Spandidos Publications style
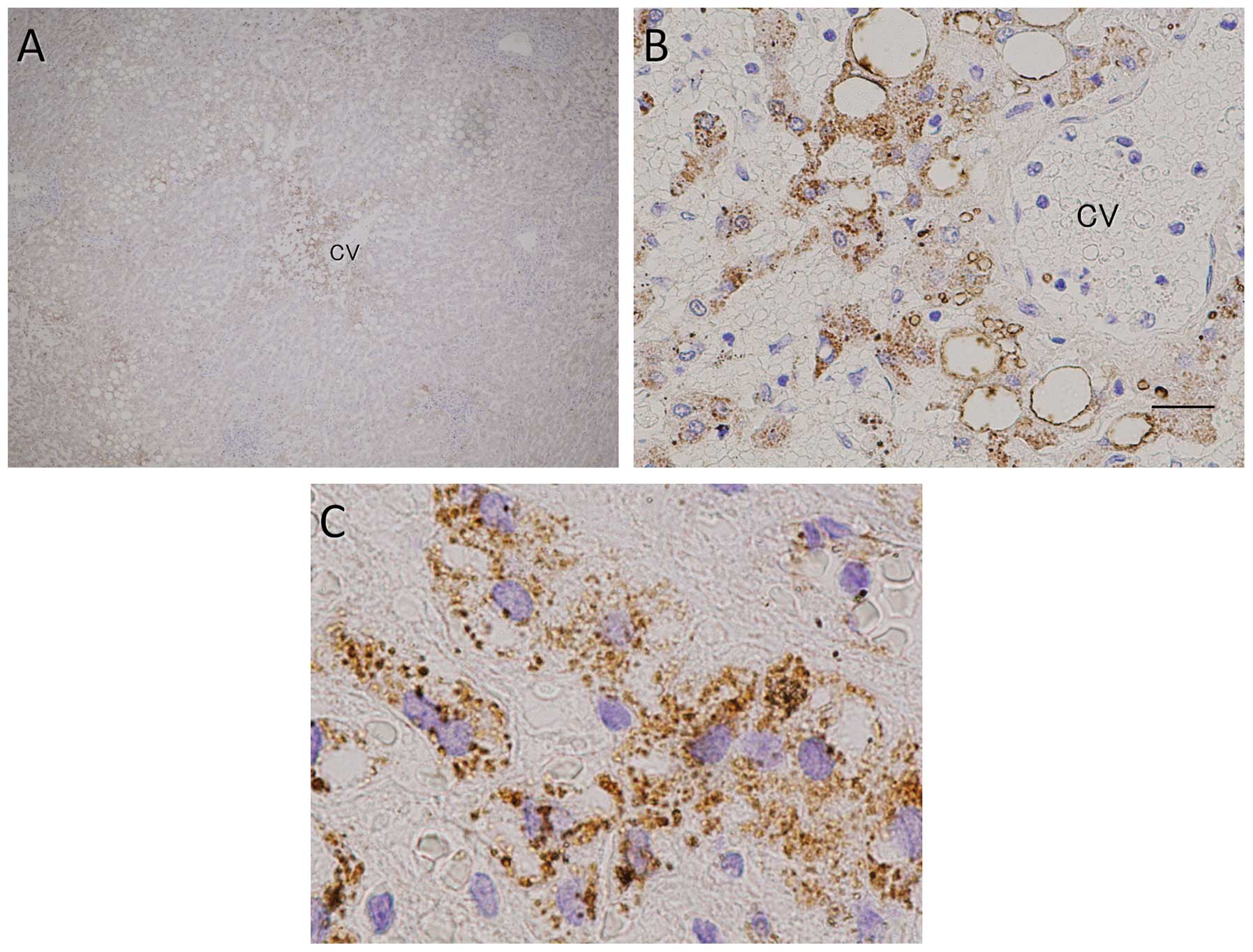
Tajima H, Ohta T, Miyashita T, Nakanuma S, Matoba M, Miyata T, Sakai S, Okamoto K, Makino I, Kinoshita J, Kinoshita J, et al: Oxaliplatin-based chemotherapy induces extravasated platelet aggregation in the liver. Mol Clin Oncol 3: 555-558, 2015.
APA
Tajima, H., Ohta, T., Miyashita, T., Nakanuma, S., Matoba, M., Miyata, T. ... Ikeda, H. (2015). Oxaliplatin-based chemotherapy induces extravasated platelet aggregation in the liver. Molecular and Clinical Oncology, 3, 555-558. https://doi.org/10.3892/mco.2015.512
MLA
Tajima, H., Ohta, T., Miyashita, T., Nakanuma, S., Matoba, M., Miyata, T., Sakai, S., Okamoto, K., Makino, I., Kinoshita, J., Hayashi, H., Nakamura, K., Oyama, K., Inokuchi, M., Nakagawara, H., Takamura, H., Kitagawa, H., Fushida, S., Ikeda, H."Oxaliplatin-based chemotherapy induces extravasated platelet aggregation in the liver". Molecular and Clinical Oncology 3.3 (2015): 555-558.
Chicago
Tajima, H., Ohta, T., Miyashita, T., Nakanuma, S., Matoba, M., Miyata, T., Sakai, S., Okamoto, K., Makino, I., Kinoshita, J., Hayashi, H., Nakamura, K., Oyama, K., Inokuchi, M., Nakagawara, H., Takamura, H., Kitagawa, H., Fushida, S., Ikeda, H."Oxaliplatin-based chemotherapy induces extravasated platelet aggregation in the liver". Molecular and Clinical Oncology 3, no. 3 (2015): 555-558. https://doi.org/10.3892/mco.2015.512