Introduction
Microsatellite instability (MSI) is a type of
genetic instability resulting from alterations in the DNA mismatch
repair (MMR) system. The microsatellites are mono-, di- or
trinucleotides, distributed in non-coding regions of the human
genome. Approximately 15% of all colorectal adenocarcinomas (CRCs)
display MSI, which occurs due to a germline mutation in one of the
MMR genes, such as hMSH2 (2p16), hMSH6 (2p16),
hPMS1 (2q31), hPMS2 (7p22) or TGFβRII,
or to epigenetic silencing of hMLH1 (3p21). Of these
mutations, the most common are those in the genes encoding the
hMSH2 and hMLH1 proteins, whereas hypermethylation of MLH1
occurs in only 2–3% of CRCs (1–5). CRC is
the second cause of digestive tract cancer-related mortality.
According to the International Classification of Disease (ICD-10,
revised in 2009), primary epithelial neoplasms of the appendix are
grouped within CRC. This type of cancer develops at the tip or base
of the appendix, and has an incidence of 0.082%. The peak incidence
of epithelial neoplasms is usually between 50 and 60 years of age,
and their association with sex is controversial. The symptoms of
appendiceal carcinoma tend to be subtle, particularly in the early
stages (6–10). Appendiceal tumors include adenomas,
adenocarcinomas, mucinous neoplasms, undifferentiated carcinoma,
small-cell carcinoma, and signet ring cell carcinoma (SRCC). Some
classify cystadenocarcinomas and non-cystic tumors separately
(11,12). Mucinous adenocarcinomas represent
~45% of all appendiceal tumors (13,14). The
peritoneal spread of mucin allows such deposits to accumulate in
particular areas, including the greater omentum, the undersurface
of the right hemidiaphragm, the pelvic cavity and the right
retrohepatic space. This redistribution is the result of tumor cell
accumulation at the sites where ascitic fluid is reabsorbed in the
abdomen. The selection of the surgical procedure depends on the
type of appendiceal carcinoma, as well as the location and size of
the tumor mass. The recommended treatment is right hemicolectomy
followed by combined adjuvant intraperitoneal chemotherapy,
supplemented by additional cycles of systemic chemotherapy
(15–18). The reported 5-year survival for
appendiceal carcinoma patients ranges between 20 and 60%, depending
on the degree of invasion of parenchymal organs and/or regional
lymph node metastases (19–21). CRC with MSI has distinctive
characteristics, including the tendency to arise in the proximal
colon, as well as poor differentiation, extensive lymphocytic
infiltration, presence of signet ring cells and abundant mucin.
Patients with MSI tumors appear to have a better
prognosis compared with those with microsatellite stable tumors
(22); however, the response to
5-fluorouracil (5-FU)-based chemotherapy regimens are poorer with
MSI tumors (23,24). At present, little information is
available regarding the prevalence of MSI in appendiceal
adenocarcinoma.
Case report
A 62-year-old man consulted a private physician due
to a 6-month history of diffuse abdominal pain (4/10 intensity) of
the colic type, radiating toward the right iliac fossa, right
testicle and thigh. The pain was associated with distension and
accompanied by chills; there was no reported nausea, vomiting,
fever, or changes in the evacuation pattern. Palpation of the
abdominal region did not reveal any masses. One week after the
clinical symptoms worsened, including pain intensification, an
axial computerized tomography (CT) scan of the abdominal area was
performed, revealing increased density of the greater omentum. An
inflammatory process was ruled out at this stage. The results of
routine laboratory analyses, including hematological and hepatic
function tests, were normal. The measurement of carcinoembryonic
antigen detected a level of <2.0 mcg/l (normal, 0–2.5 mcg/l)
during the diagnosis, treatment and follow-up of the patient.
Exploratory laparoscopy and appendectomy were performed, and the
pathological examination of the surgical specimen revealed an
uncommon appendicular lesion, namely tubulovillous
adenocarcinoma.
The postoperative period was uneventful, with
complete resolution of the abdominal pain. The patient was
discharged from the hospital in a good condition. One week later,
the patient was subjected to colonoscopy, which revealed no traces
of suspicious lesions. Two months later, the patient was admitted
to the Memorial Sloan-Kettering Cancer Center (MSKCC; New York, NY,
USA) for a new evaluation and continuation of treatment. Based on
the evaluation, it was recommended that the patient underwent
debulking surgery. During the surgery, new lesions were identified
in the peritoneum, as well as under the spleen, leading to a
splenectomy and removal of the tail of the pancreas. In the
immediate postoperative period, an abdominal CT scan revealed a
pancreatic fistula, which was treated conventionally. Since the new
investigations revealed a bifurcated pancreas, it was not possible
to administer intraperitoneal chemotherapy. Nine months later, an
adjuvant chemotherapy scheme was initiated, with FOLFOX-6 for 10
cycles.
Laboratory and imaging studies were performed
initially every 4 months during the first 2 years, and every 6–8
months thereafter. After 5 years of follow-up, the patient remains
asymptomatic with no signs of tumor activity, and attends follow-up
visits every 12 months at the MSKCC.
Radiology report
Thorax
No signs of mediastinal adenopathy or pulmonary
infiltration were observed. In the inferior lobe of the left lung,
a 12.8-mm nodule of non-specific origin with well-defined borders
was identified.
First CT scan of the abdomen and
pelvis
Areas of high density were observed in the
peritoneal fat, suggestive of secondary metastases. The liver
parenchyma exhibited low-density round lesions, 3.5 mm in diameter,
with cystic characteristics, located in segments VII and VI.
Multiple diverticula were identified in the left and sigmoid
colon.
Second CT scan of the abdomen and
pelvis
An increase in density of the greater omentum was
detected, along with free liquid adjacent to the descending colon
and thickening of the distal portion of the cecal appendix.
Diagnostic methodology
Laparotomy
An appendectomy was performed, revealing an
inflammatory appendix with a retrocecal location and turbid
purulent liquid of inflammatory origin, along with omentitis.
Pathological examination
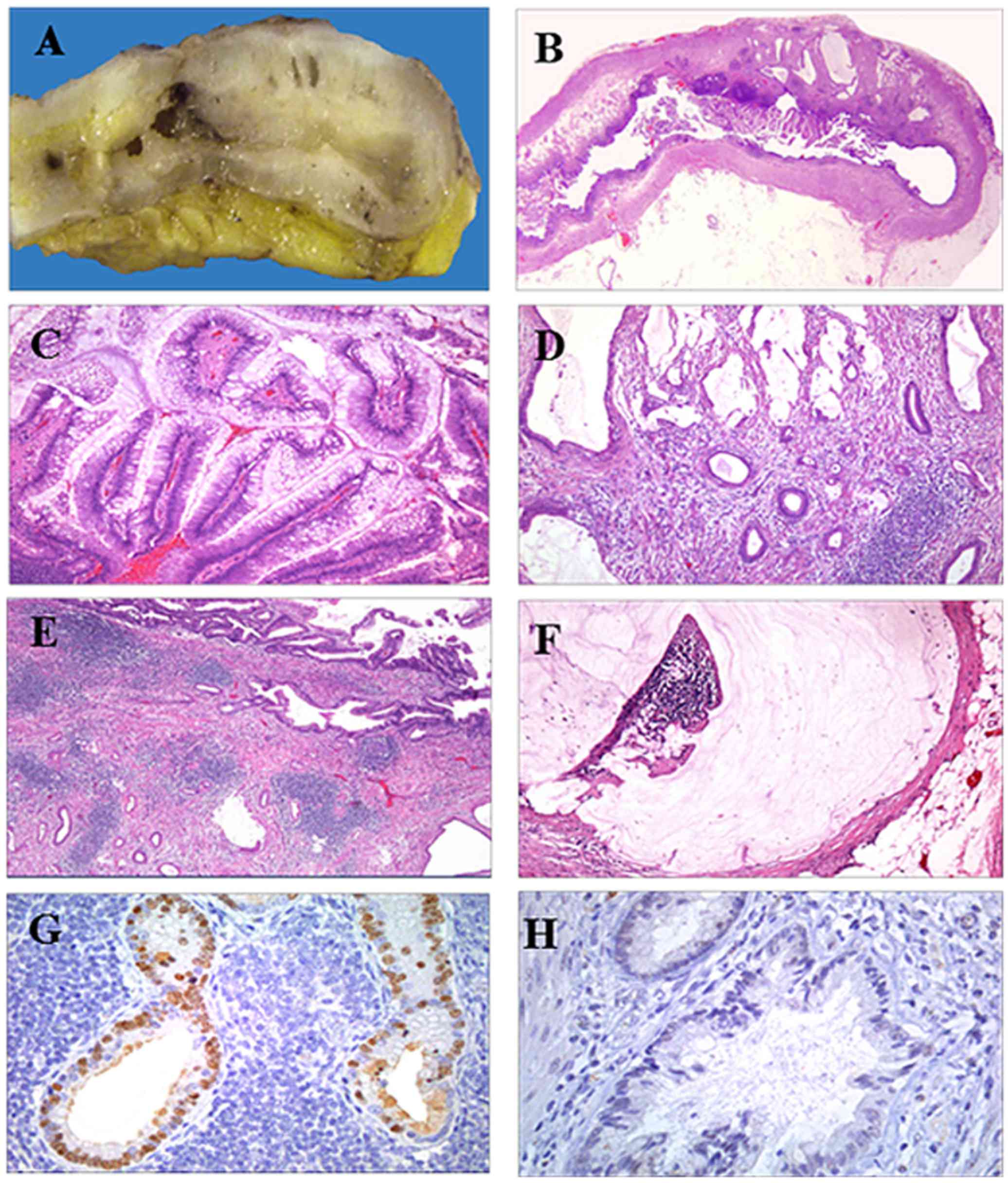
The appendix measured 6.1×0.9 cm and had a smooth
external surface. Upon sectioning, A 2.5-cm mass was encountered in
the distal third of the organ. The mass contained solid light-brown
and microcystic components, the latter being filled with mucin
(Fig. 1A and B).
Microscopic findings
The mucinous neoplasm was composed of benign tubular
glands and papillary structures (90%), the latter projecting into
the lumen. The glands and papillae were lined by a tall columnar
epithelium, which exhibited nuclear pseudostratification with mild
pleomorphism (Fig. 1C).
Part of the neoplasm (10%) consisted of small,
medium-sized, dilated and infiltrating glands that invaded the
appendicular wall and reached the subserosa (Fig. 1D). The invasive component was lying
in a sclerotic stroma and was accompanied by hyperplastic lymphoid
tissue (Fig. 1E).
The peritoneum displayed extracellular mucin
deposits, consistent with localized peritoneal adenomucinosis
(Fig. 1F). The diagnosis was
moderately differentiated adenocarcinoma with mucinous areas,
arising in a mucinous tubulopapillary adenoma. Selected sections
were obtained and embedded in paraffin for IHC analysis. The
following antibodies were used: Cytokeratin (CK) 20, CDX2, MLH-1,
MSH-2 and MSH-6.
The intestinal phenotype of tubulopapillary adenoma
and invasive adenocarcinoma was confirmed by positivity for CK20
and CDX2 (Fig. 1G). The
adenocarcinoma was negative for MLH-1, MSH-2 and MSH-6 (Fig. 1H). The pattern correlates with a
mismatch repair-deficient tumor or MSI-H.
Diagnosis
The following diagnosis was made for the patient: i)
Moderately differentiated adenocarcinoma (10% of the tumor) with
mucinous areas, infiltrating up to the subserosa (pT3), originating
in a tubulovillous adenoma (90% of the tumor) of the distal third
of the cecal appendix, with a largest diameter of 2.5 cm. ii)
Peritoneal adenomucinosis located in the periappendicular region (1
focus). iii) Surgical border (appendicular and mesoappendix) free
of tumor. iv) No lymphovascular or perineural invasion.
Materials and methods
IHC analysis
IHC staining was applied to identify CDX-2, MLH-1,
MSH-2 and MSH-6 expression. To prevent the non-specific binding of
antibodies, the sections were blocked with bovine serum albumin
(BSA) (Sigma-Aldrich Co., St. Louis, MO, USA) for 60 min. The
slides were then incubated with the primary antibody overnight at
4°C for the detection of anti-CDX-2 (AMT-28, sc-56818; dilution
1:25), anti-MLH-1 (N-20, sc-581; dilution 1:25), anti-MSH-2 (H-300,
sc-22771; dilution 1:50) (Santa Cruz Biotechnology, Santa Cruz, CA,
USA), anti-MSH-6 (HPA028446; dilution 1:100), and anti-CK-20
(SAB4502249; dilution 1:300) (Sigma-Aldrich), followed by
incubation with the appropriate secondary antibody
(Mouse/Rabbit-ImmunoDetector-HRP Cat. BSB0003-BioSB), at 1:200
dilution for 60 min at 37°C. The sections were washed and stained
with 3,3′-diaminobenzidine tetrahydrochloride (DAB) chromogen
(Zymed®/Invitrogen Inc., Carlsbad, CA, USA), and
hematoxylin was used for nuclear counterstaining (MHS-1,
Sigma-Aldrich). The sections were mounted with coverslips and
synthetic mounting medium (Entellan; Merck, Darmstadt, Germany;
OB046327).
In each case, negative controls were included that
lacked the primary antibody. Images were captured on a
Nikon-Eclipse 80i microscope coupled to a Nikon digital sight
camera (Melville, New York, NY, USA).
Discussion
Adenocarcinoma of the appendix is rare, constituting
<1% of all CRCs. Appendiceal tumors may exhibit atypical
clinical characteristics, representing a challenge for diagnosis
and treatment. Appendiceal neoplasms are seldom detected before or
during appendectomy, with <1.5% of the appendectomy specimens
harboring primary appendiceal cancers upon examination (25). CRC is divided into two general
groups, having either genomic pathways or MSI pathways.
The first group comprises 75–80% of all CRCs, while
the tumors with MSI constitute 15–20% of all cases. MSI, reflecting
inactivation of the MMR genes, is present in nearly all cancers
from individuals with hereditary non-polyposis colorectal cancer
(HNPCC). The prevalence of MSI-H in appendiceal carcinomas,
reported at 2.8%, is associated with germline mutations.
MSI is usually associated with poorly
differentiated, mucin-producing tumors that are generated by
epithelial cells, giving rise to peritoneal carcinomatosis. MSI
linked to colorectal tumors is divided into two different
phenotypes, denominated as high (MSI-H) and low (MSI-L). The tumors
with MSI-H are more susceptible to treatment by chemotherapy, and
are thus associated with better survival. However, MSI-L tumors are
more resistant to adjuvant chemotherapy. Currently, the use of
adjuvant chemotherapy is extrapolated from the beneficial effect of
this treatment on colorectal cancer, although the validity of this
extrapolation is uncertain. The largest cohort of appendiceal
adenocarcinoma patients to date, which was recently reported,
demonstrated that there was a relative protective effect for
patients who received systemic chemotherapy compared with those who
did not, applicable to both the mucinous and non-mucinous
histological types (26). Due to the
low ERCC1 expression observed in appendiceal adenocarcinomas,
platinum agents, such as cisplatin or oxaliplatin, may be combined
with either 5-FU or gemcitabine. Data in the literature indicate
that the most effective regimen following surgical resection of
advanced (stage II and III) CRC is FOLFOX, comprising 5-FU,
leucovorin and oxaliplatin. This triad reduces the risk of
recurrence and improves survival. In the present report of a case
of appendiceal carcinoma, the patient received FOLFOX for 6 months
after recovering from a pancreatic fistula.
Over the last few years, new developments include
intraoperative hyperthermic intraperitoneal chemotherapy (27) with mitomycin at 40°C, and early
postoperative intraperitoneal chemotherapy with 5-FU. These are
considered to be effective adjuvant treatments for minimal residual
disease after debulking. The long-term survival rate of patients
undergoing complete debulking and having a low-grade tumor is 80%,
whereas this rate is ~45% at 20 years in patients with high-grade
tumors. In a small cohort of 40 patients with appendiceal mucinous
neoplasms (AMNs) diagnosed between 2000 and 2011, where tissue
microarrays were constructed from a representative block of the
primary tumor, CDX2 single-staining revealed a sensitivity of 93%
and a specificity of 56% for AMNs, whereas CK20 single-staining
demonstrated a sensitivity of 98% and a specificity of 50% for AMNs
(28). CDX2 is both a sensitive and
specific marker of intestinal differentiation, and it is
overexpressed in CRC cells compared with normal intestinal
epithelium; it is a potential marker of the effectiveness of
surgical resection or other local treatment modalities (29,30).
Cytoreductive surgery is a new technique employing peritonectomy
procedures to eradicate peritoneal carcinomatosis; judging by the
absence of lymph node and other metastases, this treatment
favorably affects the prognosis of survival for CRC patients.
Systematic reviews of CRC prognosis have
demonstrated that tumors exhibiting a MSI phenotype have a better
prognosis compared with those with a microsatellite stable pattern.
The improved prognosis in the hypermutated cases may be associated
with a strong immune response to the tumor caused by the expression
of neoantigens that cause an in situ lymphocytic reaction
(31). In the present case, MSI was
determined by the absence of specific nuclear staining against
three mismatch repair proteins (MLH1, MSH2 and MSH6). Tumors
displaying this pattern are MSI-H, or mismatch repair-deficient.
The predictive value of the MSI status to chemotherapy is important
due to the variable response, particularly in cases with reported
resistance to 5-FU (32). In this
report, the patient received 10 cycles of the standard adjuvant
treatment (FOLFOX) after surgical resection, with a good response
during the 5-year post-treatment clinical follow-up. Although more
prospective studies are required to correlate the prognosis with
response to adjuvant therapy in rare colon cancers, such as
appendiceal carcinoma, we consider that the molecular
characterization of the tumor, particularly the microsatellite
pattern, may help with the selection of the therapeutic scheme.
Acknowledgements
The authors would like to thank Dr Dulce Maria
Carrillo for the review of the literature.
Funding
No funding was received.
Availability of data and materials
The findings are contained within the manuscript.
Originals are kept in the medical records.
Authors' contributions
AMM was responsible for the study design, the
preparation of the manuscript and the draft the final manuscript.
FCM performed the pathology studies and prepared the figure for the
article. IDR and CCN, both surgeon physicians, contributed to the
discussion and reviewed the manuscript.
Ethics Approval and consent to
participate
Not applicable.
Consent for publication
Written informed consent was obtained from the
patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Samowitz WS, Curtin K, Ma KN, Schaffer D,
Coleman LW, Leppert M and Slattery ML: Microsatellite instability
in sporadic colon cancer is associated with an improved prognosis
at the population level. Cancer Epidemiol Biomarkers Prev.
10:917–923. 2001.PubMed/NCBI
|
|
2
|
Stadler ZK: Diagnosis and management of
DNA mismatch repair-deficient colorectal cancer. Hematol Oncol Clin
North Am. 29:29–41. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jacob S and Praz F: DNA mismatch repair
defects: Role in colorectal carcinogenesis. Biochimie. 84:27–47.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Syngal S, Fox EA, Eng C, Kolodner RD and
Garber JE: Sensitivity and specificity of clinical criteria for
hereditary non-polyposis colorectal cancer associated mutations in
MSH2 and MLH1. J Med Genet. 37:641–645. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Taggart MW, Galbincea J, Mansfield PF,
Fournier KF, Royal RE, Overman MJ, Rashid A and Abraham SC:
High-level microsatellite instability in appendiceal carcinomas. Am
J Surg Pathol. 37:1192–1200. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Andersson A, Bergdahl L and Boquist L:
Primary carcinoma of the appendix. Ann Surg. 183:53–57. 1976.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sugarbaker PH: Epithelial appendiceal
neoplasms. Cancer J. 15:225–235. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hananel N, Powsner E and Wolloch Y:
Adenocarcinoma of the appendix: An unusual disease. Eur J Surg.
164:859–862. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Iwuagwu OC, Jameel JK, Drew PJ, Hartley JE
and Monson JR: Primary carcinoma of the appendix-Hull series. Dig
Surg. 22:163–167. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cerame MA: A 25-year review of
adenocarcinoma of the appendix. A frequently perforating carcinoma.
Dis Colon Rectum. 31:145–150. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Turaga KK, Pappas SG and Gamblin T:
Importance of histologic subtype in the staging of appendiceal
tumors. Ann Surg Oncol. 19:1379–1385. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
O'Donnell ME, Badger SA, Beattie GC,
Carson J and Garstin WI: Malignant neoplasms of the appendix. Int J
Colorectal Dis. 22:1239–1248. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Misdraji J and Young RH: Primary
epithelial neoplasms and other epithelial lesions of the appendix
(excluding carcinoid tumors). Semin Diagn Pathol. 21:120–133. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Feizi I, Maleki N and Tavosi Z: Mucinous
adenocarcinoma of the appendix. J Res Med Sci. 20:103–104.
2015.PubMed/NCBI
|
|
15
|
Chua TC, Pelz JO and Morris DL: Surgery
for colorectal peritoneal carcinomatosis. Scand J Gastroenterol.
47:277–285. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Varisco B, McAlvin B, Dias J and Franga D:
Adenocarcinoid of the appendix: Is right hemicolectomy necessary? A
meta-analysis of retrospective chart reviews. Am Surg. 70:593–599.
2004.PubMed/NCBI
|
|
17
|
Proulx GM, Willett CG, Daley W and
Shellito PC: Appendiceal carcinoma: Patterns of failure following
surgery and implications for adjuvant therapy. J Surg Oncol.
66:51–53. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
McConnell YJ, Mack LA, Gui X, Carr NJ,
Sideris L, Temple WJ, Dubé P, Chandrakumaran K, Moran BJ and Cecil
TD: Cytoreductive surgery with hyperthermic intraperitoneal
chemotherapy: An emerging treatment option for advanced goblet cell
tumors of the appendix. Ann Surg Oncol. 21:1975–1982. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ung L, Chua TC and David LM: Peritoneal
metastases of lower gastrointestinal tract origin: A comparative
study of patient outcomes following cytoreduction and
intraperitoneal chemotherapy. J Cancer Res Clin Oncol.
139:1899–1908. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nash GM, Smith JD, Tang L, Weiser MR,
Temple LK, O'Reilly E, Saltz LB, Guillem JG and Paty PB: Lymph node
metastasis predicts disease recurrence in a single-center
experience of 70 stages 1–3 appendix cancers: A retrospective
review. Ann Surg Oncol. 22:3613–3617. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Samdani T, Schultheis M, Stadler Z, Shia
J, Fancher T, Misholy J, Weiser MR and Nash GM: Lymph node yield
after colectomy for cancer: Is absence of mismatch repair a factor?
Dis Colon Rectum. 58:288–293. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kelly KJ: Management of appendix cancer.
Clin Colon Rectal Surg. 28:247–255. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ribic CM, Sargent DJ, Moore MJ, Thibodeau
SN, French AJ, Goldberg RM, Hamilton SR, Laurent-Puig P, Gryfe R,
Shepherd LE, et al: Tumor microsatellite-instability status as a
predictor of benefit from fluorouracil-based adjuvant chemotherapy
for colon cancer. N Engl J Med. 349:247–257. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Carethers JM, Smith EJ, Behling CA, Nguyen
L, Tajima A, Doctolero RT, Cabrera BL, Goel A, Arnold CA, Miyai K
and Boland CR: Use of 5-fluorouracil and survival in patients with
microsatellite-unstable colorectal cancer. Gastroenterology.
126:394–401. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Xie X, Zhou Z, Song Y, Li W, Diao D, Dang
C and Zhang H: The management and prognostic prediction of
adenocarcinoma of appendix. Sci Rep. 6:390272016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Asare EA, Compton CC, Hanna NN, Kosinski
LA, Washington MK, Kakar S, Weiser MR and Overman MJ: The impact of
stage, grade, and mucinous histology on the efficacy of systemic
chemotherapy in adenocarcinomas of the appendix: Analysis of the
National Cancer Data Base. Cancer. 122:213–221. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Glockzin G, Gerken M, Lang SA,
Klinkhammer-Schalke M, Piso P and Schlitt HJ: Oxaliplatin-based
versus irinotecan-based hyperthermic intraperitoneal chemotherapy
(HIPEC) in patients with peritoneal metastasis from appendiceal and
colorectal cancer: A retrospective analysis. BMC Cancer.
14:8072014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Alsaad KO, Serra S, Schmitt A, Perren A
and Chetty R: Cytokeratins 7 and 20 immunoexpression profile in
goblet cell and classical carcinoids of appendix. Endocr Pathol.
18:16–22. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wong SC, Ng SS, Cheung MT, Luk LY, Chan
CM, Cheung AH, Lee VH, Lai PB, Ma BB, Hui EP, et al: Clinical
significance of CDX2-positive circulating tumour cells in
colorectal cancer patients. Br J Cancer. 104:1000–1006. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Liu Q, Teh M, Ito K, Shah N, Ito Y and
Yeoh KG: CDX2 expression is progressively decreased in human
gastric intestinal metaplasia, dysplasia and cancer. Mod Pathol.
20:1286–1297. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Smyrk TC, Watson P, Kaul K and Lynch HT:
Tumor-infiltrating lymphocytes are a marker for microsatellite
instability in colorectal carcinoma. Cancer. 91:2417–2422. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Arnold CN, Goel A and Boland CR: Role of
hMLH1 promoter hypermethylation in drug resistance to
5-fluorouracil in colorectal cancer cell lines. Int J Cancer.
106:66–73. 2003. View Article : Google Scholar : PubMed/NCBI
|