Introduction
Imaging technology is continuously improving, and
advanced diagnostic imaging modalities such as high resolution
ultrasonography (US), computed tomography (CT) and magnetic
resonance imaging (MRI) can obtain images of wider areas over
shorter times. Along with this technical advancement, the detection
of unexpected lesions has increased (1). Such findings are referred to as
‘incidental findings’. Incidental findings include masses (often
called ‘incidentalomas’) or anatomic malformations. Incidental
thyroid nodular lesions are common and were first identified on CT
(2–4).
The most common type of thyroid nodule lesions are
benign while approximately 20% are malignant. Most of the malignant
lesions in the thyroid are papillary thyroid carcinoma (PTC),
followed by follicular, medullary, and anaplastic thyroid carcinoma
(5). On CT or MRI, malignant nodules
do not have specific imaging findings (6,7). PTC ≤1
cm is defined as papillary thyroid micro-carcinoma (PTMC), and it
is the most prevalent type of papillary thyroid carcinoma. A
diameter of 1 cm is regarded as the cut-off above which US
examination is suggested for incidental thyroid nodule (1).
In the present study, we examined factors including
frequency, size, age, and sex with regard to the incidental finding
of thyroid nodules in patients presenting for oral and
maxillofacial CT examination. Additionally, we conducted a
retrospective review of patients without a history of thyroid
disease who underwent CT examination in our institution between
January 2009 and December 2009 for oral and maxillofacial pathology
with incidental findings in the thyroid.
Case report
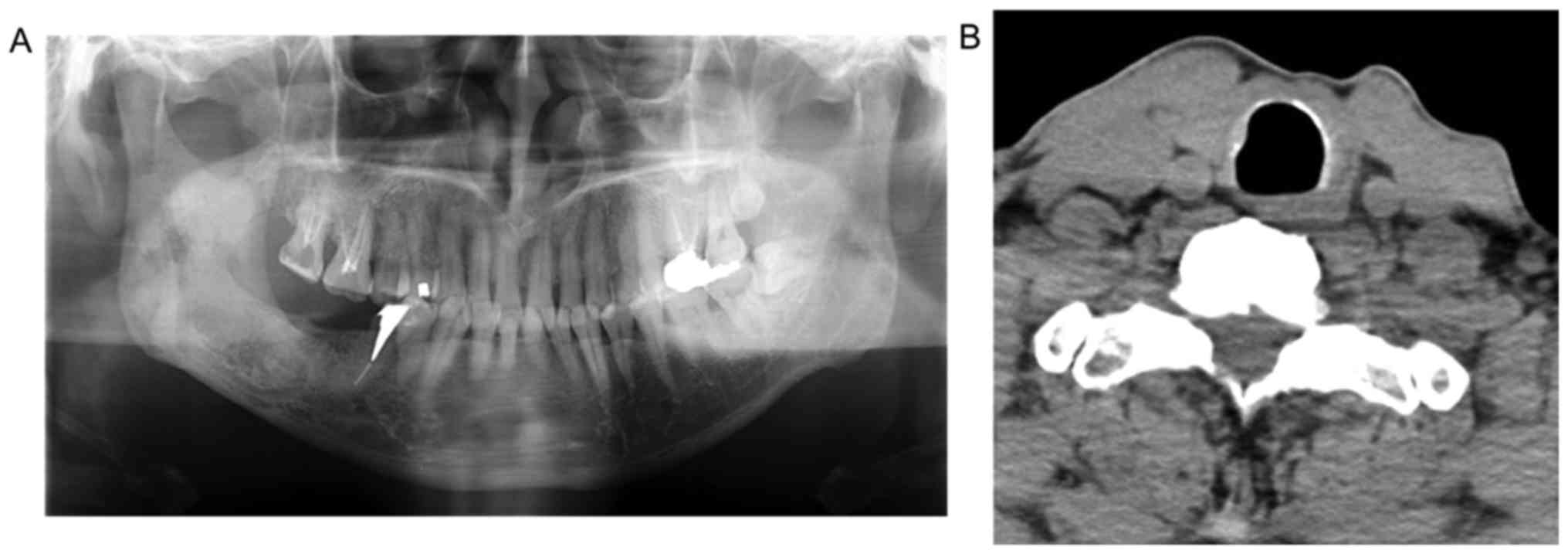
A 59-year-old man was referred from a private dental
practice. He had undergone an extraction of first molar of right
mandible for spontaneous pain. Following the extraction, the
symptoms persisted, and he was referred to our university hospital.
A panoramic radiograph showed a multiloculated radiolucency
extending from the third molar area of the right mandible extending
to the mandibular ramus. There was no root resorption of the second
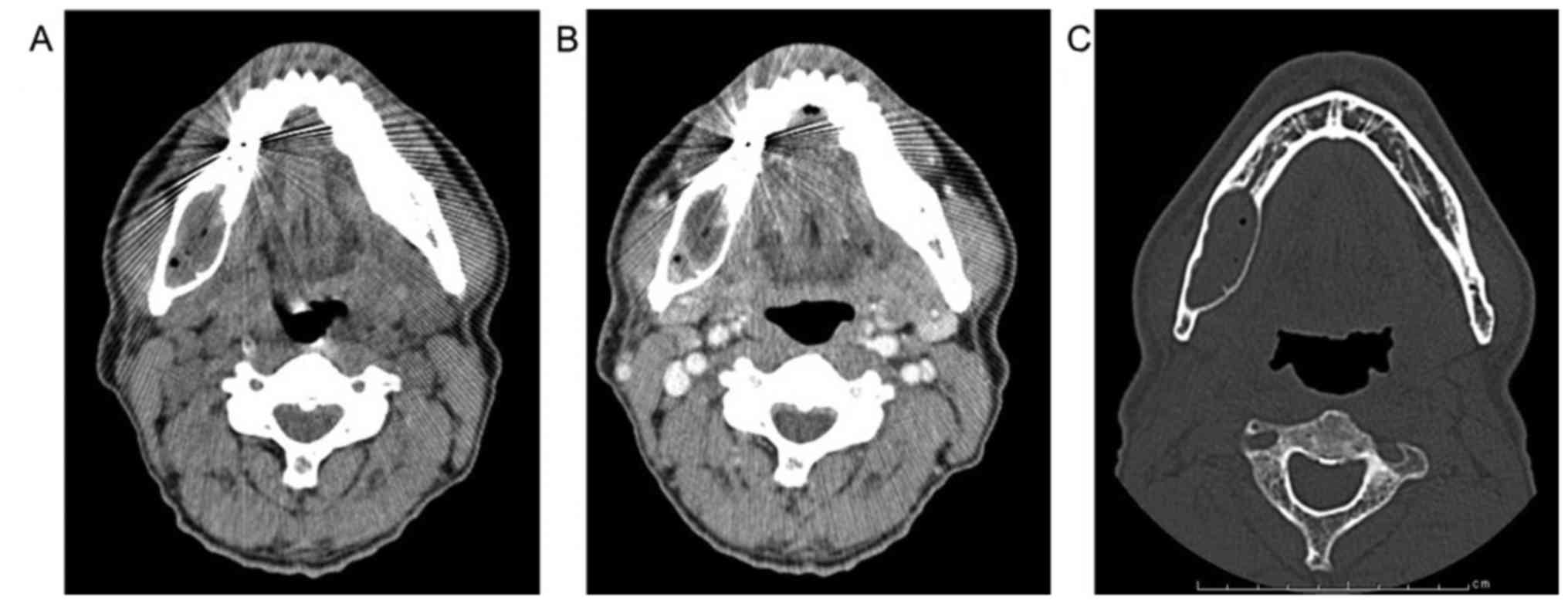
molar (Fig. 1). CT images
demonstrated low density in the multiloculated area with lingual
expansion. The interior of the lesion was of heterogeneous soft
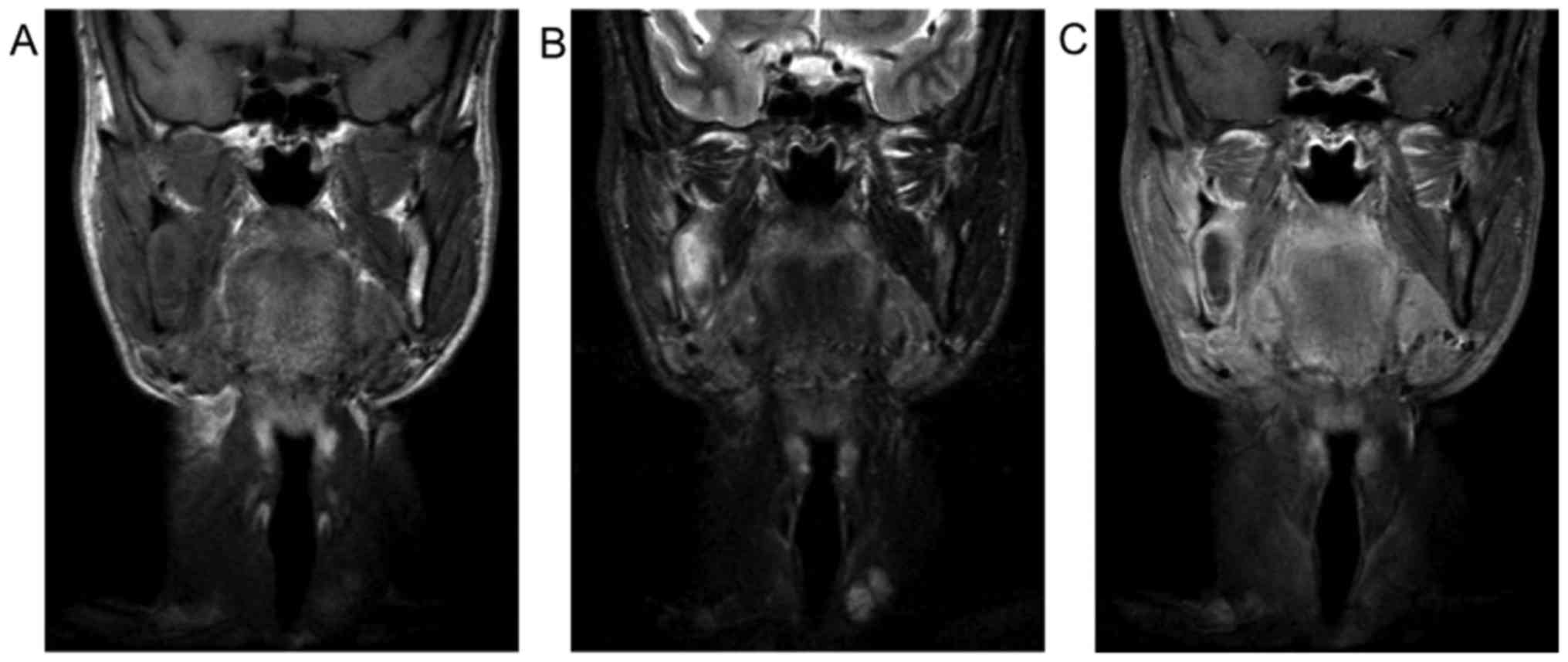
tissue density that did not undergo contrast enhancement (Fig. 2). MR images showed intermediate
signal intensity (SI) on T1WI, high to markedly high SI on STIR and
strong enhancement of the lesion's wall and weak enhancement inside
the lesion (Fig. 3). Based on these
findings, a preliminary diagnosis of keratocystic odontogenic tumor
was made.
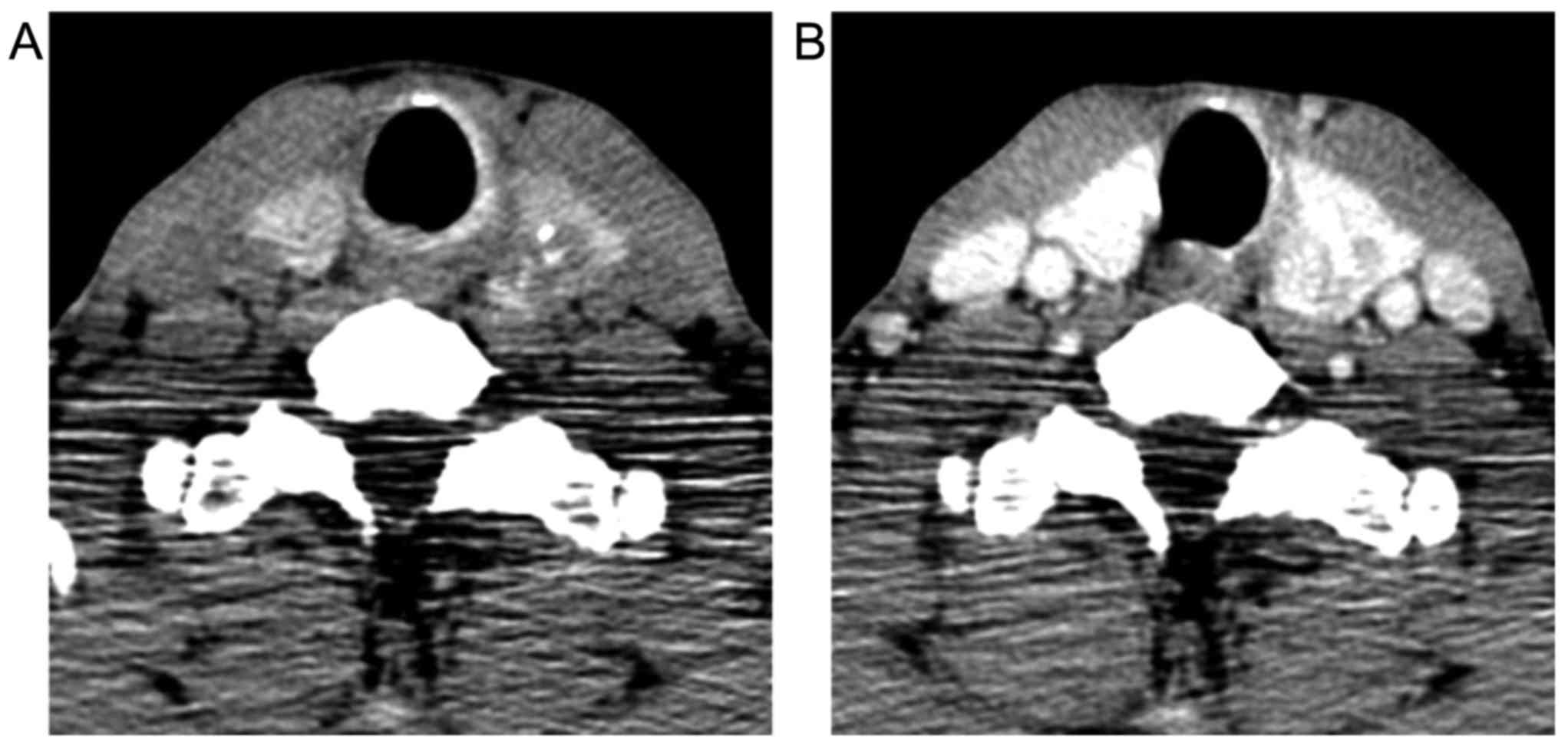
On the same CT images, the left lobe of the thyroid
was enlarged by a 28-mm nodule containing calcifications. It showed
non-uniform low density, and heterogeneous contrast enhancement
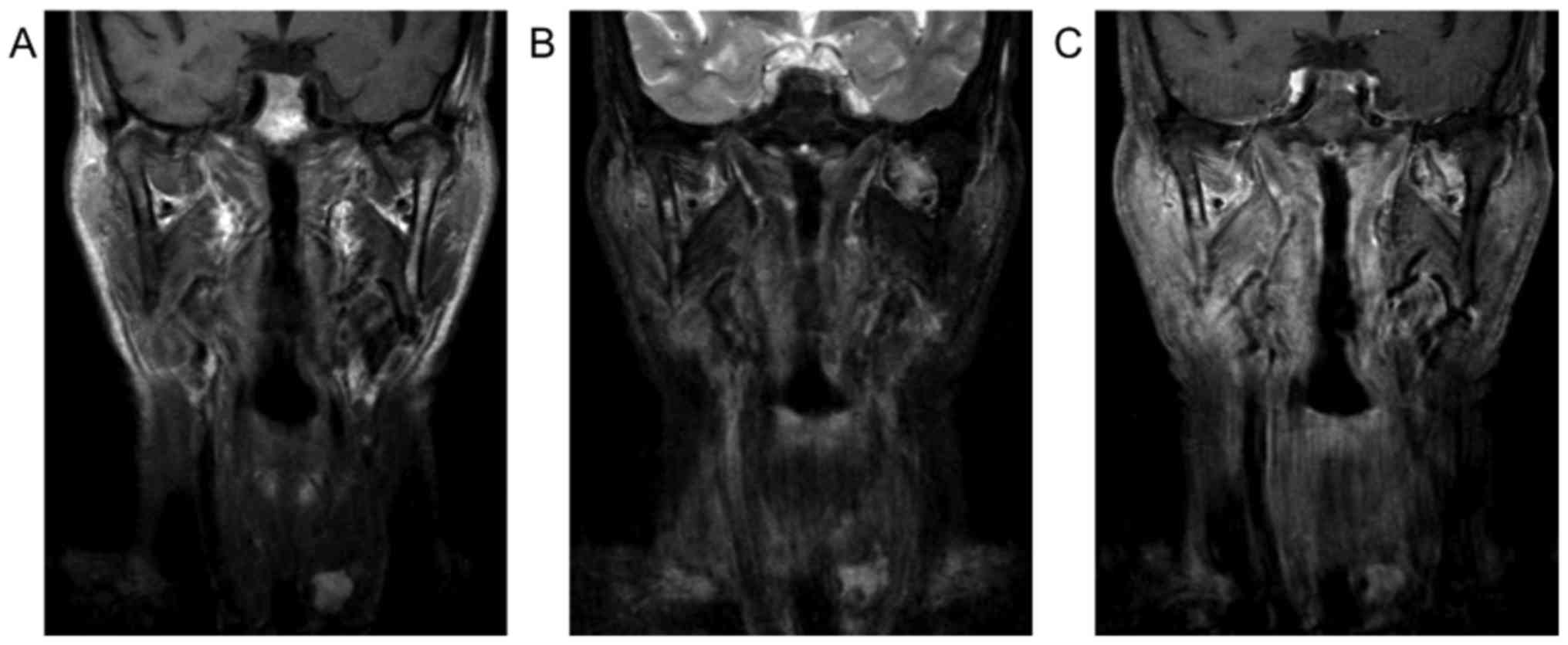
(Fig. 4). MR images demonstrated
high SI on T1WI and STIR and strong enhancement on CE-T1WI
(Fig. 5).
The patient was referred to the Department of Breast
and Thyroid Surgery. Fine-needle aspiration biopsy (FNAB) of the
thyroid nodule suggested category V (suspicious for malignancy)
based on the Bethesda System for reporting thyroid cytopathology.
He was treated with a total thyroidectomy and bilateral neck
dissection. The histological diagnosis of the surgical specimen was
papillary thyroid carcinoma. A CT performed 3 months after surgery
showed no evidence of recurrence (Fig.
6). After the patient's recovery from surgery, fenestration was
performed on the right mandibular lesion. After 3 years, panoramic
images showed no lesion recurrence in the mandible. Ten years
post-thyroidectomy, the patient is well with no evidence of
recurrence.
Retrospective review. In total, 169 patients, 87
males and 82 females, with a mean age of 67.3 years (range, 17–92
years), as well as 65 patients (38.5%), 43 (66.2%) female and 22
(33.8%) male had abnormal findings in the thyroid for one year.
Discussion
Use of advance radiology devices in oral and
maxillofacial region such as US, CT, MRI and PET-CT could produce
high quality examination of the maxillofacial region and contiguous
structures and organs. Based on the increase of quality and usage
of the devices, incidental findings in USG, CT and MRI examination
are often found.
Incidental finding is an unexpected discovery rather
than the initial purpose for which the radiographic examination was
carried out. Incidental findings may be anatomy disorder or
neoplasm, most of which are asymptomatic and insidious. In head and
neck, the most common area of incidentaloma is thyroid (8). Thyroid nodules appear with nodular or
rim calcification on CT images and may likely be malignant
(3). However, unlike US which has
adequate spatial resolution such as microcalcification or margin
detail, CT and MR images have no indicators to differentiate
between benign and malignant tumors (6,7). Both
benign and malignant tumors demonstrated intermediate signal
intensity on T1WI and high signal intensity on T2WI, even if in our
case showed high signal intensity in T1WI and STIR. Additional
investigations are required to determine malignancy such us US or
FNA (7,9–11).
Papillary thyroid carcinoma is the most common
malignant tumor in thyroid. Some risk factors of PTC are associated
with ionizing radiation exposure, particularly head and neck or
total body irradiation for bone marrow transplantation and family
history of thyroid carcinoma (12).
The PTC with less than 5 mm in diameter has almost no metastatic
potential. On PTC case size and patient age are important for
treatment consideration. Some study of PTC has grouping PTC based
on size (2,7,10,11,13).
PTC with <5 mm known as papillary thyroid microcarcinoma (PTMC),
in elderly patients, progressivity of lesion was not evident during
observation and immediate surgery was not needed (4,11,13).
As age is one of the considerations for PTC
treatment, clinicians tend to focus on younger patients (7,10) as
progression of the disease is more likely in younger patients
compared to elderly patient (2,13). In
addition, the ratio of malignant and benign was higher in younger
patients, although age was not an independent predictor of PTMC
(10,11,13).
Noguchi et al reported that thyroid PTMC
prevalence was higher in women (11), similar with our retrospective survey,
which showed a predominance of cases in females, although some
authors reported that sex was not an independent predictor of PTMC,
as the high incidence of PTMC in women was due to more frequent
exposure to diagnostic or treatment procedures (10). Radiologists have an important role to
determine incidental finding and provide a complete report and to
be aware about the potential of malignancy (4). Tanpitukponse et al reported only
a small proportion of incidental finding of thyroid lesions from CT
and MRI examinations that were referred from radiologists to
clinicians, had undergone additional examination (14). Patient age and nodule size influenced
clinicians to make decisions regarding additional examination
(6,11,13–15).
Hoang et al reported that 2 cm is the threshold size of CT
and MR examinations for incidental finding of thyroid lesion
(6). Other factors that should be
considered include patient comorbid condition or financial
condition. In addition, different perceptions between radiologists
and clinicians towards incidental finding pose a potential problem.
Therefore, collaboration between radiologists and clinicians is
imperative in the incidental finding of thyroid lesion.
In summary, the wider usage of CT and MR devices on
head neck examination increases the incidental finding of PTC.
Treatment consideration and prognosis of incidental finding of PTC
depend on nodule size and patient age. Collaboration between
radiologists and clinicians is important in the incidental finding
of PTC.
References
|
1
|
Johnson PT, Horton KM, Megibow AJ, Jeffrey
RB and Fishman EK: Common incidental findings on MDCT: Survey of
radiologist recommendations for patient management. J Am Coll
Radiol. 8:762–767. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nguyen XV, Choudhury KR, Eastwood JD,
Lyman GH, Esclamado RM, Werner JD and Hoang JK: Incidental thyroid
nodules on CT: Evaluation of 2 risk-categorization methods for
work-up of nodules. AJNR Am J Neuroradiol. 34:1812–1817. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yoon DY, Chang SK, Choi CS, Yun EJ, Seo
YL, Nam ES, Cho SJ, Rho YS and Ahn HY: The prevalence and
significance of incidental thyroid nodules identified on computed
tomography. J Comput Assist Tomogr. 32:810–815. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hoang JK, BF IV Branstetter, Gafton AR,
Lee WK and Glastonbury CM: Imaging of thyroid carcinoma with CT and
MRI: Approaches to common scenarios. Cancer Imaging. 13:128–139.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rosenkrantz AB: Differences in perceptions
among radiologists, referring physicians, and patients regarding
language for incidental findings reporting. AJR Am J Roentgenol.
208:140–143. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hoang JK, Langer JE, Middleton WD, Wu CC,
Hammers LW, Cronan JJ, Tessler FN, Grant EG and Berland LL:
Managing incidental thyroid nodules detected on imaging: White
paper of the ACR Incidental Thyroid Findings Committee. J Am Coll
Radiol. 12:143–150. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shetty SK, Maher MM, Hahn PF, Halpern EF
and Aquino SL: Significance of incidental thyroid lesions detected
on CT: Correlation among CT, sonography, and pathology. AJR Am J
Roentgenol. 187:1349–1356. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
American Thyroid Association (ATA)
Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid
Cancer, ; Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL,
Mandel SJ, Mazzaferri EL, McIver B, Pacini F, et al: Revised
American Thyroid Association management guidelines for patients
with thyroid nodules and differentiated thyroid cancer. Thyroid.
19:1167–1214. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hoang JK, Lee WK, Lee M, Johnson D and
Farrell S: US Features of thyroid malignancy: Pearls and pitfalls.
Radiographics. 27:847–865. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Slijepcevic N, Zivaljevic V, Marinkovic J,
Sipetic S, Diklic A and Paunovic I: Retrospective evaluation of the
incidental finding of 403 papillary thyroid microcarcinomas in 2466
patients undergoing thyroid surgery for presumed benign thyroid
disease. BMC Cancer. 15:3302015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Noguchi S, Yamashita H, Uchino S and
Watanabe S: Papillary microcarcinoma. World J Surg. 32:747–753.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Xu L, Li G, Wei Q, El-Naggar AK and
Sturgis EM: Family history of cancer and risk of sporadic
differentiated thyroid carcinoma. Cancer. 118:1228–1235. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ito Y, Miyauchi A, Kihara M, Higashiyama
T, Kobayashi K and Miya A: Patient age is significantly related to
the progression of papillary microcarcinoma of the thyroid under
observation. Thyroid. 24:27–34. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tanpitukpongse TP, Grady AT, Sosa JA,
Eastwood JD, Choudhury KR and Hoang JK: Incidental thyroid nodules
on CT or MRI: Discordance between what we report and what receives
workup. AJR Am J Roentgenol. 205:1281–1287. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tufano RP, Noureldine SI and Angelos P:
Incidental thyroid nodules and thyroid cancer: Considerations
before determining management. JAMA Otolaryngol Head Neck Surg.
141:566–572. 2015. View Article : Google Scholar : PubMed/NCBI
|