Introduction
Renal transplantation has been associated with a
significantly increased risk of developing cancers during long-term
follow-up. A recent meta-analysis identified a 3.18-fold higher
standardised incidence for bladder cancer in kidney transplant
recipients compared with the general population (1). The underlying mechanisms are multiple,
including cellular damage by immunosuppressive therapy, i.e.,
cyclophosphamide therapy or viral factors, such as BK virus
infection (2). The histological
findings are mostly consistent with urothelial carcinoma (3).
Paragangliomas, also referred to as extra-adrenal
pheochromocytomas, originate from mature chromaffin cells located
along the para-aortic and paravertebral axis (4). The urinary bladder is the third most
frequent primary site (11%), after the organ of Zuckerkandl (53%)
and the adrenal glands (26%), followed by the mediastinum (5%) and
the neck (5%) (5). The majority of
bladder paragangliomas are solitary, arising on the dome or on the
trigone.
We herein report the case of a kidney transplant
recipient with a bladder polyp consistent with paraganglioma of the
bladder. To the best of our knowledge, this is the first report of
a case of paraganglioma of the bladder in a kidney tranplant
recipient.
Case report
A 67-year-old woman was admitted to the Necker
Hospital in April, 2013, for bladder polyp resection 2 years after
renal transplantation. The patient had been dialyzed for 33 years
for chronic tubulointerstitial nephritis and had a history of
endometrial carcinoma treated by complete hysterectomy in 1990; she
was also treated for left adrenal pheochromocytoma by left radical
nephrectomy in 1991. The patient had been a smoker (20 pack-years)
but had quit 20 years prior to the kidney transplantation. The main
complaints on admission were general fatigue and weight loss; based
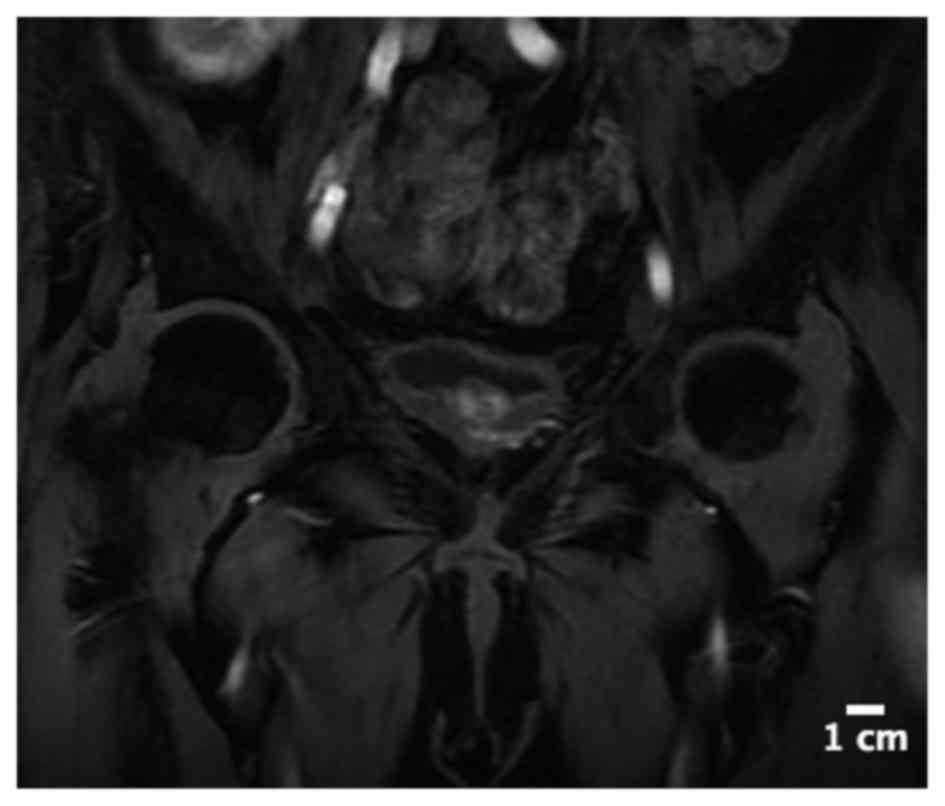
on these symptoms, abdominal computed tomography (CT) and magnetic
resonance imaging (MRI) examinations were performed and revealed a
bladder polyp (Fig. 1). There was no
hematuria or dysuria. The blood and urinary tests were unremarkable
(creatinine: 1.6 mg/dl, normal range: 0.4–1.1 mg/dl; and C-reactive
protein: 6 mg/dl, normal range: 0–10 mg/dl). The treatment included
prednisone 6 mg/day, azathioprine 75 mg/day, tacrolimus 5 mg/day,
furosemide 60 mg/day and atenolol 100 mg/day.
During bladder polyp resection, the patient
developed severe hypertension (240/110 mmHg) and flush associated
with flash pulmonary edema and acute coronary syndrome (serum
troponin: 2.53 ng/ml, normal range: <0.04 ng/ml), which resolved
with diuretics, heparin and antiplatelet treatment in association
with antihypertensive drugs (alpha- and beta-blockers).
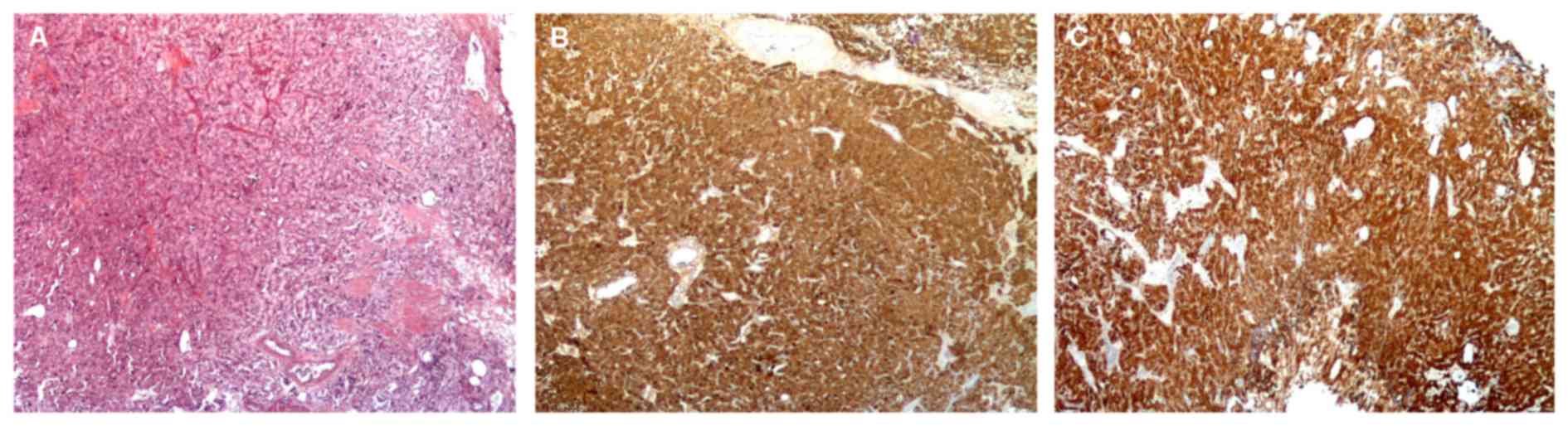
The histological analysis of the resected bladder
polyp was consistent with extra-adrenal pheochromocytoma, or
paraganglioma (Fig. 2). The patient
was asymptomatic and reported no hypertension, malaise or
thunderclap headache after voiding.
The urinary excretion of normetanephrine (286
nmol/mmol creatininuria; normal, <280 nmol/mmol creatininuria)
was marginally increased, but that of metanephrine was not (109
nmol/mmol creatininuria; normal, <200 nmol/mmol creatininuria).
Bladder MRI revealed a lesion in the bladder trigone, sized
16×11×16 mm, exhibiting contrast uptake without locoregional
dissemination. A positron emission tomography (PET) /CT scan using
18F-dihydroxyphenylalanine (F-DOPA) revealed no
metastatic dissemination. The patient finally underwent partial
cystectomy. On the last follow-up visit (January, 2017) there was
no postoperative recurrence in the absence of any additional
treatment.
Discussion
Paragangliomas, also referred to as extra-adrenal
pheochromocytomas, are often benign and non-functional tumors,
i.e., there is no secretion of metanephrine and/or catecholamine
(6). Paragangliomas of the urinary
bladder are rare. The first case of bladder pheochromocytoma was
reported in 1953 by Zimmerman et al (7). From this date onwards, >185 cases
have been reported in the literature to date (6).
Bladder paragangliomas represent 9.8% of all
extra-adrenal paragangliomas and only account for 0.06% of all
primary urinary bladder tumors. Urinary bladder paragangliomas
predominantly affect women, with a mean age of 45 years, and are
usually located intramurally in the lateral and posterior walls and
the trigone of the bladder, with a mean size of 1.9 cm (8).
The clinical symptoms are usually associated with
micturition, and they may include hematuria, flush, paroxysmal
hypertension, headache, palpitations or blurred vision during or
after voiding (8).
Diagnosis is based on the correlation of clinical
symptoms, biological results (such as elevation of urinary
catecholamines), specific localizations with F-DOPA uptake on
PET/CT and histological findings (including immunohistochemical
staining with neuroendocrine markers). A proportion of
pheochromocytomas are clinically silent and, in the majority of
those cases, the levels of catecholamines and their metabolites in
the blood and urine are found to be normal (9).
Malignancy is estimated at a rate of 5–15% (9). Genetic studies have recently
established the importance of various mutations in the progression
of paragangliomas to malignancy. The association of succinate
dehydrogenase subunit B gene mutations with pelvic paragangliomas
is frequently reported (10).
These tumors are characterized by symptom recurrence
with tumor mobilization. Cystoscopy under local anesthesia may
cause a hypertensive crisis due to bladder filling and should be
deferred whenever this diagnosis is considered.
The definitive treatment is surgical and consists of
partial cystectomy. Radiotherapy by either 131I-MIBG or
the radioactive somatostatin analogue 177Lu-octreotate
and chemotherapy may be used in cases of metastasis dissemination
(6).
To the best of our knowledge, this is the first case
of pheochromocytoma recurrence or multiple pheochromocytoma in a
kidney transplant recipient. Paraganglioma of the urinary bladder
is a rare occurrence, but it should be considered if tumor
resection is associated with a hypertensive crisis. This type of
surgery is associated with a high risk of hemodynamic failure and
should be performed with intensive care unit support.
References
|
1
|
Yan L, Chen P, Chen EZ, Gu A and Jiang ZY:
Risk of bladder cancer in renal transplant recipients: A
meta-analysis. Br J Cancer. 110:1871–1877. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Alexiev BA, Randhawa P, Martul E Vazquez,
Zeng G, Luo C, Ramos E, Drachenberg CB and Papadimitriou JC: BK
virus-associated urinary bladder carcinoma in transplant
recipients: Report of 2 cases, review of the literature, and
proposed pathogenetic model. Hum Pathol. 44:908–917. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Prabharasuth D, Moses KA, Bernstein M,
Dalbagni G and Herr HW: Management of bladder cancer after renal
transplantation. Urology. 81:813–819. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Edström E, Mahlamäki E, Nord B, Kjellman
M, Karhu R, Höög A, Goncharov N, Teh BT, Bäckdahl M and Larsson C:
Comparative genomic hybridization reveals frequent losses of
chromosomes 1p and 3q in pheochromocytomas and abdominal
paragangliomas, suggesting a common genetic etiology. Am J Pathol.
156:651–659. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Madani R, Al-Hashmi M, Bliss R and Lennard
TWJ: Ectopic pheochromocytoma: Does the rule of tens apply? World J
Surg. 32:3342008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Beilan JA, Lawton A, Hajdenberg J and
Rosser CJ: Pheochromocytoma of the urinary bladder: A systematic
review of the contemporary literature. BMC Urol. 13:222013.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zimmerman IJ, Biron RE and Macmahon HE:
Pheochromocytoma of the urinary bladder. N Engl J Med. 249:25–26.
1953. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schaefer IM, Gunawan B, Füzesi L, Blech M,
Frasunek J and Loertzer H: Chromosomal imbalances in urinary
bladder paraganglioma. Cancer Genet Cytogenet. 203:341–344. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Doran F, Varinli S, Bayazit Y, Bal N and
Ozdemir S: Pheochromocytoma of the urinary bladder. APMIS.
110:733–736. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Burnichon N, Rohmer V, Amar L, Herman P,
Leboulleux S, Darrouzet V, Niccoli P, Gaillard D, Chabrier G,
Chabolle F, et al: The succinate dehydrogenase genetic testing in a
large prospective series of patients with paragangliomas. J Clin
Endocrinol Metab. 94:2817–2827. 2009. View Article : Google Scholar : PubMed/NCBI
|