Introduction
Metanephric adenoma is a rare benign neoplasm of the
kidney that occurs predominantly in middle-aged women, with few
cases reported in childhood (1).
Only 0.2% of adult renal epithelial neoplasms are diagnosed as
metanephric adenoma (2).
Histogenetically, this lesion resembles epithelial
Wilms' tumor; metanephros, which is formed from the ureteric bud
and the metanephric blastema, is of mesodermal origin, and
metanephric adenoma and Wilms' tumor are both derived from remnants
of the metanephric blastema (1).
Thus, from a clinical and diagnostic perspective, metanephric
adenoma must be differentiated from Wilms' tumor, oncocytoma and
papillary renal cell carcinoma (RCC).
The preoperative diagnosis of this benign tumor
based on radiological findings is typically difficult; however,
accurate diagnosis is of great importance as it may avoid
unnecessary radical surgery (1). In
the present study, in order to further the understanding of the
characteristics of metanephric adenoma, a case is described along
with its immunohistochemical and radiographic findings.
Case report
A 21-year-old woman with past history of thyroid
tumor presented to the Department of Urology at Kanazawa University
Hospital (Kanazawa, Japan) in May 2014 with a complaint of left
lower back pain. There were no significant findings on physical
examination. The results of the urinalysis, blood test and chest
X-ray were normal.
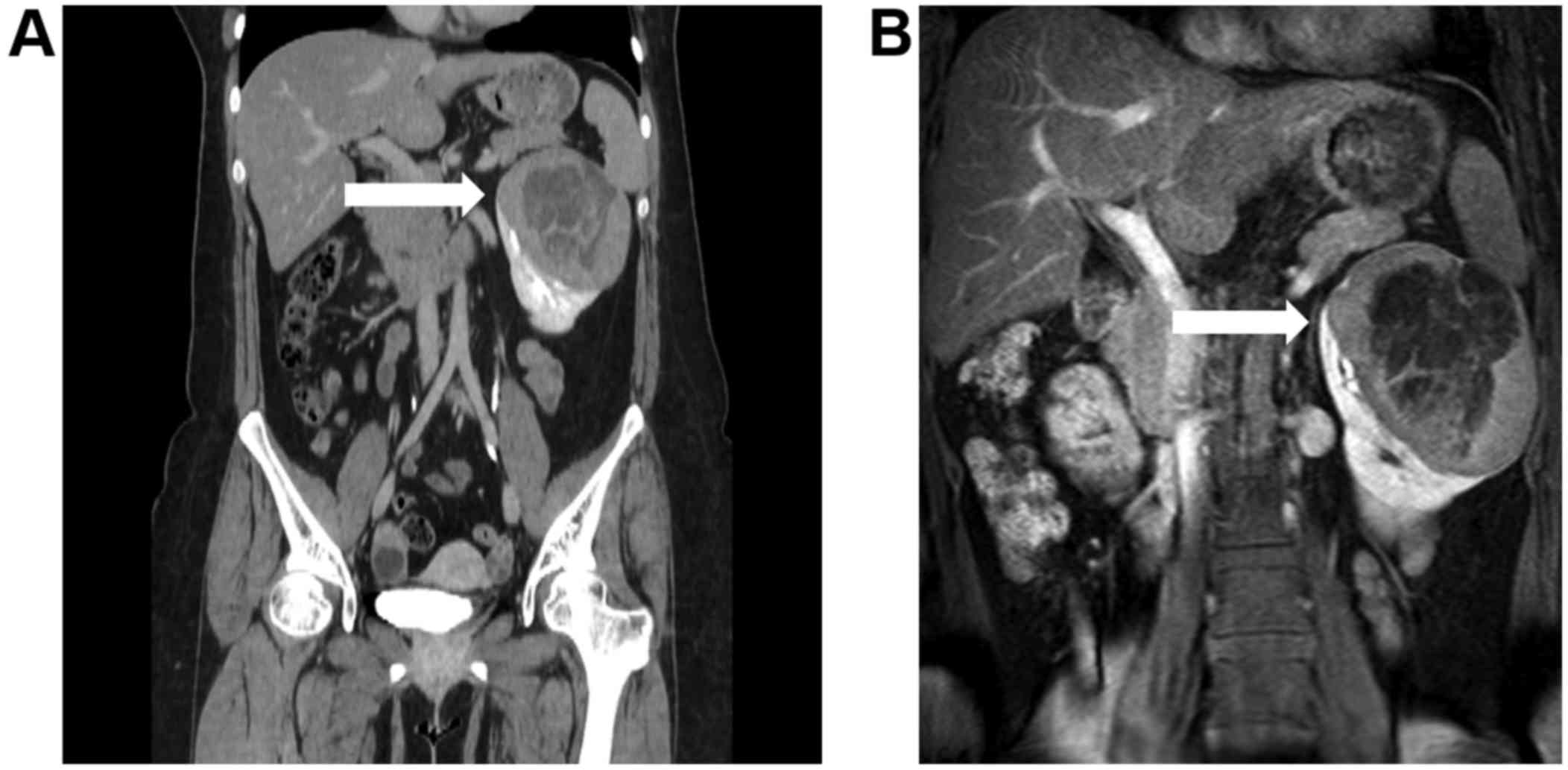
Abdominal computed tomography (CT) and magnetic
resonance imaging (MRI) revealed a large, round tumor occupying the
upper and middle regions of the left kidney (Fig. 1A and B). The tumor was not clearly
enhanced in the early contrast phase on CT imaging. There were no
significant findings on bone scintigraphy. The preoperative
diagnosis was papillary RCC, and a laparoscopic left nephrectomy
was performed, with 294 min of the operation time and 50 ml of
total bleeding.
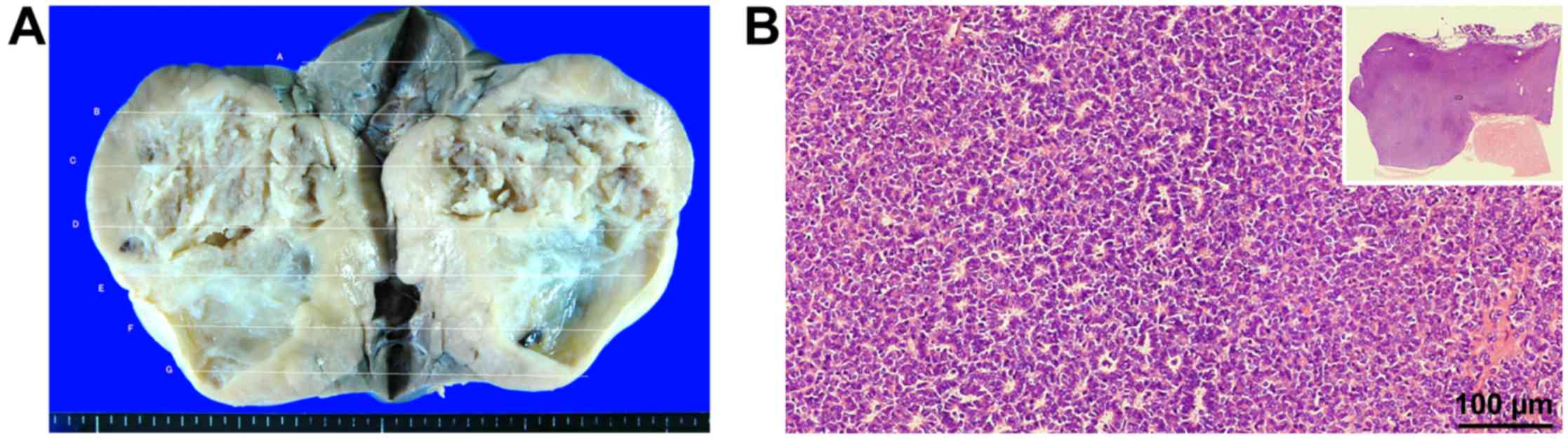
Macroscopically, the tumor contained white and
yellow regions, and measured 115×100×60 mm (Fig. 2A). On hematoxylin-eosin staining, the
number of epithelial cells with scant acidophilic cytoplasm was
increased compared with that of normal kidney tissue, and these
epithelial cells formed the tubular structures (Fig. 2B). These histological features were
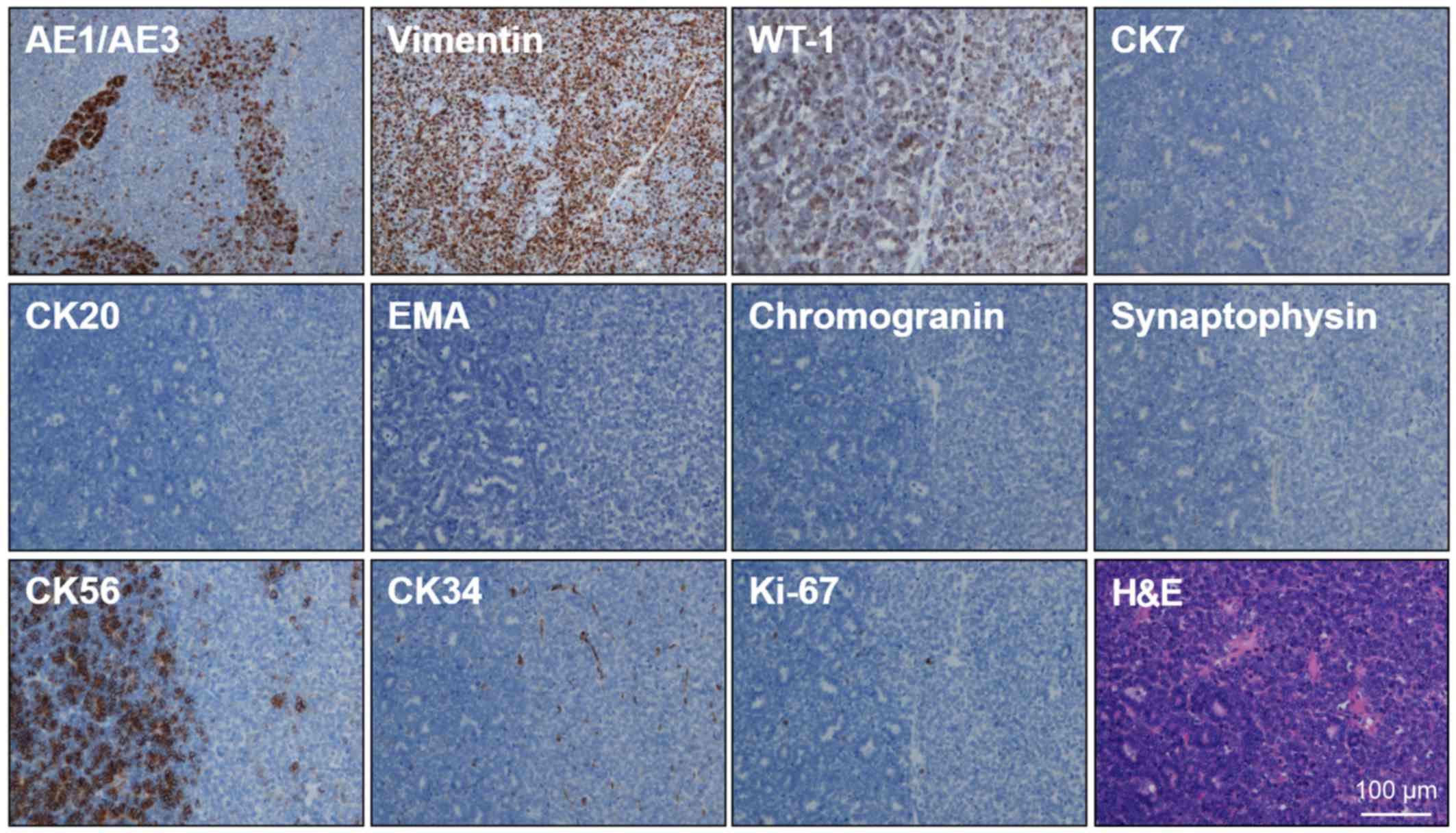
not consistent with RCC. Immunohistochemical staining revealed
positive immunoreactivity for vimentin and Wilms' tumor 1, whereas
cytokeratin (CK) AE1/AE3, CK56, and CK34 were partially positive.
CK7, CK20, epithelial membrane antigen, chromogranin A and
synaptophysin were negative, and there were very few Ki-67 positive
cells (0.2%; Fig. 3). These findings
were consistent with metanephric adenoma.
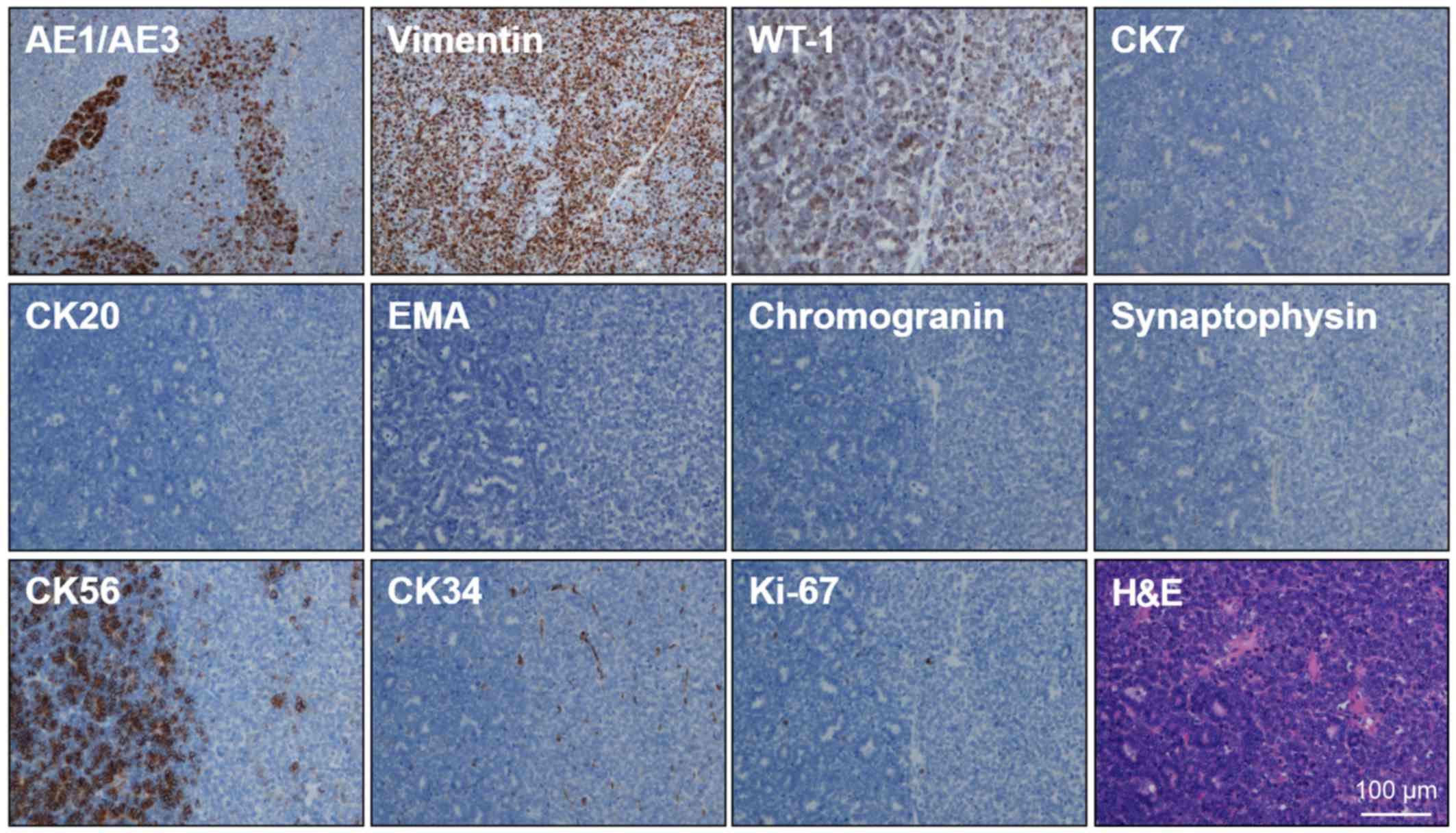 | Figure 3.Immunohistochemical staining results.
The tumor was positive for vimentin and WT-1, partially positive
for CK AE1/AE3, CK56 and CK34, and negative for CK7, CK20, EMA,
chromogranin and synaptophysin. The Ki-67 index was low. All images
are shown at the same magnification level. Hematoxylin
counterstaining was used. WT-1, Wilms' tumor 1; CK, cytokeratin;
EMA, epithelial membrane antigen; H&E, hematoxylin-eosin. |
A follow-up CT scan was performed 1 year after
surgery, and revealed no local recurrence or metastasis.
Discussion
Metanephric adenoma is a rare neoplasm that accounts
for 0.2% of adult renal epithelial neoplasms (2). Davis et al (3) reported the largest series of 50 cases
of metanephric adenoma, which included patients ranging in age from
5 to 83 years (median, 44 years). There was a distinct female
preponderance, with an approximate female:male ratio of 2:1. Almost
50% of the cases were asymptomatic and identified incidentally. The
most common presenting symptoms were abdominal pain and hematuria.
The mean tumor size was 5.5 cm, with a range of 0.3–15.0 cm
(3).
From a clinical and diagnostic perspective,
metanephric adenoma must be differentiated from Wilms' tumor,
oncocytoma and papillary RCC. Radiologically, metanephric adenoma
shows hypovascularity on contrast-enhanced CT; however, Wilms'
tumor and papillary RCC exhibit similar features (3). On T2-weighted MRI, metanephric adenoma
often exhibits low-intensity signals, which is also similar to the
findings of papillary RCC. Thus, radiological examination is not
sufficient to allow a diagnosis of metanephric adenoma, as
demonstrated in the present case.
The difficulty of diagnosing metanephric adenoma
prior to surgery is also due to the extremely low frequency of its
occurrence (4). However,
preoperative diagnosis is important to avoid excessive treatment,
such as neoadjuvant therapy. Although two previous studies reported
that needle biopsy could aid in diagnosing metanephric adenoma
(4), nephrectomy was performed in
the majority of previously reported cases as the entity could not
be distinguished from a malignant tumor (5). In order to increase the rate of
accurate diagnosis of metanephric adenoma, it should be considered
in the differential diagnosis of renal masses, particularly in
patients who are female and middle-aged, and have hypovascular
tumors with clear borders.
The majority of metanephric adenomas are diagnosed
following radical nephrectomy (5).
However, radical nephrectomy may be unnecessary for patients with
this disease as it is known to be a benign tumor. A previous study
reported the case of an 11-year-old patient with a mixed tumor,
which consisted of metanephric adenoma containing foci of Wilms'
tumor or papillary RCC (6). In that
case, metastasis was observed subsequent to surgery. In addition, a
previous case report of pure metanephric adenoma in a child
described the occurrence of lymph node metastasis subsequent to
surgery (7). To the best of our
knowledge, no previous study has reported the occurrence of
metastasis in an adult patient with metanephric adenoma. However,
the possibility of metastasis cannot be excluded, and surgical
treatment may be required, particularly in cases involving large
tumors, as large tumors have a greater probability than small
tumors of containing mixed pathological tissues. In cases of small,
hypovascular tumors occurring in middle-aged women, needle biopsy
may be appropriate, and this may be also be necessary if the
patient is unfit to undergo radical nephrectomy due to advanced age
or renal dysfunction.
In summary, the present study reports a case of
metanephric adenoma that was treated by laparoscopic nephrectomy.
Although metanephric adenoma is difficult to diagnose
preoperatively, this rare disease must be considered in order to
avoid unnecessary surgical procedures in these patients.
References
|
1
|
Pasricha S, Gandhi JS, Gupta G, Mehta A
and Beg S: Bilateral, multicenteric metanephric adenoma associated
with Wilms' tumor in a child: A rare presentation with important
diagnostic and therapeutic implications. Int J Urol. 19:1114–1117.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hwang SS and Choi YJ: Metanephric adenoma
of the kidney: Case report. Abdom Imaging. 29:309–311. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Davis CJ Jr, Barton JH, Sesterhenn IA and
Mostofi FK: Metanephric adenoma. Clinicopathological study of fifty
patients. Am J Surg Pathol. 19:1101–1114. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Terao H, Matsumoto T, Umemoto S, Onuki T,
Kobayashi K, Ohgo Y, Nogcchi S, Kishi H, Tsuura Y and Nagashima Y:
Metanephric adenoma: Report of two cases. Hinyokika Kiyo.
54:599–602. 2008.PubMed/NCBI
|
|
5
|
Ebine T, Ohara R, Momma T, Saito S and
Kuramochi S: Metanephric adenoma treated with laparoscopic
nephrectomy. Int J Urol. 11:232–234. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Drut R, Drut RM and Ortolani C: Metastatic
metanephric adenoma with foci of papillary carcinoma in a child: a
combined histologic, immunohistochemical, and FISH study. Int J
Surg Pathol. 9:241–247. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Renshaw AA, Freyer DR and Hammers YA:
Metastatic metanephric adenoma in a child. Am J Surg Pathol.
24:570–574. 2000. View Article : Google Scholar : PubMed/NCBI
|