowel
obstruction | 1 | 17 | 1.0 |
| Stoma
obstruction |
| 3 | 1.0 |
| Wound
bleeding |
| 1 | 1.0 |
| Urinary
retention |
| 7 | 1.0 |
| Ureter
injury |
| 1 | 1.0 |
|
Compartment syndrome |
| 2 | 1.0 |
|
Port-site hernia | 1 |
| 0.053 |
| Mortality | 0 (0%) | 0 (0%) | 1.0 |
| Days hospitalized
after surgery (days) | 23.5 (13–63) | 19 (8–316) | 0.07 |
| Median (range) |
| Adjuvant
chemotherapy |
|
Overall | 3 (21.4%) | 94 (37.3%) | 0.12 |
|
Tegafur-uracil/leucovorin | 2 | 48 |
|
|
Capecitabine | 1 | 5 |
|
|
S-1 |
| 9 |
|
|
XELOX |
| 17 |
|
|
SOX |
| 2 |
|
|
FOLFOX |
| 13 |
|
| Recurrence |
|
Overall | 3 (21.4%) | 60 (23.8%) | 1.0 |
|
Lung | 2 | 30 | 0.68 |
|
Liver |
| 16 | 1.0 |
| Lymph
node | 2 | 10 | 0.13 |
|
Local |
| 8 | 1.0 |
|
Dissemination |
| 4 | 1.0 |
|
Brain |
| 2 | 1.0 |
|
Skin |
| 1 | 1.0 |
Discussion
In a previous German randomized study, 92% of
patients aged ≤76 years received the prescribed RT and 89%
completed preoperative CRT (10). In
our study, 88.2% of elderly patients received the complete dose of
preoperative CRT, which is comparable to that from the previous
study. A recent American retrospective study showed that 5% of
patients aged ≤68 years received incomplete doses of radiation in
neoadjuvant CRT (3). In that study,
Freischlag et al (3) also
revealed that female patients, patients who received preoperative
therapy and surgery at different facilities, and patients without
insurance were less likely to complete preoperative therap. In our
study, all patients had national health insurance and received
preoperative CRT and surgery at the same hospital. Although there
was a larger percentage of female patients in the elderly rectal
cancer group, the complete rate of preoperative CRT was not
significantly different between the two groups.
In our study, octogenarians were more likely to
receive RT due to their age (P=0.0008). Cai et al (11) revealed that grade 3 toxicities
(diarrhea, skin toxicity, and neutropenia) occurred more often in
elderly rectal cancer patients (≥70 years old) treated with CRT
compared to those treated with RT. Guimas et al (12), noted an increase in morbidity with
the addition of oxaliplatin to standard CRT, and Margalit et
al (13), demonstrated that
treatment intensification should be performed with care in elderly
rectal cancer patients (≥70 years old) treated with preoperative
CRT or RT, because the majority of elderly patients required early
termination of treatment, treatment interruptions, or dose
reductions. On the other hand, several studies showed that
neoadjuvant CRT in elderly rectal cancer patients was a
well-tolerated treatment without any significant increase in acute
and late toxicities (14–17). In the present study, there was no
statistical difference between elderly and younger groups related
to the result of neither CRT nor the adverse event during CRT.
Therefore, although the majority of elderly patients could safely
undergo preoperative treatment consisting of RT combined with oral
tegafur-uracil and leucovorin, we need to carefully select the
elderly rectal cancer patients when adding oxaliplatin or
irinotecan to standard CRT.
Pneumonia was one of the risk factors that precluded
safe performance of treatment (preoperative CRT or curative
surgical procedure after CRT) in our study. Inoue et al
(18), reported comparably high
rates of postoperative complications in patients with pulmonary
comorbidities. Furthermore, Baré et al (19), demonstrated that COPD was associated
with higher rates of postoperative complications, antibiotic
treatment, and mortality during hospitalization, and that patients
with underlying COPD had a higher rate of postoperative infectious
complications, such as septic shock, pneumonia, and other
respiratory tract infections, compared to those without COPD. In a
previous study, we reported two elderly patients aged ≥80 years
with colorectal cancer who underwent curative surgical resection
died in the postoperative period due to pneumonia (20). Thus, to reduce pulmonary morbidity
and mortality in elderly rectal cancer patients with comorbidities,
intensive perioperative chest physiotherapy should be recommended.
Further study is needed to implement the ideal prevention strategy
for postoperative respiratory complications in elderly patients
with locally advanced rectal cancer and comorbidities.
Previously, we demonstrated that laparoscopic
surgery in elderly patients (octogenarians) with colorectal cancer
is a safe and less invasive alternative to open surgery, with less
blood loss and a shorter hospital stay (20). Several other studies also reported
the safety and feasibility of laparoscopic surgery in elderly
patients with colorectal cancer (21–23).
However, the safety and effectiveness of laparoscopic surgery is
not clear in both octogenarians and younger patients with rectal
cancer treated with preoperative CRT (24–28).
Further study is needed to confirm the safety and effectiveness of
laparoscopic surgery for the treatment of locally advanced rectal
cancer in elderly patients.
The rates of diverting stoma construction and
closure were similar in elderly and younger groups in this study.
According to large scale studies, 12–40% of defunctioning stomas
are never reversed for many reasons, such as cancer recurrence,
anastomosis site-related complications, poor general conditions,
and unsatisfactory rectal functions (29). Previous studies demonstrated that
neoadjuvant CRT is an independent risk factor for stoma
non-reversal (30,31). We also reported on the closure rate
of diverting stoma and risk factor of stoma non-reversal after low
anterior resection using a nomogram (32); one of the risk factors of stoma
non-reversal was preoperative CRT, but not the patient's age. Kim
et al (29), also did not
identify older age as a risk factor for stoma non-reversal.
Therefore, when planning rectal surgery involving a temporary stoma
for elderly patients with rectal cancer treated by preoperative
CRT, surgeons should consider the possibility that stoma
non-reversal may be caused by preoperative CRT, not by patient's
age.
In conclusion, the present study has some
limitations. First, this study was not a large-scale multicenter
randomized trial, but a retrospective study conducted at a single
institute. Second, selection bias remains a concern. There is the
possibility that some elderly patients with locally advanced rectal
cancer did not receive preoperative CRT nor surgical treatment.
However, beside these limitations, our current data still provide
support to the concept that preoperative CRT can be performed with
tolerable adverse events, completeness of CRT, and acceptable
morbidity and mortality rates in elderly patients with locally
advanced rectal cancer.
Acknowledgements
Not applicable.
Funding
The present study was supported by Grants-in-Aid for
Scientific Research (C: grant no. 16K07143, C: grant no. 16K07161,
C: grant no. 17K10620, C: grant no. 17K10621C: grant no. 17K10623
and C: grant no. 18K07194) from the Japan Society for the Promotion
of Science. This research was also supported by the Project for
Cancer Research and Therapeutic Evolution (P-CREATE, grant no.
18cm0106502h0003) from the Japan Agency for Medical Research and
Development (AMED).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
TN was conceived the design of the manuscript and
the analysis and interpretation of data and drafted the article. KK
supervised the study. KH, SE, KM, KS, TT and HN participated in the
design of this article and revised the paper critically for
important intellectual content. SI participated in the design of
this article, revised it critically for important intellectual
content and gave final approval of the version to be published.
Ethics approval and consent to
participate
The study was conducted in accordance with the
ethical guidelines of the Declaration of Helsinki and approved by
the Ethics Committee of the University of Tokyo [No. 3252-(7)].
Patient consent for publication
Patients were provided the option to opt out.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
CRT
|
chemoradiotherapy
|
|
RT
|
radiotherapy
|
References
|
1
|
Yang L, Ma Q, Yu YY, Wang C, Meng WJ,
Adell G, Albertsson M, Arbman G, Jarlsfelt I, Peng ZH, et al:
Efficacy of surgery and adjuvant therapy in older patients with
colorectal cancer: A STROBE-compliant article. Medicine
(Baltimore). 93:e2662014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jacobs L, van der Vlies E, Ten Bokkel
Huinink D, Bloemendal H, Intven M, Smits AB, Weusten BLAM, Siersema
PD, van Lelyveld N and Los M: Tolerability, safety and outcome of
neoadjuvant chemoradiotherapy with capecitabine in Patients Aged
≥70 Years with locally advanced rectal cancer. Clin Colorectal
Cancer. 17:179–186. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Freischlag K, Sun Z, Adam MA, Kim J, Palta
M, Czito BG, Migaly J and Mantyh CR: Association between incomplete
neoadjuvant radiotherapy and survival for patients with locally
advanced rectal cancer. JAMA Surg. 152:558–564. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
National Comprehensive Cancer Network:
NCCN Guidelines, version 2. Rectal cancer. Fort Washington; PA:
National Comprehensive Cancer Network, . 2016
|
|
5
|
Wong RK, Tandan V, De Silva S and
Figueredo A: Pre-operative radiotherapy and curative surgery for
the management of localized rectal carcinoma. Cochrane Database
Syst Rev. CD0021022007.PubMed/NCBI
|
|
6
|
Brierley JD, Gospodarowicz MK and
Wittekind C: UICC international union against cancer. TMN
classification of malignant tumours. 8th. Wiley-Blackwell;
Chichester, UK: 2017
|
|
7
|
National cancer institute, . Common
terminology criteria for adverse events (CTCEA) version 4.0.
http://www.eortic.be/services/doc/ctc/CTCAE
4.032010-06-14QuickReference5x7.pdfUpdated 20102009.
|
|
8
|
Japanese Society for Cancer of the Colon
and Rectum, . General rules for clinical and pathological studies
on cancer of the colon, rectum and anus. 7th. Tokyo: Kanehara;
2009
|
|
9
|
Matsusaka S, Ishihara S, Kondo K, Horie H,
Uehara K, Oguchi M, Murofushi K, Ueno M, Mizunuma N, Shimbo T, et
al: A multicenter phase II study of preoperative chemoradiotherapy
with S-1 plus oxaliplatin for locally advanced rectal cancer
(SHOGUN trial). Radiother Oncol. 116:209–13. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sauer R, Becker H, Hohenberger W, Rödel C,
Wittekind C, Fietkau R, Martus P, Tschmelitsch J, Hager E, Hess CF,
et al: Preoperative versus postoperative chemoradiotherapy for
rectal cancer. N Engl J Med. 351:1731–1740. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cai X, Wu H, Peng J, Zhu J, Cai S, Cai G
and Zhang Z: Tolerability and outcomes of radiotherapy or
chemoradiotherapy for rectal cancer in elderly patients aged 70
years and older. Radiat Oncol. 8:862013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Guimas V, Boustani J, Schipman B, Lescut
N, Puyraveau M, Bosset JF and Servagi-Vernat S: Preoperative
chemoradiotherapy for rectal cancer in patients aged 75 years and
older: Acute toxicity, compliance with treatment, and early
results. Drugs Aging. 33:419–25. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Margalit DN, Mamon HJ, Ancukiewicz M,
Kobayashi W, Ryan DP, Blaszkowsky LS, Clark J, Willett CG and Hong
TS: Tolerability of combined modality therapy for rectal cancer in
elderly patients aged 75 years and older. Int J Radiat Oncol Biol
Phys. 81:e735–e741. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tougeron D, Roullet B, Paillot B, Hamidou
H, Tourani JM, Bensadoun RJ, Michel P and Silvain C: Safety and
outcome of chemoradiotherapy in elderly patients with rectal
cancer: Results from two French tertiary centres. Dig Liver Dis.
44:350–354. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ausili Cèfaro G, Genovesi D, Vinciguerra
A, Augurio A, Di Tmmaso M, Marchese R, Borzillo V, Tsciotti L,
Taraborrelli M, Innocenti P, et al: Effects of preoperative
radiochemotherapy with capecitabine for resectable locally advanced
rectal cancer in elderly patients. Tumori. 98:622–629. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
De Felice F, Musio D, Izzo L, Pugliese F,
Izzo P, Bolognese A and Tombolini V: Preoperative chemoradiotherapy
in elderly patients with locally advanced rectal cancer. Biomed Res
Int. 2013:6107862013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
De Felice F, Llange K, Rubini F,
Bulzonetti N, Caiazzo R, Musio D and Tombolini V: Intensified
neoadjuvant chemoradiotherapy for locally advanced rectal cancer in
elderly patients: Toxicity, disease control, and survival outcomes.
Clin Colorectal Cancer. 17:e77–e81. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Inoue Y, Kawamoto A, Okugawa Y, Hiro J,
Saigusa S, Toiyam Y, Araki T, Tanaka K, Mohri Y and Kusunoki M:
Efficacy and safety of laparoscopic surgery in elderly patients
with colorectal cancer. Mol Clin Oncol. 3:897–901. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Baré M, Montón C, Mora L, Redondo M, Pont
M, Escobar A, Sarasqueta C, Fernández de Larrea N, Briones E and
Quntana JM: COPD is a clear risk factor for increased use of
resources and adverse outcomes in patients undergoing intervention
for colorectal cancer: A nationwide study in Spain. Int J Chron
Obstruct Pulmon Dis. 12:1233–1241. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nishikawa T, Ishihara S, Hata K, Murono K,
Yasuda K, Otani K, Tanaka T, Kiyomatsu T, Kawai K, Nozawa H, et al:
Short-term outcomes of open vs. laparoscopic surgery in elderly
patients with colorectal cancer. Surg Endsc. 30:5550–5557. 2016.
View Article : Google Scholar
|
|
21
|
Hinoi T, Kawaguchi Y, Hattori M, Okajima
M, Ohdan H, Yamamoto S, Hasegawa H, Horie H, Murata K, Yamaguchi S,
et al: Laparoscopic versus open surgery for colorectal cancer in
elderly patients: A multicenter matched case-control study. Ann
Surg Oncol. 22:2040–2050. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Robinson CN, Balentine CJ, Marshall CL,
Wilks JA, Anaya D, Artinyan A, Berger DH and Albo D: Minimally
invasive surgery improves short-term outcomes in elderly colorectal
cancer patients. J Surg Res. 166:182–188. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shigeta K, Baba H, Yamafuji K, Asami A,
Takeshima K, Nagasaki K, Okamoto N, Murata T, Arai S, Kubochi K and
Kitagawa Y: Effects of laparoscopic surgery on the patterns of
death in elderly colorectal cancer patients: Competing risk
analysis compared with open surgery. Surg Today. 46:422–429. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Gillou PJ, Quirke P, Thorpe H, Walker J,
Jane DG, Smith AM, Heath RM and Brown JM; MRC CLASICC trial group,
: Short-term endpoints of conventional versus laparoscopic-assisted
surgery in patients with colorectal cancer (MRC CLASICC trial):
Multicentre, randomized controlled traial. Lancet. 365:1718–1726.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lujan J, Valero G, Hernandez Q, Sanchez A,
Frutos MD and Parrilla P: Randomized clinical trial comparing
loparoscopic and open surgery in patients with rectal cancer. Br J
Surg. 96:982–989. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
26
|
van der Pas MH, Haglind E, Cuesta MA,
Fürst A, Lacy AM, Hop WC and Bonjer HJ; COlorectal cancer
Laparoscopic or Open Resection II (COLOR II) Study Group, :
Laparoscopic versus open surgery for rectal cancer (COLOR II):
Short-term outcomes of a randomised, phase 3 trial. Lancet Oncol.
14:210–218. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Fleshman J, Branda M, Sargent DJ, Boller
AM, George V, Abbas M, Peters WR Jr, Maun D, Chang G, Herline A, et
al: Effect of laparoscopic-assisted resection vs. open resection of
Stage II or III rectal cancer on pathologic outcomes. The ACOSOG
Z6051 randomized clinical trial. JAMA. 314:1346–1355. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Stevenson AR, Solomon MJ, Lumley JW,
Hewett P, Clouston AD, Gebski VJ, Davies L, Wilsn K, Hague W and
Simes J; ALaCaRT Investigators, : Effect of laparoscopic-assisted
resection vs. open resection on pathological outcomes in rectal
cancer. The ALaCaRT randomized clinical trial. JAMA. 314:1356–1363.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kim MJ, Kim YS, Park SC, Sohn DK, Kim DY,
Chang HJ and Oh JH: Risk factors for permanent stoma after rectal
cancer surgery with temporary ileostomy. Surgery. 159:721–727.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hassan I, Larson DW, Wolff BG, Cima RR,
Chua HK, Hahnloser D, O'Byrne MM, Larson DR and Pemberton JH:
Impact of pelvic radiotherapy on morbidity and durability of
sphincter preservation after coloanal anastomosis for rectal
cancers. Dis Colon Rectum. 51:32–37. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lindgren R, Hallböök O, Rutegård J,
Sjödahl R and Matthiessen P: What is the risk for a permanent stoma
after low anterior resection of the rectum for cancer? A six-year
follow-up of a multicenter trial. Dis Colon Rectum. 54:41–47. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Abe S, Kawai K, Nozawa H, Hata K,
Kiyomatsu T, Tanaka T, Nishikawa T, Otani K, Sasaki K, Kaneko M, et
al: Use of a nomogram to predict the closure rate of diverting
ileostomy after low anterior resection: A retrospective cohort
study. Int J Surg. 47:83–88. 2017. View Article : Google Scholar : PubMed/NCBI
|