Introduction
As a rare subtype of aggressive ossifying fibroma,
psammomatoid ossifying fibroma (POF), also termed juvenile
ossifying fibroma, is a benign fibro-osseous lesion predominantly
affecting the paranasal sinuses and orbits of children and young
adults (1). Histopathology reveals a
densely cellular fibrous stroma interspersed with numerous small,
spherical ossicles or psammoma bodies. It is locally aggressive,
with a high risk of relapse if not completely resected. The present
case report presented a large recurrent POF in a male patient.
Case report
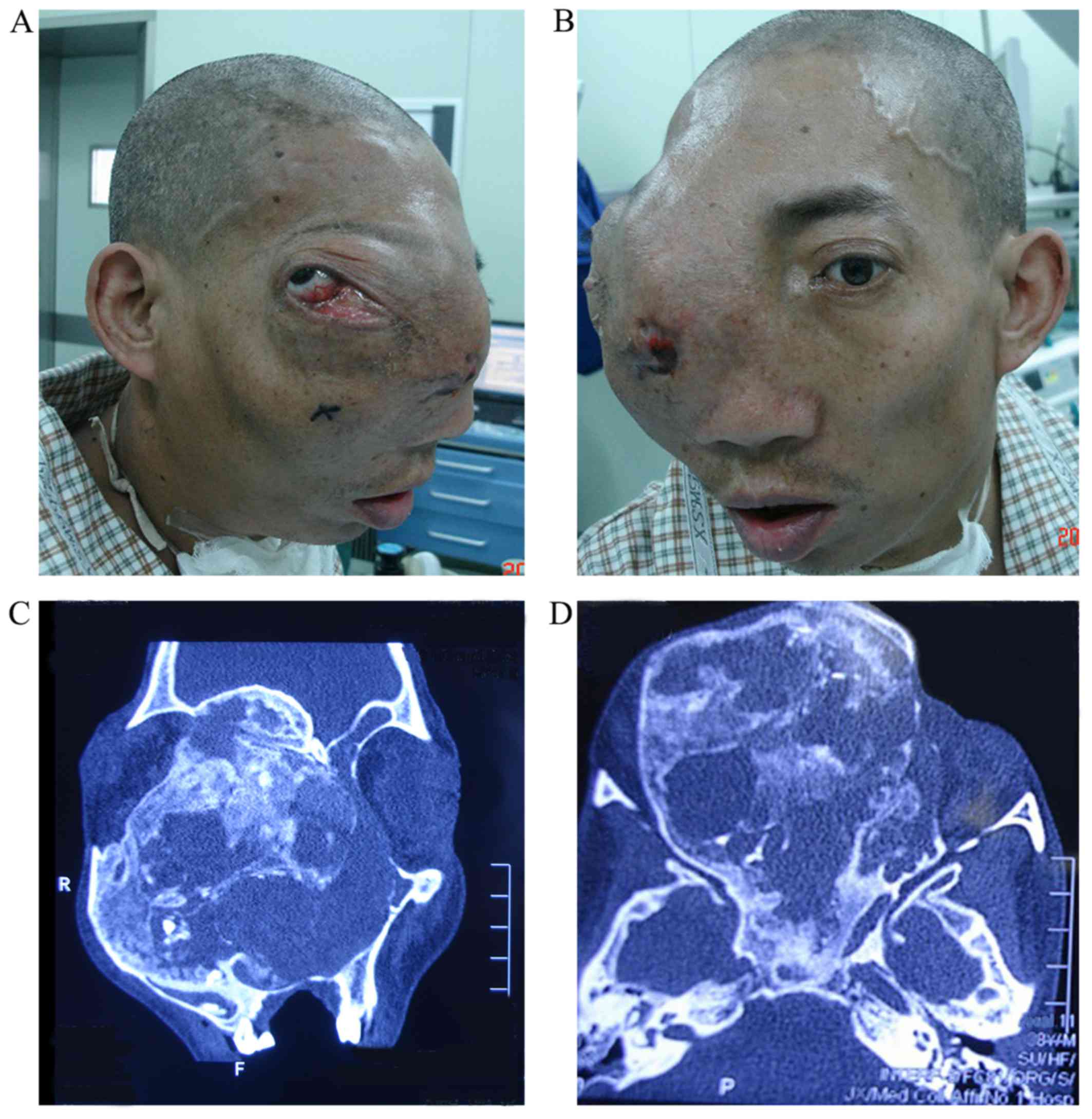
A 39-year-old male presented with a 30 year history
of progressive right eye proptosis and decreasing vision without
any obvious pain. The tumor had resulted in right craniofacial
deformity, as well as right lateral displacement of the eye ball
(Fig. 1A and B). Also, the expansile
mass had caused partial airway obstruction of the nasal cavity,
nasopharynx and oropharynx, accompanying incomplete eyelid closure
and restrictive movement of the right eye. Computed tomography (CT)
scans revealed a well demarcated, ground-glass opacity expansive
lesion extending into the right frontal, maxillary, orbit and
paranasal sinuses, with the volume of 9.4×9.8×10.5 cm (Fig. 1C and D). Due to the large tumor size,
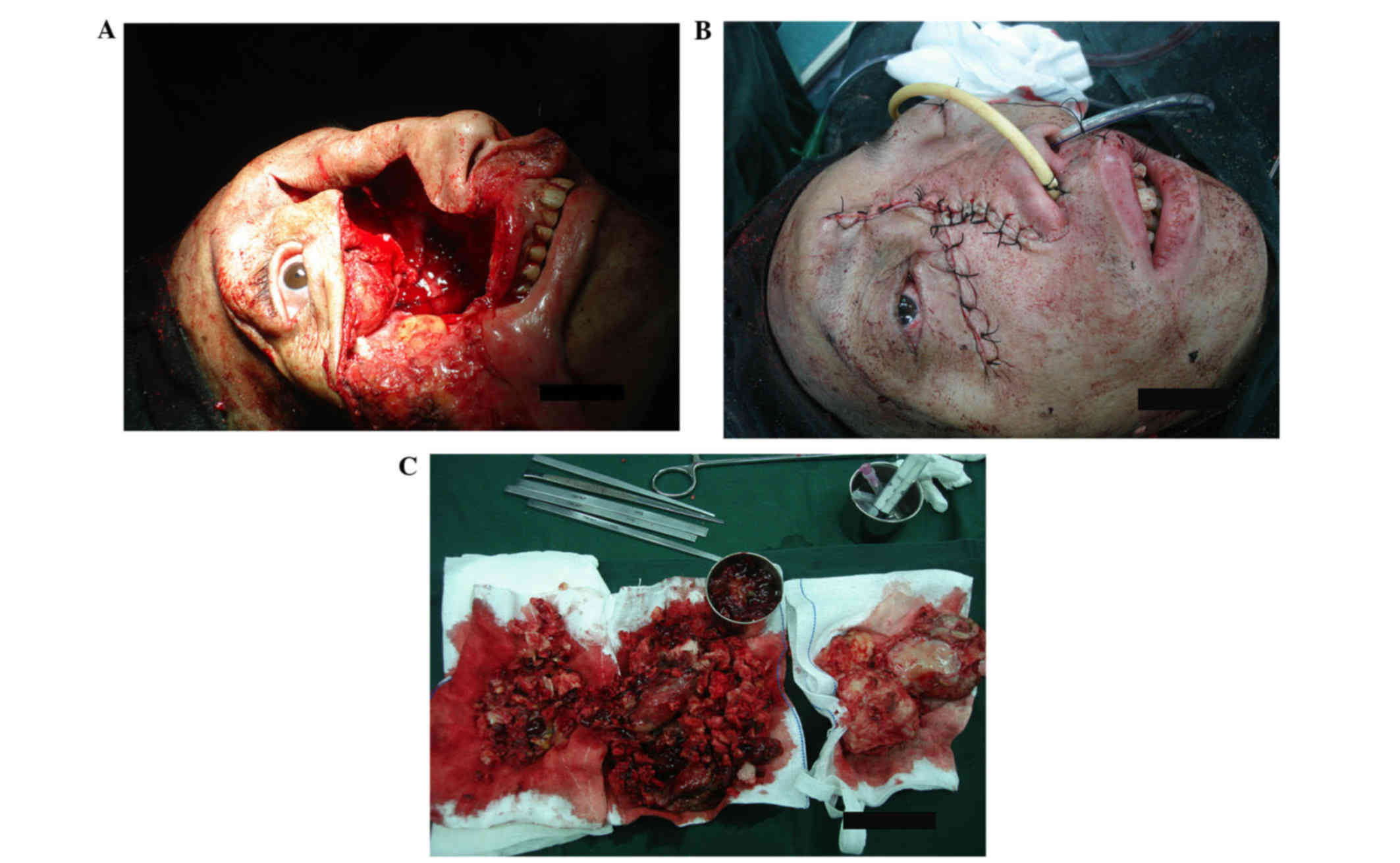
surgical removal of the lesion was the predominant treatment
(Fig. 2A and B). In addition,
pre-operative tracheotomy and external carotid artery embolization
was utilized to relieve dyspnea and reduce tumor vascularity. The
tumor appeared friable and well-vascularized with an irregular
surface. Following the removal of the tumor, the bony anterior
skull base remained paper-thin. Gelatin sponge and tela iodoform
was placed in the cavity and removed after 6 days.
The histopathology of the specimen revealed
gray-white and gray-red soft tissue, and bone fragments were
17×16×6 cm in aggregate (Fig. 2C).
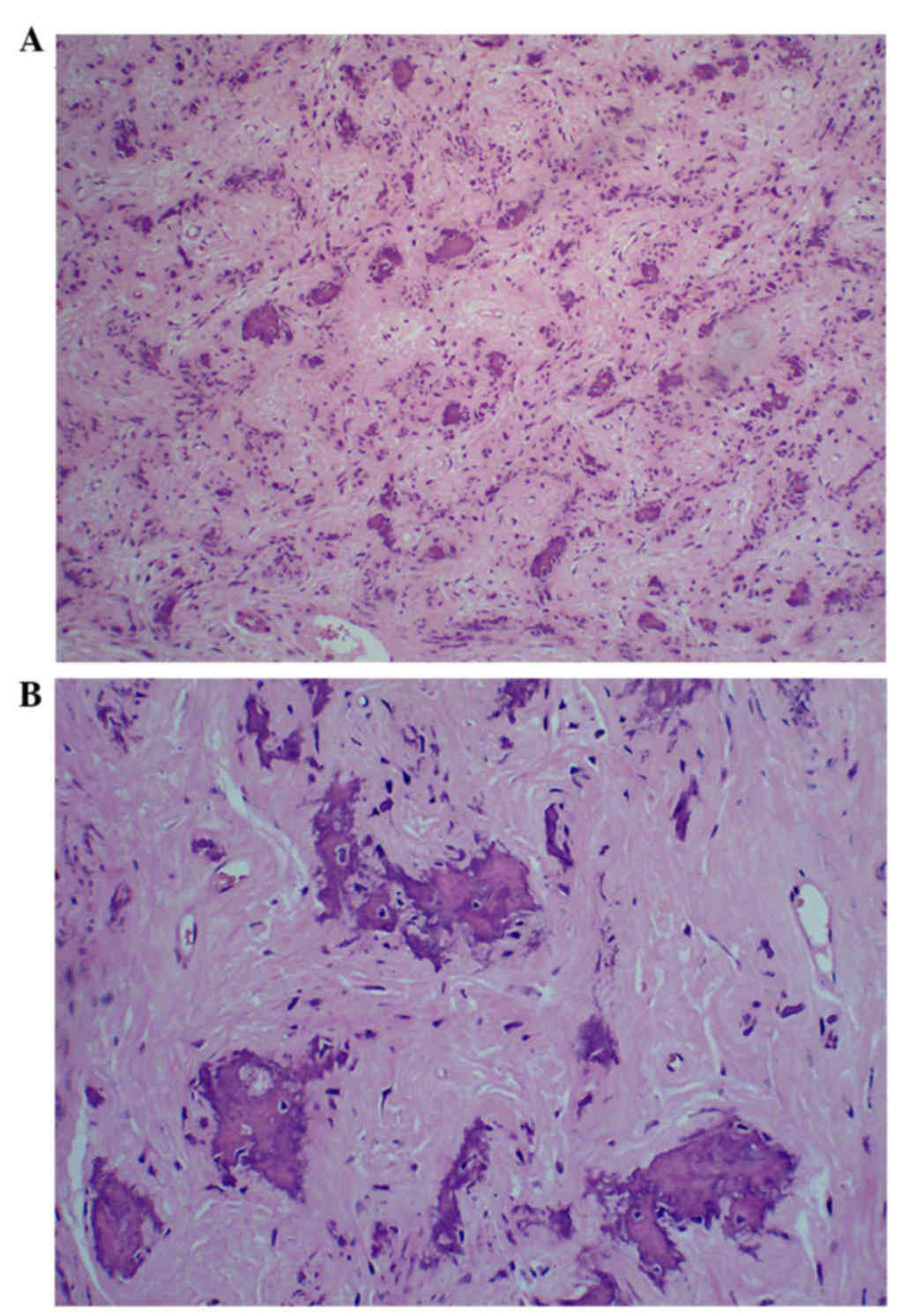
Microscopic examination revealed that the tumor with necrotic
lesions consisted of dense fibroblastic stroma with interspersed
areas of ossification and resembling psammoma bodies (Fig. 3). The pathological diagnosis was
POF.
At 13 days after surgery, the patient was discharged
without any complications. The patient was free from symptoms and
exhibited partial regression of the right eye proptosis. At the 5
month follow-up, satisfactory clinical outcome was observed. The
patient recovered well and the right eye-ball mobility was
undisturbed. CT scans revealed no recurrence in the area of nasal
cavity, nasopharynx and paranasal sinuses.
Discussion
Benign fibro-osseous craniofacial lesions include
fibrous dysplasia, ossifying fibroma and cemento-osseous dysplasia.
Ossifying fibroma is divided into conventional ossifying fibroma
and juvenile ossifying fibroma. According to the 2005 World Health
Organization classification of odontogenic tumors, juvenile
ossifying fibroma is further divided into juvenile POF and juvenile
trabecular ossifying fibroma (2).
Due to the similarity of certain histopathological features,
accurate diagnosis depends on the clinical, radiological and
histological features.
POF is a rare subtype of aggressive ossifying
fibroma and the etiology of POF remains unclear. POF is distinct
from other lesions on the basis of its site, clinical behavior,
histopathological features and age of occurrence. POF occurs more
commonly in children and young adults, although it has also been
reported in patients ranging in ages between 3 months and 72 years
(3). POF typically affects regions,
including the maxilla bone, paranasal sinuses, orbits and the
fronto-ethmoidal complex. By contrast juvenile trabecular ossifying
fibroma commonly affects patients younger than those affected by
POF, and usually arises in the maxilla or mandible with rapid
growth (4).
Clinical manifestations of POF include proptosis,
lateral displacement of the eye ball, decreasing vision with
progressive blindness and progressive craniofacial deformity. Other
symptoms include airway obstruction, headaches, facial swelling and
recurrent sinusitis. Local expansion of the lesion may extend into
adjacent structures, including the paranasal sinuses, nasal cavity,
nasopharynx, palate and cranial cavity.
Radiologically, CT scans of the POF revealed an
expansile mass and radiolucent lesion, which is well-circumscribed
by a thick bony shell with a multiloculated internal appearance and
a content of varying density. Sometimes the lesion has a
ground-glass appearance and a variable quantity of internal
calcifications, as observed in the present case. In addition,
magnetic resonance imaging reveals a mass with a thick outer shell
and assists with delineating the extent of the mass. The
radiography makes it possible to distinguish POF from other
fibro-osseous lesions, including fibrous dysplasia, since fibrous
dysplasia is less demarcated and poorly circumscribed by a fibrous
capsule (5).
Histologically, the characteristic of POF is the
presence of numerous small, spherical ossicles or psammoma bodies
that are embedded in a densely cellular fibrous stroma (6). The lesion is well-circumscribed and
interspersed with osteoblastic rimming of trabeculae and a large
quantity of vascularized fibrous stroma. Certain previous studies
have reported concurrent aneurysmal bone cyst formation with POF
(7). By contrast, fibrous dysplasia
is poorly delineated, with irregular trabeculae of woven bone or
ovoid calcifications without lamellar bone and osteoblastic rimming
of the trabeculae. Juvenile trabecular ossifying fibroma contains
osteoid matrix surrounded by trabeculae of fibrillary osteoid and
woven bone.
The predominant treatment for POF is complete
surgical excision of the tumor, and partial or incomplete removal
leads to recurrence (8). POF is
locally aggressive and potentially extends into adjacent vital
structures. In the present case, an open surgical approach was
employed to resect the tumor as it affords visibility of integrate
tumor thereby allowing complete removal. Also, the specimen for
pathology is commonly fragmented, making it impossible to evaluate
surgical margins appropriately. The successful surgical excision
requires multidisciplinary co-operation, involving neurosurgeons,
ophthalmologists and otolaryngologists. In the present case, the
prognosis of the patient was considered good without malignant
degeneration and metastases, which was evidenced by post-operative
radiological examination indicating complete removal of the
tumor.
References
|
1
|
Linhares P, Pires E, Carvalho B and Vaz R:
Juvenile psammomatoid ossifying fibroma of the orbit and paranasal
sinuses. A case report. Acta Neurochir (Wien). 153:1983–1988. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sarode SC, Sarode GS, Waknis P, Patil A
and Jashika M: Juvenile psammomatoid ossifying fibroma: A review.
Oral Oncol. 47:1110–1116. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bohn OL, Kalmar JR, Allen CM, Kirsch C,
Williams D and Leon ME: Trabecular and psammomatoid juvenile
ossifying fibroma of the skull base mimicking psammomatoid
meningioma. Head Neck Pathol. 5:71–75. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Patigaroo SA: Juvenile psammomatoid
ossifying fibroma (JPOF) of maxilla-a rare entity. J Maxillofac
Oral Surg. 10:155–158. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Figueiredo LM, de Oliveira TF, Paraguassú
GM, de Hollanda Valente RO, do Costa WR and Sarmento VA:
Psammomatoid juvenile ossifying fibroma: Case study and a review.
Oral Maxillofac Surg. 18:87–93. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zawadzka-Glos L, Brozek-Madry E, Chmielik
M, Brzewski M, Biejat A and Maldyk J: Aggressive psammomatoid
ossifying fibroma in a 3-month-old boy-A case report. International
Journal of Pediatric Otorhinolaryngology Extra. 6:143–145. 2011.
View Article : Google Scholar
|
|
7
|
Nasser MJ: Psammomatoid ossifying fibroma
with secondary aneurysmal bone cyst of frontal sinus. Child Nerv
Syst. 25:1513–1516. 2009. View Article : Google Scholar
|
|
8
|
Noudel R, Chauvet E, Cahn V, Mérol JC,
Chays A and Rousseaux P: Transcranial resection of a large
sinonasal juvenile psammomatoid ossifying fibroma. Child Nerv Syst.
25:1115–1120. 2009. View Article : Google Scholar
|