Introduction
Brenner tumor, an uncommon subtype of surface
epithelial-stromal tumors, which are a class of ovarian neoplasms,
was first described by Brenner in 1907 (1). It is an uncommon neoplasm, accounting
for ~1.4–2.5% of all ovarian tumors (2). Brenner tumors are classified into three
categories according to the World Health Organization, namely
benign, borderline and malignant (3). Extraovarian Brenner tumors are
extremely rare, and are mainly found in the broad ligament, uterus,
vagina, testis and epididymis (4–7). In the
present study, we report a case of Brenner tumor of the right
testis and discuss the clinical and pathological characteristics of
this disease. The study was approved by the Ethics Committee of
Peking University Shenzhen Hospital (Shenzhen, China) and written
informed consent was obtained from the patient for the publication
of the case details.
Case report
The patient, a A 55-year-old man presented with a
swelling of the right scrotum for ~20 days. There were no obvious
precipitating or alleviating factors. The patient experienced a
painless sensation of heaviness of the right testis. The only
positive physical finding was a mildly tender mass in the right
scrotum. The results of the laboratory and imaging examinations
(hemogram, urinalysis, β-human chorionic gonadotropin,
a-fetoprotein, liver and kidney function tests and chest X-ray)
were normal. However, the results of a superficial color Doppler
ultrasound examination suggested that the right scrotum had
multiple cystic lesions, and an epididymal was considered as the
possible clinical diagnosis.
Following the doctors' recommendation, the patient
consented to right epididymal cystectomy in Novermber, 2013. During
the operation, the cyst was found to be located between the testis
and the head of the epididymis and was sized ~50×30 mm. The cyst
exhibited inflammatory adhesions to the surrounding organs,
although invasion was not observed. On gross pathological
examination, the resected specimen was a cyst with a thin wall (1
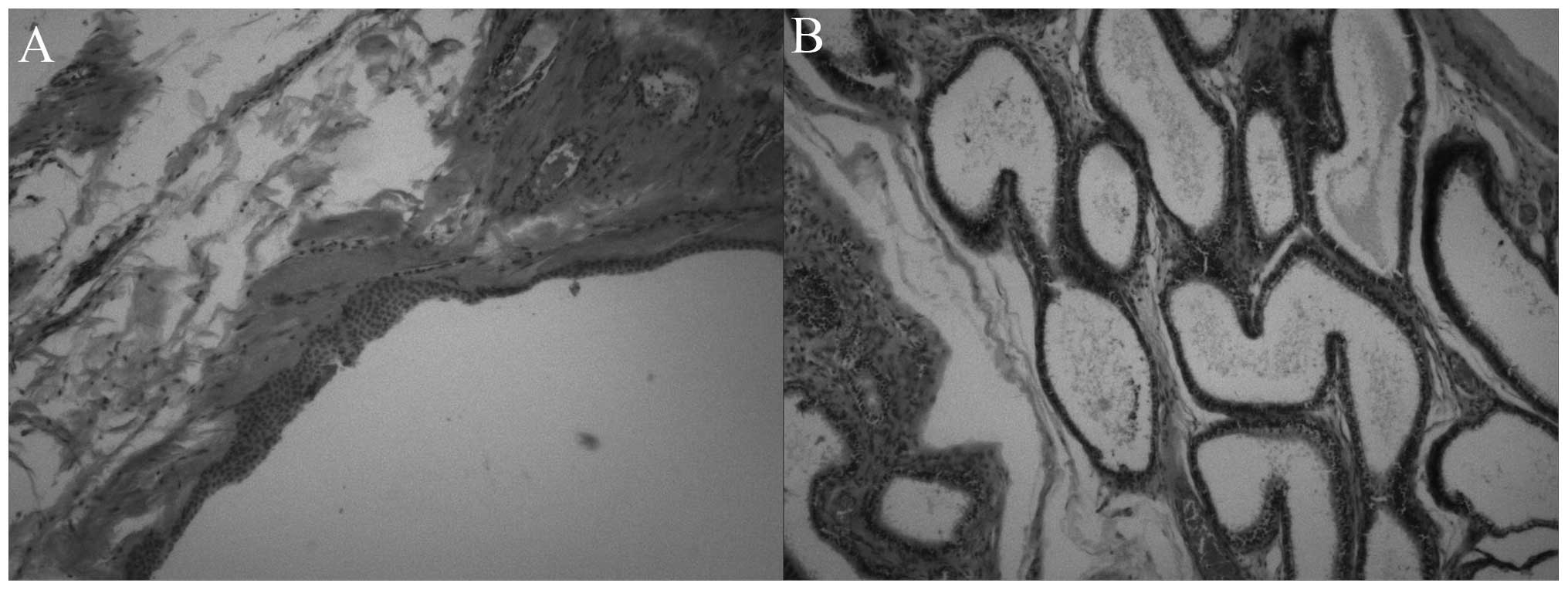
mm), sized 6.5×4×3.5 cm, containing a clear liquid. On microscopic
examination, the fibrous cystic wall was coated with a monolayer or
stratified squamous epithelium. Epithelium-like nests and a small
quantity of epididymal canal tissue were also identified (Fig. 1). The pathological diagnosis was
Brenner tumor of the right testis. Postoperatively, the patient
recovered well. After 29 months of follow-up, the patient has no
evidence of recurrence on laboratory and imaging examinations.
Discussion
Brenner tumor is a rare ovarian tumor, which was
first identified by McNaughton-Jones in 1989, and was then first
described in detail by Brenner in 1907 (1). Brenner tumors are similar to Walthard
nests and tubal/mesothelial transitional metaplasia, which are
composed of urothelial/transitional-type epithelium. It remains a
matter of debate whether ovarian-type epithelial tumors of the
testis originate from the remnants of Müllerian ducts in the
paratesticular connective tissue, epididymis and spermatic cord, or
from Müllerian metaplasia of the mesothelium of the tunica
vaginalis testis. Goldman considered Brenner tumors in the testis
to originate from Müllerian vestiges, as the testis and epididymis
originated from these structures (8), whereas Arhelger and Bocian believed
that Brenner tumors in the wall of the uterus were formed by
Walthard nests (9). With clearer
understanding of Brenner tumors, scholars have realized that the
urinary epithelial cells and ovarian epithelial cells originate
from coelomic epithelial cells during embryonic development. Thus,
it is possible that the urinary epithelium develops from ovarian
epithelium through metaplasia (10).
It is difficult to diagnose Brenner tumors by
imaging examinations, due to the lack of specific morphological
characteristics (11,12). A number of pathologists suggest that
Brenner tumors are similar to Walthard nests in morphology,
suggesting an association between the two. Thus, Roma and
MasandAnders analyzed immunohistochemical markers in Brenner tumors
and Walthard nests, such as paired box (PAX) 8, PAX2, spalt-like
transcription factor 4 and GATA-binding protein 3. The results
suggested that Brenner tumors may be immunohistochemically related
to Walthard nests (13).
ly rare. To the best of our knowledge, only 5 cases
of Brenner tumor of the testis have been described to date
(7,8,14–16) with
our patient being the sixth reported case. The previous cases are
summarized in Table I (full details
on the fifth report were not available). Upon reviewing the
diagnosis and treatment of the 6 cases, the following shared
characteristics were identified: i) The age at onset was 37–67
years, with 66.7% of the patients aged >50 years; ii) a cystic
mass was the most common clinical manifestation, but the
characteristics and size of the mass varied; iii) diagnosis is
based on pathological examination. As this type of tumor is not
associated with typical clinical symptoms, without specific
laboratory results and imaging examinations, it is often
misdiagnosed as hydrocele or epididymal cancer; iv) due to the
sparsity of reported cases, the survival rate is uncertain;
however, based on the available studies on Brenner tumor of the
ovary, survival depends on the stage of the tumor. In general,
following surgery, the prognosis of benign Brenner tumor is good,
while the prognosis of malignant Brenner tumor is poor. The 5-year
survival of stage III/IV disease is ~0%, with only 1 known case
surviving for >2 years following intensive systemic chemotherapy
(1).
 | Table I.Brenner tumor of the testis. |
Table I.
Brenner tumor of the testis.
| Authors, year | Patient age
(years) | Presentation | Location | Size (cm) | Histology | (Refs.) |
|---|
| Caccamo et al,
1991 | 62 | Unknown | Testis and
epididymis | Unknown | Brenner tumor | (7) |
| Ronald and Goldman,
1970 | 41 | Vague intermittent
aching sensation and tender mass | Left testis | 2.7×2.2×2.0 | Brenner tumor | (8) |
| Nogales et al,
1979 | 37 | Cystic mass | Testis | 3 | Mixed Brenner and
adenomatoid tumor | (14) |
| Ross et al,
1968 | 61 | Diabetes with
cardiovascular complications | Paratesticular
greatest diameter | 6 mm in | Brenner tumor | (15) |
| Vechinski et
al, 1965 | 67 | 40-year history of
inguinal hernia and swelling of the scrotum in 4 weeks | Testis | 7.3 | Brenner tumor | (16) |
In conclusion, Brenner tumor is rare and difficult
to diagnose, particularly when occurring in unusual locations. This
report presents a case of Brenner tumor of the testis, which is the
sixth known case of testicular Brenner tumor. This report may be
helpful in further elucidating this disease and reducing the rate
of clinical and pathological misdiagnosis.
Acknowledgements
The present study was supported by grants from the
National Natural Science Foundation of China (no. 81101922), the
Science and Technology Development Fund Project of Shenzhen (nos.
JCY20130402114702124 and JCY20150403091443329) and funds from the
Guangdong Key Medical Subject.
References
|
1
|
Han JH, Kim DY, Lee SW, Park JY, Kim JH,
Kim YM, Kim YT and Nam JH: Intensive systemic chemotherapy is
effective against recurrent malignant Brenner tumor of the ovary:
An analysis of 10 cases within a single center. Taiwan J Obstet
Gynecol. 54:178–182. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Verma A, Chander B, Verma S and Soni A:
Malignant brenner tumor of ovary. J Obstet Gynaecol India.
64:148–149. 2014. View Article : Google Scholar
|
|
3
|
Böcker W: WHO classification of breast
tumors and tumors of the female genital organs: Pathology and
genetics. Verh Dtsch Ges Pathol. 86:116–119. 2002.PubMed/NCBI
|
|
4
|
Leoncini L: Brenner tumor of the broad
ligament. Arch De Vecchi Anat Patol. 64:97–102. 1980.PubMed/NCBI
|
|
5
|
Angeles-Angeles A, Gutiérrez-Villalobos
LI, Lome-Maldonado C and Jiménez-Moreno A: Polypoid Brenner tumor
of the uterus. Int J Gynecol Pathol. 21:86–87. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shaco-Levy R and Benharroch D: Vaginal
brenner tumor. Int J Gynecol Pathol. 32:238–241. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Caccamo D, Socias M and Truchet C:
Malignant Brenner tumor of the testis and epididymis. Arch Pathol
Lab Med. 115:524–527. 1991.PubMed/NCBI
|
|
8
|
Goldman RL: A brenner tumor of the testis.
Cancer. 26:853–856. 1970. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Arhelger RB and Bocian JJ: Brenner tumor
of the uterus. Cancer. 38:1741–1743. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bürger T, Schildhaus HU, Inniger R, Hansen
J, Mayer P, Schweyer S, Radzun HJ, Ströbel P and Bremmer F:
Ovarian-type epithelial tumours of the testis: Immunohistochemical
and molecular analysis of two serous borderline tumours of the
testis. Diagn Pathol. 10:1182015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dierickx I, Valentin L, Van Holsbeke C,
Jacomen G, Lissoni AA, Licameli A, Testa A, Bourne T and Timmerman
D: Imaging in gynecological disease (7): Clinical and ultrasound
features of Brenner tumors of the ovary. Ultrasound Obstet Gynecol.
40:706–713. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Moon WJ, Koh BH, Kim SK, Kim YS, Rhim HC,
Cho OK, Hahm CK, Byun JY, Cho KS and Kim SH: Brenner tumor of the
ovary: CT and MR findings. J Comput Assist Tomogr. 24:72–76. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Roma AA and Masand RP: Ovarian Brenner
tumors and Walthard nests: A histologic and immunohistochemical
study. Hum Pathol. 45:2417–2422. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nogales FF Jr, Matilla A, Ortega I and
Alvarez T: Mixed Brenner and adenomatoid tumor of the testis: An
ultrastructural study and histogenetic considerations. Cancer.
43:539–543. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ross L: Paratesticular Brenner-like tumor.
Cancer. 21:722–726. 1968. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Vechinski TO, Jaeschke WH and Vermund H:
Testicular tumors. An analysis of 112 consecutive cases. Am J
Roentgenol Radium Ther Nucl Med. 95:494–514. 1965. View Article : Google Scholar : PubMed/NCBI
|